Volume 26, Issue 3 (Autumn 2025)
jrehab 2025, 26(3): 380-397 |
Back to browse issues page
Ethics code: IR.USWR.REC.1403.054
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
omidi O, Biglarian A, Heydari Z, Baghaie Rodsari R. Impact of a Milled Insole on Kinematic Gait Parameters in People With Mild Structural Leg Length Discrepancy. jrehab 2025; 26 (3) :380-397
URL: http://rehabilitationj.uswr.ac.ir/article-1-3572-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3572-en.html
1- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Biostatics and Epidemiology, Social Determinants of Health Research Center, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Rehabilitation and Medical Science, Iran-helal Institute of Applied Science and Technology, Tehran, Iran. & Research Center of Health Management in Mass Gadering, Red Crescent Society of the Islamic Republic of Iran, Tehran, Iran.
4- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,roshanakbaghaei@yahoo.com
2- Department of Biostatics and Epidemiology, Social Determinants of Health Research Center, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Rehabilitation and Medical Science, Iran-helal Institute of Applied Science and Technology, Tehran, Iran. & Research Center of Health Management in Mass Gadering, Red Crescent Society of the Islamic Republic of Iran, Tehran, Iran.
4- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Full-Text [PDF 4844 kb]
(163 Downloads)
| Abstract (HTML) (1880 Views)
Full-Text: (235 Views)
Introduction
Leg length discrepancy (LLD) or anisomelia refers to a significant difference in the length of two legs. According to statistics, 27% of adults have a LLD of more than 10 mm [1, 2]. The LLD is classified into two structural (shortness in bone length) and functional (asymmetry in lower limb mechanisms) types. individuals with structural LLD are classified into three groups based on the degree of shortness: Mild (<30 mm), moderate (30-60 mm), and severe (>60 mm) [3]. According to Moseley, an LLD of less than 20 mm falls into the mild category [4].
LLD is one of the most common musculoskeletal issues, significantly affecting gait. Some of the frequent changes in kinematic gait parameters due to LLD include increased supination, reduction or loss of the first rocker, forefoot impact during initial contact, vaulting, reduced ankle dorsiflexion, decreased knee flexion, reduced hip flexion and abduction, increased pelvic deviation in the shorter leg as well as increased pronation, enhanced ankle dorsiflexion, increased knee flexion, greater hip flexion and adduction in the longer leg [2, 5-9]. Gait disorders, as a key factor in functional independence, impose significant healthcare costs on the health system of countries each year; in the United States, the annual treatment expenses have exceeded one hundred billion dollars [10].
Due to limited information on the long-term effects of mild LLD, interventions are implemented cautiously [11]. Medical interventions are applied based on two factors: The degree of discrepancy and the severity of symptoms, and are carried out in two forms: Orthotic and surgical approaches [12]. Orthotic interventions are typically used for structural LLDs up to 50 millimeters [13-15]. These interventions include the use of insoles, heel lifts, modification of sole height, and splint use [14, 16, 17]. Insoles and heel lifts are primarily recommended as minimally invasive interventions to compensate for mild structural LLD [14]. Some studies have shown that the use of insoles and heel lifts can improve kinetic and kinematic gait variables [2, 18], while others have linked the effects of insoles to an individual’s adaptability and unconscious compensatory movements, and reported no improvement in gait parameters [7, 18]. Menez et al. [2] investigated the immediate changes in kinematic variables following the application of a thermoforming insole with 50% LLD correction. They divided participants into two groups: One with LLD <1 cm and the other with LLD >1 cm. Their results indicated a significant improvement in pelvic joint symmetry in the frontal plane and ankle symmetry in the sagittal plane. Tirtashi et al. [19] conducted a study to examine the effects of polyvinyl acetate insoles with 100% LLD correction on the maximum anterior and lateral pelvic tilt angles for both sides, hip abduction on both sides, knee abduction on both sides, and plantar flexion of the shorter leg. Their findings indicated significant changes in all variables except for the maximum anterior and lateral pelvic tilt of the shorter leg when using corrective insoles compared to regular shoes.
It seems that insole use is the most commonly used orthotic intervention for correcting mild structural LLDs. There is no available study on the effects of computer numerical control (CNC)-milled insoles on various gait parameters in individuals with structural LLD of <20 mm [2, 18, 20]. Therefore, this study aimed to investigate the effects of insoles milled by a CNC machine on the kinematic gait parameters of individuals with structural LLD <20 mm.
Materials and Methods
This is a quasi-experimental study, conducted in 2024. The study population consisted of 15 individuals with a mean age of 23±2.9 years with mild congenital structural LLD. Considering a 95% confidence interval (CI), a test power of 80%, a variance of 3.25, and an accuracy of 3.7 in pelvic movements in the frontal plane during the stance phase [20], the sample size was determined as 15. Participants were selected using a non-probability convenience sampling method from individuals aged 18-35 years who visited hospitals and rehabilitation clinics affiliated with the University of Social Welfare and Rehabilitation Sciences, based on the inclusion criteria. Eligible individuals were examined by a therapist and, after signing an informed consent form, they entered into the study. The inclusion criteria were a mild structural LLD (<2 cm) [2], and the ability to walk more than 30 meters without using a cane [21]. The exclusion criteria were the use of insoles or heel lifts in the past three months [21], systemic diseases such as rheumatoid arthritis [21], musculoskeletal and neurological disorders in the lower limbs [1], and a history of musculoskeletal injury or surgery in the lower limbs [22].
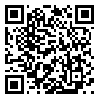
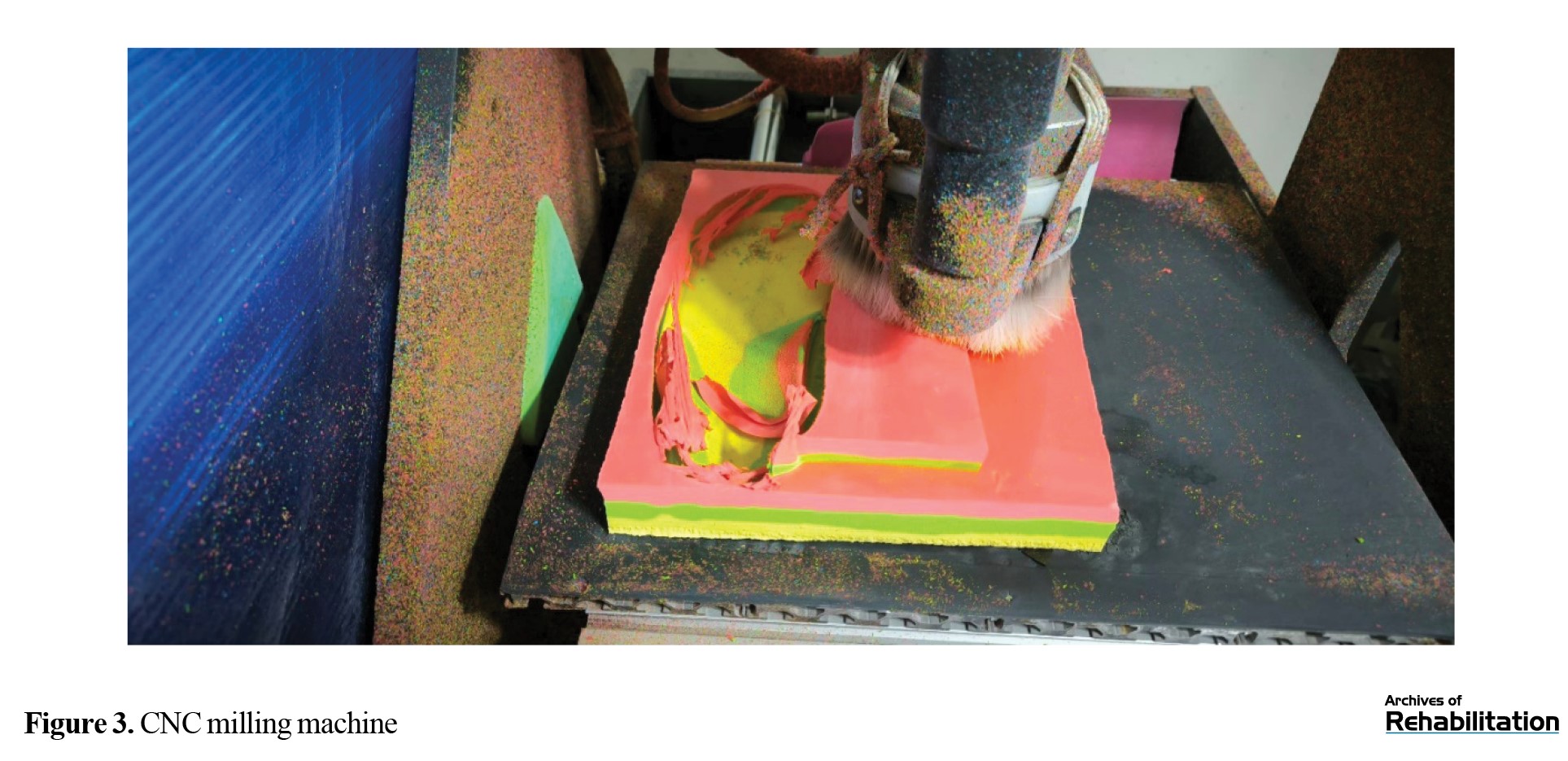
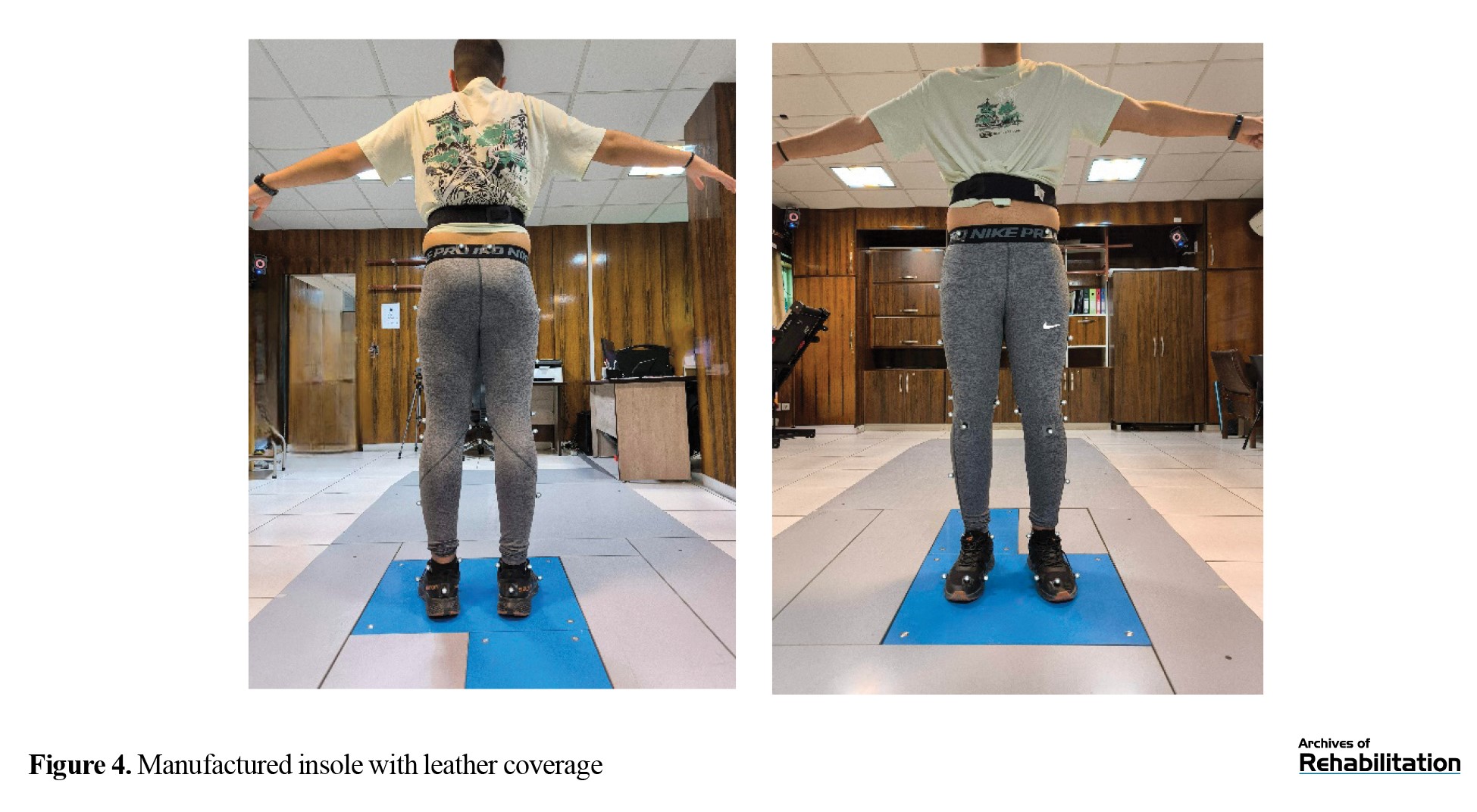
To create the insole, the LLD degree was first determined using radiography [23]. After scanning the individual’s foot with a scanner (Model 4452F40, Payatek Fanavaran Co., Iran; Figure 1), the insole was designed in Rhino software with a 30% lift to compensate for the discrepancy. The design was then transferred to ArtCAM software for G-code generation (Figure 2). Next, the insole was manufactured from ethylene-vinyl acetate (EVA) foam with a Shore A hardness of 30 using a CNC milling machine (Model PT-MILL, Payatek Fanavaran Co., Iran; Figure 3). To enhance durability and breathability, the insole was covered with synthetic leather. It has a standard amount of internal and external arch support, a metatarsal pad, and a heel cup (Figure 4). After participants wore tight-fitting sportswear and standard shoes, marker were placed different points of lower limbs according to the Plug-in protocol. The landmarks included the anterior and posterior iliac spines, external prominence of the greater trochanter, lateral epicondyle of the femur, mid-femur, proximal apex of the fibular head, anterior prominence of the tibia, mid-tibia, medial and lateral malleoli, Achilles tendon attachment to the calcaneus, and the borders of the first and fifth metatarsal heads [2], as shown in Figure 5. Participants were then asked to stand on a pressure plate to record the necessary static data. Then, to familiarize them with the laboratory environment, they were instructed to walk for ten minutes on a six-meter path at a self-selected speed. In the middle of this path, a Kistler pressure plate had been placed, surrounded by four MX T40-S infrared cameras and six Vicon Vero (v2.2) infrared cameras. Five gait cycles without insoles were first recorded. Then, participants were asked to repeat all previous steps while using the milled insoles. The test would be repeated if the individual’s leg was not correctly placed on the pressure plates.
After data collection, the relevant charts were generated using Microsoft Excel (2016) and MATLAB (R2024a) applications, and the SPSS software, version 23 was used for data description and analysis. After assessing the normality of data distribution, the paired t-test (for data with normal distribution) or the Wilcoxon signed-rank test (for data with abnormal distribution) was used to compare gait parameters with and without wearing insoles. The significance level was set at 0.05.
Results
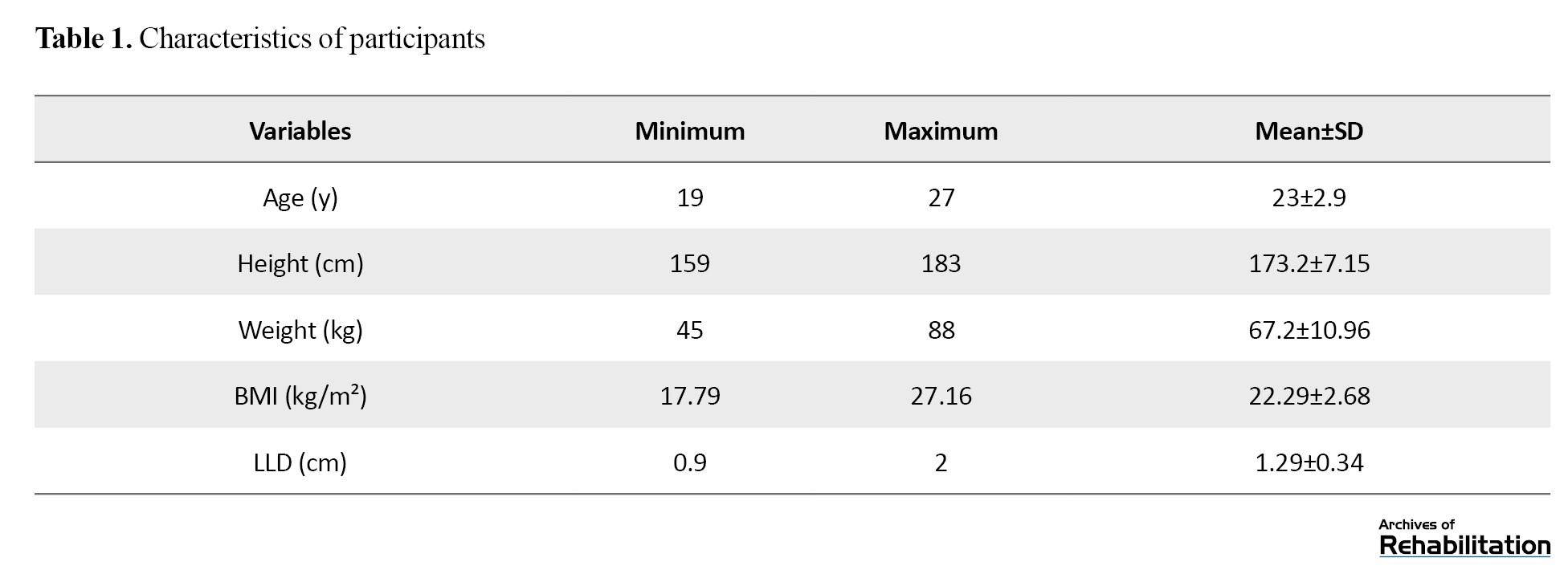
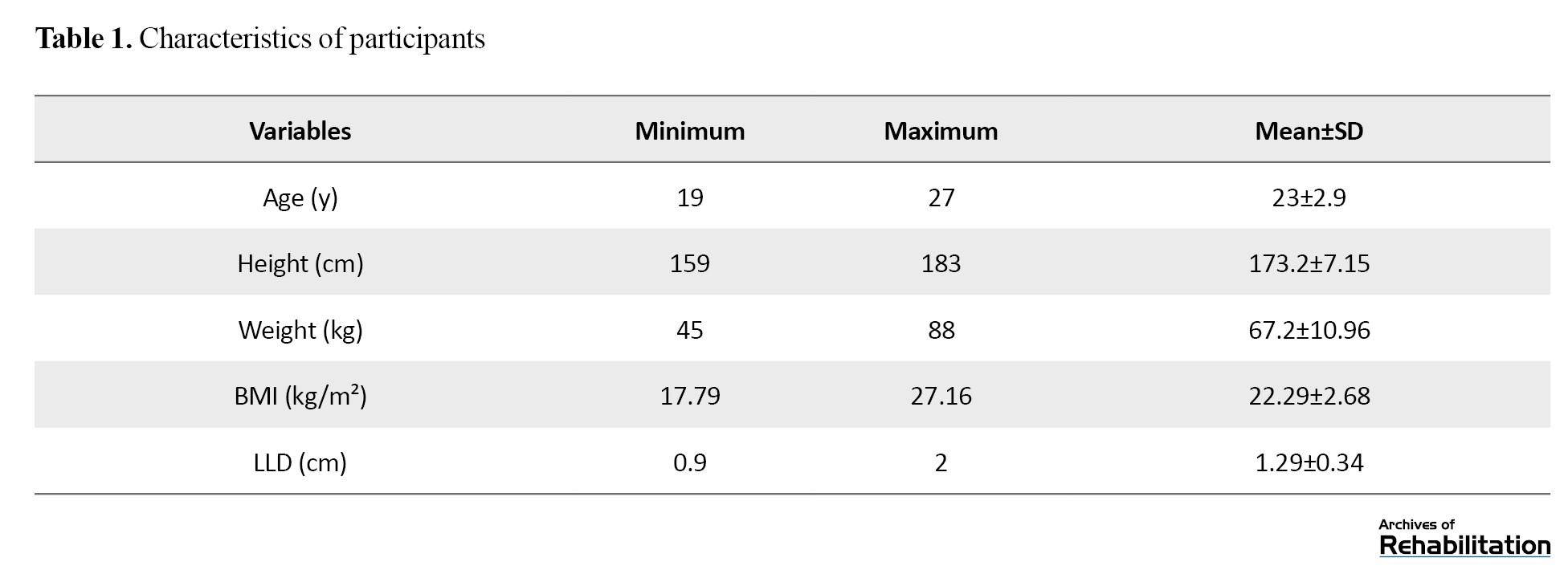
Participants included 6 females and 9 males, with a mean age of 23 years and a mean body mass index (BMI) of 22.29 kg/m². Based on radiographic imaging, their mean structural LLD was 1.29 cm (Table 1).
According to the results in Table 2, in the stance phase of gait, the mean range of motion (ROM) of the knee joint in the shorter leg significantly increased on the frontal plane after using the insole (P=0.03).
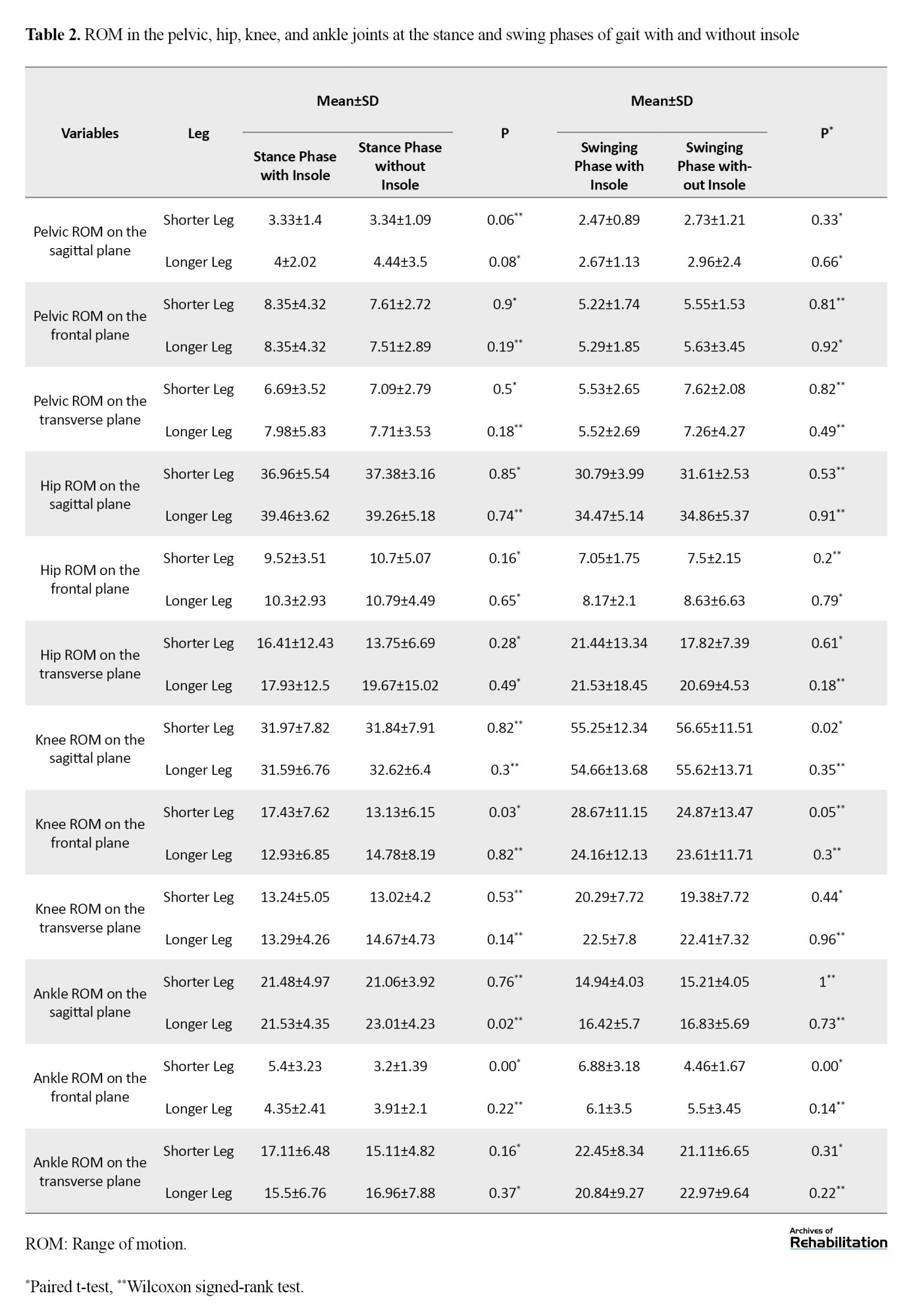
The mean ROM of the ankle joint in the longer leg significantly decreased after using the insole on the sagittal plane (P=0.02), while the mean ROM of the ankle joint in the shorter leg significantly increased on the frontal plane (P<0.001). In the swing phase, the mean ROM of the knee joint in the shorter leg significantly decreased on the sagittal plane (P=0.02), and the mean ROM of the ankle joint in the shorter leg significantly increased on the frontal plane (P<0.001).
Regarding changes in the maximum angle in the stance phase of gait (Table 3), the maximum angle of inversion in the ankle joints of both legs significantly increased (P=0.04 for shorter leg, P=0.02 for longer leg).
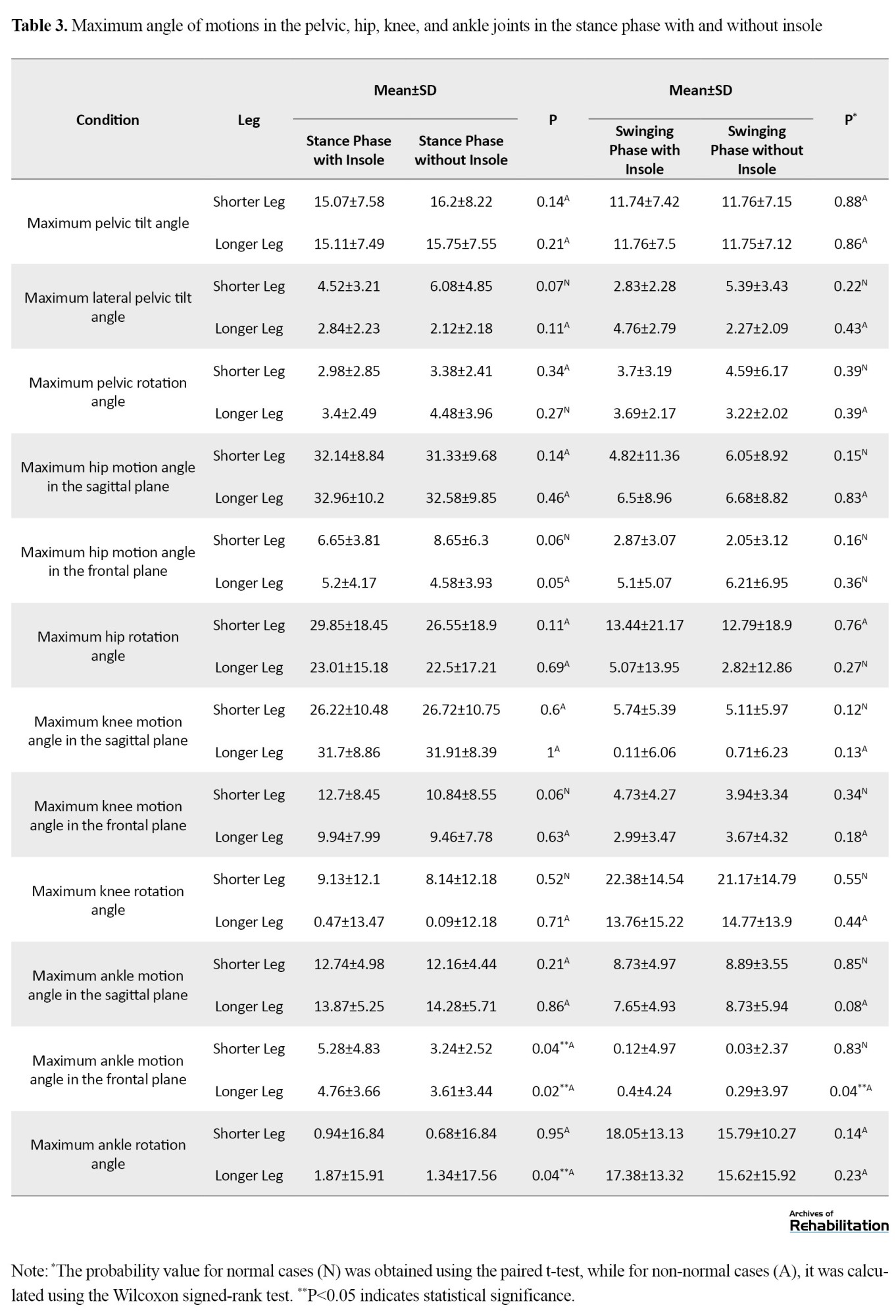
The maximum eversion angle of the ankle joint in the longer leg (P=0.04), and the maximum internal rotation angle of the ankle joint in the longer leg (P=0.04) also showed a significant increase.
Discussion
The purpose of this study was to examine the effects of CNC-milled insoles on various kinematic gait variables in individuals with mild structural LLD. The findings revealed significant changes in certain kinematic variables, including the knee ROM of the shorter leg on the frontal plane, the ankle ROM of the shorter leg on the frontal plane, and the ankle ROM of the longer leg on the sagittal plane during the stance phase of gait. In the swing phase, significant changes were observed in the knee ROM of the shorter leg on the sagittal plane and in the ankle ROM of the shorter limb on the frontal plane. Additionally, in the stance phase, the maximum ankle inversion angle in both legs, the maximum ankle eversion angle of the longer leg, and the maximum ankle internal rotation of the longer leg increased significantly after wearing the milled insole.
The results of this study support the results of previous studies indicating that mild structural LLD affects gait deviations [2, 5]. Additionally, these findings complement the work of Bangerter et al., who suggested that structural LLDs between 20 and 60 mm can lead to gait deviations [24]. Our findings are also in agreement with Resende et al.’s findings, which showed that the compensatory movements during walking in individuals with LLD were reduced after wearing corrective insoles [5]. Tirtashi et al. indicated significant changes in the maximum anterior and lateral pelvic tilt of the longer leg, hip abduction in both legs, knee abduction in both legs, and plantar flexion of the shorter leg when using a corrective insole compared to standard shoes [19]. Menez et al. also showed significant improvement in pelvic joint symmetry on the frontal plane and ankle alignment on the sagittal plane following a 50% LLD correction. The differences between the results of our study and those of Menez et al. and Tirtashi et al. may be due to variations in the degree of discrepancy correction. The non-significant changes in some gait parameters after wearing the milled insole in our study can be attributed to the specific amount of correction applied, warranting further studies using different correction rates. Another possible reason can be the short duration of assessing gait changes. Considering that individuals develop complex compensatory movements over the years, instant corrections may not be feasible, and long-term evaluations of insole effects on these mechanisms are necessary.
The limitations of this study included a small sample size and the absence of a control group, due to time and financial constraints. Another limitation was the short duration of insole impact evaluation due to financial problems and difficulties in long-term follow-up. This prevented a definitive conclusion regarding the durability and persistence of the results. In this regard, future studies should consider conducting research with a larger sample size and a longer duration, incorporating both control and experimental groups. This would allow for a more comprehensive evaluation of the effectiveness of insole use over time. Additionally, future research should examine the impact of different rates of LLD correction to gain a deeper understanding of the relationship between the degree of correction and the biomechanical responses. Furthermore, future studies are recommended to examine kinetic variables such as ground reaction forces, joint torques, and movement patterns. These variables can provide more precise and comprehensive insights into how insoles affect biomechanical performance, offering a deeper understanding of the study findings.
Conclusion
The use of CNC-milled insoles can help improve some compensatory movements resulting from LLD. The insole milled in this study can improve some kinematic gait parameters, such as the knee ROM of the shorter leg on the frontal plane, ankle ROM of the shorter leg on the frontal plane, and the ankle ROM of the longer limb on the sagittal plane during the stance phase of gait in people with mild structural LLD. Additionally, in the swing phase, significant improvements were observed in the knee ROM of the shorter leg on the sagittal plane and the ankle ROM of the shorter leg on the frontal plane. These findings suggest that the milled insole can help reduce the effects of LLD and enhance individuals’ movement performance. Therefore, CNC-milled insoles are recommended as an effective non-invasive intervention for managing mild structural LLDs.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1403.054). All participants signed a written informed consent form after being informed about the study procedure. They were free to leave the study at any time. Furthermore, all patient information remained confidential.
Funding
This study was extracted from the master’s thesis of Omid Omidi approved by the Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Authors' contributions
Conceptualization: Roshanak Baghaie Rodsari, Omid Omidi, and Zhaleh Heydari; Investigation and resources: Omid Omidi; Methodology, data analysis, and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Leg length discrepancy (LLD) or anisomelia refers to a significant difference in the length of two legs. According to statistics, 27% of adults have a LLD of more than 10 mm [1, 2]. The LLD is classified into two structural (shortness in bone length) and functional (asymmetry in lower limb mechanisms) types. individuals with structural LLD are classified into three groups based on the degree of shortness: Mild (<30 mm), moderate (30-60 mm), and severe (>60 mm) [3]. According to Moseley, an LLD of less than 20 mm falls into the mild category [4].
LLD is one of the most common musculoskeletal issues, significantly affecting gait. Some of the frequent changes in kinematic gait parameters due to LLD include increased supination, reduction or loss of the first rocker, forefoot impact during initial contact, vaulting, reduced ankle dorsiflexion, decreased knee flexion, reduced hip flexion and abduction, increased pelvic deviation in the shorter leg as well as increased pronation, enhanced ankle dorsiflexion, increased knee flexion, greater hip flexion and adduction in the longer leg [2, 5-9]. Gait disorders, as a key factor in functional independence, impose significant healthcare costs on the health system of countries each year; in the United States, the annual treatment expenses have exceeded one hundred billion dollars [10].
Due to limited information on the long-term effects of mild LLD, interventions are implemented cautiously [11]. Medical interventions are applied based on two factors: The degree of discrepancy and the severity of symptoms, and are carried out in two forms: Orthotic and surgical approaches [12]. Orthotic interventions are typically used for structural LLDs up to 50 millimeters [13-15]. These interventions include the use of insoles, heel lifts, modification of sole height, and splint use [14, 16, 17]. Insoles and heel lifts are primarily recommended as minimally invasive interventions to compensate for mild structural LLD [14]. Some studies have shown that the use of insoles and heel lifts can improve kinetic and kinematic gait variables [2, 18], while others have linked the effects of insoles to an individual’s adaptability and unconscious compensatory movements, and reported no improvement in gait parameters [7, 18]. Menez et al. [2] investigated the immediate changes in kinematic variables following the application of a thermoforming insole with 50% LLD correction. They divided participants into two groups: One with LLD <1 cm and the other with LLD >1 cm. Their results indicated a significant improvement in pelvic joint symmetry in the frontal plane and ankle symmetry in the sagittal plane. Tirtashi et al. [19] conducted a study to examine the effects of polyvinyl acetate insoles with 100% LLD correction on the maximum anterior and lateral pelvic tilt angles for both sides, hip abduction on both sides, knee abduction on both sides, and plantar flexion of the shorter leg. Their findings indicated significant changes in all variables except for the maximum anterior and lateral pelvic tilt of the shorter leg when using corrective insoles compared to regular shoes.
It seems that insole use is the most commonly used orthotic intervention for correcting mild structural LLDs. There is no available study on the effects of computer numerical control (CNC)-milled insoles on various gait parameters in individuals with structural LLD of <20 mm [2, 18, 20]. Therefore, this study aimed to investigate the effects of insoles milled by a CNC machine on the kinematic gait parameters of individuals with structural LLD <20 mm.
Materials and Methods
This is a quasi-experimental study, conducted in 2024. The study population consisted of 15 individuals with a mean age of 23±2.9 years with mild congenital structural LLD. Considering a 95% confidence interval (CI), a test power of 80%, a variance of 3.25, and an accuracy of 3.7 in pelvic movements in the frontal plane during the stance phase [20], the sample size was determined as 15. Participants were selected using a non-probability convenience sampling method from individuals aged 18-35 years who visited hospitals and rehabilitation clinics affiliated with the University of Social Welfare and Rehabilitation Sciences, based on the inclusion criteria. Eligible individuals were examined by a therapist and, after signing an informed consent form, they entered into the study. The inclusion criteria were a mild structural LLD (<2 cm) [2], and the ability to walk more than 30 meters without using a cane [21]. The exclusion criteria were the use of insoles or heel lifts in the past three months [21], systemic diseases such as rheumatoid arthritis [21], musculoskeletal and neurological disorders in the lower limbs [1], and a history of musculoskeletal injury or surgery in the lower limbs [22].
To create the insole, the LLD degree was first determined using radiography [23]. After scanning the individual’s foot with a scanner (Model 4452F40, Payatek Fanavaran Co., Iran; Figure 1), the insole was designed in Rhino software with a 30% lift to compensate for the discrepancy. The design was then transferred to ArtCAM software for G-code generation (Figure 2). Next, the insole was manufactured from ethylene-vinyl acetate (EVA) foam with a Shore A hardness of 30 using a CNC milling machine (Model PT-MILL, Payatek Fanavaran Co., Iran; Figure 3). To enhance durability and breathability, the insole was covered with synthetic leather. It has a standard amount of internal and external arch support, a metatarsal pad, and a heel cup (Figure 4). After participants wore tight-fitting sportswear and standard shoes, marker were placed different points of lower limbs according to the Plug-in protocol. The landmarks included the anterior and posterior iliac spines, external prominence of the greater trochanter, lateral epicondyle of the femur, mid-femur, proximal apex of the fibular head, anterior prominence of the tibia, mid-tibia, medial and lateral malleoli, Achilles tendon attachment to the calcaneus, and the borders of the first and fifth metatarsal heads [2], as shown in Figure 5. Participants were then asked to stand on a pressure plate to record the necessary static data. Then, to familiarize them with the laboratory environment, they were instructed to walk for ten minutes on a six-meter path at a self-selected speed. In the middle of this path, a Kistler pressure plate had been placed, surrounded by four MX T40-S infrared cameras and six Vicon Vero (v2.2) infrared cameras. Five gait cycles without insoles were first recorded. Then, participants were asked to repeat all previous steps while using the milled insoles. The test would be repeated if the individual’s leg was not correctly placed on the pressure plates.
After data collection, the relevant charts were generated using Microsoft Excel (2016) and MATLAB (R2024a) applications, and the SPSS software, version 23 was used for data description and analysis. After assessing the normality of data distribution, the paired t-test (for data with normal distribution) or the Wilcoxon signed-rank test (for data with abnormal distribution) was used to compare gait parameters with and without wearing insoles. The significance level was set at 0.05.
Results
Participants included 6 females and 9 males, with a mean age of 23 years and a mean body mass index (BMI) of 22.29 kg/m². Based on radiographic imaging, their mean structural LLD was 1.29 cm (Table 1).
According to the results in Table 2, in the stance phase of gait, the mean range of motion (ROM) of the knee joint in the shorter leg significantly increased on the frontal plane after using the insole (P=0.03).
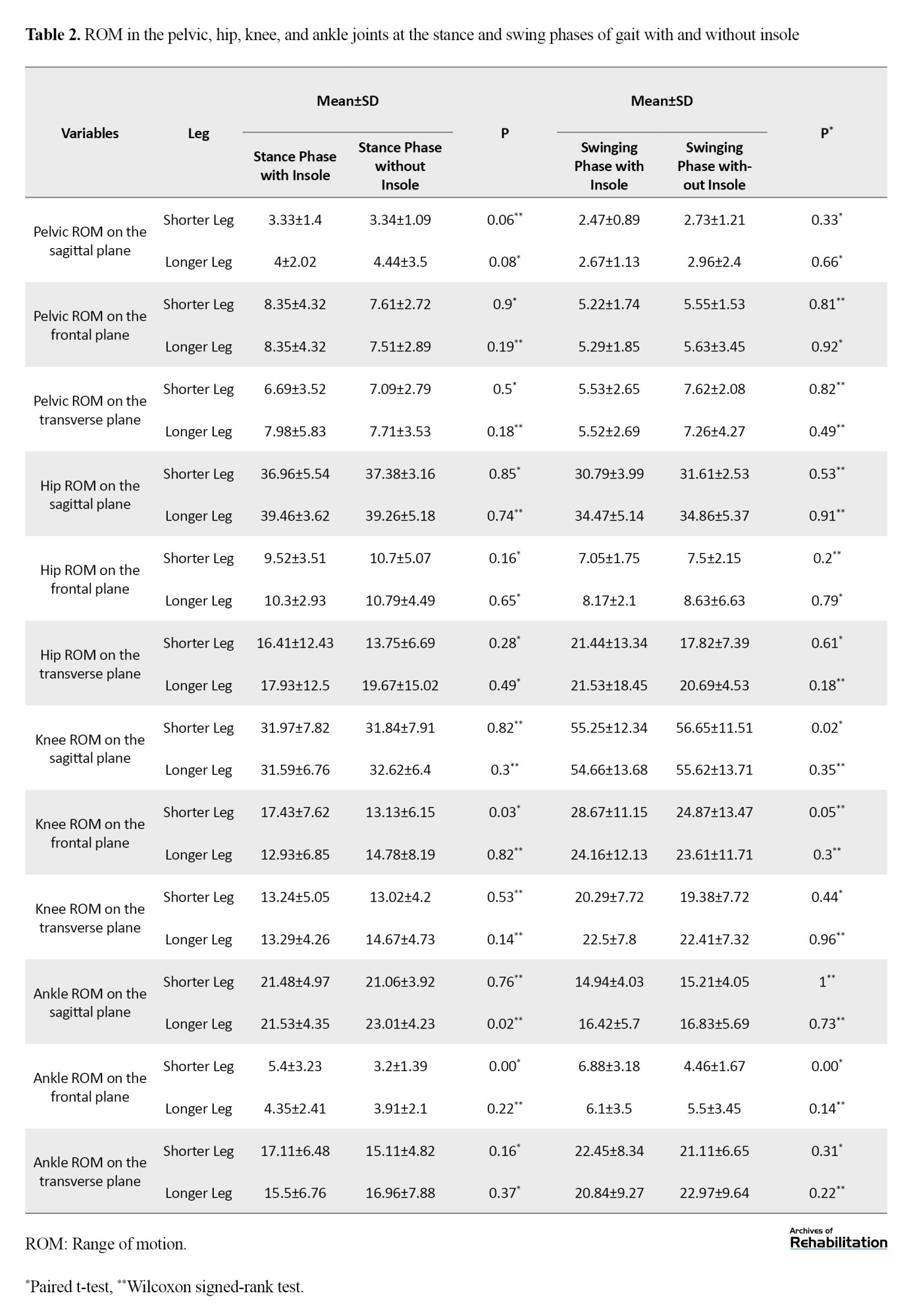
The mean ROM of the ankle joint in the longer leg significantly decreased after using the insole on the sagittal plane (P=0.02), while the mean ROM of the ankle joint in the shorter leg significantly increased on the frontal plane (P<0.001). In the swing phase, the mean ROM of the knee joint in the shorter leg significantly decreased on the sagittal plane (P=0.02), and the mean ROM of the ankle joint in the shorter leg significantly increased on the frontal plane (P<0.001).
Regarding changes in the maximum angle in the stance phase of gait (Table 3), the maximum angle of inversion in the ankle joints of both legs significantly increased (P=0.04 for shorter leg, P=0.02 for longer leg).
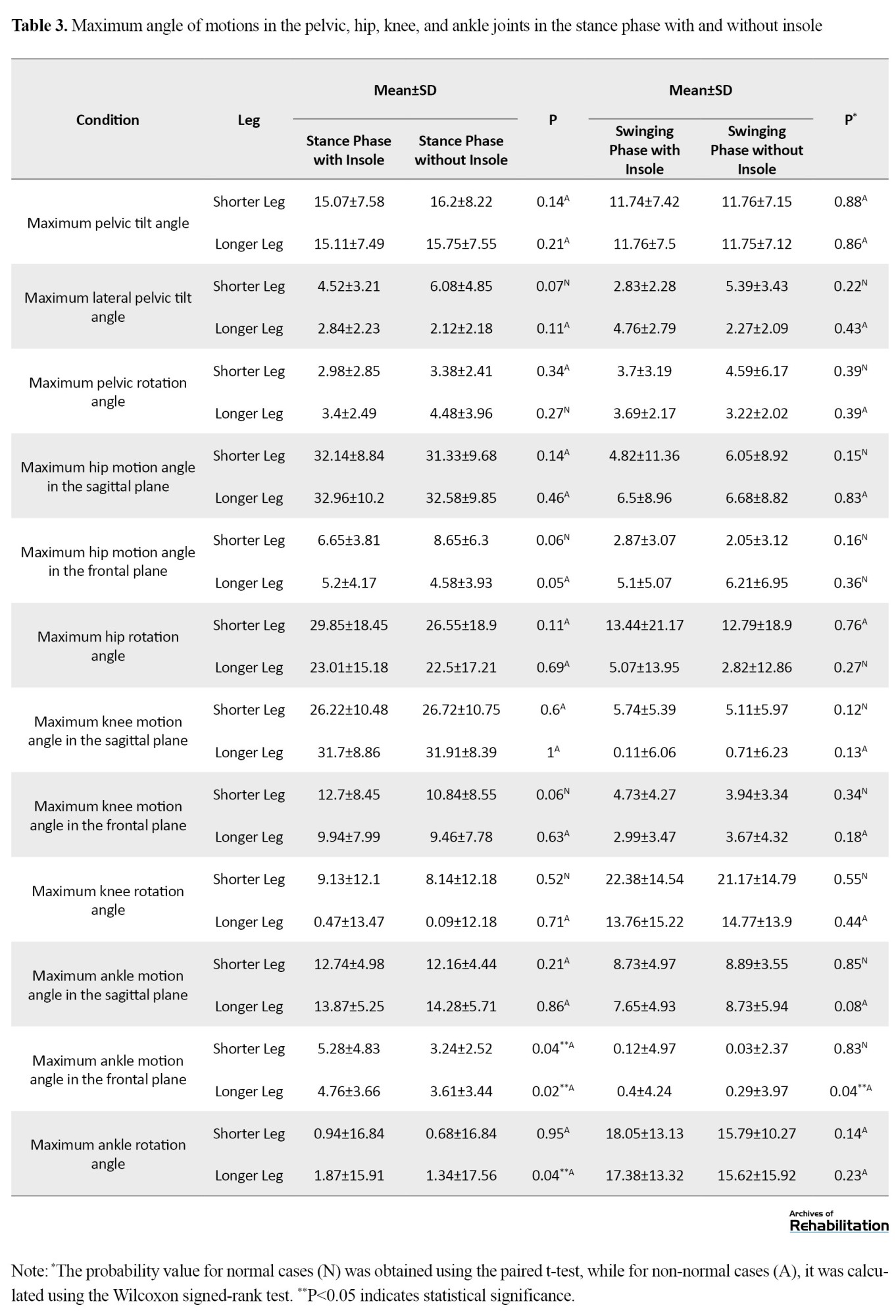
The maximum eversion angle of the ankle joint in the longer leg (P=0.04), and the maximum internal rotation angle of the ankle joint in the longer leg (P=0.04) also showed a significant increase.
Discussion
The purpose of this study was to examine the effects of CNC-milled insoles on various kinematic gait variables in individuals with mild structural LLD. The findings revealed significant changes in certain kinematic variables, including the knee ROM of the shorter leg on the frontal plane, the ankle ROM of the shorter leg on the frontal plane, and the ankle ROM of the longer leg on the sagittal plane during the stance phase of gait. In the swing phase, significant changes were observed in the knee ROM of the shorter leg on the sagittal plane and in the ankle ROM of the shorter limb on the frontal plane. Additionally, in the stance phase, the maximum ankle inversion angle in both legs, the maximum ankle eversion angle of the longer leg, and the maximum ankle internal rotation of the longer leg increased significantly after wearing the milled insole.
The results of this study support the results of previous studies indicating that mild structural LLD affects gait deviations [2, 5]. Additionally, these findings complement the work of Bangerter et al., who suggested that structural LLDs between 20 and 60 mm can lead to gait deviations [24]. Our findings are also in agreement with Resende et al.’s findings, which showed that the compensatory movements during walking in individuals with LLD were reduced after wearing corrective insoles [5]. Tirtashi et al. indicated significant changes in the maximum anterior and lateral pelvic tilt of the longer leg, hip abduction in both legs, knee abduction in both legs, and plantar flexion of the shorter leg when using a corrective insole compared to standard shoes [19]. Menez et al. also showed significant improvement in pelvic joint symmetry on the frontal plane and ankle alignment on the sagittal plane following a 50% LLD correction. The differences between the results of our study and those of Menez et al. and Tirtashi et al. may be due to variations in the degree of discrepancy correction. The non-significant changes in some gait parameters after wearing the milled insole in our study can be attributed to the specific amount of correction applied, warranting further studies using different correction rates. Another possible reason can be the short duration of assessing gait changes. Considering that individuals develop complex compensatory movements over the years, instant corrections may not be feasible, and long-term evaluations of insole effects on these mechanisms are necessary.
The limitations of this study included a small sample size and the absence of a control group, due to time and financial constraints. Another limitation was the short duration of insole impact evaluation due to financial problems and difficulties in long-term follow-up. This prevented a definitive conclusion regarding the durability and persistence of the results. In this regard, future studies should consider conducting research with a larger sample size and a longer duration, incorporating both control and experimental groups. This would allow for a more comprehensive evaluation of the effectiveness of insole use over time. Additionally, future research should examine the impact of different rates of LLD correction to gain a deeper understanding of the relationship between the degree of correction and the biomechanical responses. Furthermore, future studies are recommended to examine kinetic variables such as ground reaction forces, joint torques, and movement patterns. These variables can provide more precise and comprehensive insights into how insoles affect biomechanical performance, offering a deeper understanding of the study findings.
Conclusion
The use of CNC-milled insoles can help improve some compensatory movements resulting from LLD. The insole milled in this study can improve some kinematic gait parameters, such as the knee ROM of the shorter leg on the frontal plane, ankle ROM of the shorter leg on the frontal plane, and the ankle ROM of the longer limb on the sagittal plane during the stance phase of gait in people with mild structural LLD. Additionally, in the swing phase, significant improvements were observed in the knee ROM of the shorter leg on the sagittal plane and the ankle ROM of the shorter leg on the frontal plane. These findings suggest that the milled insole can help reduce the effects of LLD and enhance individuals’ movement performance. Therefore, CNC-milled insoles are recommended as an effective non-invasive intervention for managing mild structural LLDs.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1403.054). All participants signed a written informed consent form after being informed about the study procedure. They were free to leave the study at any time. Furthermore, all patient information remained confidential.
Funding
This study was extracted from the master’s thesis of Omid Omidi approved by the Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Authors' contributions
Conceptualization: Roshanak Baghaie Rodsari, Omid Omidi, and Zhaleh Heydari; Investigation and resources: Omid Omidi; Methodology, data analysis, and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Kim Y. Comparison of the effect of insole correction on three-dimensional knee joint moments during gait in standing workers with leg length discrepancy. Journal of Musculoskeletal Science and Technology. 2021; 5(1):21-6. [DOI:10.29273/jmst.2021.5.1.21]
- Menez C, L'Hermette M, Coquart J. Orthotic insoles improve gait symmetry and reduce immediate pain in subjects with mild leg length discrepancy. Frontiers in Sports and Active Living. 2020; 2:579152. [DOI:10.3389/fspor.2020.579152] [PMID]
- Brady RJ, Dean JB, Skinner TM, Gross MT. Limb length inequality: Clinical implications for assessment and intervention. Journal of Orthopaedic & Sports Physical Therapy. 2003; 33(5):221-34. [DOI:10.2519/jospt.2003.33.5.221] [PMID]
- Moseley CF. Assessment and prediction in leg-length discrepancy. Instructional Course Lectures. 1989; 38:325-30. [PMID]
- Resende RA, Kirkwood RN, Deluzio KJ, Cabral S, Fonseca ST. Biomechanical strategies implemented to compensate for mild leg length discrepancy during gait. Gait & Posture. 2016; 46:147-53. [DOI:10.1016/j.gaitpost.2016.03.012] [PMID]
- Ali A, Walsh M, O'Brien T, Dimitrov BD. The importance of submalleolar deformity in determining leg length discrepancy. The Surgeon. 2014; 12(4):201-5. [DOI:10.1016/j.surge.2013.12.003] [PMID]
- Khamis S, Carmeli E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait & Posture. 2017; 57:115-23. [DOI:10.1016/j.gaitpost.2017.05.028] [PMID]
- Assogba TF, Boulet S, Detrembleur C, Mahaudens P. The effects of real and artificial leg length discrepancy on mechanical work and energy cost during the gait. Gait & Posture. 2018; 59:147-51. [DOI:10.1016/j.gaitpost.2017.10.004] [PMID]
- Kwon YJ, Song M, Baek IH, Lee T. The effect of simulating a leg-length discrepancy on pelvic position and spinal posture. Journal of Physical Therapy Science. 2015; 27(3):689-91. [DOI:10.1589/jpts.27.689] [PMID]
- Campbell TM, Ghaedi B, Tanjong Ghogomu E, Ramsay T, Welch V. Shoe and heel lifts for leg length inequality in adults with musculoskeletal conditions. The Cochrane Database of Systematic Reviews. 2021; 2021(12):CD014456. [PMCID]
- Gordon JE, Davis LE. Leg Length Discrepancy: The natural history (and what do we really know). Journal of Pediatric Orthopedics. 2019; 39(6):S10-3. [DOI:10.1097/BPO.0000000000001396] [PMID]
- Vogt B, Gosheger G, Wirth T, Horn J, Rödl R. Leg length discrepancy- treatment indications and strategies. Deutsches Arzteblatt International. 2020; 117(24):405-11. [DOI:10.3238/arztebl.2020.0405] [PMID]
- Kotaška J, Trč T. Limb shortening in the management of leg length discrepancy. Casopis Lekaru Ceskych. 2016; 155(8):417-22. [PMID]
- Hefti F, Hasler C, Krieg A. [Achsen und Längen (Persian)]. In: Hefti F, editor. Kinderorthopädie in der Praxis. Heidelberg: Springer; 2014. [DOI:10.1007/978-3-642-44995-6_10]
- Althobaiti MS, Aloraini LI, Alamri S, Binsaddik OK, Alobaysi YMY, Alabdulrahman FK, et al. Updates in the management of leg length discrepancy: A systematic review. Cureus. 2024; 16(6):e62599. [DOI:10.7759/cureus.62599]
- Hyungsoo S, Hyunsung K. Effects of self exercise program on leg length and balance in subjects with leg-length discrepancy. Journal of International Academy of Physical Therapy Research. 2020; 11(4):2197-202. [DOI:10.20540/jiaptr.2020.11.4.2197]
- Campbell TM, Ghaedi BB, Tanjong Ghogomu E, Welch V. Shoe lifts for leg length discrepancy in adults with common painful musculoskeletal conditions: A systematic review of the literature. Archives of Physical Medicine and Rehabilitation. 2018; 99(5):981-93.e2. [DOI:10.1016/j.apmr.2017.10.027] [PMID]
- Shi Y, Pang H, Xu H, Li X, Cao Y, Merryweather A, et al. Effects of orthotic insole on gait patterns in children with mild leg length discrepancy. Gait & Posture. 2022; 93:191-7. [DOI:10.1016/j.gaitpost.2022.02.003] [PMID]
- Tirtashi FH, Eslami M, Taghipour M. Effect of shoe insole on the dynamics of lower extremities in individuals with leg length discrepancy during walking. Journal of Bodywork and Movement Therapies. 2022; 31:51-56. [DOI:10.1016/j.jbmt.2022.03.006] [PMID]
- Kim Y. Effect of correction of leg length discrepancy on the biomechanical characteristics of the pelvis and hip joints among standing workers. Work. 2022; 71(4):1129-36. [DOI:10.3233/WOR-205160] [PMID]
- Wang K, Lu C, Ye R, He W, Wei X, Li Y, et al. Research and development of 3D printing orthotic insoles and preliminary treatment of leg length discrepancy patients. Technology and Health Care. 2020; 28(6):615-24. [DOI:10.3233/THC-202170] [PMID]
- D'Amico M, Kinel E, Roncoletta P. Leg length discrepancy and nonspecific low back pain: 3-D stereophotogrammetric quantitative posture evaluation confirms positive effects of customized heel-lift orthotics. Frontiers in Bioengineering and Biotechnology. 2022; 9:743132. [DOI:10.3389/fbioe.2021.743132] [PMID]
- Ashour R, Abdelraouf O, Abdallah A, Sweif R. Effect of footwear modification on postural symmetry and body balance in leg length Discrepancy: A randomized controlled study. International Journal of Osteopathic Medicine. 2019; 32:13-20. [DOI:10.1016/j.ijosm.2019.02.001]
- Bangerter C, Romkes J, Lorenzetti S, Krieg AH, Hasler CC, Brunner R, et al. What are the biomechanical consequences of a structural leg length discrepancy on the adolescent spine during walking? Gait & Posture. 2019; 68:506-13. [DOI:10.1016/j.gaitpost.2018.12.040] [PMID]
Type of Study: Applicable |
Subject:
Orthotics & Prosthetics
Received: 25/11/2024 | Accepted: 1/07/2025 | Published: 1/10/2025
Received: 25/11/2024 | Accepted: 1/07/2025 | Published: 1/10/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |