Volume 26, Issue 3 (Autumn 2025)
jrehab 2025, 26(3): 446-463 |
Back to browse issues page
Ethics code: IR.SBU.RETECH.REC.1402.859
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khademi Kalantari S. The Impact of Architectural Elements In Occupational Therapy Centers On The Sensory Profile of Children With Attention Deficit Hyperactivity Disorder. jrehab 2025; 26 (3) :446-463
URL: http://rehabilitationj.uswr.ac.ir/article-1-3639-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3639-en.html
Department of Architecture, Faculty of Architecture and Urban Planning, Shahid Beheshti University, Tehran, Iran. , sasankhademic2w@gmail.com
Keywords: Health architecture, Sensory integration, Attention deficit hyperactivity disorder (ADHD), Occupational therapy
Full-Text [PDF 1854 kb]
(231 Downloads)
| Abstract (HTML) (1048 Views)
References
Full-Text: (318 Views)
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders. ADHD typically begins in childhood and may persist into adulthood. Individuals with ADHD often experience difficulties with concentration, behavioral control, and regulation of motor activities, which manifest as inattention, hyperactivity, or impulsivity. Inattention refers to difficulty in maintaining focus on tasks, concentrating, and staying organized. Hyperactivity refers to a state of restlessness and excessive activity. Impulsivity refers to sudden, unplanned actions, which can result in social and academic problems. Genetic and environmental factors have a role in the etiology of ADHD. This disorder can significantly affect a child’s academic performance, social interactions, and daily life functioning [1]. Numerous studies have shown that many children with ADHD also experience sensory integration difficulties. Inability to appropriately process and respond to sensory stimuli may exacerbate behavioral problems and reduce the effectiveness of therapeutic interventions and educational outcomes [2]. Various treatment approaches have been used for children with ADHD, including medication therapy, behavioral therapy, and occupational therapy based on sensory integration and sensory processing assessments [3]. Sensory-based occupational therapy approaches focus on enhancing the brain’s ability to process and organize sensory information, thereby improving the child’s interaction with their environment [4]. However, the physical and spatial characteristics of the treatment environment can affect the success of such therapeutic interventions [5]. Several assessment tools have been developed to evaluate the severity of ADHD and the effectiveness of therapeutic programs in children with ADHD. One standardized tool for assessing sensory integration is the short sensory profile (SSP) developed by Winnie Dunn in 1999 [6]. This tool is widely used to assess sensory processing patterns in children aged 3-14 years. The Persian version of the SSP was translated and validated by Shahbazi et al. [7]. Multiple studies have shown that children with ADHD have lower SSP scores compared to their typically developing peers [8].
Health architecture, as an emerging discipline in designing therapeutic environments, plays a vital role in improving patient experience, especially for individuals with sensory processing disorders such as autism and ADHD [9]. Designing therapeutic environments that consider the sensory needs of patients can reduce anxiety, enhance concentration, and improve quality of life [10]. Studies have shown that the use of natural light, soft color palettes, and natural materials, such as wood and stone, can reduce sensory overstimulation and help create a relaxing environment [11]. Acoustic control by using sound-absorbing materials and proper spatial design can also reduce stress and enhance comfort. Flexible and adaptable environments, such as Snoezelen sensory rooms, enable customization of sensory input based on individual needs [12]. These rooms, offering adjustable lighting, calming sounds, and diverse tactile surfaces, help patients gain a greater sense of control over their surroundings and achieve better emotional regulation. Additionally, designing clear and predictable routes can help reduce anxiety and enhance patients’ safety. The use of visual cues and guide colors in these routes can improve way-finding and reduce confusion [13]. Ultimately, health architecture, focusing on the sensory needs of patients, can lead to the creation of inclusive and supportive environments, benefiting not only individuals with sensory processing disorders but also all users of therapeutic environments [6, 7]. The impact of the environment on children’s sensory processing has also been investigated in outdoor spaces [14]. In a 2024 study by Finnigan [15], individuals with conditions such as autism, ADHD, and dyslexia were surveyed. Their results demonstrated that specific characteristics of built environments can function as either barriers or facilitators for these individuals. For instance, minor changes in open-space design such as material selection, light quality, sound levels, spatial layout, and access to nature, can significantly influence sensory experience and behavioral functioning in ADHD children. The study introduced a theoretical model called the sensory responsive environments framework (SREF), which emphasizes the importance of designing multisensory environments responsive to the sensory needs of neurodivergent individuals. The framework provides guidance for architects, urban designers, and educators on creating more inclusive and supportive environments.
Despite growing awareness of the unique needs of children with ADHD, suffering from sensory processing and emotional regulation challenges, there are still no well-defined, codified, and comprehensive standards for designing therapeutic environments tailored to their sensory, behavioral, and cognitive profiles, especially in Iran [16]. This gap has led to many rehabilitation centers in the country lacking purposefully designed spaces that can effectively support attention, concentration, emotional regulation, and stress reduction in these children. In contrast, interdisciplinary research and empirical evidence in developed countries have led to the adoption of principles such as low-stimulation design, use of calming and neutral colors, precise noise control, natural and adjustable lighting, and attention to environmental spatial factors [17]. These principles have become standard practice in therapeutic settings for children with special needs. In Iran, such considerations are still applied sporadically and unsystematically. Most designs are based on general and non-specialized standards and fail to adequately address the complex and diverse sensory processing needs of children with ADHD. Additionally, there are no formal guidelines for designing specialized therapeutic environments for this population, nor is there effective interdisciplinary collaboration among architects, occupational therapists, child psychologists, and other relevant professionals. Furthermore, there is limited research to establish a scientific framework for design. These scientific and practical limitations not only compromise the quality of therapeutic environments but may also directly impact the effectiveness of treatment and the psychological well-being of children [18]. Therefore, conducting interdisciplinary research, developing localized and applicable design guidelines, and implementing targeted programs in the field of therapeutic environment design for children with ADHD in Iran is a critical.
This study was conducted as the continuation of prior research that identified and analyzed architectural factors influencing the design of rehabilitation environments for children with ADHD and autism in Iran [19]. In the present study, we aim to empirically assess the impact of architectural modifications in 12 occupational therapy centers located in Tehran and Karaj cities on the sensory profile of children with ADHD.
Materials and Methods
Study design and participants
This is a quasi-experimental study conducted in two separate phases. Phase 1 included a comparison between rehabilitation environments with optimal and suboptimal architectural features regarding the impact of their architectural design on sensory processing performance in children with ADHD. In phase 2, the centers identified as suboptimal in phase 1 underwent architectural modifications, and the degree of change and improvement in the children’s sensory performance was assessed and compared with their progress during phase I. Participants were 64 children diagnosed with ADHD, including 20 girls and 44 boys (mean age=8.5±2.2 years), who had been enrolled in occupational therapy centers for less than one week and had no prior therapeutic history, and were selected using a convenience sampling method from 12 occupational therapy clinics located in Tehran and Karaj in 2024. To determine the sample size, a significance level of α=0.05, a test power of 80% and a medium effect size (Cohen’s d=0.5) were considered. The required sample size for comparing group means was calculated to be 50. Considering potential dropout, it increased to 64. These participants were recruited. Inclusion criteria for participation were age 5-10 years, Diagnosis of moderate ADHD based on the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) criteria by a psychiatrist or pediatric neurologist, no comorbid severe disorders (e.g. autism spectrum disorder or intellectual disability), regular attendance in occupational therapy sessions (2 sessions per week) and written informed consent of the parents. The children were divided into two groups based on the type of treatment center, including optimal centers (n=25) and suboptimal centers (n=39).
Occupational therapy
All participants received a sensory-based occupational therapy program tailored to their individual sensory processing profiles. The intervention included play-based activities, stimulation of various sensory systems (vestibular, proprioceptive, tactile, and visual), and modulated sensory exercises designed to enhance responsiveness to environmental stimuli. The intervention lasted six weeks, consisting of twelve 45-minute sessions.
Instruments
For center classification, a checklist was used, derived from a detailed questionnaire containing 30 items and six architectural domains [19, 20]. The face and content validity of this questionnaire had been confirmed, with a Cronbach’s α coefficient of 0.81. Each rehabilitation center was evaluated based on six architectural criteria: Lighting, acoustics, color scheme, spatial access/layout, ventilation, and spatial organization/safety. Centers were rated using a five-point Likert scale. Centers scoring above the average total score (65 out of 90) were classified as “optimal” (7 centers), while those with lower scores were considered “suboptimal” (5 centers).
Sensory processing performance was assessed using the Persian version of the SSP [6]. It consists of 7 domains and 38 items, assessing various sensory patterns, including sensory seeking, sensory avoidance, sensory sensitivity, and low registration. Scoring is based on a five-point Likert scale (always, frequently, occasionally, seldom, never), with scores ranging from 38 to 190. Lower scores indicate greater difficulties with sensory processing. According to normative data from typically developing children, SSP scores are classified as follows: >155 (typical performance), 142–154 (probable difference), and <141 (definite difference) [8]. The Persian version of the SSP has already been translated and validated by Shahbazi et al., who demonstrated its satisfactory reliability and validity [7]. The questionnaire was completed by the parents of children before the intervention and after the end of therapy sessions.
Architectural modifications of suboptimal centers
Targeted architectural changes were implemented in the five centers previously identified as suboptimal in terms of architectural features influencing therapeutic outcomes for children with ADHD. After these modifications, therapy programs continued, and the impact of these changes on sensory processing performance was evaluated. The modifications included: Controlling natural light with curtains to reduce direct light intensity, improving acoustic insulation to reduce background noise and prevent sudden auditory stimuli, the use of cool and muted color schemes on walls, flooring, and furniture (via covers), and designing separate activity zones with varying levels of sensory stimulation.
Statistical analysis
Data analysis was performed in SPSS software, version 26. The independent t-test was used to compare groups in phase 1, and a paired t-test was used to compare pre- and post-intervention differences in phase 2. The significance level was set at 0.05 for all analyses.
Results
Within-group comparison of SSP scores
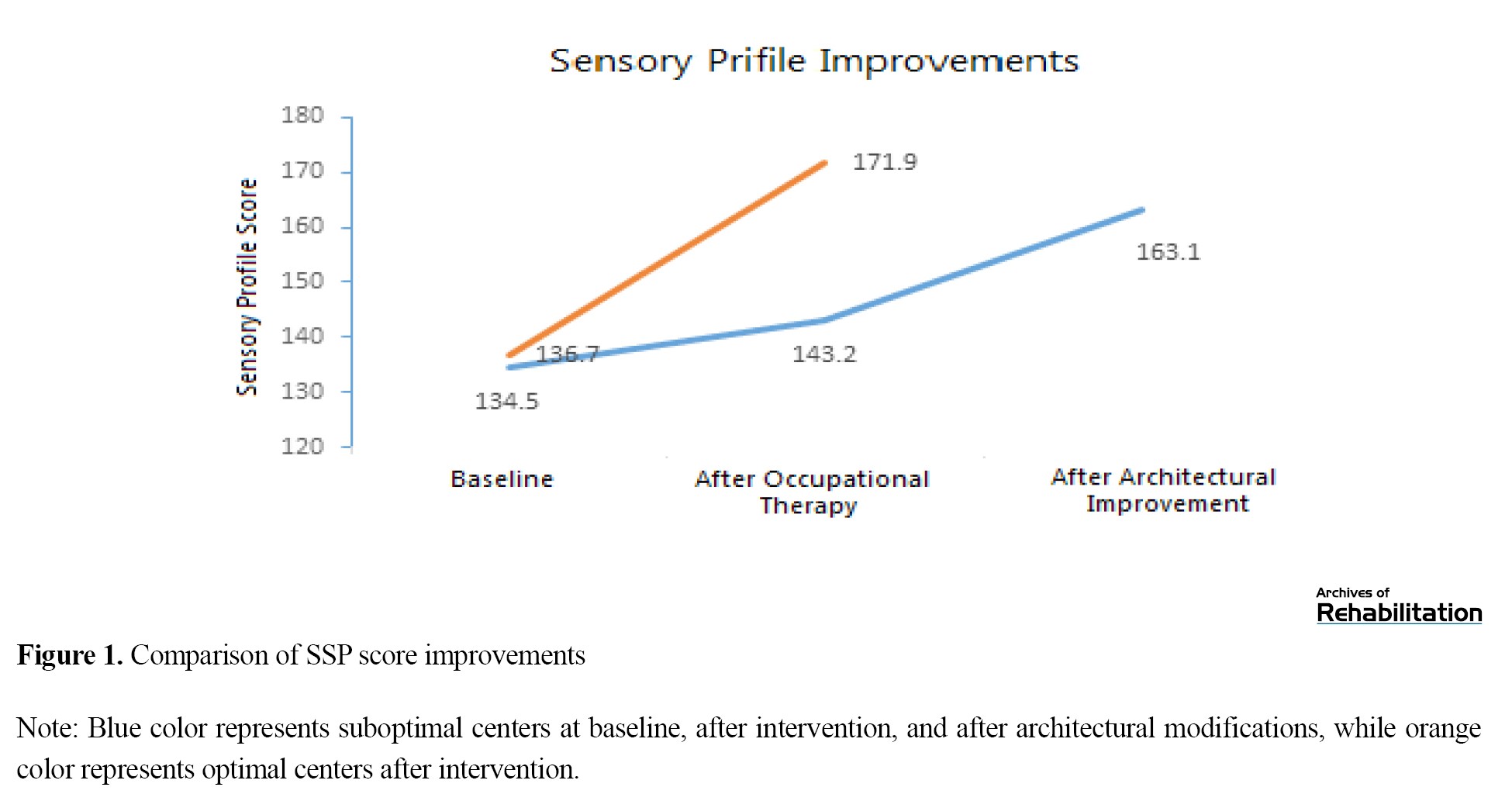
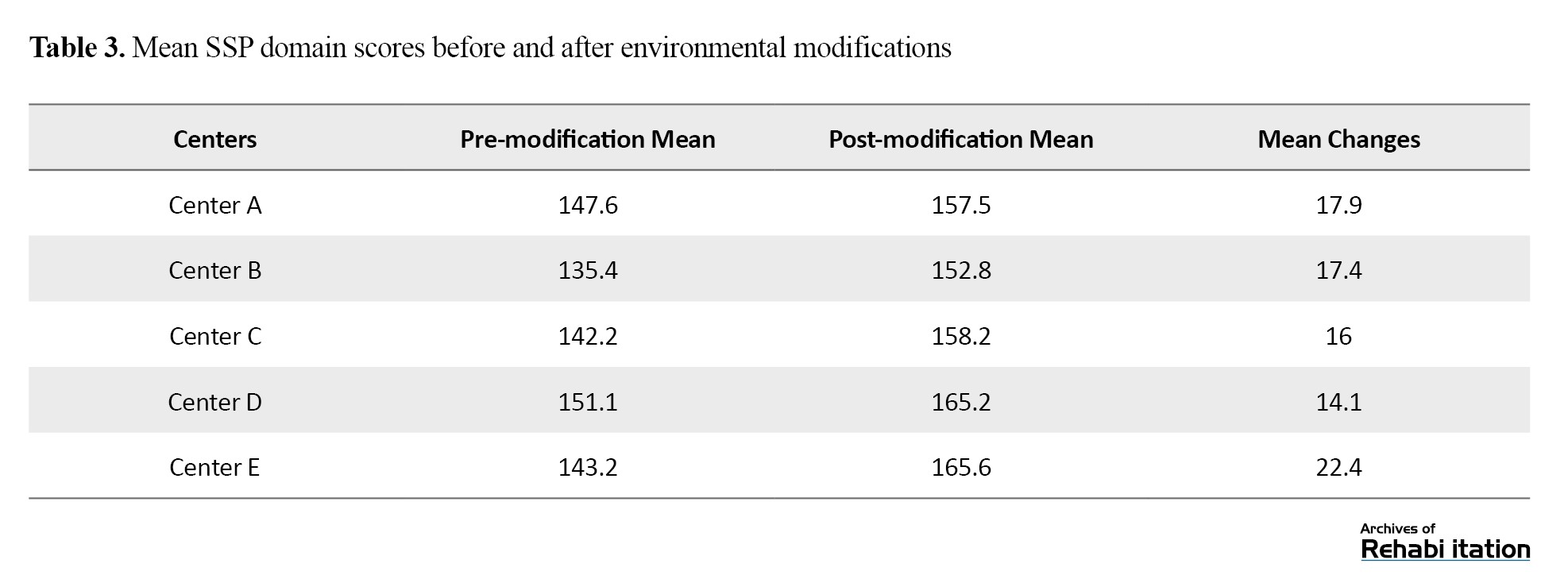
In phase 1, the mean SSP scores were compared within two groups. The pre-test–post-test comparison revealed that children attending centers with optimal architectural features exhibited significantly higher SSP domain scores (Table 1).
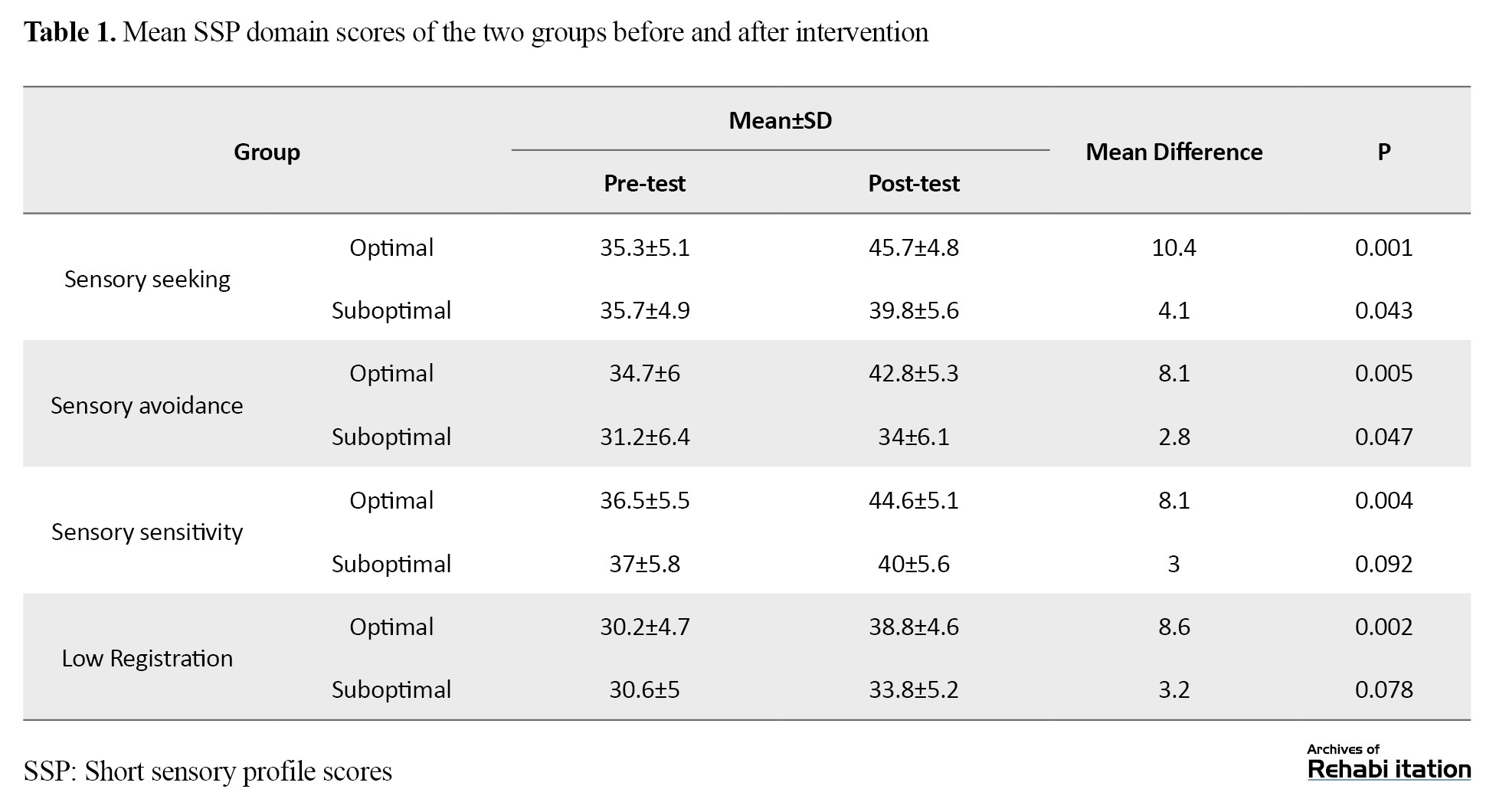
In both groups, the total SSP score increased significantly after intervention, indicating improvement in sensory processing performance. However, in the suboptimal group, this increase was less pronounced and borderline significant (P=0.048). The improvement in the optimal group was statistically more significant (P<0.001).
Between-group comparison of SSP scores
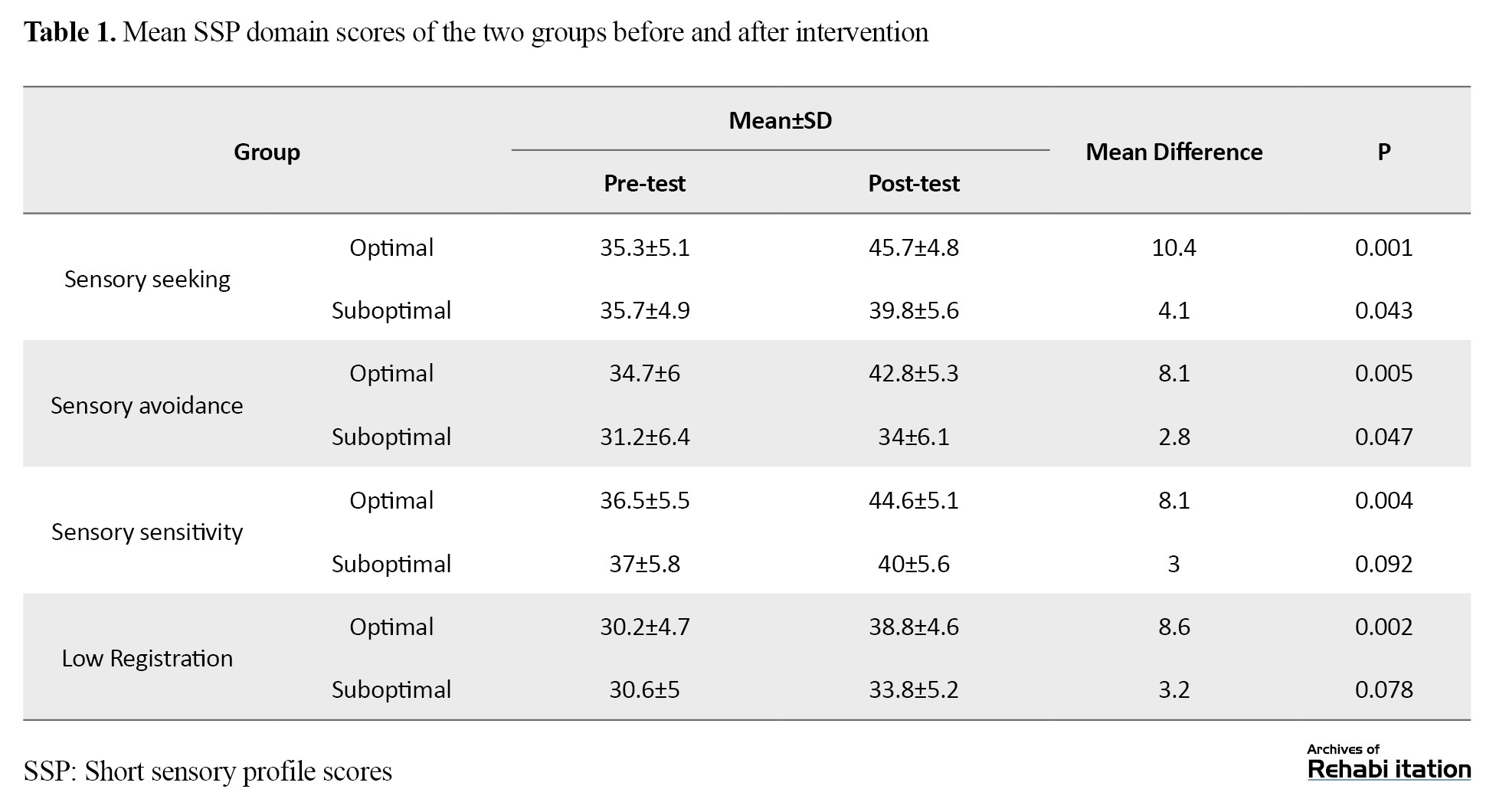
The optimal centers group showed significantly greater improvement across all SSP subscales compared to the suboptimal centers group (Table 2).
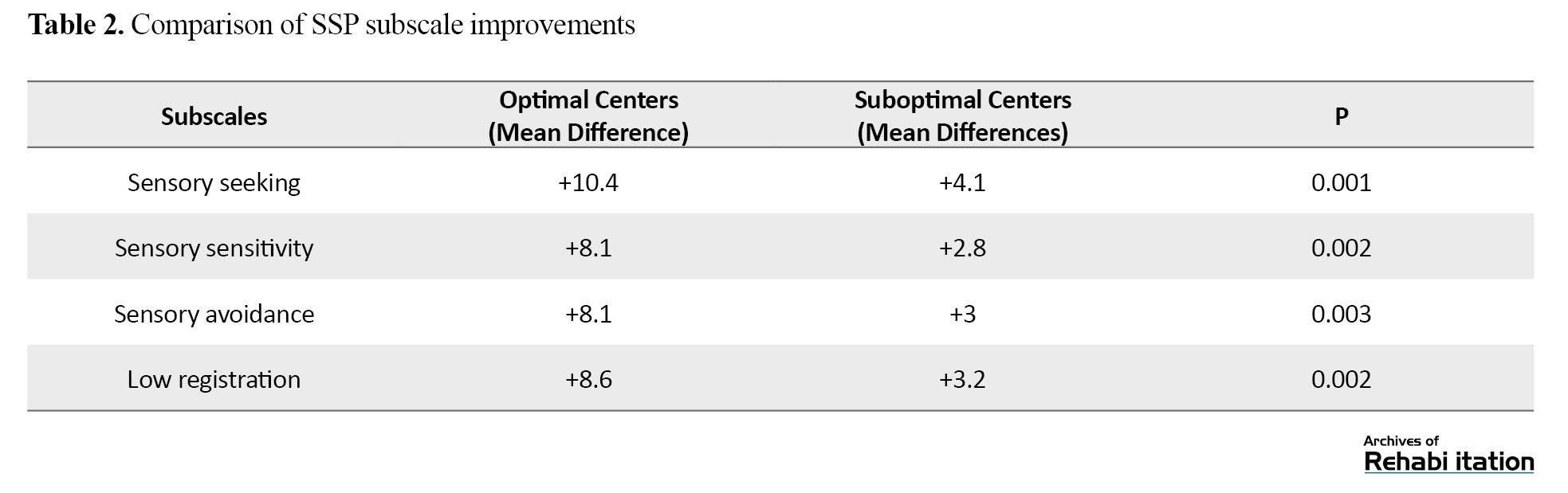
In both groups, the sensory seeking subscale demonstrated the highest significant improvement, while other indices showed relatively similar improvement.
Impact of architectural modifications in suboptimal centers
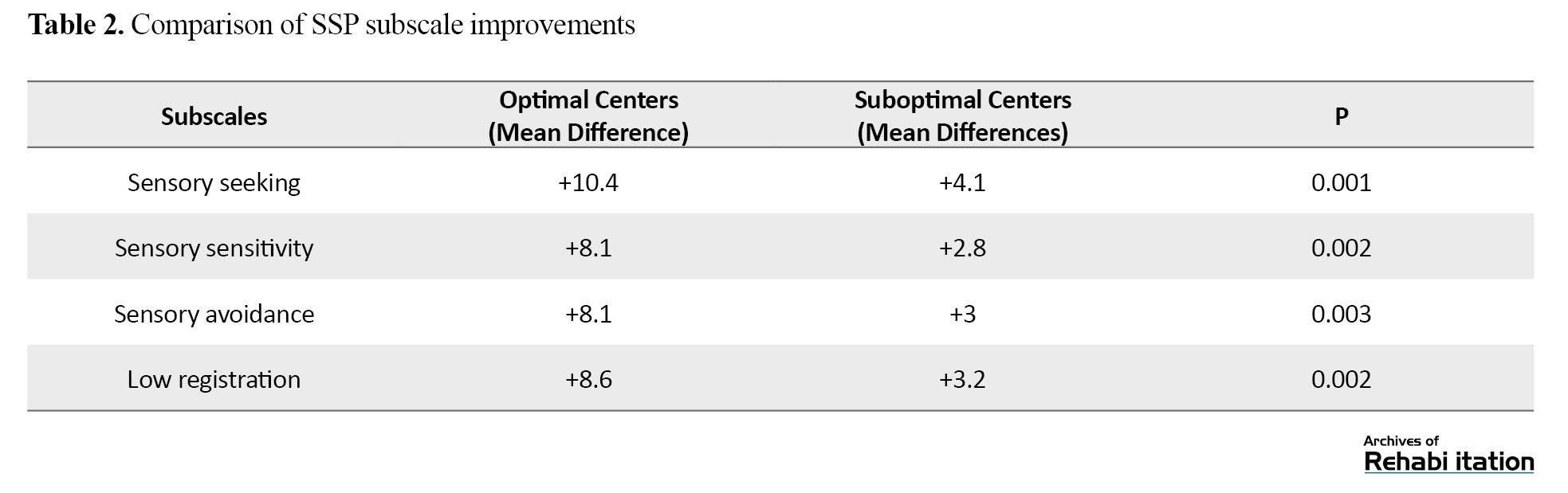
In phase 2, architectural improvements were implemented in five suboptimal centers. Children who had participated in Phase 1 continued to receive a new 12-session occupational therapy program within the same centers after modifications. The change in SSP scores was reassessed and compared to the pre-modification scores seen in phase 1. Although the mean total SSP score improved following architectural modifications, the magnitude of change was not significantly different compared to the phase I results (P=0.06), indicating a positive trend but a non-significant size (Table 3).
However, a significant difference was observed when comparing the improvement in modified centers to that of optimal centers (P=0.01).
The difference in the slope of improvement curves in Figure 1 for optimal and suboptimal centers (before modifications) highlights the critical role of architectural features in supporting sensory processing improvement in children with ADHD.
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders. ADHD typically begins in childhood and may persist into adulthood. Individuals with ADHD often experience difficulties with concentration, behavioral control, and regulation of motor activities, which manifest as inattention, hyperactivity, or impulsivity. Inattention refers to difficulty in maintaining focus on tasks, concentrating, and staying organized. Hyperactivity refers to a state of restlessness and excessive activity. Impulsivity refers to sudden, unplanned actions, which can result in social and academic problems. Genetic and environmental factors have a role in the etiology of ADHD. This disorder can significantly affect a child’s academic performance, social interactions, and daily life functioning [1]. Numerous studies have shown that many children with ADHD also experience sensory integration difficulties. Inability to appropriately process and respond to sensory stimuli may exacerbate behavioral problems and reduce the effectiveness of therapeutic interventions and educational outcomes [2]. Various treatment approaches have been used for children with ADHD, including medication therapy, behavioral therapy, and occupational therapy based on sensory integration and sensory processing assessments [3]. Sensory-based occupational therapy approaches focus on enhancing the brain’s ability to process and organize sensory information, thereby improving the child’s interaction with their environment [4]. However, the physical and spatial characteristics of the treatment environment can affect the success of such therapeutic interventions [5]. Several assessment tools have been developed to evaluate the severity of ADHD and the effectiveness of therapeutic programs in children with ADHD. One standardized tool for assessing sensory integration is the short sensory profile (SSP) developed by Winnie Dunn in 1999 [6]. This tool is widely used to assess sensory processing patterns in children aged 3-14 years. The Persian version of the SSP was translated and validated by Shahbazi et al. [7]. Multiple studies have shown that children with ADHD have lower SSP scores compared to their typically developing peers [8].
Health architecture, as an emerging discipline in designing therapeutic environments, plays a vital role in improving patient experience, especially for individuals with sensory processing disorders such as autism and ADHD [9]. Designing therapeutic environments that consider the sensory needs of patients can reduce anxiety, enhance concentration, and improve quality of life [10]. Studies have shown that the use of natural light, soft color palettes, and natural materials, such as wood and stone, can reduce sensory overstimulation and help create a relaxing environment [11]. Acoustic control by using sound-absorbing materials and proper spatial design can also reduce stress and enhance comfort. Flexible and adaptable environments, such as Snoezelen sensory rooms, enable customization of sensory input based on individual needs [12]. These rooms, offering adjustable lighting, calming sounds, and diverse tactile surfaces, help patients gain a greater sense of control over their surroundings and achieve better emotional regulation. Additionally, designing clear and predictable routes can help reduce anxiety and enhance patients’ safety. The use of visual cues and guide colors in these routes can improve way-finding and reduce confusion [13]. Ultimately, health architecture, focusing on the sensory needs of patients, can lead to the creation of inclusive and supportive environments, benefiting not only individuals with sensory processing disorders but also all users of therapeutic environments [6, 7]. The impact of the environment on children’s sensory processing has also been investigated in outdoor spaces [14]. In a 2024 study by Finnigan [15], individuals with conditions such as autism, ADHD, and dyslexia were surveyed. Their results demonstrated that specific characteristics of built environments can function as either barriers or facilitators for these individuals. For instance, minor changes in open-space design such as material selection, light quality, sound levels, spatial layout, and access to nature, can significantly influence sensory experience and behavioral functioning in ADHD children. The study introduced a theoretical model called the sensory responsive environments framework (SREF), which emphasizes the importance of designing multisensory environments responsive to the sensory needs of neurodivergent individuals. The framework provides guidance for architects, urban designers, and educators on creating more inclusive and supportive environments.
Despite growing awareness of the unique needs of children with ADHD, suffering from sensory processing and emotional regulation challenges, there are still no well-defined, codified, and comprehensive standards for designing therapeutic environments tailored to their sensory, behavioral, and cognitive profiles, especially in Iran [16]. This gap has led to many rehabilitation centers in the country lacking purposefully designed spaces that can effectively support attention, concentration, emotional regulation, and stress reduction in these children. In contrast, interdisciplinary research and empirical evidence in developed countries have led to the adoption of principles such as low-stimulation design, use of calming and neutral colors, precise noise control, natural and adjustable lighting, and attention to environmental spatial factors [17]. These principles have become standard practice in therapeutic settings for children with special needs. In Iran, such considerations are still applied sporadically and unsystematically. Most designs are based on general and non-specialized standards and fail to adequately address the complex and diverse sensory processing needs of children with ADHD. Additionally, there are no formal guidelines for designing specialized therapeutic environments for this population, nor is there effective interdisciplinary collaboration among architects, occupational therapists, child psychologists, and other relevant professionals. Furthermore, there is limited research to establish a scientific framework for design. These scientific and practical limitations not only compromise the quality of therapeutic environments but may also directly impact the effectiveness of treatment and the psychological well-being of children [18]. Therefore, conducting interdisciplinary research, developing localized and applicable design guidelines, and implementing targeted programs in the field of therapeutic environment design for children with ADHD in Iran is a critical.
This study was conducted as the continuation of prior research that identified and analyzed architectural factors influencing the design of rehabilitation environments for children with ADHD and autism in Iran [19]. In the present study, we aim to empirically assess the impact of architectural modifications in 12 occupational therapy centers located in Tehran and Karaj cities on the sensory profile of children with ADHD.
Materials and Methods
Study design and participants
This is a quasi-experimental study conducted in two separate phases. Phase 1 included a comparison between rehabilitation environments with optimal and suboptimal architectural features regarding the impact of their architectural design on sensory processing performance in children with ADHD. In phase 2, the centers identified as suboptimal in phase 1 underwent architectural modifications, and the degree of change and improvement in the children’s sensory performance was assessed and compared with their progress during phase I. Participants were 64 children diagnosed with ADHD, including 20 girls and 44 boys (mean age=8.5±2.2 years), who had been enrolled in occupational therapy centers for less than one week and had no prior therapeutic history, and were selected using a convenience sampling method from 12 occupational therapy clinics located in Tehran and Karaj in 2024. To determine the sample size, a significance level of α=0.05, a test power of 80% and a medium effect size (Cohen’s d=0.5) were considered. The required sample size for comparing group means was calculated to be 50. Considering potential dropout, it increased to 64. These participants were recruited. Inclusion criteria for participation were age 5-10 years, Diagnosis of moderate ADHD based on the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) criteria by a psychiatrist or pediatric neurologist, no comorbid severe disorders (e.g. autism spectrum disorder or intellectual disability), regular attendance in occupational therapy sessions (2 sessions per week) and written informed consent of the parents. The children were divided into two groups based on the type of treatment center, including optimal centers (n=25) and suboptimal centers (n=39).
Occupational therapy
All participants received a sensory-based occupational therapy program tailored to their individual sensory processing profiles. The intervention included play-based activities, stimulation of various sensory systems (vestibular, proprioceptive, tactile, and visual), and modulated sensory exercises designed to enhance responsiveness to environmental stimuli. The intervention lasted six weeks, consisting of twelve 45-minute sessions.
Instruments
For center classification, a checklist was used, derived from a detailed questionnaire containing 30 items and six architectural domains [19, 20]. The face and content validity of this questionnaire had been confirmed, with a Cronbach’s α coefficient of 0.81. Each rehabilitation center was evaluated based on six architectural criteria: Lighting, acoustics, color scheme, spatial access/layout, ventilation, and spatial organization/safety. Centers were rated using a five-point Likert scale. Centers scoring above the average total score (65 out of 90) were classified as “optimal” (7 centers), while those with lower scores were considered “suboptimal” (5 centers).
Sensory processing performance was assessed using the Persian version of the SSP [6]. It consists of 7 domains and 38 items, assessing various sensory patterns, including sensory seeking, sensory avoidance, sensory sensitivity, and low registration. Scoring is based on a five-point Likert scale (always, frequently, occasionally, seldom, never), with scores ranging from 38 to 190. Lower scores indicate greater difficulties with sensory processing. According to normative data from typically developing children, SSP scores are classified as follows: >155 (typical performance), 142–154 (probable difference), and <141 (definite difference) [8]. The Persian version of the SSP has already been translated and validated by Shahbazi et al., who demonstrated its satisfactory reliability and validity [7]. The questionnaire was completed by the parents of children before the intervention and after the end of therapy sessions.
Architectural modifications of suboptimal centers
Targeted architectural changes were implemented in the five centers previously identified as suboptimal in terms of architectural features influencing therapeutic outcomes for children with ADHD. After these modifications, therapy programs continued, and the impact of these changes on sensory processing performance was evaluated. The modifications included: Controlling natural light with curtains to reduce direct light intensity, improving acoustic insulation to reduce background noise and prevent sudden auditory stimuli, the use of cool and muted color schemes on walls, flooring, and furniture (via covers), and designing separate activity zones with varying levels of sensory stimulation.
Statistical analysis
Data analysis was performed in SPSS software, version 26. The independent t-test was used to compare groups in phase 1, and a paired t-test was used to compare pre- and post-intervention differences in phase 2. The significance level was set at 0.05 for all analyses.
Results
Within-group comparison of SSP scores
In phase 1, the mean SSP scores were compared within two groups. The pre-test–post-test comparison revealed that children attending centers with optimal architectural features exhibited significantly higher SSP domain scores (Table 1).
In both groups, the total SSP score increased significantly after intervention, indicating improvement in sensory processing performance. However, in the suboptimal group, this increase was less pronounced and borderline significant (P=0.048). The improvement in the optimal group was statistically more significant (P<0.001).
Between-group comparison of SSP scores
The optimal centers group showed significantly greater improvement across all SSP subscales compared to the suboptimal centers group (Table 2).
In both groups, the sensory seeking subscale demonstrated the highest significant improvement, while other indices showed relatively similar improvement.
Impact of architectural modifications in suboptimal centers
In phase 2, architectural improvements were implemented in five suboptimal centers. Children who had participated in Phase 1 continued to receive a new 12-session occupational therapy program within the same centers after modifications. The change in SSP scores was reassessed and compared to the pre-modification scores seen in phase 1. Although the mean total SSP score improved following architectural modifications, the magnitude of change was not significantly different compared to the phase I results (P=0.06), indicating a positive trend but a non-significant size (Table 3).
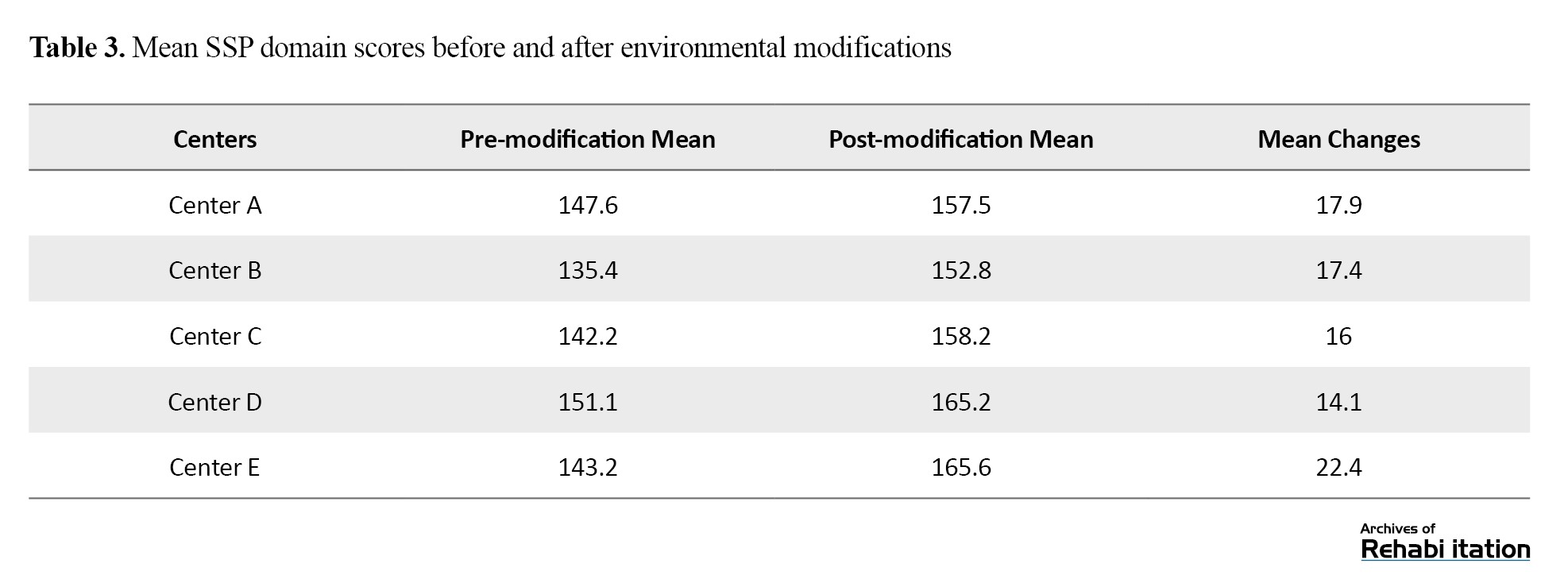
However, a significant difference was observed when comparing the improvement in modified centers to that of optimal centers (P=0.01).
The difference in the slope of improvement curves in Figure 1 for optimal and suboptimal centers (before modifications) highlights the critical role of architectural features in supporting sensory processing improvement in children with ADHD.
Although the trend after architectural modifications showed a more favorable slope in suboptimal centers, a noticeable gap remained compared to the outcomes in optimal centers.
Discussion
The primary objective of this study was to investigate the impact of architectural features of rehabilitation centers on the improvement of sensory processing performance in children with ADHD. The results revealed that therapeutic centers with favorable architectural characteristics had a significantly greater effect on enhancing children’s sensory processing compared to centers lacking such features. This finding aligns with the results of Voola [21], which emphasized the role of physical environment in reducing sensory and behavioral difficulties among children with special needs. In this study, targeted and specific architectural modifications were implemented in key domains to examine their effects on the sensory processing performance of children with ADHD. These modifications included controlling natural light by using curtains to reduce direct light intensity, improving acoustic insulation to minimize background noise and sudden auditory stimuli, applying cool and soft color patterns to walls, floors, and furniture (using covers), and designing separate activity spaces with varying levels of sensory stimulation. These changes according to the findings of recent studies such as Voola [21], which demonstrated that even minor environmental interventions can help regulate sensory responses and improve behavioral outcomes in children with special needs. Nevertheless, financial and structural limitations hindered more extensive modifications in some centers, resulting in relatively lower levels of sensory improvement compared to those with fully optimized environments. This highlights the importance of comprehensive and intentional design in therapeutic settings particularly in factors such as lighting, acoustics, color, and spatial arrangement which can play a crucial role in facilitating treatment processes and enhancing the quality of life for children with ADHD. These results are also consistent with modern therapeutic approaches like sensory integration (SI) and neurodevelopmental treatment (NDT), both of which emphasize environmental regulation as a foundational component of effective intervention.
From a qualitative perspective, several architectural modifications were associated with improved sensory processing. The presence of soft, indirect light with appropriate intensity regulation was associated with reduced sensory sensitivity and improved attention during therapy sessions. Studies suggest that natural lighting with warm color temperature can enhance cognitive performance and reduce anxiety in children with ADHD [22]. Background noise is a disruptive stimulus for children with attention disorders. Centers with better sound control reported reduced sensory sensitivity and improved therapy tolerance among children. Recent research highlights that reducing sound levels and minimizing echo in therapy spaces can improve concentration and reduce self-stimulatory behaviors in children who are sensitive to sound [23]. The use of cool, calming colors and soft textures on walls and floors was effective in emotional regulation and preventing sensory overload. Contemporary findings have also shown that pastel and muted colors create a relaxing environment [24]. The design of spaces for activities needed high stimulation (e.g. trampolines or balance games) separated from quiet spaces (e.g. individual therapy rooms) facilitated better sensory regulation. The creation of predictable routes and shelters can contribute to reduced cognitive load and a greater sense of security for children [25]. Multisensory and interactive spaces such as dark rooms with colored lights, textured walls, or sensory equipment like balance balls, were more frequently observed in optimized centers. Studies have shown that multisensory response rooms can improve sensory regulation and reduce anxiety in children with sensory processing difficulties [26–28].
Although after architectural modifications in suboptimal centers, noticeable improvements in the rate and extent of sensory progress were reported, these improvements were not statistically significant compared to the pre-modification scores (phase 1). Furthermore, the degree of improvement remained significantly lower than that observed in optimized centers. This may be attributed to the limited scope of modifications due to technical, financial, and structural constraints. Most changes in these centers were limited but noticeable, particularly in the lighting and coloring of the environment, the control of ambient noise, and the layout of the therapy room. On average, these improvements increased the SSP scores numerically by about 10.5 units. Among the five modified centers, three centers reached the desirable level, while two centers, despite quality improvements, remained within the desirable range. It is possible that more extensive and complete changes would have resulted in better therapeutic outcomes. However, the mean score differences indicated clinically noticeable improvement that could be effective in management and decisions about the design of rehabilitation centers in Iran. Voola [21] also demonstrated that environmental changes, even if small, can help modulate sensory responses in children with ADHD. These findings further support the environmental regulation model emphasized in modern occupational therapy frameworks such as SI and NDT [12, 14].
In therapeutic settings for children with sensory processing disorders, proper design of environmental elements such as acoustics, lighting, color, and spatial arrangement plays a vital role in enhancing sensory integration and reducing anxiety. Research shows that bright flickering, or fluorescent light, can lead to visual overstimulation, headaches, or discomfort in children with sensory sensitivities, while the use of controlled natural light or light with a warm, uniform color temperature helps better regulate visual stimuli [24]. Color schemes in therapy environments for children with sensory processing problems are also a crucial factor. Cool, soft colors like light blue, green, or light gray have a calming effect, while strong colors like red or yellow may cause overstimulation. The use of neutral and soft colors can help reduce visual stimulation and improve attention [24]. Regarding auditory stimuli, research has shown that sudden, loud, or irregular sounds can cause anxiety, distraction, or extreme behavioral responses in children with sensory impairment. The use of soundproofing materials, soft background music, and controlled sound sources can help calm the nervous system of these children [23]. Finally, the layout of therapeutic spaces has been identified as a key factor. Organized, predictable spaces with clear boundaries help reduce anxiety and improve attention. Creating calming zones with sensory tools such as heavy blankets, tactile toys, and quiet corners supports children in managing sensory stimuli more effectively [28].
This study had some limitations. The study was restricted to rehabilitation centers located in Tehran and Karaj cities. Also, there was a limited number of study centers. Further studies in other cities and provinces of Iran, using a higher number of participating centers and children, are recommended.
Conclusion
This study demonstrated that the architectural design of rehabilitation centers has a significant impact on sensory processing quality and, consequently, the effectiveness of therapy in children with ADHD. The centers designed based on sensory-regulation principles such as controlled natural light, soundproofing, soft and calming color palettes, functional separation of spaces, and the presence of natural elements, were more effective in improving sensory profiles of ADHD children compared to the centers lacking these features. Although limited architectural modifications in suboptimal centers led to improvements, the statistically non-significant results indicated that superficial and limited changes cannot replace foundational space design. Therefore, it is crucial that in the design or redesign of pediatric rehabilitation centers, the sensory-regulation principles of architecture responsive to sensory needs should be considered from the beginning. Also, close collaboration between architects and occupational therapists in the design or renovation of therapeutic environments is needed. Further studies should investigate the effects of specific environmental elements (e.g. color, sound, texture) separately on the sensory performance of ADHD children or on other functional aspects of children such as attention, sleep quality, and emotional regulation. The use of neuroimaging techniques (e.g. fMRI, EEG) to examine brain activity changes in architecturally modified rehabilitation centers is also recommended. A simulation software should be developed for designing therapeutic spaces tailored to children with neurodevelopmental disorders such as ADHD.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Vice Chancellor of the Faculty of Technology and Engineering, Saveh Branch, Islamic Azad University (Code: 18160202952016).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The author sincerely thank all the participating children, their parents, and the managers of the occupational therapy centers for their cooperation. The author also sincerely acknowledge the valuable consultations and guidance of Navid Mirzakhany.
Discussion
The primary objective of this study was to investigate the impact of architectural features of rehabilitation centers on the improvement of sensory processing performance in children with ADHD. The results revealed that therapeutic centers with favorable architectural characteristics had a significantly greater effect on enhancing children’s sensory processing compared to centers lacking such features. This finding aligns with the results of Voola [21], which emphasized the role of physical environment in reducing sensory and behavioral difficulties among children with special needs. In this study, targeted and specific architectural modifications were implemented in key domains to examine their effects on the sensory processing performance of children with ADHD. These modifications included controlling natural light by using curtains to reduce direct light intensity, improving acoustic insulation to minimize background noise and sudden auditory stimuli, applying cool and soft color patterns to walls, floors, and furniture (using covers), and designing separate activity spaces with varying levels of sensory stimulation. These changes according to the findings of recent studies such as Voola [21], which demonstrated that even minor environmental interventions can help regulate sensory responses and improve behavioral outcomes in children with special needs. Nevertheless, financial and structural limitations hindered more extensive modifications in some centers, resulting in relatively lower levels of sensory improvement compared to those with fully optimized environments. This highlights the importance of comprehensive and intentional design in therapeutic settings particularly in factors such as lighting, acoustics, color, and spatial arrangement which can play a crucial role in facilitating treatment processes and enhancing the quality of life for children with ADHD. These results are also consistent with modern therapeutic approaches like sensory integration (SI) and neurodevelopmental treatment (NDT), both of which emphasize environmental regulation as a foundational component of effective intervention.
From a qualitative perspective, several architectural modifications were associated with improved sensory processing. The presence of soft, indirect light with appropriate intensity regulation was associated with reduced sensory sensitivity and improved attention during therapy sessions. Studies suggest that natural lighting with warm color temperature can enhance cognitive performance and reduce anxiety in children with ADHD [22]. Background noise is a disruptive stimulus for children with attention disorders. Centers with better sound control reported reduced sensory sensitivity and improved therapy tolerance among children. Recent research highlights that reducing sound levels and minimizing echo in therapy spaces can improve concentration and reduce self-stimulatory behaviors in children who are sensitive to sound [23]. The use of cool, calming colors and soft textures on walls and floors was effective in emotional regulation and preventing sensory overload. Contemporary findings have also shown that pastel and muted colors create a relaxing environment [24]. The design of spaces for activities needed high stimulation (e.g. trampolines or balance games) separated from quiet spaces (e.g. individual therapy rooms) facilitated better sensory regulation. The creation of predictable routes and shelters can contribute to reduced cognitive load and a greater sense of security for children [25]. Multisensory and interactive spaces such as dark rooms with colored lights, textured walls, or sensory equipment like balance balls, were more frequently observed in optimized centers. Studies have shown that multisensory response rooms can improve sensory regulation and reduce anxiety in children with sensory processing difficulties [26–28].
Although after architectural modifications in suboptimal centers, noticeable improvements in the rate and extent of sensory progress were reported, these improvements were not statistically significant compared to the pre-modification scores (phase 1). Furthermore, the degree of improvement remained significantly lower than that observed in optimized centers. This may be attributed to the limited scope of modifications due to technical, financial, and structural constraints. Most changes in these centers were limited but noticeable, particularly in the lighting and coloring of the environment, the control of ambient noise, and the layout of the therapy room. On average, these improvements increased the SSP scores numerically by about 10.5 units. Among the five modified centers, three centers reached the desirable level, while two centers, despite quality improvements, remained within the desirable range. It is possible that more extensive and complete changes would have resulted in better therapeutic outcomes. However, the mean score differences indicated clinically noticeable improvement that could be effective in management and decisions about the design of rehabilitation centers in Iran. Voola [21] also demonstrated that environmental changes, even if small, can help modulate sensory responses in children with ADHD. These findings further support the environmental regulation model emphasized in modern occupational therapy frameworks such as SI and NDT [12, 14].
In therapeutic settings for children with sensory processing disorders, proper design of environmental elements such as acoustics, lighting, color, and spatial arrangement plays a vital role in enhancing sensory integration and reducing anxiety. Research shows that bright flickering, or fluorescent light, can lead to visual overstimulation, headaches, or discomfort in children with sensory sensitivities, while the use of controlled natural light or light with a warm, uniform color temperature helps better regulate visual stimuli [24]. Color schemes in therapy environments for children with sensory processing problems are also a crucial factor. Cool, soft colors like light blue, green, or light gray have a calming effect, while strong colors like red or yellow may cause overstimulation. The use of neutral and soft colors can help reduce visual stimulation and improve attention [24]. Regarding auditory stimuli, research has shown that sudden, loud, or irregular sounds can cause anxiety, distraction, or extreme behavioral responses in children with sensory impairment. The use of soundproofing materials, soft background music, and controlled sound sources can help calm the nervous system of these children [23]. Finally, the layout of therapeutic spaces has been identified as a key factor. Organized, predictable spaces with clear boundaries help reduce anxiety and improve attention. Creating calming zones with sensory tools such as heavy blankets, tactile toys, and quiet corners supports children in managing sensory stimuli more effectively [28].
This study had some limitations. The study was restricted to rehabilitation centers located in Tehran and Karaj cities. Also, there was a limited number of study centers. Further studies in other cities and provinces of Iran, using a higher number of participating centers and children, are recommended.
Conclusion
This study demonstrated that the architectural design of rehabilitation centers has a significant impact on sensory processing quality and, consequently, the effectiveness of therapy in children with ADHD. The centers designed based on sensory-regulation principles such as controlled natural light, soundproofing, soft and calming color palettes, functional separation of spaces, and the presence of natural elements, were more effective in improving sensory profiles of ADHD children compared to the centers lacking these features. Although limited architectural modifications in suboptimal centers led to improvements, the statistically non-significant results indicated that superficial and limited changes cannot replace foundational space design. Therefore, it is crucial that in the design or redesign of pediatric rehabilitation centers, the sensory-regulation principles of architecture responsive to sensory needs should be considered from the beginning. Also, close collaboration between architects and occupational therapists in the design or renovation of therapeutic environments is needed. Further studies should investigate the effects of specific environmental elements (e.g. color, sound, texture) separately on the sensory performance of ADHD children or on other functional aspects of children such as attention, sleep quality, and emotional regulation. The use of neuroimaging techniques (e.g. fMRI, EEG) to examine brain activity changes in architecturally modified rehabilitation centers is also recommended. A simulation software should be developed for designing therapeutic spaces tailored to children with neurodevelopmental disorders such as ADHD.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Vice Chancellor of the Faculty of Technology and Engineering, Saveh Branch, Islamic Azad University (Code: 18160202952016).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The author sincerely thank all the participating children, their parents, and the managers of the occupational therapy centers for their cooperation. The author also sincerely acknowledge the valuable consultations and guidance of Navid Mirzakhany.
References
- Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics. 2015; 135(4):e994-1001. [DOI:10.1542/peds.2014-3482] [PMID]
- Miller LJ, Nielsen DM, Schoen SA, Brett-Green BA. Perspectives on sensory processing disorder: A call for translational research. Frontiers in Integrative Neuroscience. 2009; 3:22. [DOI:10.3389/neuro.07.022.2009] [PMID]
- Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. The lancet. Psychiatry. 2018; 5(9):727-38. [DOI:10.1016/S2215-0366(18)30269-4] [PMID]
- Schaaf RC, Dumont RL, Arbesman M, May-Benson TA. Efficacy of occupational therapy using Ayres Sensory Integration®: A systematic review. The American Journal of Occupational Therapy. 2018; 72(1):7201190010p1-0. [DOI:10.5014/ajot.2018.028431]
- Case-Smith J, Weaver LL, Fristad MA. A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism. 2015; 19(2):133-48. [DOI:10.1177/1362361313517762] [PMID]
- Dunn W. The short sensory profile. San Antonio: The Psychological Corporation; 1999. [Link]
- Shahbazi M, Mirzakhany N, Alizadeh Zarei M, Zayeri F, Daryabor A. Translation and cultural adaptation of the Sensory Profile 2 to the Persian language. British Journal of Occupational Therapy. 2021; 84(12):794-805. [DOI:10.1177/0308022621991768]
- Bandyopadhyay A, Nath S, Mandal U, Ghoshal S, Dandapath A, Mallick S. Sensory processing patterns in children with attention-deficit hyperactivity disorder: A case-control study. Asian Journal of Medical Sciences. 2024; 15(6):95-100. [DOI:10.71152/ajms.v15i6.3621]
- Sternberg E, Karlin E, Gage-White L. Healing spaces: The science of architecture and health. Cambridge: Harvard University Press; 2009. [Link]
- Devlin AS, Arneill AB. Health care environments and patient outcomes: A review of the literature. Environment and Behavior. 2003; 35(5):665-94. [DOI:10.1177/0013916503255102]
- Ulrich RS, Zimring C, Zhu X, DuBose J, Seo HB, Choi YS, et al. A review of the research literature on evidence-based healthcare design. HERD. 2008; 1(3):125-61. [DOI:10.1177/193758670800100306] [PMID]
- Ruiz-Herrera N, Cellini N, Prehn-Kristensen A, Guillén-Riquelme A, Buela-Casal G. Characteristics of sleep spindles in school-aged children with attention-deficit/hyperactivity disorder. Research in Developmental Disabilities. 2021; 112:103896. [DOI:10.1016/j.ridd.2021.103896] [PMID]
- Pati D, Harvey TE Jr, Willis DA, Pati S. Identifying elements of the health care environment that contribute to wayfinding. HERD. 2015; 8(3):44-67. [DOI:10.1177/1937586714568864] [PMID]
- Vanaken, GJ, Danckaerts M. Impact of green space exposure on children’s and adolescents’ mental health: A systematic review. International Journal of Environmental Research and Public Health.2018; 15(12):2668. [DOI:10.3390/ijerph15122668]
- Finnigan KA. Sensory responsive environments: A qualitative study on perceived relationships between outdoor built environments and sensory sensitivities. Land. 2024; 13(5):636. [DOI:10.3390/land13050636]
- Kelly S, Kerr J, Rieger J, Cushing DF. Let’s Play: Co-designing inclusive school playgrounds with neurodivergent children. International Journal of Educational Research Open. 2025; 9:100494. [DOI:10.1016/j.ijedro.2025.100494]
- Villa-Velásquez J, Reynaldos-Grandón K, Chepo Chepo M, Rivera-Rojas F, Valencia-Contrera M. Interdisciplinary approach to the care of children and adolescents with special health needs: An integrative review. Archivos Argentinos de Pediatria. 2025; 123(4):e202410577. [DOI:10.5546/aap.2024-10577.eng] [PMID]
- Hegde A. Sensory sensitivity and the built environment. Lighting Design+Application. 2015; 45(1):56-60. [DOI:10.1177/036063251504500116]
- Irani N, Bavar C, Mirzakhani Araghi N. [The relationship between physical factors and architecture of rehabilitation educational therapeutic centers with the quality of rehabilitation services in children with autism from the perspective of their occupational therapists and parents (Persian)]. Scientific Journal of Rehabilitation Medicine. 2023; 12(1):164-85. [DOI:10.32598/SJRM.12.1.11]
- Irani N, Bavar C, Mirzakhani N, Daryabor A, Pashmdarfard M, Khademi Kalantari S. [Effect of interior architecture of rehabilitation centers on the outcome of occupational therapy for children with autism spectrum disorders (Persian)]. Archives of Rehabilitation. 2024; 24(4):602-15. [DOI:10.32598/RJ.24.4.3671.2]
- Voola SI. Home garden to sensory play space: Paving the way to quality outdoor play. Current Pediatric Research. 2023; 27(10):1185-9. [Link]
- Chidiac, S.E.; Reda, M.A.; Marjaba, G.E. Built Environment for People with Sensory Disabilities. Encyclopedia [Unpublished]. [DOI:10.3390/buildings14030707]
- Tola G, Talu V, Congiu T, Bain P, Lindert J. Built environment design and people with autism spectrum disorder (ASD): A scoping review. International Journal of Environmental Research and public health. 2021; 18(6):3203. [DOI:10.3390/ijerph18063203] [PMID]
- Nair AS, Priya RS, Rajagopal P, Pradeepa C, Senthil R, Dhanalakshmi S, et al. A case study on the effect of light and colors in the built environment on autistic children's behavior. Frontiers in Psychiatry. 2022; 13:1042641. [DOI:10.3389/fpsyt.2022.1042641] [PMID]
- Schilling DL, Washington K, Billingsley FF, Deitz J. Classroom seating for children with attention deficit hyperactivity disorder: Therapy balls versus chairs. The American Journal of Occupational Therapy. 2003; 57(5):534-41. [DOI:10.5014/ajot.57.5.534] [PMID]
- Ashburner J, Ziviani J, Rodger S. Sensory processing and classroom emotional, behavioral, and educational outcomes in children with autism spectrum disorder. The American Journal of Occupational Therapy. 2008; 62(5):564-73. [DOI:10.5014/ajot.62.5.564] [PMID]
- Voola SI, Kumari MV. Sensory garden: Piloting an affordable nature-based intervention for functional behavior of children with attention deficit hyperactivity disorder (ADHD). Current Pediatric Research. 2022; 26(5):5. [Link]
- Koenig KP, Rudney SG. Performance challenges for children and adolescents with difficulty processing and integrating sensory information: A systematic review. The American Journal of Occupational Therapy. 2010; 64(3):430-42. [DOI:10.5014/ajot.2010.09073] [PMID]
Type of Study: Original |
Subject:
Occupational Therapy
Received: 25/06/2025 | Accepted: 13/08/2025 | Published: 1/10/2025
Received: 25/06/2025 | Accepted: 13/08/2025 | Published: 1/10/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |