Volume 26, Issue 4 (Winter 2026)
jrehab 2026, 26(4): 510-527 |
Back to browse issues page
Ethics code: IR.USWR.REC.1402.099
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Afshari M, Najafi Z, Foroughi Z, Abdi K. Strengthen of Stewardship of Rehabilitation Services in Iran: A Policy Brief. jrehab 2026; 26 (4) :510-527
URL: http://rehabilitationj.uswr.ac.ir/article-1-3669-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3669-en.html
1- Social Determinants of Health Research Center, Saveh University of Medical Sciences, Saveh, Iran.
2- Department of Management, Economic and Health Policy, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
3- Education Development Center, Iran University of Medical Sciences, Tehran, Iran.
4- Social Determinants of Health Research Center, Social Health Research Institute, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Department of Rehabilitation Management, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,k55abdi@yahoo.com
2- Department of Management, Economic and Health Policy, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
3- Education Development Center, Iran University of Medical Sciences, Tehran, Iran.
4- Social Determinants of Health Research Center, Social Health Research Institute, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Department of Rehabilitation Management, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Full-Text [PDF 2183 kb]
(65 Downloads)
| Abstract (HTML) (1321 Views)
Full-Text: (44 Views)
Introduction
Rehabilitation services are considered one of the key pillars of the health system and play a fundamental role in improving quality of life, reducing social costs, and increasing social participation for individuals with disabilities [1]. Given the aging population, the rise in non-communicable diseases, and the high prevalence of disabilities, the need for rehabilitation services is increasingly growing [2]. It is projected that by 2050, approximately 2.1 billion people over 60 years old—equivalent to more than 22% of the world’s population—will require rehabilitation services, with 80% of them living in low- and middle-income countries, including Iran [3]. However, the absence of a clear and efficient stewardship structure poses a major barrier to achieving equitable coverage of rehabilitation services in Iran [4, 5].
In Iran, despite the multiplicity of responsible institutions in this field, integrated stewardship and governance of rehabilitation services have not yet been defined. Overlapping responsibilities among the Ministry of Health, the Welfare Organization, the Red Crescent Society, the Martyrs Foundation, and the Exceptional Education Organization have led to resource dispersion, parallel work, and reduced policy effectiveness [6, 7].
Existing studies and evidence emphasize that stewardship is the missing link in rehabilitation within Iran’s health system and its problems in the country have been classified as the result of unbalanced policies and laws, irresponsible intervention, weak comprehensive supervision, lack of thoughtful and compassionate management, and intra- and inter-sectoral incoordination [6, 7].
In the country’s upstream documents, such as the General Health Policies [8], and also in World Health Organization (WHO) documents [9], the Ministry of Health is introduced as the steward of the health system. This recommendation includes rehabilitation services as one of the key dimensions of the health system. However, this issue remains an unresolved challenge in Iran [10]. In Iran, since the 1980s, the Welfare Organization has been recognized as the primary steward of rehabilitation. But in subsequent decades, the Ministry of Health and other institutions also entered the field of service provision, resulting in fragmentation and duplication [5, 10]. The outcome of this ambiguity in rehabilitation stewardship has been the failure to prioritize rehabilitation in health system policies and the lack of achieving equity in societal access to rehabilitation services [11-13].
Despite this evidence, a significant knowledge gap persists in Iran’s policy landscape regarding the stewardship of rehabilitation services. Most existing studies have focused on service aspects, with less attention to analyzing governance structures. Therefore, the authors conducted a mixed-methods study to analyze the current situation and propose policy solutions to strengthen the stewardship of rehabilitation services in Iran [1, 10, 14]. This policy brief, derived from that research effort, addresses the question: “What are the strategies for improving the unclear stewardship status of rehabilitation services in Iran?” It is hoped that it will provide a clear path forward for policymakers and health system managers, enabling them to take a significant step toward providing equitable rehabilitation services to society and contributing to universal health coverage by clarifying and strengthening the position of rehabilitation stewardship.
Materials and Methods
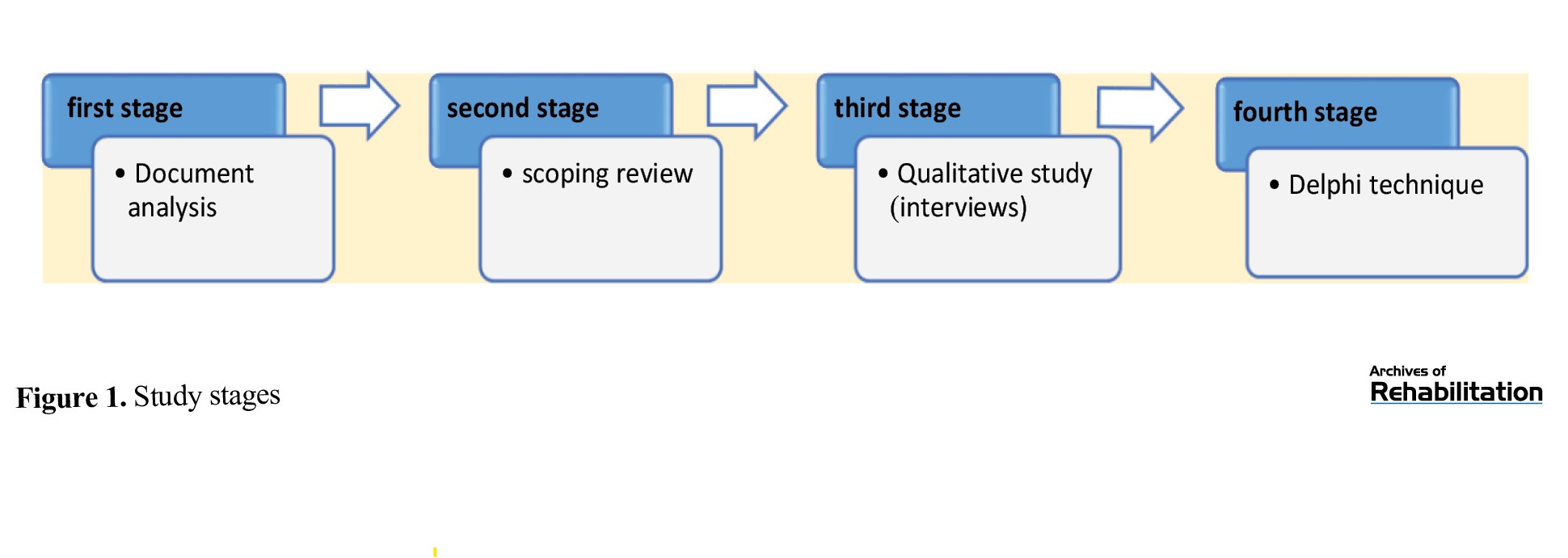
This policy brief is derived from the findings of a research project conducted by the authors in 2024. The aforementioned study was conducted using a mixed-methods approach in four stages (Figure 1).
Rehabilitation services are considered one of the key pillars of the health system and play a fundamental role in improving quality of life, reducing social costs, and increasing social participation for individuals with disabilities [1]. Given the aging population, the rise in non-communicable diseases, and the high prevalence of disabilities, the need for rehabilitation services is increasingly growing [2]. It is projected that by 2050, approximately 2.1 billion people over 60 years old—equivalent to more than 22% of the world’s population—will require rehabilitation services, with 80% of them living in low- and middle-income countries, including Iran [3]. However, the absence of a clear and efficient stewardship structure poses a major barrier to achieving equitable coverage of rehabilitation services in Iran [4, 5].
In Iran, despite the multiplicity of responsible institutions in this field, integrated stewardship and governance of rehabilitation services have not yet been defined. Overlapping responsibilities among the Ministry of Health, the Welfare Organization, the Red Crescent Society, the Martyrs Foundation, and the Exceptional Education Organization have led to resource dispersion, parallel work, and reduced policy effectiveness [6, 7].
Existing studies and evidence emphasize that stewardship is the missing link in rehabilitation within Iran’s health system and its problems in the country have been classified as the result of unbalanced policies and laws, irresponsible intervention, weak comprehensive supervision, lack of thoughtful and compassionate management, and intra- and inter-sectoral incoordination [6, 7].
In the country’s upstream documents, such as the General Health Policies [8], and also in World Health Organization (WHO) documents [9], the Ministry of Health is introduced as the steward of the health system. This recommendation includes rehabilitation services as one of the key dimensions of the health system. However, this issue remains an unresolved challenge in Iran [10]. In Iran, since the 1980s, the Welfare Organization has been recognized as the primary steward of rehabilitation. But in subsequent decades, the Ministry of Health and other institutions also entered the field of service provision, resulting in fragmentation and duplication [5, 10]. The outcome of this ambiguity in rehabilitation stewardship has been the failure to prioritize rehabilitation in health system policies and the lack of achieving equity in societal access to rehabilitation services [11-13].
Despite this evidence, a significant knowledge gap persists in Iran’s policy landscape regarding the stewardship of rehabilitation services. Most existing studies have focused on service aspects, with less attention to analyzing governance structures. Therefore, the authors conducted a mixed-methods study to analyze the current situation and propose policy solutions to strengthen the stewardship of rehabilitation services in Iran [1, 10, 14]. This policy brief, derived from that research effort, addresses the question: “What are the strategies for improving the unclear stewardship status of rehabilitation services in Iran?” It is hoped that it will provide a clear path forward for policymakers and health system managers, enabling them to take a significant step toward providing equitable rehabilitation services to society and contributing to universal health coverage by clarifying and strengthening the position of rehabilitation stewardship.
Materials and Methods
This policy brief is derived from the findings of a research project conducted by the authors in 2024. The aforementioned study was conducted using a mixed-methods approach in four stages (Figure 1).
This research was a prospective policy analysis study aimed at policy analysis for policymaking, with the goal of developing policy strategies to enhance the stewardship of rehabilitation services in Iran. In the first stage, documents and upstream policies, laws, and frameworks for the stewardship of rehabilitation services in Iran [10]band globally were analyzed. Additionally, the existing gap between rehabilitation stewardship in Iran and the world was examined. In the second stage, through a scoping review [15], published articles on strategies and challenges related to rehabilitation stewardship were reviewed. The first and second stages, in addition to providing deeper understanding and insight for the researchers on the topic, were used in preparing the interview guide and compiling an initial list of key actors in rehabilitation stewardship in Iran to identify potential interviewees, as well as for stakeholder analysis. In the third stage, using the perspectives and experiences of key informed individuals, stakeholders, and various role-players obtained through semi-structured interviews, the position, role, and relationships of key actors in rehabilitation stewardship in Iran, the process of rehabilitation stewardship in Iran, and the contextual factors influencing rehabilitation stewardship in Iran were examined [14]. In the fourth stage, after synthesizing the results from the previous stages, the researchers developed initial policy options (drafts) and then evaluated them based on four criteria—desirability, feasibility, importance, and appropriateness—using the Turoff policy Delphi technique model [16]. A checklist of policy options was prepared and shared with experts, and their final opinions on the policy options were incorporated.
Policy recommendations
The Veillard et al. [17] framework for health system stewardship was used to identify and propose policy solutions. This framework outlines six stewardship functions in relation to the national context, values, and ultimate goals pursued by the health system. These six dimensions include:
1) Setting the health vision and strategy to achieve better health; 2) influencing all sectors for better health; 3) governing the health system in alignment with prevailing values; 4) ensuring the health system design aligns with health system goals; 5) enhancing current legal and regulatory tools; 6) collecting, disseminating, and utilizing information [17].
Enhancing the health vision and strategy for better access to rehabilitation services
In order to achieve the health vision and strategy for better rehabilitation services, actions must be taken in three dimensions: social, economic, and technological.
Social dimension
In the social dimension, the following solutions are proposed to improve rehabilitation stewardship:
1) Increasing political commitment and prioritizing rehabilitation services in health system policymaking by changing the perspectives and attitudes of policymakers, managers, and health service providers through holding educational programs to raise awareness about the importance of rehabilitation; 2) specialized training to integrate a culture of serving people with disabilities at different levels of producing public and individual goods and services; 3) adopting a holistic approach to providing rehabilitation services at both policymaking and service delivery levels; 4) education and awareness-raising at the family level for caring for patients with disabilities, and activating the role of society and organizations in combating discrimination against people with disabilities by utilizing mass media for information dissemination and improving societal attitudes; 5) engaging and utilizing people with disabilities and their representatives in rehabilitation policymaking to enhance responsiveness, efficiency, effectiveness, and sustainability of programs, and to strengthen decision-making and user satisfaction with services; 6) Strengthening and empowering non-governmental organizations (NGOs) run by people with disabilities with the support of the government sector.
Economic and technological dimension
In the economic and technological dimension, the following solutions can be guiding:
1) Utilizing support facilities and creating incentives for government and private sector organizations providing rehabilitation services; 2) investing in knowledge-based and domestic companies in the field of rehabilitation technology; 3) upgrading and improving technological infrastructure to facilitate the participation of people with disabilities in society.
Influencing other sectors and advocacy for strengthening rehabilitation services
Since rehabilitation services require intersectoral collaborations, the following solutions are proposed to strengthen these collaborations:
1) Advocacy to address rehabilitation services in the country’s general policies, vision document, and development plans, and strengthening advocacy from the Health Commission of Parliament regarding elevating the position of rehabilitation in the country’s health system; 2) using policy discourse to garner cooperation from all organizations involved in rehabilitation; 3) supporting private and civil society institutions in providing rehabilitation services; 4) increasing community participation in rehabilitation services through raising public awareness; 5) forming alliances among various rehabilitation associations, such as optometry, audiology, speech therapy, etc., through the establishment of a National Rehabilitation Network to increase the participation of rehabilitation specialists in the policymaking process.
Strengthening health system governance
Given the multisectoral nature of rehabilitation service provision, there is a need for integrated governance at the macro level, free from duplication. Therefore, the following solutions are proposed:
1) Creating integration, coordination, and collaboration in rehabilitation service stewardship through the establishment of a Supreme Council for Welfare, Rehabilitation, and Aging at the national level under the President and Cabinet as the legislative and central governance body that will develop a comprehensive rehabilitation services document. This document will guide all subordinate agencies, their roles, and their interactions with other agencies; 2) creating and developing an active role for Physical Medicine and Rehabilitation Departments in the Supreme Council for Welfare, Rehabilitation, and Aging to facilitate leadership and governance skills; 3) creating and developing an active role for representatives of government organizations involved in providing rehabilitation services and representatives of civil society organizations in the field of rehabilitation in the Supreme Council for Welfare, Rehabilitation, and Aging; 4) establishing and developing a Deputy for Rehabilitation and Social Health under the Minister of Health to strengthen the stewardship role of rehabilitation services in the Ministry of Health; 5) forming an Aging and Rehabilitation Commission in the Islamic Consultative Assembly (Parliament); 6) developing strategic and operational programs for various levels of rehabilitation service provision to clarify the roles of different actors; 7) increasing and expanding the capacities of the Welfare Organization as the executive arm for rehabilitation services and support services.
Strengthening the health system in line with rehabilitation service stewardship
Since the health system plays a special role in the stewardship of rehabilitation services, the following solutions are proposed to strengthen the health system:
1) Gradually shifting the Ministry of Health’s approach from a treatment-oriented perspective to a preventive one, to understand the importance of rehabilitation services by incorporating rehabilitation outcome indicators into the performance evaluation system of hospitals and health centers; 2) determining the position of rehabilitation services at all first, second, and third levels in the country’s comprehensive rehabilitation document and integrating rehabilitation services into the primary health care system and strengthening the referral system to expand inclusive rehabilitation services; 3) paying attention to the importance of assistive technologies in rehabilitation and improving access to modern assistive equipment for individuals with disabilities; 4) specifying hierarchies and accountability levels in rehabilitation services and delegating authority commensurate with the assigned duties to each accountable entity; 5) developing and implementing policies for sustainable financing and efficient insurance coverage for rehabilitation services (with emphasis on horizontal and vertical equity); 6) developing and implementing policies to increase capacity and equitable distribution of rehabilitation specialists and to develop knowledge and skills of human resources active in rehabilitation management; 7) expanding comprehensive rehabilitation centers for individuals with disabilities in collaboration with the non-governmental sector; 8) revising the curricula of various medical sciences disciplines to familiarize them with rehabilitation services and enhance their ability to collaborate in interdisciplinary teams.
Strengthening legal and regulatory tools for rehabilitation services
One of the most important dimensions of improving the stewardship of rehabilitation services is strengthening the legal and regulatory tools for rehabilitation services. The following strategies can enhance the legal and regulatory capacity of rehabilitation services:
1) Implementation of the National Rehabilitation Services Document, standards, protocols, and clinical guidelines in various domains of rehabilitation services to guide service providers in ensuring the integrity, safety, and quality of the services provided; 2) supporting adopted policies in the field of rehabilitation services through the development of comprehensive regulatory laws and regulations that ensure the implementation of these policies and provide a basis for monitoring and supervising their execution; 3) determining the structure for supervision, monitoring, and control of rehabilitation services under the Comprehensive Rehabilitation Services Document, including levels of supervision, monitoring, and control for rehabilitation services, and establishing mechanisms for the full and proper implementation of the Comprehensive Law on People with Disabilities; 4) determining the structure for supervision, monitoring, control, and accountability levels for rehabilitation services under the Comprehensive Rehabilitation Services Document, along with delegating appropriate levels of authority corresponding to the tasks assigned to each accountable entity in the document; 5) establishing an accreditation mechanism for rehabilitation centers by the Ministry of Health, including the development of key performance indicators, care standards, and accreditation criteria for these centers.
Strengthening methods of collecting, disseminating, and utilizing information on rehabilitation services
Improving the governance of rehabilitation services requires proper policy-making and planning, taking into account the current situation and anticipating future needs. In this regard, the following strategies are proposed:
1) Creating and developing the infrastructure for a comprehensive rehabilitation services information management system, including designating the responsible entity in this area, registering individuals with disabilities and impairments, registering rehabilitation services, registering human resources and specialists in the rehabilitation field, registering information on rehabilitation centers, and integrating it into the current electronic health record; 2) integrating national rehabilitation information through the sharing of data among various agencies; 3) appropriately and efficiently allocating resources following precise needs assessment and data-driven planning; 4) strengthening investment in rehabilitation research to leverage scientific evidence in rehabilitation policy-making and to enhance policymakers’ understanding and awareness for prioritizing the needs of individuals with disabilities.
Policy recommendation (top proposed policy)
The top policy recommendation in this study is shaped based on the six-dimensional governance framework of the health system by Willard and colleagues. A comprehensive and coordinated approach that encompasses all relevant sectors and actors:
Creating an integrated and centralized governance structure
Establishing the Supreme Council for Welfare, Rehabilitation, and Aging, chaired by the President, as the supervisory and legislative body; Developing a comprehensive national rehabilitation services document with precise task descriptions for agencies and coordination among them.
Strengthening specialized human resources and continuous education
Reviewing educational programs in medical and rehabilitation disciplines, developing interdisciplinary training, and ensuring equitable distribution of rehabilitation specialists.
Sustainable financing through efficient insurance mechanisms
Reforming the insurance system to provide comprehensive coverage for rehabilitation services, accompanied by incentive policies for both public and private sectors.
Strengthening legal and regulatory tools
Approving and implementing comprehensive laws supporting individuals with disabilities, developing standards and protocols for rehabilitation services, and establishing an accreditation system for rehabilitation centers.
Developing an information system and data-based research
Creating a comprehensive registration and management system for rehabilitation information, integrating data, and facilitating access to scientific evidence for intelligent policymaking.
Increasing community participation and non-governmental organizations
Empowering and enhancing the role of NGOs, along with active involvement of individuals with disabilities in the decision-making process, to ensure accountability and effectiveness of policies.
This proposed policy, with an emphasis on centralization and transparency in the roles of actors, can pave the way for improving the effectiveness, access, and quality of rehabilitation services.
Executive application of the proposed policy
For the successful implementation of the aforementioned policies, the following executive actions are recommended:
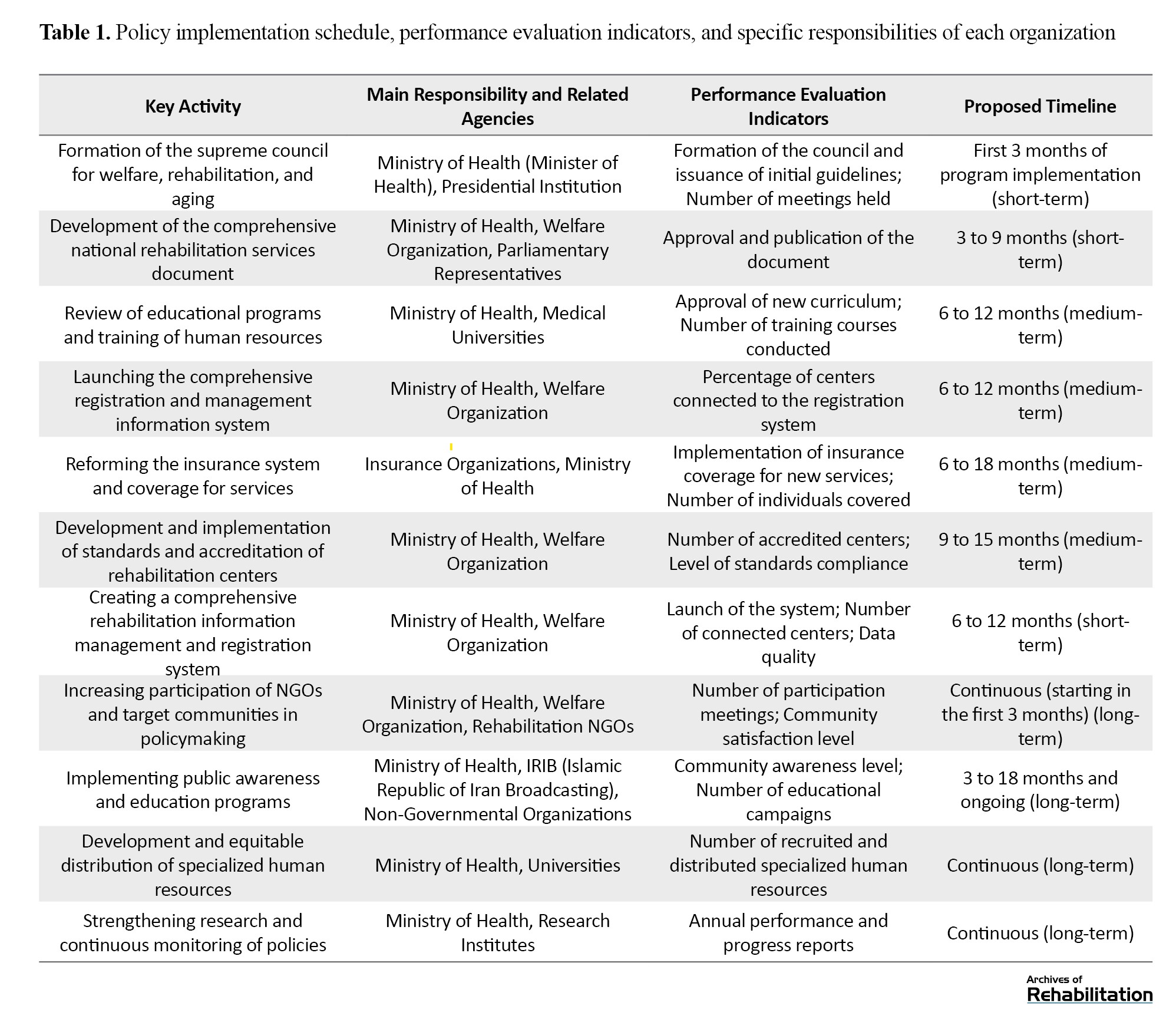
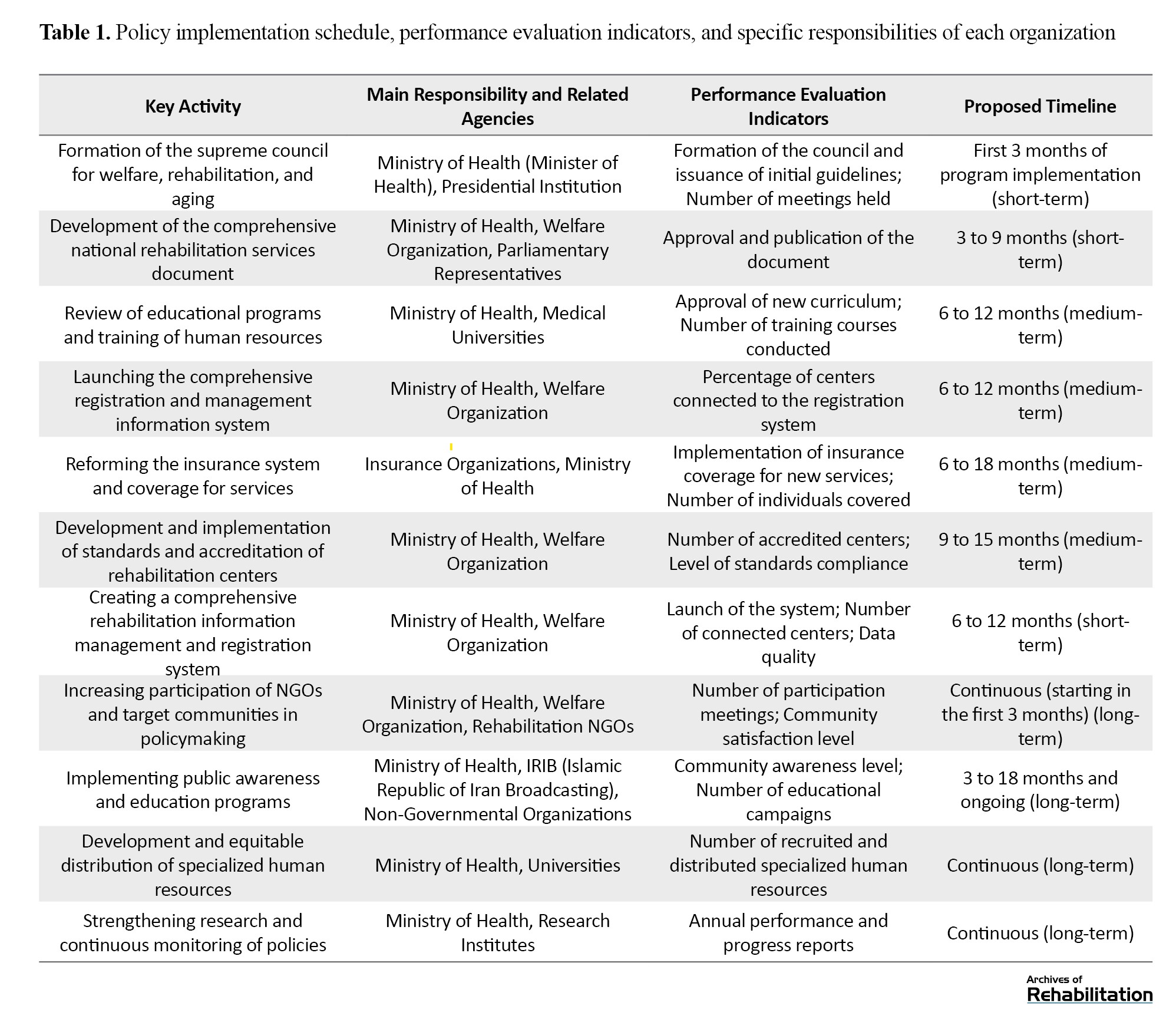
1) Formation and activation of the Supreme Council for Welfare, Rehabilitation, and Aging, with an agenda focused on developing a comprehensive document, inter-sectoral coordination, and continuous supervision of policy implementation; 2) planning and execution of revised educational programs in medical universities, emphasizing interdisciplinary rehabilitation skills and the training of specialized human resources; 3) reforming the payment and insurance system for rehabilitation services by defining specific service packages and ensuring timely payments to service-providing centers; 4) establishing transparent legal and supervisory mechanisms through the development of regulations, implementation of center accreditation, and formation of follow-up and accountability committees; 5) launching a comprehensive rehabilitation information registration system in collaboration with relevant agencies to register patient status, services, and rehabilitation centers; 6) providing government financial support and incentive policies to expand services in both public and non-public sectors, as well as to develop assistive and knowledge-based technologies; 7) enhancing stakeholder and community participation through the formation of specialized associations and widespread public education to promote a culture of support for individuals with disabilities; 8) the implementation of these actions requires the allocation of sufficient resources, the creation of cohesive management structures, and continuous supervision by responsible agencies. The proposed schedule for policy implementation, performance evaluation indicators, and specific responsibilities of each agency is given in Table 1.
Discussion
The implementation of policies to enhance the governance of rehabilitation services in Iran is accompanied by various considerations and challenges:
Organizational resistance and the need for inter-sectoral consensus
Different organizations with varying interests and perspectives can create challenges in establishing coordinated collaboration. Creating a space for dialogue and continuous interaction is vital.
Limitations in financial resources and human capital
Shortages in budget and specialized workforce are fundamental barriers that require medium- and long-term programs for enhancement and optimal resource allocation. Lack of efficient and transparent supervisory structures: Providing legal, supervisory, and reporting infrastructures that enable precise monitoring of governance performance is essential.
Need for public awareness and universal education
Changing public and professional attitudes toward the importance of rehabilitation and the rights of individuals with disabilities is one of the key prerequisites for the effectiveness of policies.
Technological challenges and access to assistive devices
Developing indigenous technologies and importing appropriate equipment, along with training on their use, should be prioritized.
Necessity for continuous monitoring and policy revision
Policies must be flexible and updated based on available data and experiences to achieve the desired effectiveness. Embracing the active role of all stakeholders and strengthening political commitment at various decision-making levels is the key to success in implementing these policies.
Conclusion
In the Islamic Republic of Iran, access to rehabilitation services is not fully provided for all those in need. This situation is primarily due to the lack of integrated and systematic management in delivering rehabilitation services, as well as limitations in human and financial resources. To enhance the coverage and quality of rehabilitation services, coordinated and multifaceted actions are necessary in three key areas:
Organizing the management of rehabilitation services
Establishing an integrated stewardship structure and defining national policies and standards in the areas of planning, equipment supply, and supervision of service delivery is essential to increase synergy among public, private, and non-governmental sectors, while reducing fragmentation and duplication of efforts.
Strengthening specialized human resources
Developing educational programs and capacity-building initiatives to train a larger number of rehabilitation specialists (including physiotherapists, occupational therapists, speech therapists, and other related professionals) and enhancing their clinical and managerial skills is imperative to meet the growing needs of society.
Expanding insurance coverage for rehabilitation services
Developing and deepening insurance coverage for these services will reduce the financial burden on families, increase access to effective treatments, and prevent interruptions in essential therapies.
In the absence of implementing these actions, significant negative consequences are likely, including depriving a large number of individuals in need from receiving vital rehabilitation services, increasing the burden of disease and disability in society, and consequently raising direct and indirect costs for the health system. Therefore, targeted planning and investment in management, human resources, and insurance structures for improving the rehabilitation services delivery system is a public health necessity.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1402.099).
Funding
Research budget from the University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Conceptualization: Mahnaz Afshari and Kianoush Abdi; Investigation, editing & review: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Policy recommendations
The Veillard et al. [17] framework for health system stewardship was used to identify and propose policy solutions. This framework outlines six stewardship functions in relation to the national context, values, and ultimate goals pursued by the health system. These six dimensions include:
1) Setting the health vision and strategy to achieve better health; 2) influencing all sectors for better health; 3) governing the health system in alignment with prevailing values; 4) ensuring the health system design aligns with health system goals; 5) enhancing current legal and regulatory tools; 6) collecting, disseminating, and utilizing information [17].
Enhancing the health vision and strategy for better access to rehabilitation services
In order to achieve the health vision and strategy for better rehabilitation services, actions must be taken in three dimensions: social, economic, and technological.
Social dimension
In the social dimension, the following solutions are proposed to improve rehabilitation stewardship:
1) Increasing political commitment and prioritizing rehabilitation services in health system policymaking by changing the perspectives and attitudes of policymakers, managers, and health service providers through holding educational programs to raise awareness about the importance of rehabilitation; 2) specialized training to integrate a culture of serving people with disabilities at different levels of producing public and individual goods and services; 3) adopting a holistic approach to providing rehabilitation services at both policymaking and service delivery levels; 4) education and awareness-raising at the family level for caring for patients with disabilities, and activating the role of society and organizations in combating discrimination against people with disabilities by utilizing mass media for information dissemination and improving societal attitudes; 5) engaging and utilizing people with disabilities and their representatives in rehabilitation policymaking to enhance responsiveness, efficiency, effectiveness, and sustainability of programs, and to strengthen decision-making and user satisfaction with services; 6) Strengthening and empowering non-governmental organizations (NGOs) run by people with disabilities with the support of the government sector.
Economic and technological dimension
In the economic and technological dimension, the following solutions can be guiding:
1) Utilizing support facilities and creating incentives for government and private sector organizations providing rehabilitation services; 2) investing in knowledge-based and domestic companies in the field of rehabilitation technology; 3) upgrading and improving technological infrastructure to facilitate the participation of people with disabilities in society.
Influencing other sectors and advocacy for strengthening rehabilitation services
Since rehabilitation services require intersectoral collaborations, the following solutions are proposed to strengthen these collaborations:
1) Advocacy to address rehabilitation services in the country’s general policies, vision document, and development plans, and strengthening advocacy from the Health Commission of Parliament regarding elevating the position of rehabilitation in the country’s health system; 2) using policy discourse to garner cooperation from all organizations involved in rehabilitation; 3) supporting private and civil society institutions in providing rehabilitation services; 4) increasing community participation in rehabilitation services through raising public awareness; 5) forming alliances among various rehabilitation associations, such as optometry, audiology, speech therapy, etc., through the establishment of a National Rehabilitation Network to increase the participation of rehabilitation specialists in the policymaking process.
Strengthening health system governance
Given the multisectoral nature of rehabilitation service provision, there is a need for integrated governance at the macro level, free from duplication. Therefore, the following solutions are proposed:
1) Creating integration, coordination, and collaboration in rehabilitation service stewardship through the establishment of a Supreme Council for Welfare, Rehabilitation, and Aging at the national level under the President and Cabinet as the legislative and central governance body that will develop a comprehensive rehabilitation services document. This document will guide all subordinate agencies, their roles, and their interactions with other agencies; 2) creating and developing an active role for Physical Medicine and Rehabilitation Departments in the Supreme Council for Welfare, Rehabilitation, and Aging to facilitate leadership and governance skills; 3) creating and developing an active role for representatives of government organizations involved in providing rehabilitation services and representatives of civil society organizations in the field of rehabilitation in the Supreme Council for Welfare, Rehabilitation, and Aging; 4) establishing and developing a Deputy for Rehabilitation and Social Health under the Minister of Health to strengthen the stewardship role of rehabilitation services in the Ministry of Health; 5) forming an Aging and Rehabilitation Commission in the Islamic Consultative Assembly (Parliament); 6) developing strategic and operational programs for various levels of rehabilitation service provision to clarify the roles of different actors; 7) increasing and expanding the capacities of the Welfare Organization as the executive arm for rehabilitation services and support services.
Strengthening the health system in line with rehabilitation service stewardship
Since the health system plays a special role in the stewardship of rehabilitation services, the following solutions are proposed to strengthen the health system:
1) Gradually shifting the Ministry of Health’s approach from a treatment-oriented perspective to a preventive one, to understand the importance of rehabilitation services by incorporating rehabilitation outcome indicators into the performance evaluation system of hospitals and health centers; 2) determining the position of rehabilitation services at all first, second, and third levels in the country’s comprehensive rehabilitation document and integrating rehabilitation services into the primary health care system and strengthening the referral system to expand inclusive rehabilitation services; 3) paying attention to the importance of assistive technologies in rehabilitation and improving access to modern assistive equipment for individuals with disabilities; 4) specifying hierarchies and accountability levels in rehabilitation services and delegating authority commensurate with the assigned duties to each accountable entity; 5) developing and implementing policies for sustainable financing and efficient insurance coverage for rehabilitation services (with emphasis on horizontal and vertical equity); 6) developing and implementing policies to increase capacity and equitable distribution of rehabilitation specialists and to develop knowledge and skills of human resources active in rehabilitation management; 7) expanding comprehensive rehabilitation centers for individuals with disabilities in collaboration with the non-governmental sector; 8) revising the curricula of various medical sciences disciplines to familiarize them with rehabilitation services and enhance their ability to collaborate in interdisciplinary teams.
Strengthening legal and regulatory tools for rehabilitation services
One of the most important dimensions of improving the stewardship of rehabilitation services is strengthening the legal and regulatory tools for rehabilitation services. The following strategies can enhance the legal and regulatory capacity of rehabilitation services:
1) Implementation of the National Rehabilitation Services Document, standards, protocols, and clinical guidelines in various domains of rehabilitation services to guide service providers in ensuring the integrity, safety, and quality of the services provided; 2) supporting adopted policies in the field of rehabilitation services through the development of comprehensive regulatory laws and regulations that ensure the implementation of these policies and provide a basis for monitoring and supervising their execution; 3) determining the structure for supervision, monitoring, and control of rehabilitation services under the Comprehensive Rehabilitation Services Document, including levels of supervision, monitoring, and control for rehabilitation services, and establishing mechanisms for the full and proper implementation of the Comprehensive Law on People with Disabilities; 4) determining the structure for supervision, monitoring, control, and accountability levels for rehabilitation services under the Comprehensive Rehabilitation Services Document, along with delegating appropriate levels of authority corresponding to the tasks assigned to each accountable entity in the document; 5) establishing an accreditation mechanism for rehabilitation centers by the Ministry of Health, including the development of key performance indicators, care standards, and accreditation criteria for these centers.
Strengthening methods of collecting, disseminating, and utilizing information on rehabilitation services
Improving the governance of rehabilitation services requires proper policy-making and planning, taking into account the current situation and anticipating future needs. In this regard, the following strategies are proposed:
1) Creating and developing the infrastructure for a comprehensive rehabilitation services information management system, including designating the responsible entity in this area, registering individuals with disabilities and impairments, registering rehabilitation services, registering human resources and specialists in the rehabilitation field, registering information on rehabilitation centers, and integrating it into the current electronic health record; 2) integrating national rehabilitation information through the sharing of data among various agencies; 3) appropriately and efficiently allocating resources following precise needs assessment and data-driven planning; 4) strengthening investment in rehabilitation research to leverage scientific evidence in rehabilitation policy-making and to enhance policymakers’ understanding and awareness for prioritizing the needs of individuals with disabilities.
Policy recommendation (top proposed policy)
The top policy recommendation in this study is shaped based on the six-dimensional governance framework of the health system by Willard and colleagues. A comprehensive and coordinated approach that encompasses all relevant sectors and actors:
Creating an integrated and centralized governance structure
Establishing the Supreme Council for Welfare, Rehabilitation, and Aging, chaired by the President, as the supervisory and legislative body; Developing a comprehensive national rehabilitation services document with precise task descriptions for agencies and coordination among them.
Strengthening specialized human resources and continuous education
Reviewing educational programs in medical and rehabilitation disciplines, developing interdisciplinary training, and ensuring equitable distribution of rehabilitation specialists.
Sustainable financing through efficient insurance mechanisms
Reforming the insurance system to provide comprehensive coverage for rehabilitation services, accompanied by incentive policies for both public and private sectors.
Strengthening legal and regulatory tools
Approving and implementing comprehensive laws supporting individuals with disabilities, developing standards and protocols for rehabilitation services, and establishing an accreditation system for rehabilitation centers.
Developing an information system and data-based research
Creating a comprehensive registration and management system for rehabilitation information, integrating data, and facilitating access to scientific evidence for intelligent policymaking.
Increasing community participation and non-governmental organizations
Empowering and enhancing the role of NGOs, along with active involvement of individuals with disabilities in the decision-making process, to ensure accountability and effectiveness of policies.
This proposed policy, with an emphasis on centralization and transparency in the roles of actors, can pave the way for improving the effectiveness, access, and quality of rehabilitation services.
Executive application of the proposed policy
For the successful implementation of the aforementioned policies, the following executive actions are recommended:
1) Formation and activation of the Supreme Council for Welfare, Rehabilitation, and Aging, with an agenda focused on developing a comprehensive document, inter-sectoral coordination, and continuous supervision of policy implementation; 2) planning and execution of revised educational programs in medical universities, emphasizing interdisciplinary rehabilitation skills and the training of specialized human resources; 3) reforming the payment and insurance system for rehabilitation services by defining specific service packages and ensuring timely payments to service-providing centers; 4) establishing transparent legal and supervisory mechanisms through the development of regulations, implementation of center accreditation, and formation of follow-up and accountability committees; 5) launching a comprehensive rehabilitation information registration system in collaboration with relevant agencies to register patient status, services, and rehabilitation centers; 6) providing government financial support and incentive policies to expand services in both public and non-public sectors, as well as to develop assistive and knowledge-based technologies; 7) enhancing stakeholder and community participation through the formation of specialized associations and widespread public education to promote a culture of support for individuals with disabilities; 8) the implementation of these actions requires the allocation of sufficient resources, the creation of cohesive management structures, and continuous supervision by responsible agencies. The proposed schedule for policy implementation, performance evaluation indicators, and specific responsibilities of each agency is given in Table 1.
Discussion
The implementation of policies to enhance the governance of rehabilitation services in Iran is accompanied by various considerations and challenges:
Organizational resistance and the need for inter-sectoral consensus
Different organizations with varying interests and perspectives can create challenges in establishing coordinated collaboration. Creating a space for dialogue and continuous interaction is vital.
Limitations in financial resources and human capital
Shortages in budget and specialized workforce are fundamental barriers that require medium- and long-term programs for enhancement and optimal resource allocation. Lack of efficient and transparent supervisory structures: Providing legal, supervisory, and reporting infrastructures that enable precise monitoring of governance performance is essential.
Need for public awareness and universal education
Changing public and professional attitudes toward the importance of rehabilitation and the rights of individuals with disabilities is one of the key prerequisites for the effectiveness of policies.
Technological challenges and access to assistive devices
Developing indigenous technologies and importing appropriate equipment, along with training on their use, should be prioritized.
Necessity for continuous monitoring and policy revision
Policies must be flexible and updated based on available data and experiences to achieve the desired effectiveness. Embracing the active role of all stakeholders and strengthening political commitment at various decision-making levels is the key to success in implementing these policies.
Conclusion
In the Islamic Republic of Iran, access to rehabilitation services is not fully provided for all those in need. This situation is primarily due to the lack of integrated and systematic management in delivering rehabilitation services, as well as limitations in human and financial resources. To enhance the coverage and quality of rehabilitation services, coordinated and multifaceted actions are necessary in three key areas:
Organizing the management of rehabilitation services
Establishing an integrated stewardship structure and defining national policies and standards in the areas of planning, equipment supply, and supervision of service delivery is essential to increase synergy among public, private, and non-governmental sectors, while reducing fragmentation and duplication of efforts.
Strengthening specialized human resources
Developing educational programs and capacity-building initiatives to train a larger number of rehabilitation specialists (including physiotherapists, occupational therapists, speech therapists, and other related professionals) and enhancing their clinical and managerial skills is imperative to meet the growing needs of society.
Expanding insurance coverage for rehabilitation services
Developing and deepening insurance coverage for these services will reduce the financial burden on families, increase access to effective treatments, and prevent interruptions in essential therapies.
In the absence of implementing these actions, significant negative consequences are likely, including depriving a large number of individuals in need from receiving vital rehabilitation services, increasing the burden of disease and disability in society, and consequently raising direct and indirect costs for the health system. Therefore, targeted planning and investment in management, human resources, and insurance structures for improving the rehabilitation services delivery system is a public health necessity.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1402.099).
Funding
Research budget from the University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Conceptualization: Mahnaz Afshari and Kianoush Abdi; Investigation, editing & review: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- World Health Organization (WHO). Rehabilitation [Internet]. 2024 [Updated 2024 April 22]. Available from: [Link]
- Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: A systematic analysis for the global burden of disease study 2019. Lancet. 2021; 396(10267):2006-2017. [DOI:10.1016/S0140-6736(20)32340-0] [PMID]
- World Health Organization (WHO). Global report on health equity for persons with disabilities [Internet]. 2022 [Updated 2025 December 15]. Available From: [Link]
- Najafi Z, Abdi K, Khanjani MS, Dalvand H, Amiri M. Convention on the rights of persons with disabilities: Qualitative exploration of barriers to the implementation of articles 25 (health) and 26 (rehabilitation) in Iran. Medical Journal of the Islamic Republic of Iran. 2021; 35:10. [DOI:10.47176/mjiri.35.10] [PMID]
- Iravani M, Riahi L, Abdi K, Tabibi SJ. A comparative study of the rehabilitation services systems for people with disabilities. Archives of Rehabilitation. 2021; 21(4):544-63. [DOI:10.32598/RJ.21.4.3225.1]
- Abdi K, Arab M, Khankeh H, Kamali M, Rashidian A, Farahani F, et al. Challenges in providing rehabilitation services for people with disabilities in Iran: A qualitative study. British Journal of Medicine and Medical Research. 2016; 13(4):1. [Link]
- Najafi Z, Abdi K, Soltani S. Stewardship; the missing loop of rehabilitation in the health system: A policy brief. Medical Journal of the Islamic Republic of Iran. 2023; 37:66. [DOI:10.47176/mjiri.37.66] [PMID]
- Khamenei. ir. Communicating general “health” policies (Persian) [Internet]. 2019 [Updated 2026 January 2]. Available from: [Link]
- World Health Organization (WHO). Rehabilitation in health systems: Guide for action. Geneva: World Health Organization; 2019. [Link]
- Abdi K, Najafi Z, Foroughi Z, Afshari M. Health policy analysis for stewardship of rehabilitation services. BMC Health Services Research. 2024; 24(1):1301. [DOI:10.1186/s12913-024-11746-x] [PMID]
- Najafi1 Z, Najafi E, Yarandi RB, Soltani S, Basakha M, Abdi K. [Socioeconomic inequalities in healthcare and rehabilitation expenditure: An analysis of costs for people with disabilities in Iran (Persian)]. Middle East Journal of Rehabilitation and Health Studies. 2025; 12(2):e157878. [DOI:10.5812/mejrh-157878]
- Soltani S, Takian A, Akbari Sari A, Kamali M, Majdzadeh R, Karami Matin B. Disregarded health problems of people with disabilities: A qualitative study of policymakers’ perspective. Archives of Rehabilitation. 2019; 20(2):136-49. [DOI:10.32598/rj.20.2.136]
- Farahbod M, Masoudi Asl I, Tabibi S J, Kamali M. Comparing the rehabilitation structures in the health systems of Iran, Germany, Japan, Canada, Turkey, and South Africa. Archives of Rehabilitation. 2023; 24(1):96-113 [DOI:10.32598/RJ.24.1.3582.1]
- Afshari M, Najafi Z, Foroughi Z, Abdi K. Stewardship of rehabilitation services in Iran: A qualitative study exploring current challenges and solutions. Disability and Rehabilitation. 2025; 47(25):6632-44. [DOI:10.1080/09638288.2025.2519505] [PMID]
- Abdi K, Foroughi Z, Najafi Z, Afshari M. Challenges and solutions to effective stewardship of rehabilitation services: A scoping review. BMC Health Services Research. 2025; 25(1):1211. [DOI:10.1186/s12913-025-13366-5] [PMID]
- Turoff M. The design of a policy Delphi. Technological Forecasting and Social Change. 1970; 2(2):149-71. [DOI:10.1016/0040-1625(70)90161-7]
- Veillard JHM, Brown AD, Barış E, Permanand G, Klazinga NS. Health system stewardship of National Health Ministries in the WHO European region: Concepts, functions and assessment framework. Health Policy. 2011; 103(2-3):191-9. [DOI:10.1016/j.healthpol.2011.09.002] [PMID]
Type of Study: Policy brief |
Subject:
Rehabilitation Management
Received: 3/08/2025 | Accepted: 15/11/2025 | Published: 1/01/2026
Received: 3/08/2025 | Accepted: 15/11/2025 | Published: 1/01/2026
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |