Volume 26, Issue 1 (Spring 2025)
jrehab 2025, 26(1): 134-149 |
Back to browse issues page
Ethics code: IR.USWR.REC.1401.220
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mehboodi R, Javanbakht M, Ramezani M, Ebrahimi A A, Bakhshi E. Normalization and Validation of the Persian Version of the Scale of Auditory Behaviors. jrehab 2025; 26 (1) :134-149
URL: http://rehabilitationj.uswr.ac.ir/article-1-3508-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3508-en.html
Reyhane Mehboodi1 

 , Mohanna Javanbakht2
, Mohanna Javanbakht2 

 , Maryam Ramezani *3
, Maryam Ramezani *3 

 , Amir Abbas Ebrahimi4
, Amir Abbas Ebrahimi4 

 , Enayatollah Bakhshi5
, Enayatollah Bakhshi5 




 , Mohanna Javanbakht2
, Mohanna Javanbakht2 

 , Maryam Ramezani *3
, Maryam Ramezani *3 

 , Amir Abbas Ebrahimi4
, Amir Abbas Ebrahimi4 

 , Enayatollah Bakhshi5
, Enayatollah Bakhshi5 


1- Department of Audiology, School of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Audiology, School of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Audiology, School of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,maryamramezani16@gmail.com
4- Department of Audiology Special Education Organization, Tehran, Iran.
5- Department of Biostatistics and Epidemiology, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Audiology, School of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Audiology, School of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
4- Department of Audiology Special Education Organization, Tehran, Iran.
5- Department of Biostatistics and Epidemiology, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Keywords: Scale of auditory behaviors (SABs), Screening, Auditory processing disorder (ADP), Reliability, Validity
Full-Text [PDF 1779 kb]
(711 Downloads)
| Abstract (HTML) (2896 Views)
Full-Text: (543 Views)
Introduction
Auditory processing disorder (ADP) is a type of perceptual processing disorder involving auditory information in the central nervous system and its biological activities. Individuals with this disorder, despite having normal hearing thresholds and average intelligence, experience difficulties in processing auditory stimuli, particularly speech in the presence of environmental background noise [1]. Individuals with ADP exhibit poor auditory performance in environments with competing noise or highly reverberant settings struggle to follow verbal instructions effectively and face challenges in understanding rapid or degraded speech, especially in the presence of competing noise. Difficulties also arise in sound localization and directional hearing. Common issues include frequent requests for repetition or clarification, language impairments, difficulties in reading and pronunciation, challenges in telephone conversations, and an inability to detect subtle tonal changes essential for humor and sarcasm. These individuals often struggle to learn a foreign language or new verbal material, maintain attention, sing, or understand music. Educational challenges are also prevalent among subjects with ADP [2].
APD is observed across various populations, including children and adults [3]. Among children, due to their developmental stage and involvement in learning and education, it holds particular significance [4]. Studies estimate the prevalence of APD in school-aged children to range from 2% to 20% [5, 6, 7, 8, 9, 10]. Meanwhile, in Iran, the prevalence of suspected APD in children is reported around 9.8% [11]. In school-aged children in Tehran City, Iran, the prevalence is reported as 3.3% in girls, 3.8% in boys, and 4.6% overall [12]. Early identification and diagnosis of APD can significantly mitigate its adverse effects on children’s education and learning [13]. The diagnosis of APD varies significantly depending on the evaluation criteria and tools used [2]. Various disorders, such as attention deficit hyperactivity disorder (ADHD) and learning disabilities may present with similar clinical manifestations, necessitating precise diagnosis for effective management and treatment [14].
Currently, several tests and questionnaires are available for evaluating and diagnosing APD in children. Given the complexity of diagnosis and the importance of early intervention, screening is essential to refer children for comprehensive diagnostic tests. Screening tools help identify children needing further evaluation, differentiate APD from similar disorders, help in faster identification of ADP and thereby more effective interventions and minimize the negative impact on children and their families. Additional benefits of screening include reducing unnecessary referrals and prioritizing children for diagnostic evaluations, thus lowering overall clinical intervention costs and improving rehabilitation efficiency [15].
The screening phase typically involves questionnaires, behavioral tests, or a combination of both. Cost-effective and easily administered tools are essential for screening a wide population. Accordingly, questionnaires, in particular, offer practical and detailed information about individuals’ daily challenges and are considered a preferable first step compared to behavioral tests [16]. Current screening tools for APD include the Fisher’s auditory problems checklist, the children’s auditory processing performance scale, the scale of auditory behaviors (SABs), the auditory processing domain questionnaire, and the Buffalo model questionnaire [7, 8, 16]. In Iran, validated Persian versions of these tools include the auditory processing domain questionnaire, developed at Iran University of Medical Sciences in 2017 [12, 13], the Buffalo model questionnaire, developed at Tehran University of Medical Sciences in 2020 [17], and the Fisher’s checklist, developed at the University of Tehran in 2018 [18].
One comprehensive diagnostic test battery is the multiple auditory processing assessment (MAPA), which identifies and diagnoses APD early to expedite intervention [19]. Alongside MAPA, the SABs serves as a screening tool. The SAB was designed based on studies by Chermak (1998) and Shiffman (1999) to identify individuals with APD in conjunction with behavioral diagnostic tests [20].
It consists of 12 questions addressing listening-related behaviors, which reflect the behaviors that arise often in people with ADP and I rated on a scale from 1 (frequently) to 5 (never) by parents, teachers, or knowledgeable adults. Scores range from 12 to 60, with scores below 46 indicating a risk for APD in the original version. The SAB should be used alongside at least one subtest from the MAPA for functional assessment of results [21]. Considering the importance of questionnaires in APD screening, their ease of scoring by knowledgeable adults such as parents or teachers, high validity, and applicability in clinical research, the present study develops a Persian version of the SAB and determines its cutoff point, reliability, and validity.
Materials and Methods
In the initial phase, after obtaining permission from the creator of the SAB questionnaire, the translation process was conducted following the international protocol for quality-of-life assessment. The questionnaire was first translated into Persian by two bilingual translators fluent in English and experts in Persian. To ensure alignment with the original version, the translated questionnaire was back-translated into English by a third person, an English speaker fluent in Persian. The back-translated English version was then sent to the original author, and after their approval, the Persian translation was reviewed by audiology specialists working in the field of ADPs. These specialists evaluated the translation for standard quality, face validity, and content validity.
Based on their suggestions and the research team’s review, necessary modifications were applied to the questions. In the second phase, convenience sampling was employed to recruit 360 school-aged children from Tehran City and Shiraz City, Iran, whose parents provided informed consent; meanwhile, their medical history showed no evidence of neurological, psychological, or auditory problems. All children underwent otoscopy, audiometry, and tympanometry tests. Exclusion criteria were the lack of willingness by the child or parent to continue the study, inability to complete the tests, or loss of eligibility during the study. Based on these criteria, 32 children were diagnosed with APD, and 328 children were classified as typically developing for normative data calculation.
The participants underwent the following tests: Working memory assessment and the behavioral subtests of MAPA, including the monaural selective auditory attention test, dichotic digit test, and pitch pattern sequence test. The monaural selective auditory attention test assesses selective auditory attention in children. In this test, an engaging age-appropriate story is played, interspersed with some keywords (e.g. “point to the apple.”). The child is instructed to ignore the story and respond only to the keywords. The test consists of 25 items, each with six closed-set responses. A child distracted by the story fails to identify the target words. This test evaluates speech perception in noise and auditory selective attention [22]. The pitch pattern sequence test evaluates a child’s pattern recognition and frequency discrimination abilities. It includes 20 sets of high- and low-pitched tones presented in a specific order, which the child must reproduce in the same sequence [23].
The dichotic digit test includes four-digit sequences, with two digits presented simultaneously to each ear. The child repeats the numbers heard. This test is ideal for evaluating central auditory processing issues due to its high sensitivity, short duration (under 5 min), ease of administration, rapid scoring, low linguistic load, clear instructions, and tolerance of mild conductive or sensorineural hearing loss. Scoring is based on individual ear performance and interaural differences [24].
The participants were classified into APD and typically developing groups based on low scores in at least two of the three behavioral tests from the MAPA subtests. The SAB questionnaire was administered to parents and teachers (to eliminate bias) of both groups across four age categories as follows: 8–9, 9–10, 10–11, and 11–12 years. Questionnaire scores were compared with the MAPA results. Reliability was assessed using the test re-test method, calculating intra-class correlation coefficients (ICC). Internal consistency reliability was measured using the Cronbach α method. For this purpose, parents and teachers of 30 children completed the questionnaire again after a two-week interval, and the reliability of the questionnaire was analyzed.
Results
This study developed a Persian version of the SAB questionnaire and evaluated its validity and reliability to create a robust and reliable tool for screening children with APD and for clinical use. The statistical analysis of the results and related discussions are presented here.
The acceptable threshold for content validity ratio, based on the participation of 10 audiologists in the survey, is above 0.62. For the content validity index of each question, a value above 0.79 is considered acceptable. In this study, the necessity of each question in the Persian version of the SAB questionnaire was assessed by experts, and the content validity ratio exceeded the minimum threshold of 0.62. The average content validity index for the criteria of relevance, clarity, and simplicity of the Persian SAB questionnaire was 1.00, 0.99, and 0.99, respectively; values well above the 0.79 benchmark indicate strong content validity.
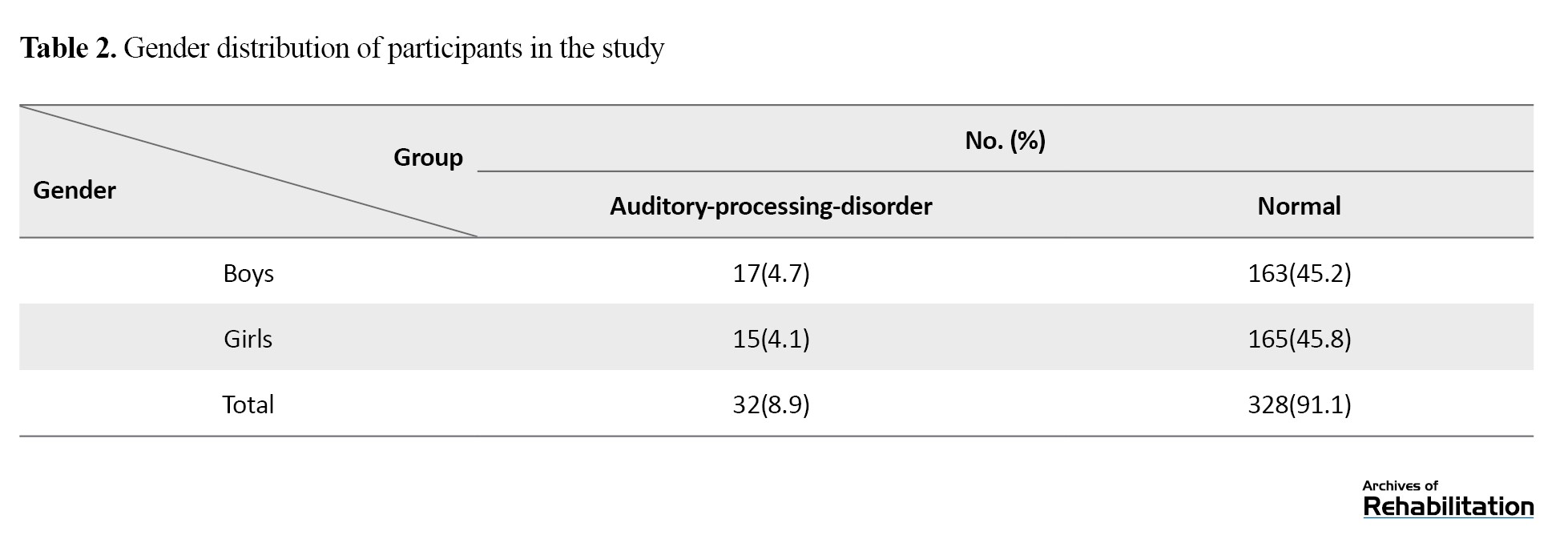
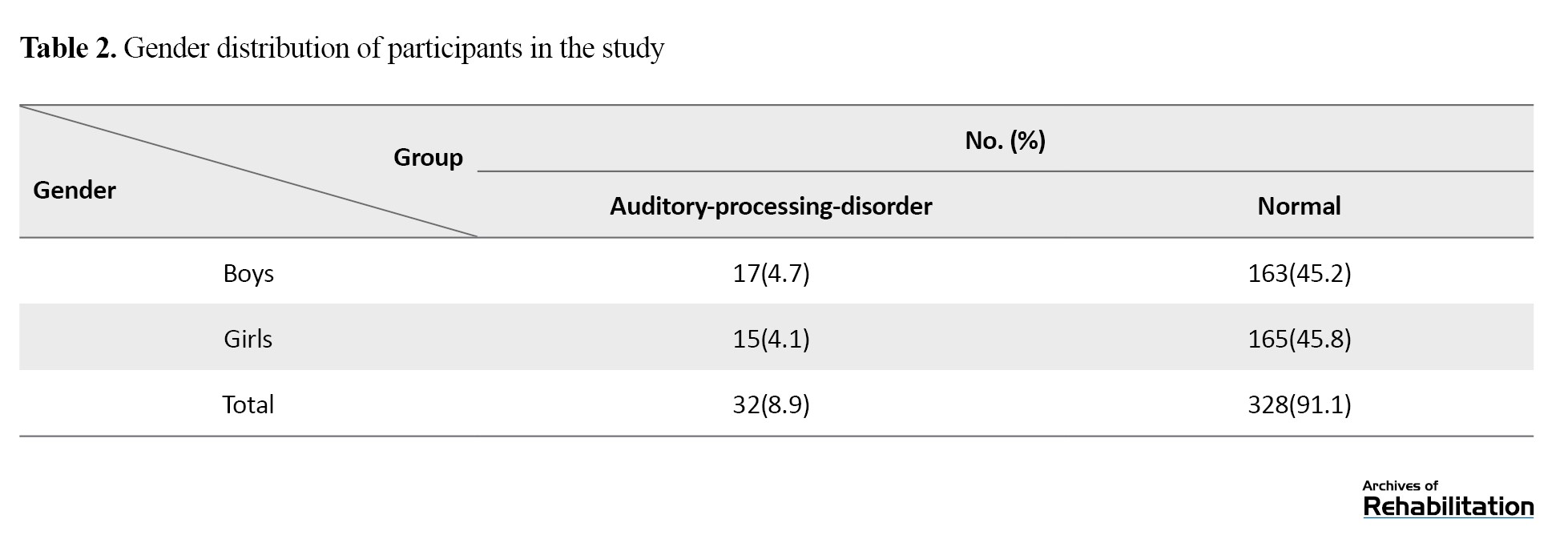
The Persian version of the SAB questionnaire was tested on a sample of 360 children aged 8 to 12 years, representing the largest psychometric analysis of this scale to date. The Mean±SD score for the parent version of the SAB was 50.59±7.45), while the teacher version had a Mean±SD score of 49.68±6.79). The gender distribution of the study participants is shown in Table 1.
In the present study, the scores of the SAB questionnaire in the teacher and parent versions were examined separately in different age groups and no significant difference was observed between the different groups. (P<0.05)
For discriminative validity and reliability assessment, 360 school-aged children were studied across four age groups (90 children per group): 8–9, 9–10, 10–11, and 11–12 years. The APD group included 32 children (15 girls and 17 boys), while the typically developing group included 328 children (165 girls and 163 boys). Scores from the parent and teacher versions of the SAB were divided into the APD and typically developing groups. To examine the relationship between SAB questionnaire results and the findings from the MAPA subtests, the chi-square test was employed.
In comparing the scores of the parent questionnaire, 30 out of 32 students with APD were correctly identified (93.8%), and 326 out of 328 typically developing students were accurately classified (99.3%). Similarly, for the teacher questionnaire, 30 out of 32 APD students were correctly identified (93.8%), while 325 out of 328 typically developing students were accurately classified (99.1%). Due to the low frequency of certain values and the fact that 25% of the data points were below 5, the Fisher exact test was used to assess the association or independence of the grouped scores. P for the teacher questionnaire were <0.001, indicating a significant relationship between the grouped questionnaire scores and the grouped results of the MAPA.
The strong correlation between the SAB questionnaire and MAPA results in the Persian version confirms their convergent validity and compatibility. To compare questionnaire scores across different age groups, a one-way analysis of variance was conducted, showing no significant differences between groups (P>0.05) (Table 2).
Test re-test reliability was assessed using ICC. The parents and teachers of 30 children completed the SAB questionnaire twice at a 2-week interval. The ICC for the parent questionnaire was 0.96, indicating a strong and significant correlation between the two administrations. Internal consistency reliability was calculated using Cronbach α for all participants. The Cronbach α coefficient was 0.92 for the parent questionnaire and 0.93 for the teacher questionnaire, demonstrating high internal consistency.
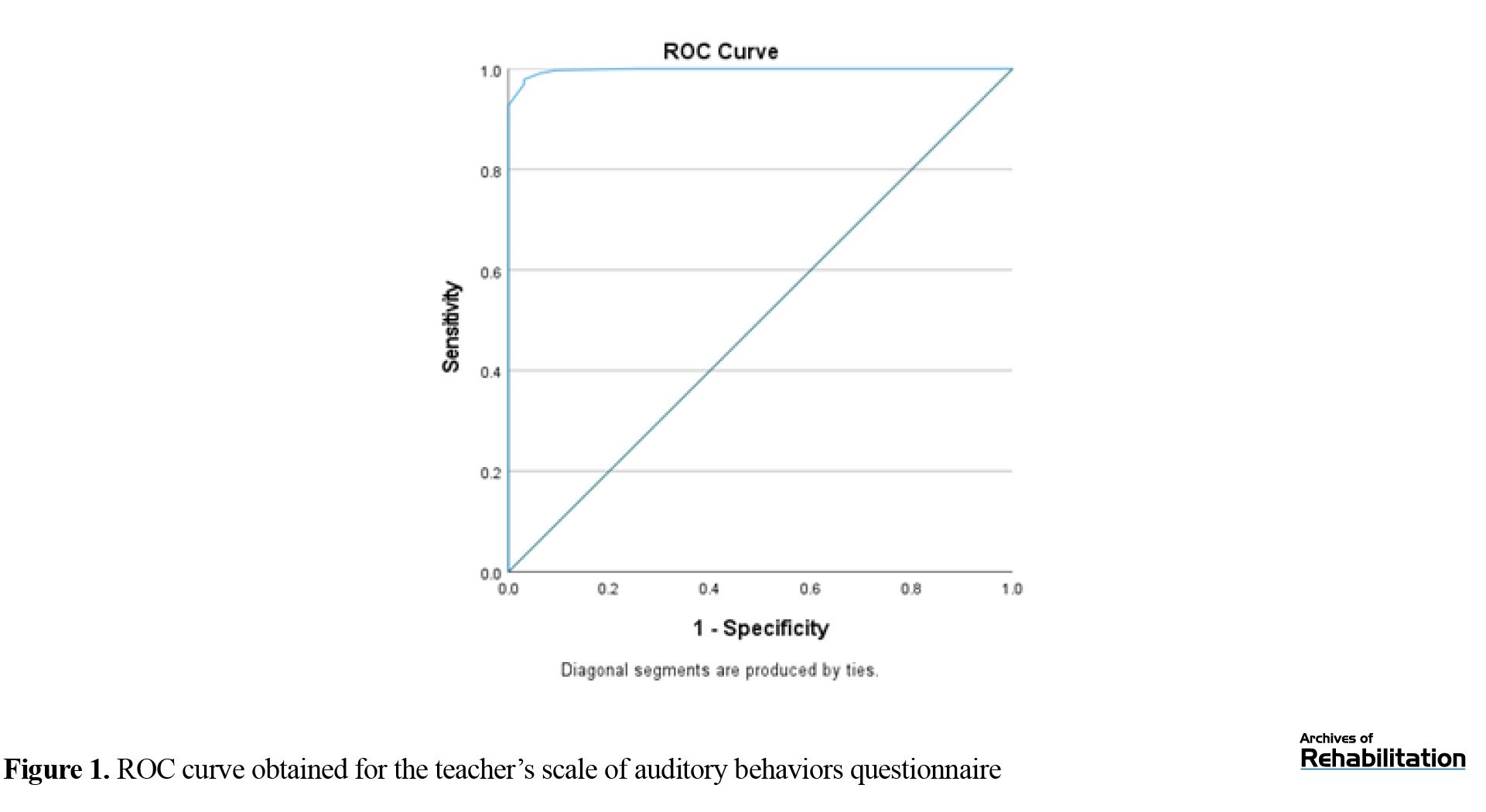
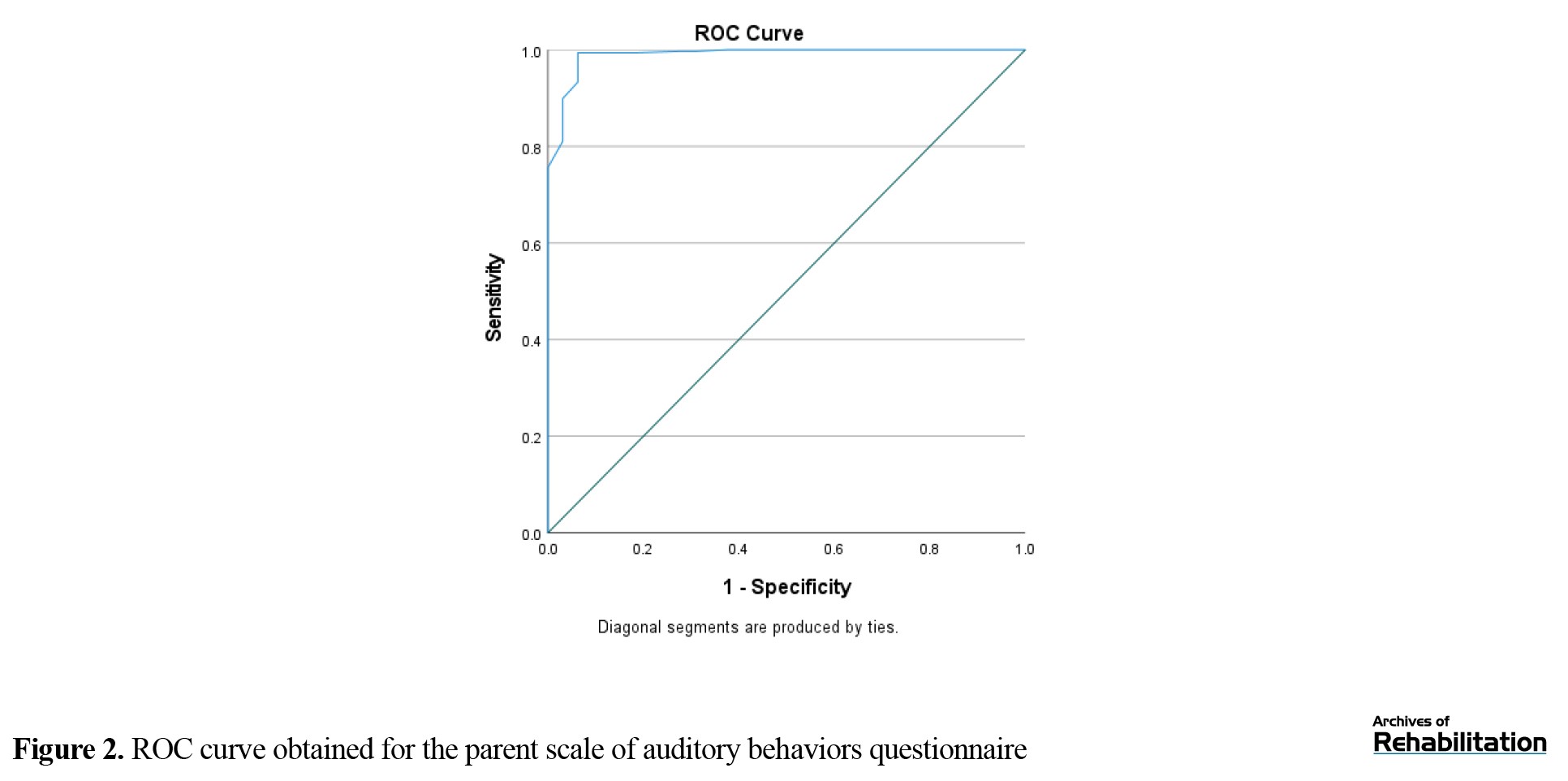
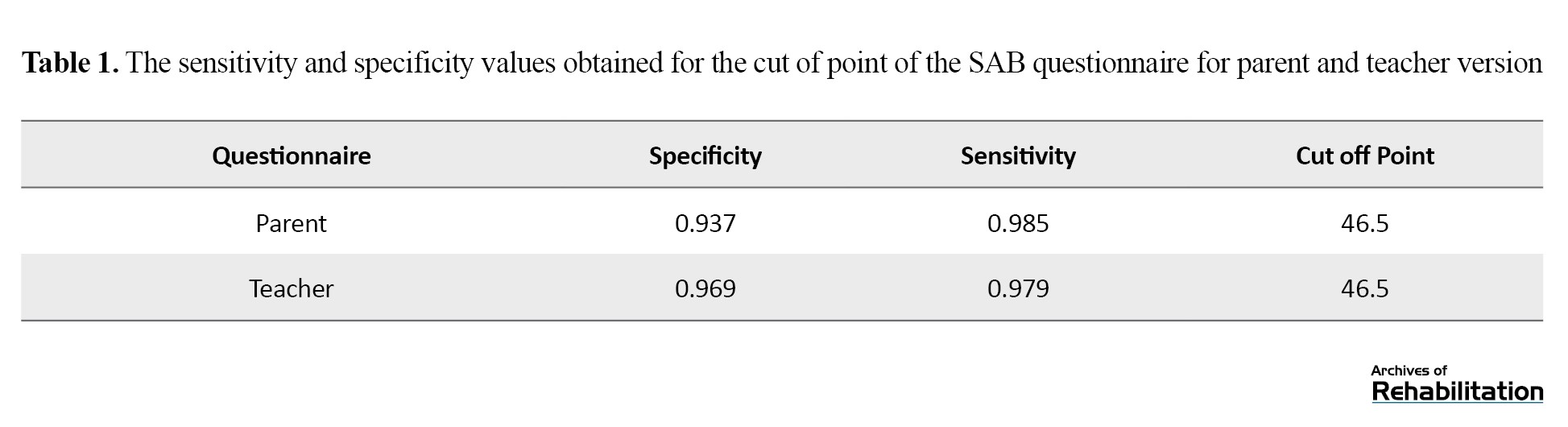
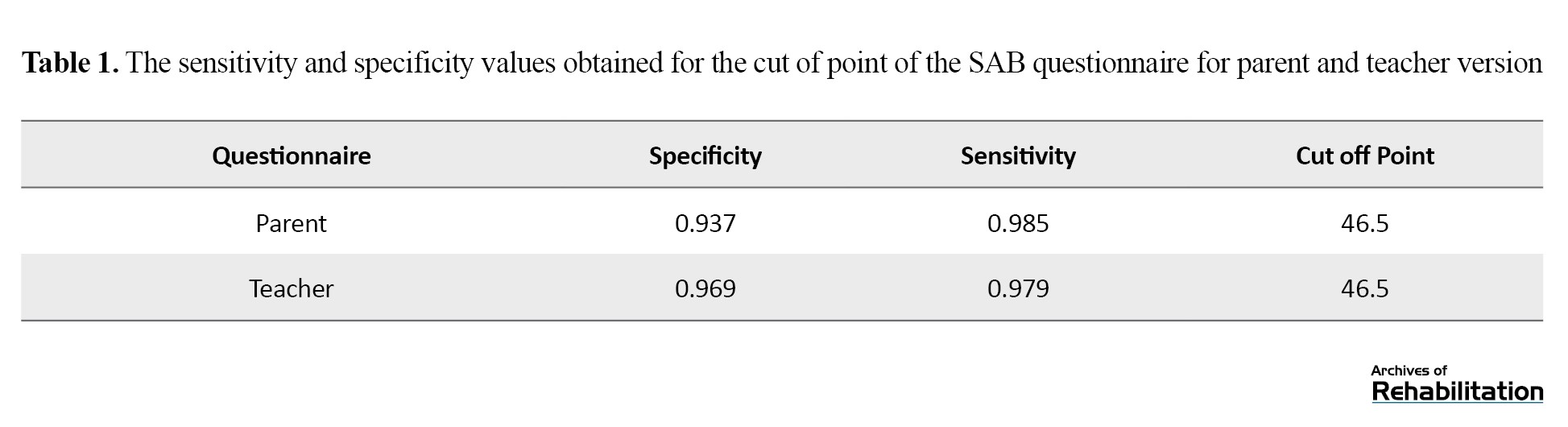
To determine the cut-off point, sensitivity, and specificity, a receiver operating characteristic (ROC) curve analysis was performed (Figure 1 and 2). The ROC curve plots sensitivity against the false-positive rate, with curves closer to the top-left corner of the graph indicating higher accuracy. The area under the ROC curve (AUC) for the teacher questionnaire scores was 99%. A cut-off score of 46 demonstrated 99% sensitivity and 94% specificity. Similarly, the AUC for the parent questionnaire scores with the same cut-off of 46 also showed 99% sensitivity and 94% specificity (Table 1).
The cut-off score of 46 for the Persian version of the SAB questionnaire is highly sensitive and specific, meaning that individuals scoring 46 or below are considered at risk for APD.
Discussion
This study developed the Persian version of the SAB questionnaire and performed statistical analyses to assess its validity and reliability. Initially, the SAB questionnaire was translated from English to Persian by experts proficient in English. The translated version was then reviewed by the target population and audiology specialists. After addressing ambiguities and confirming the face and content validity of the translated questionnaire, it was finalized for use in subsequent stages of the study. Based on the findings, the semantic, conceptual, and terminological consistency of the Persian version with the original SAB questionnaire was confirmed.
During the content validity assessment, specialists evaluated the necessity of each question in the Persian SAB. The content validity ratio exceeded the minimum acceptable value of 0.62. Additionally, the content validity index was assessed for relevance, clarity, and simplicity, with all indices scoring above 0.79, indicating the high content validity of the Persian SAB. Accordingly, the Persian questionnaire was developed methodically and adheres to international standards, maintaining clarity and alignment with the original version. Similar processes have been followed in developing Portuguese, Spanish, and Polish versions of the SAB [21, 25, 26].
Researchers have used different sets of auditory tests to validate the SAB questionnaire, all showing significant correlations [20, 21, 23, 25, 26]. Summers reported a mean score of 46 for children aged 8–12 years [20]. In the Polish version, the Mean±SD score was 46.6±9.02 [21]. The Spanish version, used in a population of Argentinian children aged 4–5, reported a Mean±SD score of 48.6±7.57 [2]. In the current study, the Mean±SD scores for the Persian SAB were 50.59±7.45 for the parent version and 49.68±6.79 for the teacher version.
Differential validity was assessed using the Fisher exact test, comparing questionnaire scores between the typical and APD groups. Statistical analyses confirmed significant differences between the two groups, demonstrating the translated questionnaire’s strong ability to differentiate individuals with APD from typical individuals. Using the ROC curve and the AUC, a cut-off score of 46 was determined for the Persian SAB, closely matching the cut-off values reported in the Portuguese, Spanish, and Polish versions [21, 25, 26].
Reliability was evaluated using intra-class correlation coefficient (ICC) and internal consistency. The ICC, calculated from repeated assessments, was 0.96, demonstrating high test re-test reliability. This aligns with findings from the Polish version, which reported an ICC of 93.2% [21]. Internal consistency, measured by the Cronbach α method, was 0.923 for the parent version and 0.933 for the teacher version in this study. The Portuguese and Polish versions also demonstrated high internal consistency, with Cronbach α values of 0.84 and 0.93, respectively [21, 26].
The results of this study indicate that the Persian SAB is a valid and reliable tool for screening ADPs. Clinically, the questionnaire enables specialists to gain insights into individuals with APD, facilitating quicker and more efficient identification of problems. The data collected can support diagnosis, further testing, and treatment planning.
Conclusion
The results indicated that the Persian version of this questionnaire is a reliable and valid tool that can be utilized as a non-invasive clinical and research instrument for differentiating children with ADPs.
The study was conducted in full compliance with all 31 ethical codes established by the Ministry of Health, Treatment, and Medical Education that are pertinent to this research, as detailed below:
General ethical codes: IR.USWR.REC.1401.220
1. Primary objective: The main goal of this study was to enhance human health while fully respecting the dignity and rights of individuals.
4. Risk considerations: Factors such as speed, ease, researcher convenience, lower cost, or simply the practicality of the study in no way placed the participants at risk or caused any additional harm.
8. Scientific rigor: The design and implementation of this research, which involved human subjects, conform to accepted scientific principles based on current knowledge and a comprehensive review of the available scientific literature and previous studies.
13. Informed consent: Informed consent was obtained from all study participants via a consent form before their involvement in the study procedures.
15. Transparency and withdrawal: The testing procedures and the roles of all individuals involved were explained fully and transparently. Participants were also informed that they could withdraw from the study at any time if they chose not to continue.
25. Confidentiality: Participants were assured that the personal information collected in the questionnaire would be used exclusively for this research and not for any other purpose.
27. Feedback on results: For those participants interested in knowing the outcomes, a summary of the research findings was provided upon request.
28. Accurate reporting: The results of the study will be published accurately, comprehensively, and honestly.
29. Rights of all parties: The reporting and announcement of the research outcomes will ensure that the material and intellectual rights of all relevant parties (participants, researchers, and the affiliated organization) are fully respected.
31. Cultural and social alignment: The research methodology does not conflict with the social, cultural, or religious values of the community.
Ethical codes for research involving vulnerable groups:
2. Focus on child health: The objective of the research was to advance knowledge regarding the health of infants and children, or to enhance the health and care provided to this group.
4. Consent for children: For children aged 7 to 15 years, written informed consent was obtained from their legal guardians. Additionally, following the child’s level of understanding, the child’s informed assent was also obtained. Children were given the right to receive appropriate information to the extent of their comprehension, to express their opinions, and to make decisions. The methods used to provide information and secure consent were tailored to the child’s age and cognitive capacity.
12. Therapeutic research justification: In therapeutic research, the balance between benefits and expected risks for the participants was carefully evaluated to ensure that the study was justified by the potential benefits to the subjects.
16. Minimizing distress: Given that the research involved questionnaires, whether via interviews or written surveys, care was taken to avoid inducing undue feelings of guilt, mistrust, or anxiety among the parents. Appropriate explanations were provided as part of the informed consent process.
17. Compensation and incentives: No financial compensation was provided to the children or their legal guardians for participating in the research; however, any expenses incurred as a result of participation were reimbursed. Moreover, providing small, low-value gifts (such as a small set of colored pencils, a pack of colored paper, or simple snacks) to the child participants was considered ethically acceptable and was encouraged.
18. Parental presence: Legal guardians had the right to accompany their child during the research process.
19. Opportunity for consultation: The children’s legal guardians were provided with sufficient opportunity to consult with relatives, healthcare providers, or independent advisors regarding participation in the study, should they wish to do so.
20. Addressing concerns: All questions and concerns raised by the children’s guardians during the study were answered appropriately.
21. Independent consent collection: Informed consent from both the child and the guardians was preferably obtained by individuals who were not part of the child’s treatment team.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethic Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1401.220).
Funding
Center for Pediatric Neuroscience Research funded this research.
Authors' contributions
Conceptualization: Mohanna Javan Bakht and Amir Abbas Ebrahimi; Methodology and analysis: Enayatollah Bakhshi; Validation, investigation, writing, project management, and funding: Reyhaneh Mahboudi; Supervision: Maryam Ramazani, Mohanna Javan Bakht, Amir Abbas Ebrahimi, and Enayatollah Bakhshi.
Conflict of interest
The authors declared no conflict of interest.
References
Auditory processing disorder (ADP) is a type of perceptual processing disorder involving auditory information in the central nervous system and its biological activities. Individuals with this disorder, despite having normal hearing thresholds and average intelligence, experience difficulties in processing auditory stimuli, particularly speech in the presence of environmental background noise [1]. Individuals with ADP exhibit poor auditory performance in environments with competing noise or highly reverberant settings struggle to follow verbal instructions effectively and face challenges in understanding rapid or degraded speech, especially in the presence of competing noise. Difficulties also arise in sound localization and directional hearing. Common issues include frequent requests for repetition or clarification, language impairments, difficulties in reading and pronunciation, challenges in telephone conversations, and an inability to detect subtle tonal changes essential for humor and sarcasm. These individuals often struggle to learn a foreign language or new verbal material, maintain attention, sing, or understand music. Educational challenges are also prevalent among subjects with ADP [2].
APD is observed across various populations, including children and adults [3]. Among children, due to their developmental stage and involvement in learning and education, it holds particular significance [4]. Studies estimate the prevalence of APD in school-aged children to range from 2% to 20% [5, 6, 7, 8, 9, 10]. Meanwhile, in Iran, the prevalence of suspected APD in children is reported around 9.8% [11]. In school-aged children in Tehran City, Iran, the prevalence is reported as 3.3% in girls, 3.8% in boys, and 4.6% overall [12]. Early identification and diagnosis of APD can significantly mitigate its adverse effects on children’s education and learning [13]. The diagnosis of APD varies significantly depending on the evaluation criteria and tools used [2]. Various disorders, such as attention deficit hyperactivity disorder (ADHD) and learning disabilities may present with similar clinical manifestations, necessitating precise diagnosis for effective management and treatment [14].
Currently, several tests and questionnaires are available for evaluating and diagnosing APD in children. Given the complexity of diagnosis and the importance of early intervention, screening is essential to refer children for comprehensive diagnostic tests. Screening tools help identify children needing further evaluation, differentiate APD from similar disorders, help in faster identification of ADP and thereby more effective interventions and minimize the negative impact on children and their families. Additional benefits of screening include reducing unnecessary referrals and prioritizing children for diagnostic evaluations, thus lowering overall clinical intervention costs and improving rehabilitation efficiency [15].
The screening phase typically involves questionnaires, behavioral tests, or a combination of both. Cost-effective and easily administered tools are essential for screening a wide population. Accordingly, questionnaires, in particular, offer practical and detailed information about individuals’ daily challenges and are considered a preferable first step compared to behavioral tests [16]. Current screening tools for APD include the Fisher’s auditory problems checklist, the children’s auditory processing performance scale, the scale of auditory behaviors (SABs), the auditory processing domain questionnaire, and the Buffalo model questionnaire [7, 8, 16]. In Iran, validated Persian versions of these tools include the auditory processing domain questionnaire, developed at Iran University of Medical Sciences in 2017 [12, 13], the Buffalo model questionnaire, developed at Tehran University of Medical Sciences in 2020 [17], and the Fisher’s checklist, developed at the University of Tehran in 2018 [18].
One comprehensive diagnostic test battery is the multiple auditory processing assessment (MAPA), which identifies and diagnoses APD early to expedite intervention [19]. Alongside MAPA, the SABs serves as a screening tool. The SAB was designed based on studies by Chermak (1998) and Shiffman (1999) to identify individuals with APD in conjunction with behavioral diagnostic tests [20].
It consists of 12 questions addressing listening-related behaviors, which reflect the behaviors that arise often in people with ADP and I rated on a scale from 1 (frequently) to 5 (never) by parents, teachers, or knowledgeable adults. Scores range from 12 to 60, with scores below 46 indicating a risk for APD in the original version. The SAB should be used alongside at least one subtest from the MAPA for functional assessment of results [21]. Considering the importance of questionnaires in APD screening, their ease of scoring by knowledgeable adults such as parents or teachers, high validity, and applicability in clinical research, the present study develops a Persian version of the SAB and determines its cutoff point, reliability, and validity.
Materials and Methods
In the initial phase, after obtaining permission from the creator of the SAB questionnaire, the translation process was conducted following the international protocol for quality-of-life assessment. The questionnaire was first translated into Persian by two bilingual translators fluent in English and experts in Persian. To ensure alignment with the original version, the translated questionnaire was back-translated into English by a third person, an English speaker fluent in Persian. The back-translated English version was then sent to the original author, and after their approval, the Persian translation was reviewed by audiology specialists working in the field of ADPs. These specialists evaluated the translation for standard quality, face validity, and content validity.
Based on their suggestions and the research team’s review, necessary modifications were applied to the questions. In the second phase, convenience sampling was employed to recruit 360 school-aged children from Tehran City and Shiraz City, Iran, whose parents provided informed consent; meanwhile, their medical history showed no evidence of neurological, psychological, or auditory problems. All children underwent otoscopy, audiometry, and tympanometry tests. Exclusion criteria were the lack of willingness by the child or parent to continue the study, inability to complete the tests, or loss of eligibility during the study. Based on these criteria, 32 children were diagnosed with APD, and 328 children were classified as typically developing for normative data calculation.
The participants underwent the following tests: Working memory assessment and the behavioral subtests of MAPA, including the monaural selective auditory attention test, dichotic digit test, and pitch pattern sequence test. The monaural selective auditory attention test assesses selective auditory attention in children. In this test, an engaging age-appropriate story is played, interspersed with some keywords (e.g. “point to the apple.”). The child is instructed to ignore the story and respond only to the keywords. The test consists of 25 items, each with six closed-set responses. A child distracted by the story fails to identify the target words. This test evaluates speech perception in noise and auditory selective attention [22]. The pitch pattern sequence test evaluates a child’s pattern recognition and frequency discrimination abilities. It includes 20 sets of high- and low-pitched tones presented in a specific order, which the child must reproduce in the same sequence [23].
The dichotic digit test includes four-digit sequences, with two digits presented simultaneously to each ear. The child repeats the numbers heard. This test is ideal for evaluating central auditory processing issues due to its high sensitivity, short duration (under 5 min), ease of administration, rapid scoring, low linguistic load, clear instructions, and tolerance of mild conductive or sensorineural hearing loss. Scoring is based on individual ear performance and interaural differences [24].
The participants were classified into APD and typically developing groups based on low scores in at least two of the three behavioral tests from the MAPA subtests. The SAB questionnaire was administered to parents and teachers (to eliminate bias) of both groups across four age categories as follows: 8–9, 9–10, 10–11, and 11–12 years. Questionnaire scores were compared with the MAPA results. Reliability was assessed using the test re-test method, calculating intra-class correlation coefficients (ICC). Internal consistency reliability was measured using the Cronbach α method. For this purpose, parents and teachers of 30 children completed the questionnaire again after a two-week interval, and the reliability of the questionnaire was analyzed.
Results
This study developed a Persian version of the SAB questionnaire and evaluated its validity and reliability to create a robust and reliable tool for screening children with APD and for clinical use. The statistical analysis of the results and related discussions are presented here.
The acceptable threshold for content validity ratio, based on the participation of 10 audiologists in the survey, is above 0.62. For the content validity index of each question, a value above 0.79 is considered acceptable. In this study, the necessity of each question in the Persian version of the SAB questionnaire was assessed by experts, and the content validity ratio exceeded the minimum threshold of 0.62. The average content validity index for the criteria of relevance, clarity, and simplicity of the Persian SAB questionnaire was 1.00, 0.99, and 0.99, respectively; values well above the 0.79 benchmark indicate strong content validity.
The Persian version of the SAB questionnaire was tested on a sample of 360 children aged 8 to 12 years, representing the largest psychometric analysis of this scale to date. The Mean±SD score for the parent version of the SAB was 50.59±7.45), while the teacher version had a Mean±SD score of 49.68±6.79). The gender distribution of the study participants is shown in Table 1.
In the present study, the scores of the SAB questionnaire in the teacher and parent versions were examined separately in different age groups and no significant difference was observed between the different groups. (P<0.05)
For discriminative validity and reliability assessment, 360 school-aged children were studied across four age groups (90 children per group): 8–9, 9–10, 10–11, and 11–12 years. The APD group included 32 children (15 girls and 17 boys), while the typically developing group included 328 children (165 girls and 163 boys). Scores from the parent and teacher versions of the SAB were divided into the APD and typically developing groups. To examine the relationship between SAB questionnaire results and the findings from the MAPA subtests, the chi-square test was employed.
In comparing the scores of the parent questionnaire, 30 out of 32 students with APD were correctly identified (93.8%), and 326 out of 328 typically developing students were accurately classified (99.3%). Similarly, for the teacher questionnaire, 30 out of 32 APD students were correctly identified (93.8%), while 325 out of 328 typically developing students were accurately classified (99.1%). Due to the low frequency of certain values and the fact that 25% of the data points were below 5, the Fisher exact test was used to assess the association or independence of the grouped scores. P for the teacher questionnaire were <0.001, indicating a significant relationship between the grouped questionnaire scores and the grouped results of the MAPA.
The strong correlation between the SAB questionnaire and MAPA results in the Persian version confirms their convergent validity and compatibility. To compare questionnaire scores across different age groups, a one-way analysis of variance was conducted, showing no significant differences between groups (P>0.05) (Table 2).
Test re-test reliability was assessed using ICC. The parents and teachers of 30 children completed the SAB questionnaire twice at a 2-week interval. The ICC for the parent questionnaire was 0.96, indicating a strong and significant correlation between the two administrations. Internal consistency reliability was calculated using Cronbach α for all participants. The Cronbach α coefficient was 0.92 for the parent questionnaire and 0.93 for the teacher questionnaire, demonstrating high internal consistency.
To determine the cut-off point, sensitivity, and specificity, a receiver operating characteristic (ROC) curve analysis was performed (Figure 1 and 2). The ROC curve plots sensitivity against the false-positive rate, with curves closer to the top-left corner of the graph indicating higher accuracy. The area under the ROC curve (AUC) for the teacher questionnaire scores was 99%. A cut-off score of 46 demonstrated 99% sensitivity and 94% specificity. Similarly, the AUC for the parent questionnaire scores with the same cut-off of 46 also showed 99% sensitivity and 94% specificity (Table 1).
The cut-off score of 46 for the Persian version of the SAB questionnaire is highly sensitive and specific, meaning that individuals scoring 46 or below are considered at risk for APD.
Discussion
This study developed the Persian version of the SAB questionnaire and performed statistical analyses to assess its validity and reliability. Initially, the SAB questionnaire was translated from English to Persian by experts proficient in English. The translated version was then reviewed by the target population and audiology specialists. After addressing ambiguities and confirming the face and content validity of the translated questionnaire, it was finalized for use in subsequent stages of the study. Based on the findings, the semantic, conceptual, and terminological consistency of the Persian version with the original SAB questionnaire was confirmed.
During the content validity assessment, specialists evaluated the necessity of each question in the Persian SAB. The content validity ratio exceeded the minimum acceptable value of 0.62. Additionally, the content validity index was assessed for relevance, clarity, and simplicity, with all indices scoring above 0.79, indicating the high content validity of the Persian SAB. Accordingly, the Persian questionnaire was developed methodically and adheres to international standards, maintaining clarity and alignment with the original version. Similar processes have been followed in developing Portuguese, Spanish, and Polish versions of the SAB [21, 25, 26].
Researchers have used different sets of auditory tests to validate the SAB questionnaire, all showing significant correlations [20, 21, 23, 25, 26]. Summers reported a mean score of 46 for children aged 8–12 years [20]. In the Polish version, the Mean±SD score was 46.6±9.02 [21]. The Spanish version, used in a population of Argentinian children aged 4–5, reported a Mean±SD score of 48.6±7.57 [2]. In the current study, the Mean±SD scores for the Persian SAB were 50.59±7.45 for the parent version and 49.68±6.79 for the teacher version.
Differential validity was assessed using the Fisher exact test, comparing questionnaire scores between the typical and APD groups. Statistical analyses confirmed significant differences between the two groups, demonstrating the translated questionnaire’s strong ability to differentiate individuals with APD from typical individuals. Using the ROC curve and the AUC, a cut-off score of 46 was determined for the Persian SAB, closely matching the cut-off values reported in the Portuguese, Spanish, and Polish versions [21, 25, 26].
Reliability was evaluated using intra-class correlation coefficient (ICC) and internal consistency. The ICC, calculated from repeated assessments, was 0.96, demonstrating high test re-test reliability. This aligns with findings from the Polish version, which reported an ICC of 93.2% [21]. Internal consistency, measured by the Cronbach α method, was 0.923 for the parent version and 0.933 for the teacher version in this study. The Portuguese and Polish versions also demonstrated high internal consistency, with Cronbach α values of 0.84 and 0.93, respectively [21, 26].
The results of this study indicate that the Persian SAB is a valid and reliable tool for screening ADPs. Clinically, the questionnaire enables specialists to gain insights into individuals with APD, facilitating quicker and more efficient identification of problems. The data collected can support diagnosis, further testing, and treatment planning.
Conclusion
The results indicated that the Persian version of this questionnaire is a reliable and valid tool that can be utilized as a non-invasive clinical and research instrument for differentiating children with ADPs.
The study was conducted in full compliance with all 31 ethical codes established by the Ministry of Health, Treatment, and Medical Education that are pertinent to this research, as detailed below:
General ethical codes: IR.USWR.REC.1401.220
1. Primary objective: The main goal of this study was to enhance human health while fully respecting the dignity and rights of individuals.
4. Risk considerations: Factors such as speed, ease, researcher convenience, lower cost, or simply the practicality of the study in no way placed the participants at risk or caused any additional harm.
8. Scientific rigor: The design and implementation of this research, which involved human subjects, conform to accepted scientific principles based on current knowledge and a comprehensive review of the available scientific literature and previous studies.
13. Informed consent: Informed consent was obtained from all study participants via a consent form before their involvement in the study procedures.
15. Transparency and withdrawal: The testing procedures and the roles of all individuals involved were explained fully and transparently. Participants were also informed that they could withdraw from the study at any time if they chose not to continue.
25. Confidentiality: Participants were assured that the personal information collected in the questionnaire would be used exclusively for this research and not for any other purpose.
27. Feedback on results: For those participants interested in knowing the outcomes, a summary of the research findings was provided upon request.
28. Accurate reporting: The results of the study will be published accurately, comprehensively, and honestly.
29. Rights of all parties: The reporting and announcement of the research outcomes will ensure that the material and intellectual rights of all relevant parties (participants, researchers, and the affiliated organization) are fully respected.
31. Cultural and social alignment: The research methodology does not conflict with the social, cultural, or religious values of the community.
Ethical codes for research involving vulnerable groups:
2. Focus on child health: The objective of the research was to advance knowledge regarding the health of infants and children, or to enhance the health and care provided to this group.
4. Consent for children: For children aged 7 to 15 years, written informed consent was obtained from their legal guardians. Additionally, following the child’s level of understanding, the child’s informed assent was also obtained. Children were given the right to receive appropriate information to the extent of their comprehension, to express their opinions, and to make decisions. The methods used to provide information and secure consent were tailored to the child’s age and cognitive capacity.
12. Therapeutic research justification: In therapeutic research, the balance between benefits and expected risks for the participants was carefully evaluated to ensure that the study was justified by the potential benefits to the subjects.
16. Minimizing distress: Given that the research involved questionnaires, whether via interviews or written surveys, care was taken to avoid inducing undue feelings of guilt, mistrust, or anxiety among the parents. Appropriate explanations were provided as part of the informed consent process.
17. Compensation and incentives: No financial compensation was provided to the children or their legal guardians for participating in the research; however, any expenses incurred as a result of participation were reimbursed. Moreover, providing small, low-value gifts (such as a small set of colored pencils, a pack of colored paper, or simple snacks) to the child participants was considered ethically acceptable and was encouraged.
18. Parental presence: Legal guardians had the right to accompany their child during the research process.
19. Opportunity for consultation: The children’s legal guardians were provided with sufficient opportunity to consult with relatives, healthcare providers, or independent advisors regarding participation in the study, should they wish to do so.
20. Addressing concerns: All questions and concerns raised by the children’s guardians during the study were answered appropriately.
21. Independent consent collection: Informed consent from both the child and the guardians was preferably obtained by individuals who were not part of the child’s treatment team.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethic Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1401.220).
Funding
Center for Pediatric Neuroscience Research funded this research.
Authors' contributions
Conceptualization: Mohanna Javan Bakht and Amir Abbas Ebrahimi; Methodology and analysis: Enayatollah Bakhshi; Validation, investigation, writing, project management, and funding: Reyhaneh Mahboudi; Supervision: Maryam Ramazani, Mohanna Javan Bakht, Amir Abbas Ebrahimi, and Enayatollah Bakhshi.
Conflict of interest
The authors declared no conflict of interest.
References
- Arabi A, Mehrkian S, Mirzaei H, Bakhshi E. Comparing auditory sustained attention in children with auditory processing disorder and normal children. Koomesh. 2020; 22(4):650-4. [Link]
- American Speech-Language-Hearing Association. American Speech-Language-Hearing Association Practice Policy. Maryland: American Speech-Language-Hearing Association; 2005. [Link]
- Musiek FE, Baran JA, Bellis TJ, Chermak GD, Hall JW, Keith RW, et al. Guidelines for the Diagnosis, Treatment and Management of Children and Adults with Central Auditory Processing Disorder. American Academy of Audiology. 2010; 1-51. [Link]
- Rockville M. Auditory processing disorders working group on auditory processing disorders. American Speech-Language Hearing Association. 2005. [Link]
- Bamiou DE, Musiek FE, Luxon LM. Aetiology and clinical presentations of auditory processing disorders--a review. Archives of Disease in Childhood. 2001; 85(5):361-5. [DOI:10.1136/adc.85.5.361] [PMID]
- O’Hara B, Mealings K. Developing the auditory processing domains questionnaire (APDQ): A differential screening tool for auditory processing disorder. International Journal of Audiology. 2018; 57(10):764-75. [DOI:10.1080/14992027.2018.1487087] [PMID]
- Jerger J, Musiek F. Report of the Consensus Conference on the Diagnosis of Auditory Processing Disorders in School-Aged Children. Journal of the American Academy of Audiology. 2000; 11(9):467-74. [DOI:10.1055/s-0042-1748136] [PMID]
- Katz J, Chasin M, Kristina M, Hood LJ, Tillery KL. Handbook of clinical audiology. Philadelphia: Wolters Kluwer Health; 2015. [Link]
- Schow RL, Seikel JA, Chermak GD, Berent M. Central auditory processes and test measures: ASHA 1996 revisited. American Journal of Audiology. 2000; 9(2):63-8. [DOI:10.1044/1059-0889(2000/013)] [PMID]
- Cacace AT, McFarland DJ. Central auditory processing disorder in school-aged children: A critical review. Journal of Speech, Language, and Hearing Research. 1998; 41(2):355-73. [DOI:10.1044/jslhr.4102.355] [PMID]
- Arezou M, Masoumeh R, Nariman R, Hasan S. Estimation of the referral rate of suspected cases of central auditory processing disorders in children aged 8-12 years old in Oshnavieh, Western Iran, based on auditory processing domain questionnaire and speech in noise and dichotic digit tests. Auditory and Vestibular Research. 2018; 27(3):164-70. [Link]
- Jarollahi F, Pourbakht A, Jalaie S, Oruie M. Screening of auditory processing disorders in school- aged children in Tehran, Iran using the Auditory Processing Domain Questionnaire. Auditory and Vestibular Research. 2022; 31(1):17-22. [Link]
- Ahmadi Z, Jarollahi F, Ahadi M, Hosseini AF. Normalization and validation of Auditory Processing Domain Questionnaire in normal 8-12 year-old children. Auditory and Vestibular Research. 2017; 26(2):93-8. [Link]
- Geffner D, Ross-Swain D. Auditory processing disorders: Assessment, management, and treatment. San Diego: Plural Publishing, Incorporated; 2017. [Link]
- Sanchez L, Lam E. Evaluation of screening instruments for auditory processing disorder (APD) in a sample of referred children. Australian and New Zealand Journal of Audiology, The. 2007; 29(1):26-39. [Link]
- Musiek FE, Chermak GD. Handbook of central auditory processing disorder, volume I: Auditory neuroscience and diagnosis. California: Plural Publishing; 2013. [Link]
- Negin E, Farahani S, Babaei S, Faryadras R, Barootiyan SS. Cross-cultural adaptation and determining validity and reliability of the Persian revised Buffalo model questionnaire. Auditory and Vestibular Research. 2020; 29(3):178-85. [Link]
- Shakiba S, Rouhbakhsh N, Mohammadkhani Q, Abdollahi FZ, Zadeh EF. Translation, validity, and reliability of the persian version of the fisher auditory problems checklist. Journal of Modern Rehabilitation. 2018; 12(3):169-80. [DOI:10.32598/JMR.V12.N3.169]
- Domitz DM, Schow RL. A new CAPD battery-multiple auditory processing assessment: factor analysis and comparisons with SCAN. American Journal of Audiology. 2000; 9(2):101-11. [DOI:10.1044/1059-0889(2000/012)] [PMID]
- Summers SA. Factor structure, correlations, and mean data on Form A of the Beta III version of Multiple Auditory Processing Assessment (MAPA)[PhD dissertation]. Pocatello: Idaho State University; 2003. [Link]
- Skarżyński H, Bieńkowska K, Gos E, Skarżyński PH, Grudzień D, Czajka N, et al. Cross-Cultural Adaptation of the Scale of Auditory Behaviors Questionnaire. Language, Speech, and Hearing Services in Schools. 2019; 50(4):683-92. [DOI:10.1044/2019_LSHSS-19-0014] [PMID]
- Aarabi S, Jarollahi F, Jalaie S. Development and determination of the validity of Persian version of monaural selective auditory attention test in learning disabled children. Auditory and Vestibular Research. 2016; 25(1):49-54. [Link]
- Schow RL, Whitaker MM, Seikel JA, Brockett JE, Domitz Vieira DM. Validity of the Multiple Auditory Processing Assessment-2: A test of auditory processing disorder. Language, Speech, and Hearing Services in Schools. 2020; 51(4):993-1006. [DOI:10.1044/2020_LSHSS-20-00001] [PMID]
- Carvalho NG, Ubiali T, Amaral MIRD, Colella-Santos MF. Procedures for central auditory processing screening in schoolchildren. Brazilian Journal of Otorhinolaryngology. 2019; 85(3):319-28. [DOI:10.1016/j.bjorl.2018.02.004] [PMID]
- Nunes CL, Pereira LD, Carvalho GS. Scale of Auditory Behaviors and auditory behavior tests for auditory processing assessment in Portuguese children. CoDAS. 2013; 25(3):209-15. [PMID]
- Miranda AR, Bruera JA, Serra SV. Scale of auditory behaviors: Normative reference values for healthy Argentinian children. ACTA Neuropsychologica. 2017; 15(2):119. [DOI:10.5604/01.3001.0010.2403]
Type of Study: Original |
Subject:
Audiometery
Received: 2/07/2024 | Accepted: 4/01/2025 | Published: 1/04/2025
Received: 2/07/2024 | Accepted: 4/01/2025 | Published: 1/04/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |