Volume 25, Issue 4 (Winter 2025)
jrehab 2025, 25(4): 864-889 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mavaeian Z, Mir S M, Shadmehr A, Malmir K. The Effect of Core Stabilization Exercises Compared to Balance Training on Proprioception and Dynamic Balance in Healthy Female Amateur Soccer Players: A Randomized Controlled Trial. jrehab 2025; 25 (4) :864-889
URL: http://rehabilitationj.uswr.ac.ir/article-1-3461-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3461-en.html
1- Department of Physical Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran. , mavaeianzahra93@gmail.com
2- Department of Physical Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran., Tehran
3- Department of Physical Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Physical Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran., Tehran
3- Department of Physical Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran.
Keywords: Core stabilization training, Balance training, Proprioception, Dynamic balance, Female athlete, Futsal
Full-Text [PDF 4143 kb]
(833 Downloads)
| Abstract (HTML) (5986 Views)
Full-Text: (1243 Views)
Introduction
Women are more likely to be injured in sports than men due to their anatomical, hormonal, biomechanical, and neuromuscular differences [1]. Factors that raise the possibility of sports injuries generally include proprioceptive disorder, scar tissue formation, and pathological variations in joint range of motion [2]. In these cases, proprioception is crucial because it protects against movement injuries and plays a role in establishing joint constancy and natural coordination of movements [3، 4]. Joint position sense is a subset of proprioception, involving the awareness and ability to reconstruct the angle of a joint after movement [5, 6]. Proprioception plays a big part in the awareness and unawareness of the senses, spontaneous detection of movements, coordination and learning of movement, posture, and balance [5]. Soccer players need a significant dynamic balance to act rightly and reduce the risk of injury during fast and cutting movements. The capability to maintain body stability while standing is called static balance, and while moving, it is called dynamic balance. Dynamic balance involves some degree of predictable movement near the center of gravity [7-9]. There are a few points in this regard. Among different sports, soccer is one of the most risky sports [10] as this sport is called “knee injury disease” [11]. Proprioception becomes more important in athletes, especially soccer players because the highest level of performance is expected from them [12]. Among the joints of the human body, the knee is one of the richest joints with proprioceptive receptors, and has the extensor and flexor muscles, which are the largest in the body, also have the largest number of muscle spindles [13].
Physiotherapists are searching for effective ways to return joint proprioception to a normal state to provide optimal stability and mobility in static and dynamic situations. Proprioception can be influenced by various factors, including age, injuries, diseases, and physical activity [14]. No definite therapeutic exercise method currently improves proprioception [15, 16]. Still, several exercises have been suggested to improve proprioception, such as balance training (BT) [14], closed chain exercises, plyometric, and core stability training (CST) [9, 17]. Hübscher stated in his study that more comparative studies should be conducted to determine the best exercises to reduce the risk of injury in different sports [18]. In the past, numerous studies have demonstrated that CST has an impressive role in enhancing athletic efficiency, progressing balance, and decreasing the risk of sports injuries [19, 20]. Despite the importance of proprioception, very few studies have evaluated the effect of CST on proprioception, and most of the effects of BT or a combination of exercises on improving proprioception have been researched. Despite the theoretical advantages proposed for each exercise, few studies have compared these methods. Additionally, there is not enough information about the most effective training method and the benefits of each training alone. Therefore, this research was conducted to compare the impact of CST with BT, which is more commonly used to improve proprioception. Considering that no research has been done to compare the consequence of CST and BT on knee proprioception in female soccer players, this study aims to determine the impact of these two exercise methods on knee proprioception and dynamic balance of healthy female athletes and also to compare the effects of these exercises with each other.
Materials and Methods
Trial Design
The design of this research was an interventional study.
Blinding
This research was single-blinded (participants were blind to the type of intervention of their training group).
Sample Size
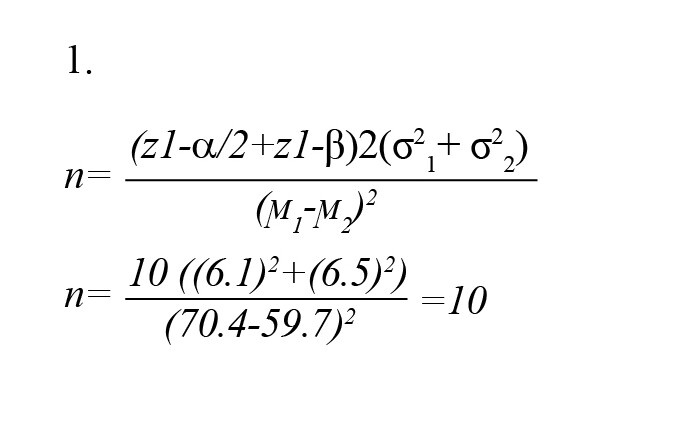
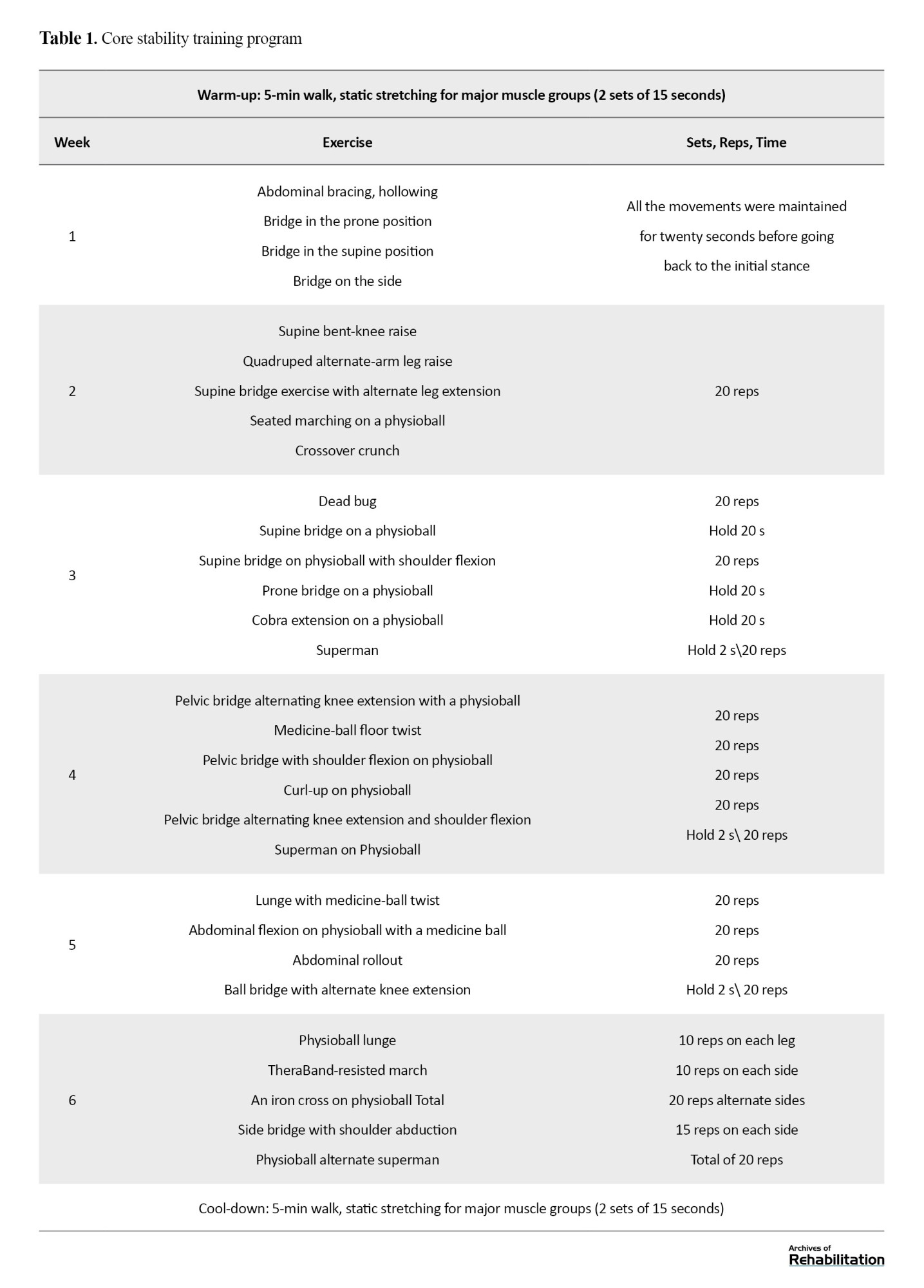
A comparison equation of averages was used to conduct a sample calculation to determine the sample size. The equation originated from the mean reach distance assessed in the star excursion balance test (SEBT) as part of the data in Filipa et al.’s research [20]. The mean difference for improvement was 10%, and the standard deviation was 7.5%. A significance level 0.05 was adopted, and the correlation power was set at 80% [21]. Thus, the sample consisted of 10 women in each group (Equation 1).
Study Participants
After permission from the Ethics Committee (IR.TUMS.FNM.REC.1399.012), 20 female soccer athletes completed the study. Most participants were selected from the female athletes participating in the sports complexes and volunteered to participate in this study. For inclusion in the study, athletes had to meet the following criteria: female gender, aged between 20 and 30 years, and participating in an unprofessional level of soccer [16]. The exclusion criteria were as follows: having had lower limb or lumbar-spine problems or had an operation in the last half year; experienced neurological, vestibular, or visual disorders within the previous 6 months; were presently participating in another training program; did not finish the interventions and evaluations; or attended less than 80% of the exercise meetings (16 out of 18 sessions) [21].
Randomization
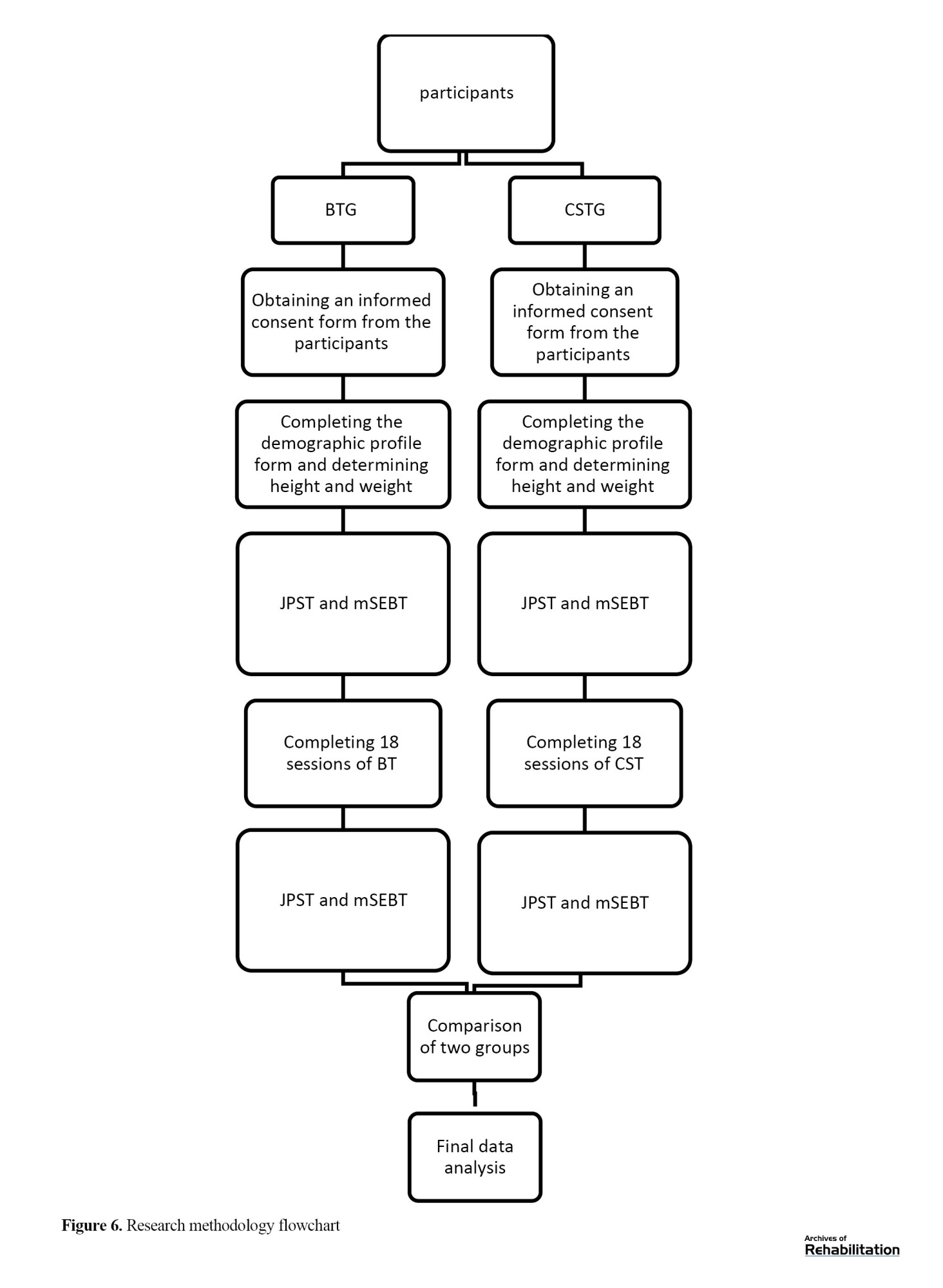
The subjects were split into two groups utilizing the sealed envelope technique: 10 in the core stabilization training group (CSTG) and 10 in the balance training group (BTG). A summary of the research objectives was presented to participants, and they signed the informed consent form.
Outcome Measures
Information regarding the participant’s age, height, weight, and leg length were gathered. Knee proprioception was measured by using the joint position sense test (JPST) [9], and dynamic balance was measured by using the modified star excursion balance test (mSEBT) one week before and immediately after the 6-week interventions [22].
Intervention
The subjects completed the CST or BT program three times a week. They practiced on the days that were part of their regular schedule. The training program lasted around 30 minutes per session for 6 weeks, totaling 18 sessions. Considering that the participants in this study were blind, they performed the exercises separately and under the supervision of the physiotherapist.
The Core Stability Training Program
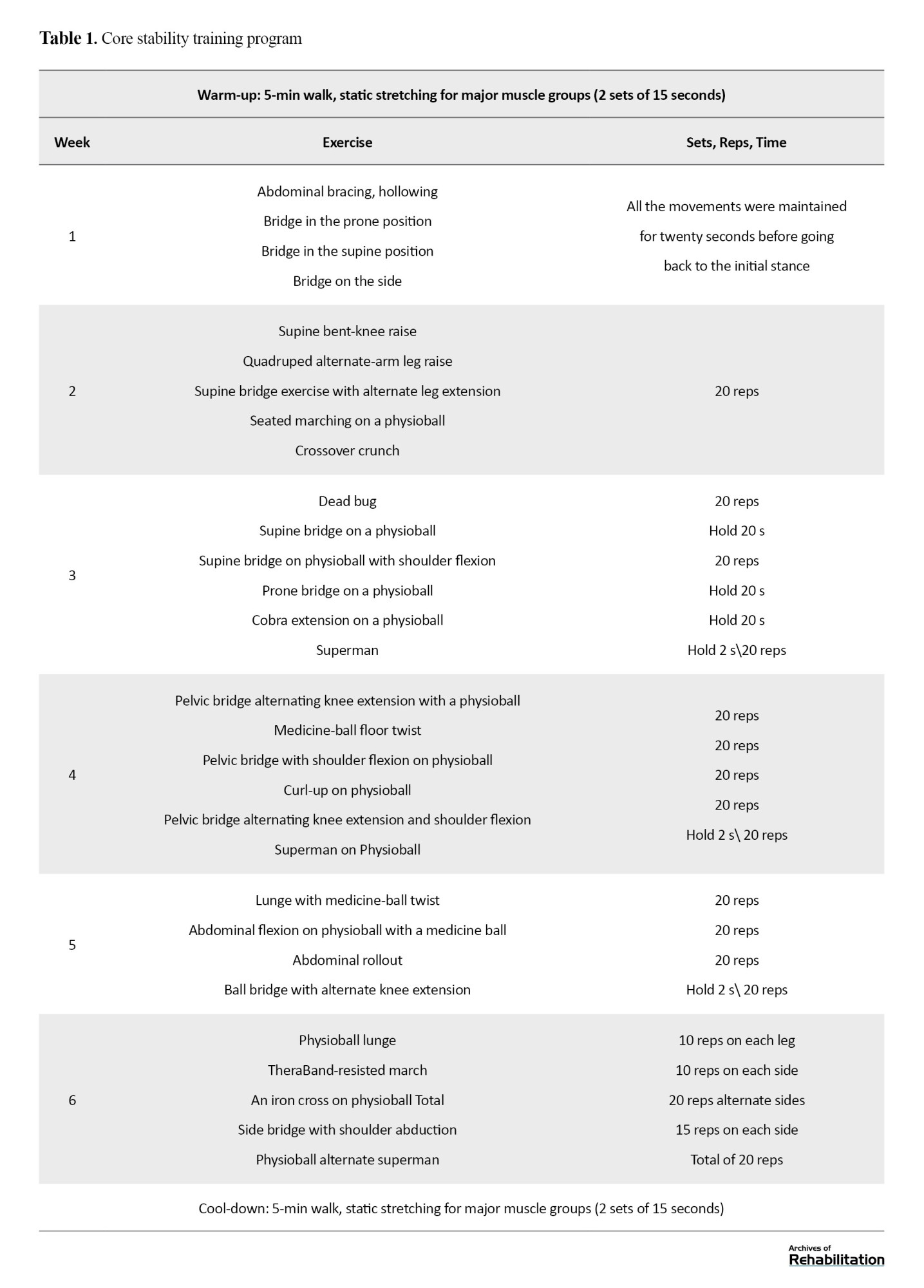
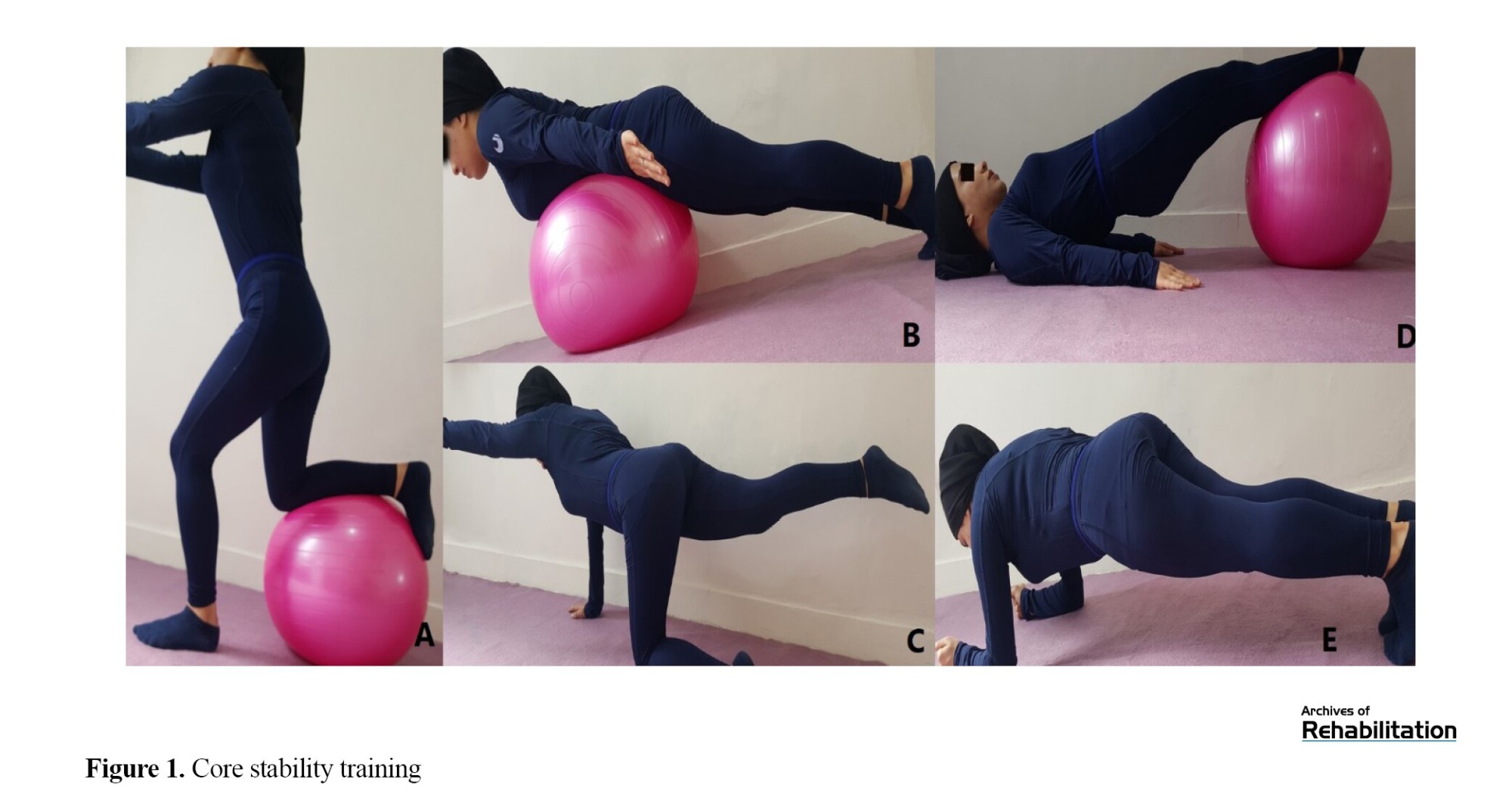
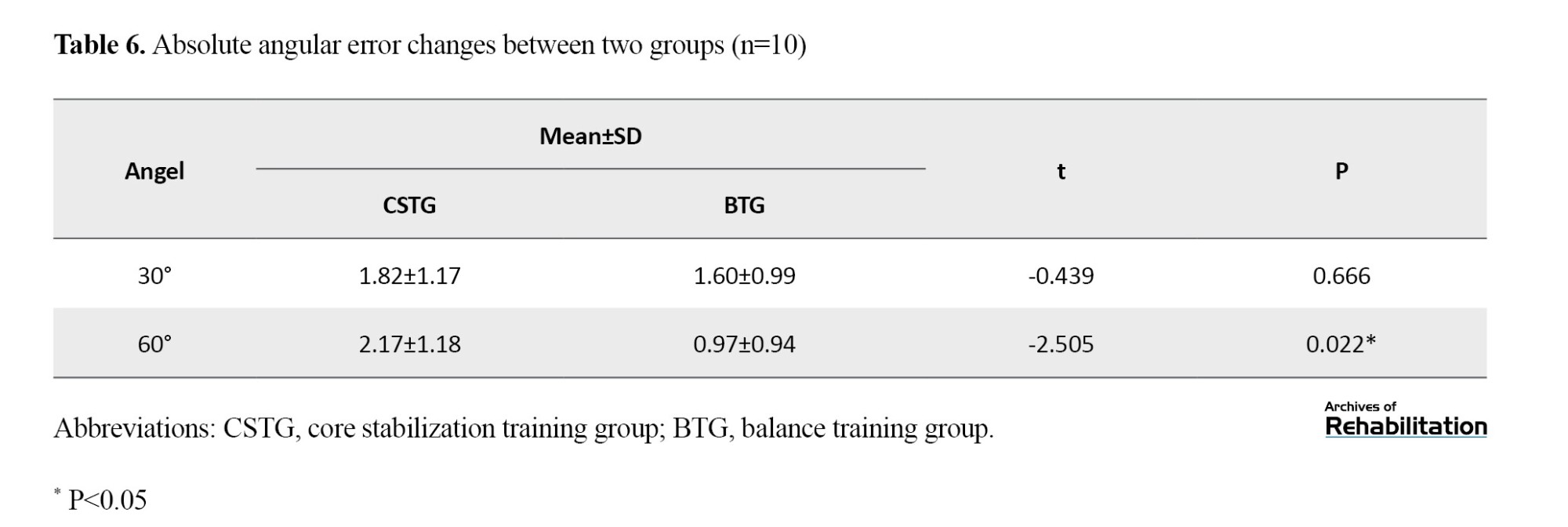
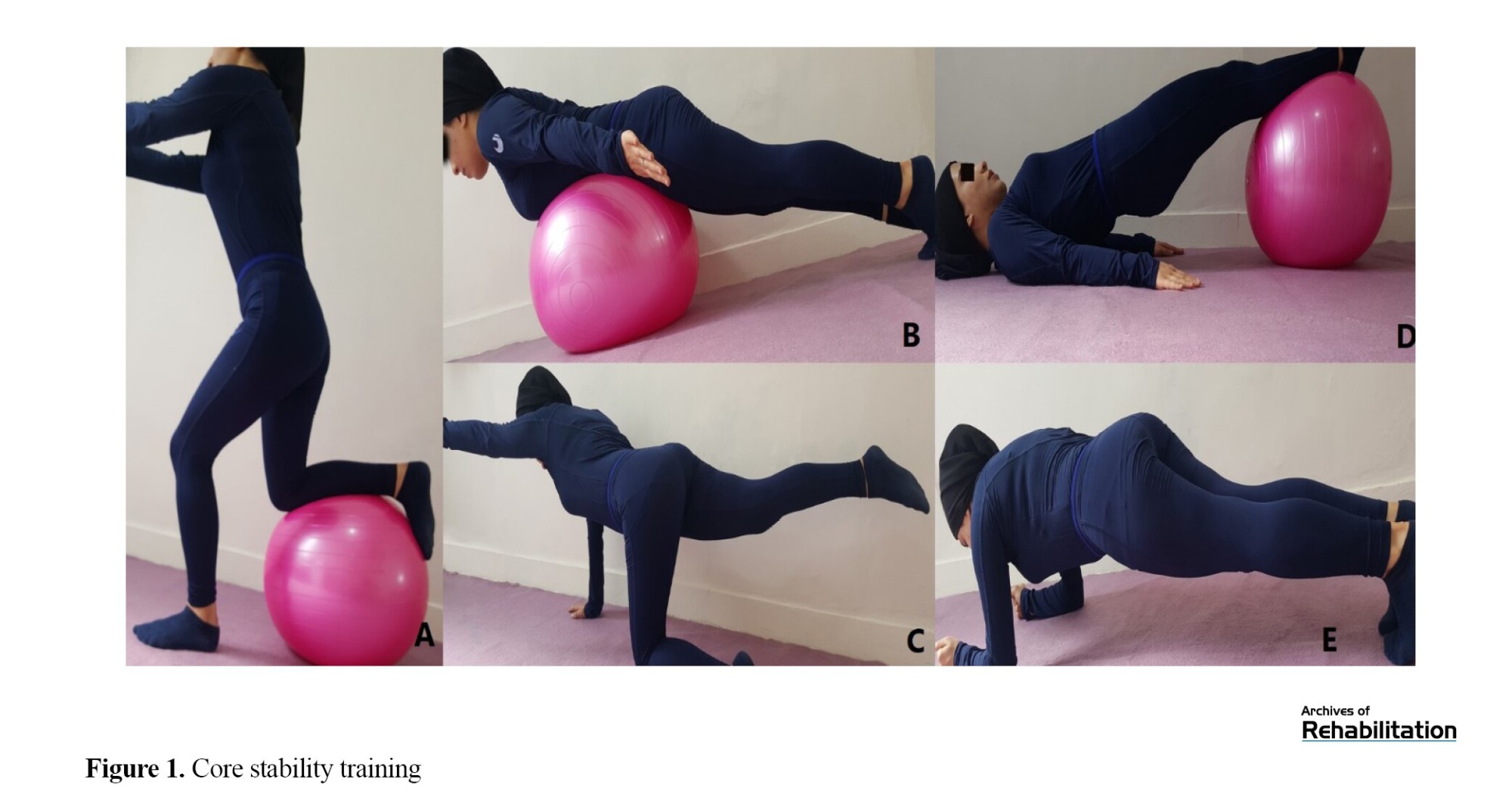
The participants engaged in a six-week exercise program with the investigator, meeting thrice weekly for up to half an hour. The CST program comprises three exercises designed to increase the trunk muscles’ power and enhance neuromuscular coordination [23-26]. The CST program protocol is based on the training program set in Jeffreys’ research [27]. The exercise program had three levels, each with different types of exercises. The first level involved stationary exercises, then low motions in an unsteady setting were achieved gradually. Participants in the second level engaged in stationary contractions in an unsteady setting and transitioned to active motions in a steadier environment. In the third level, participants performed motion on uneven surfaces while also incorporating resistance. The type of exercises was changed and improved every week, and each training session was 30 minutes long. The session began with a 10-minute warm-up, including a 5-minute walk and static stretching for the major muscle groups. Despite learning new activities each week, specific exercises built upon the previous weeks by incorporating a new action or changing the surface [22]. The protocol is described in Table 1 in the attachment and is shown in Figure 1.
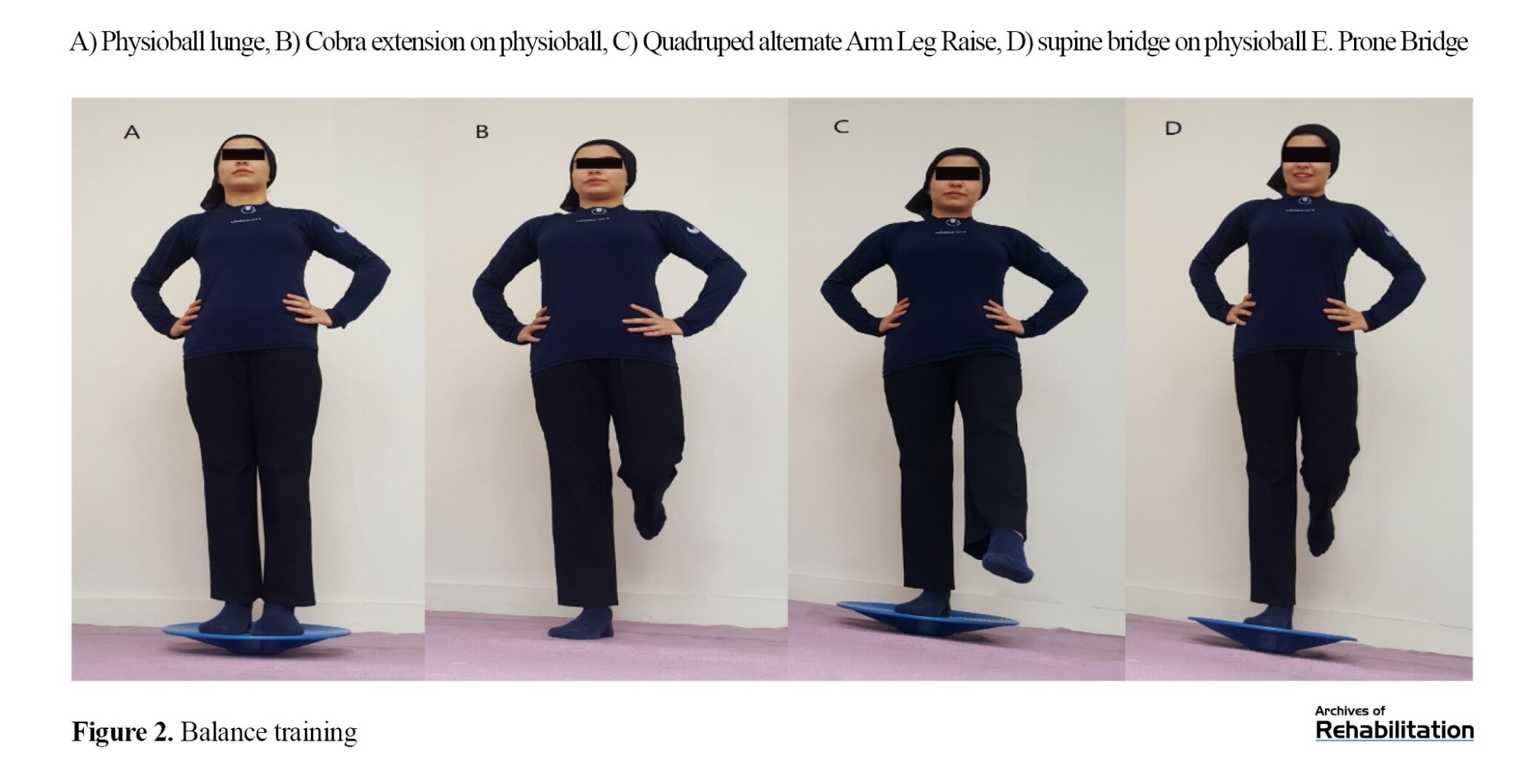
Balance Training Program
The program involved three weekly sessions and was designed based on scientifically validated BT protocols from previous studies [28]. The program consisted of a 5-phase BT approach, with details outlined in Figure 2 and Table 2.
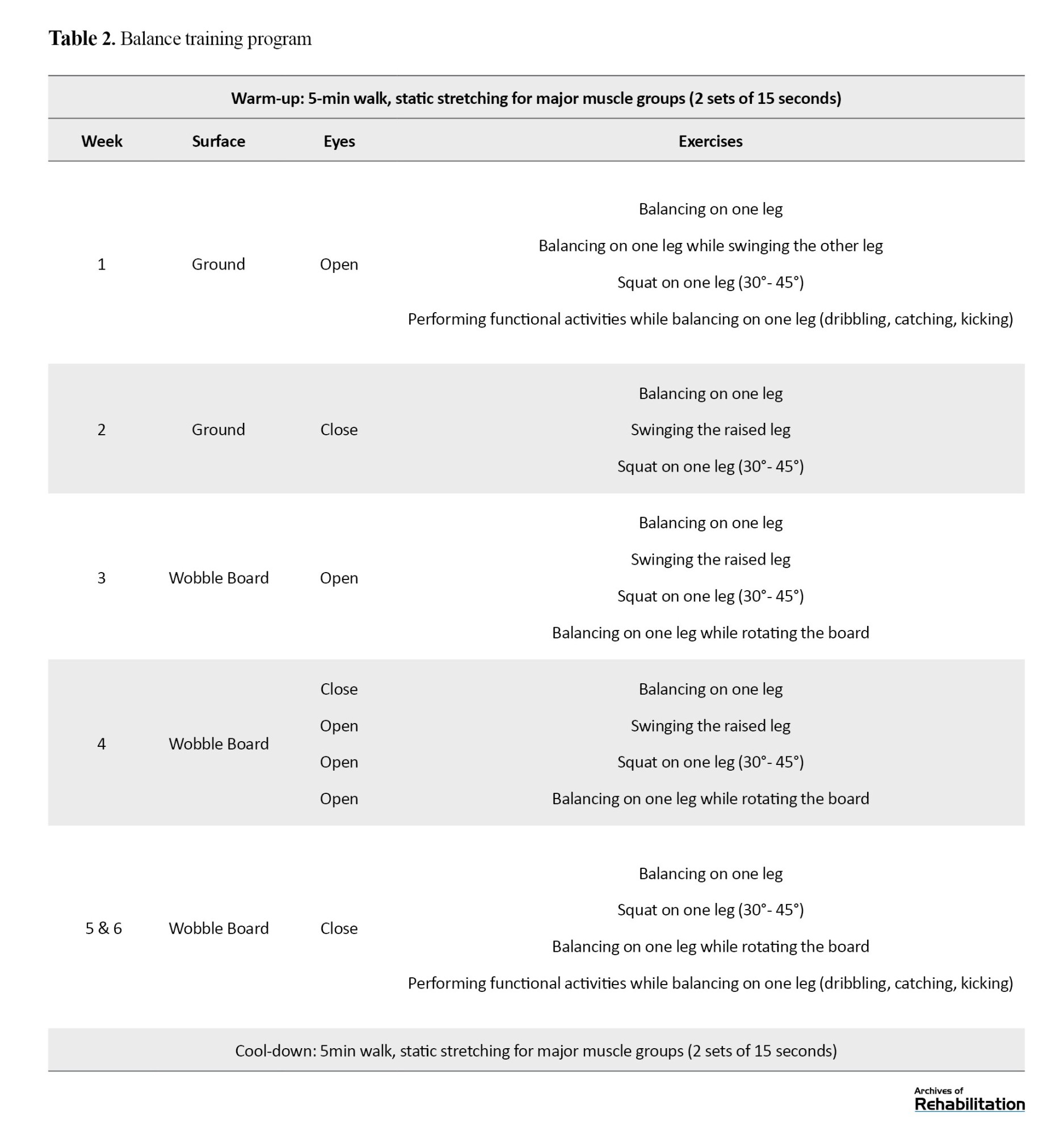
During each phase, exercises were carried out for up to half a minute, and there was a half-minute rest interval between each exercise. The exercises were improved every week. The difficulty of the exercises was changed by opening and closing the eyes and doing the exercise on the floor or wobbleboard. The protocol of these exercises in the first week was that the person maintained her balance on one leg while using her sense of sight and standing on the ground. Progress was made to the point that in the sixth week, balance exercises were performed by standing on one leg on the balance board with eyes closed and functional movements of the upper leg. All exercises were performed for up to 30 seconds during all phases, with 30 seconds of rest in between, during which the legs were alternated [28].
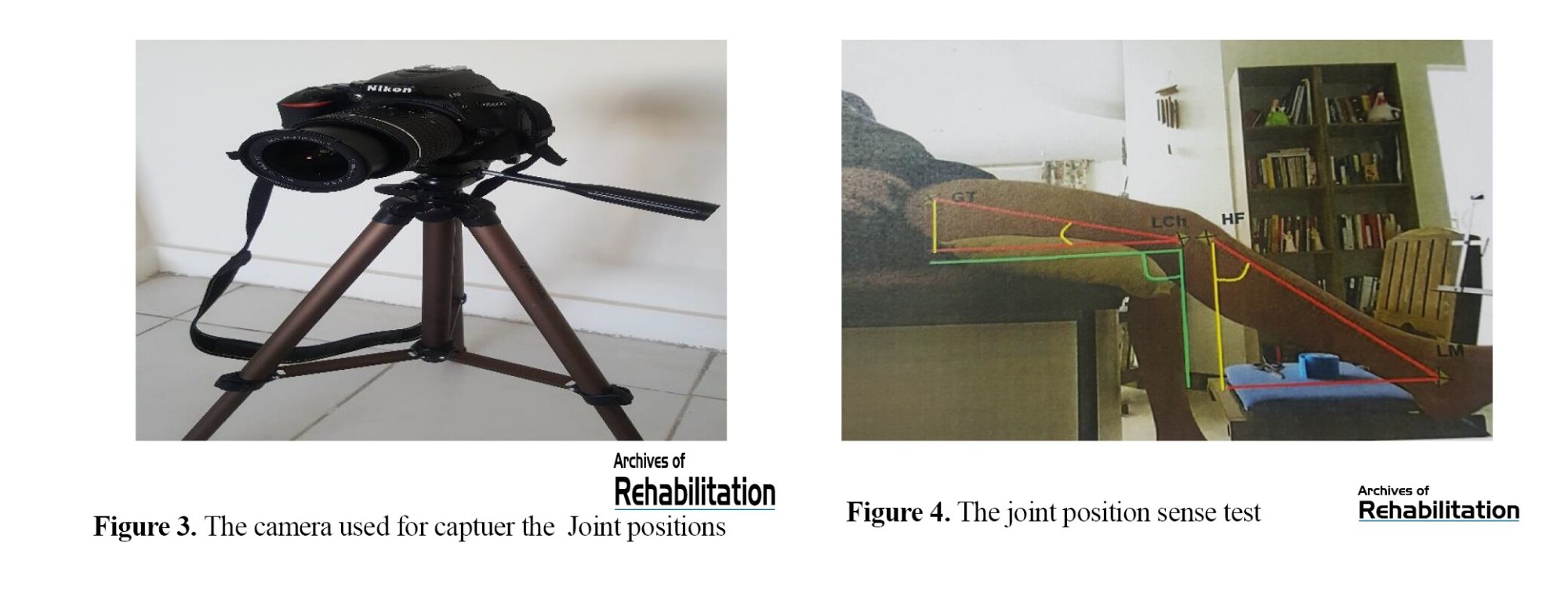
Proprioception Test
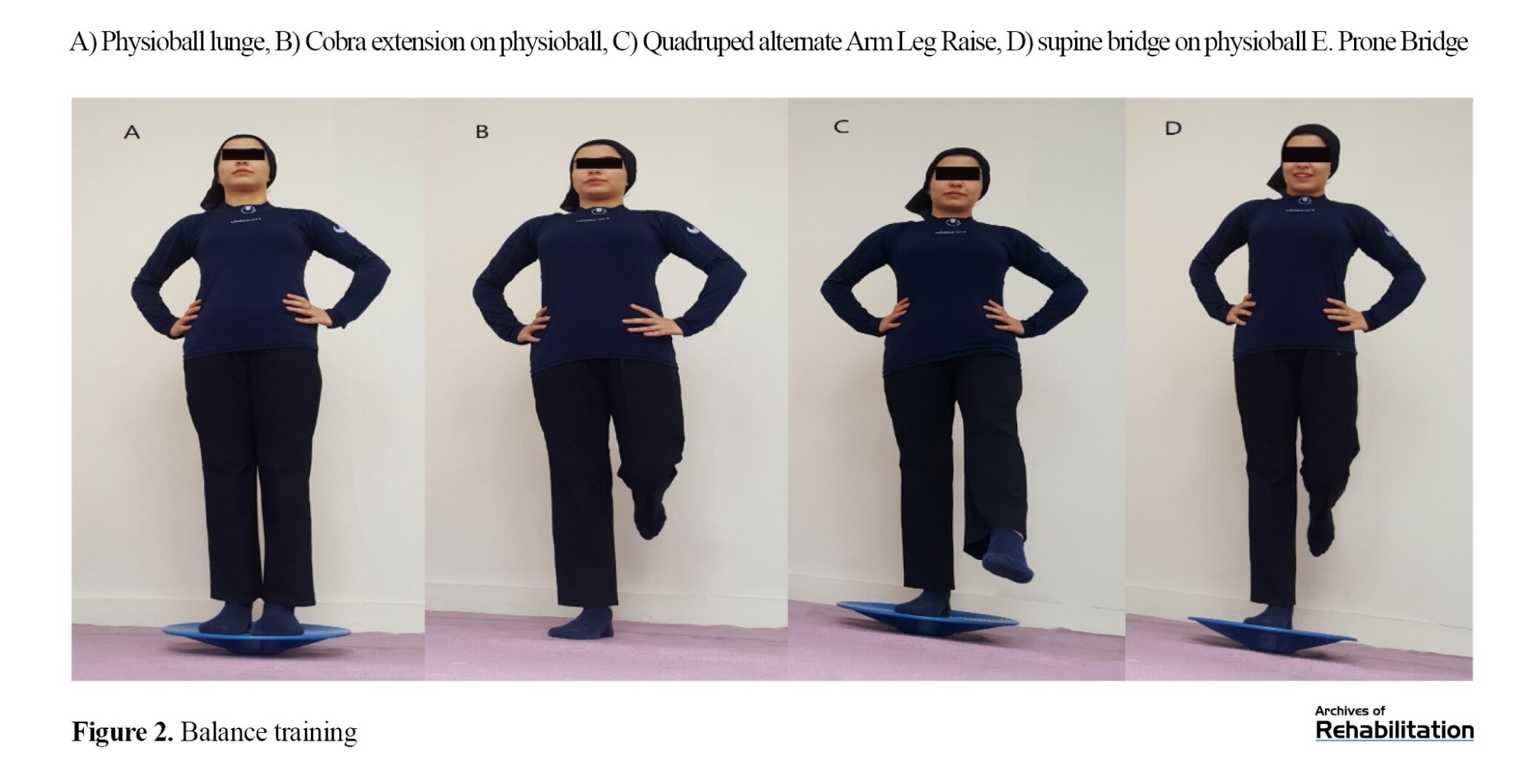
To measure knee joint position sense, the error rate in the JPST was evaluated using skin markers, digital photography, and ImageJ software .[9] A previous study showed an intraclass correlation coefficient (ICC) of 0.910 for this method of JPS assessment [29]. Nikon’s 24-megapixel digital camera model D5600 was used to take photographs of the joint positions in this study (Figure 3). Before starting the assessments, the reliability of this digital camera was assessed by computing ICC= 0.99.
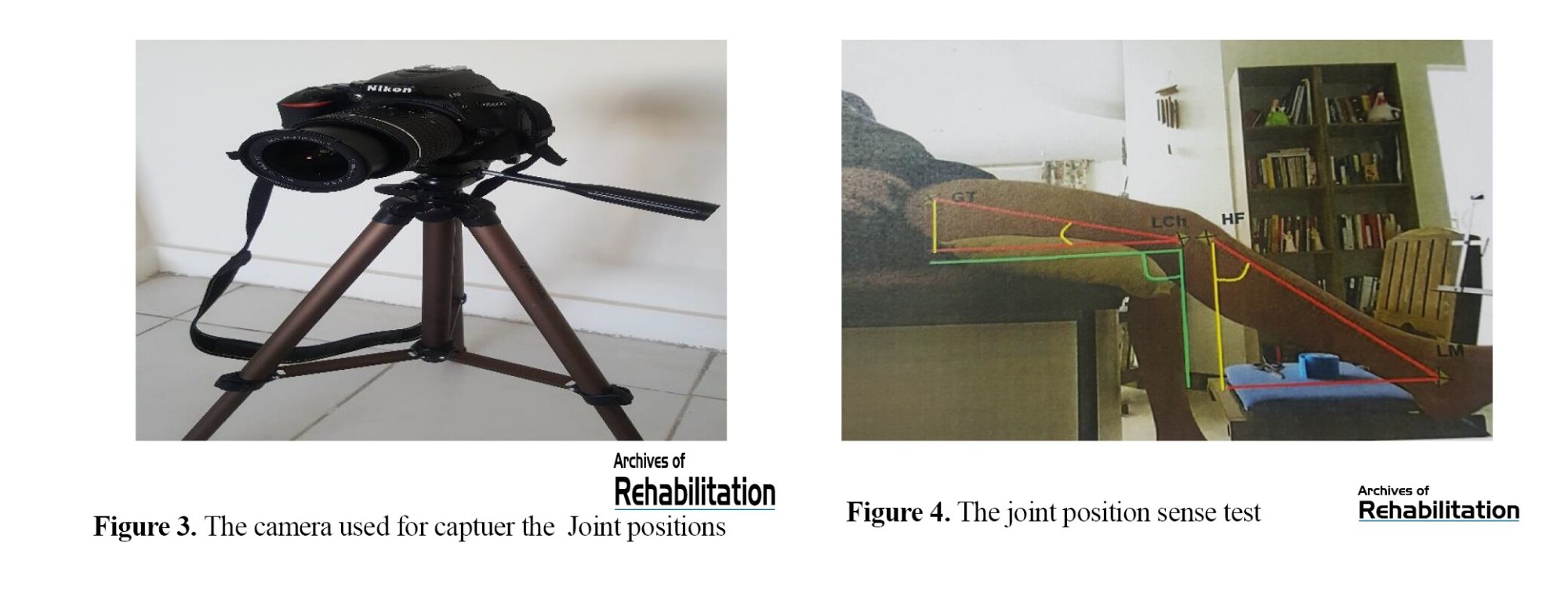
This study evaluated the dominant leg; the angles of 30 and 60 degrees of knee flexion were considered the target angles [30]. Reflective markers were placed before the assessment. To attach the first marker, we connected an imaginary line from the greater trochanter of the femur to the external joint line of the knee and placed a skin marker on the upper third of this line. The second marker was attached to the neck of the fibula, and the third marker to the upper part of the external malleolus. Then, the person was sitting on a chair and in a position where the knee was bent at 90 degrees, and the fourth marker was attached to the upper part of the popliteal fold in alignment with the upper edge of the patella [31]. The method of JPST in this research was passive-active and was performed while sitting. During the test, the subjects sat comfortably on the edge of a bed, with their legs hanging freely without touching the ground and their eyes closed. The camera was 80 cm away from the participant’s knee and positioned parallel to the knee’s axis (Figure 4).
The following process was used to conduct the test. First, the person administering the test moved the leg gradually (at a speed of about 10 degree/s) from the starting position (90° knee flexion) to the test positions (30° or 60° knee flexion) using a goniometer. Second, the person administering the test took a photo of the subject from the reference angle. Third, the subject was required to maintain the test position for 5 seconds actively. This process was repeated 5 times to learn the target angle. Finally, the participant actively tried to move the foot to the target angle. Lastly, for each target angle, the participants tried to make that angle 5 times, and the examiner took a picture of each of these times. Then, all photos, including those taken from the examiner’s and participants’ angles, were transferred to ImageJ software, and the exact number of these angles was calculated. Next, the amount of angle reconstructed by the participant was deducted from the angle made by the examiner. The obtained number was recorded as an absolute error. Then, it was averaged from 5 repetitions and recorded as the average absolute error in each target angle. Based on articles, ImageJ shows high reliability (ICC=0.96) when assessing knee flexion angles [32]. Absolute error is the signless arithmetic difference between test and response angles [33].
Dynamic Balance Test
The mSEBT was done to assess dynamic balance. To perform the mSEBT, the participants were placed in the center of the figure of Y, which was drawn on the ground in three directions: anterior (Ant), posteromedial (PM), and posterolateral (PL). As shown in figure 5, the test was performed so that the participants stood on the dominant leg, moved the other leg as far as they could along the determined line, and touched the tip of the toe on the ground. Subsequently, they were instructed to return the extended leg to a stable stance on both legs while the dominant leg should not be moved. This condition was repeated four times in each direction. The order of obtaining the directions was such that if the person’s right leg was dominant, the test was done clockwise, and if the left leg was dominant, it was done counterclockwise.
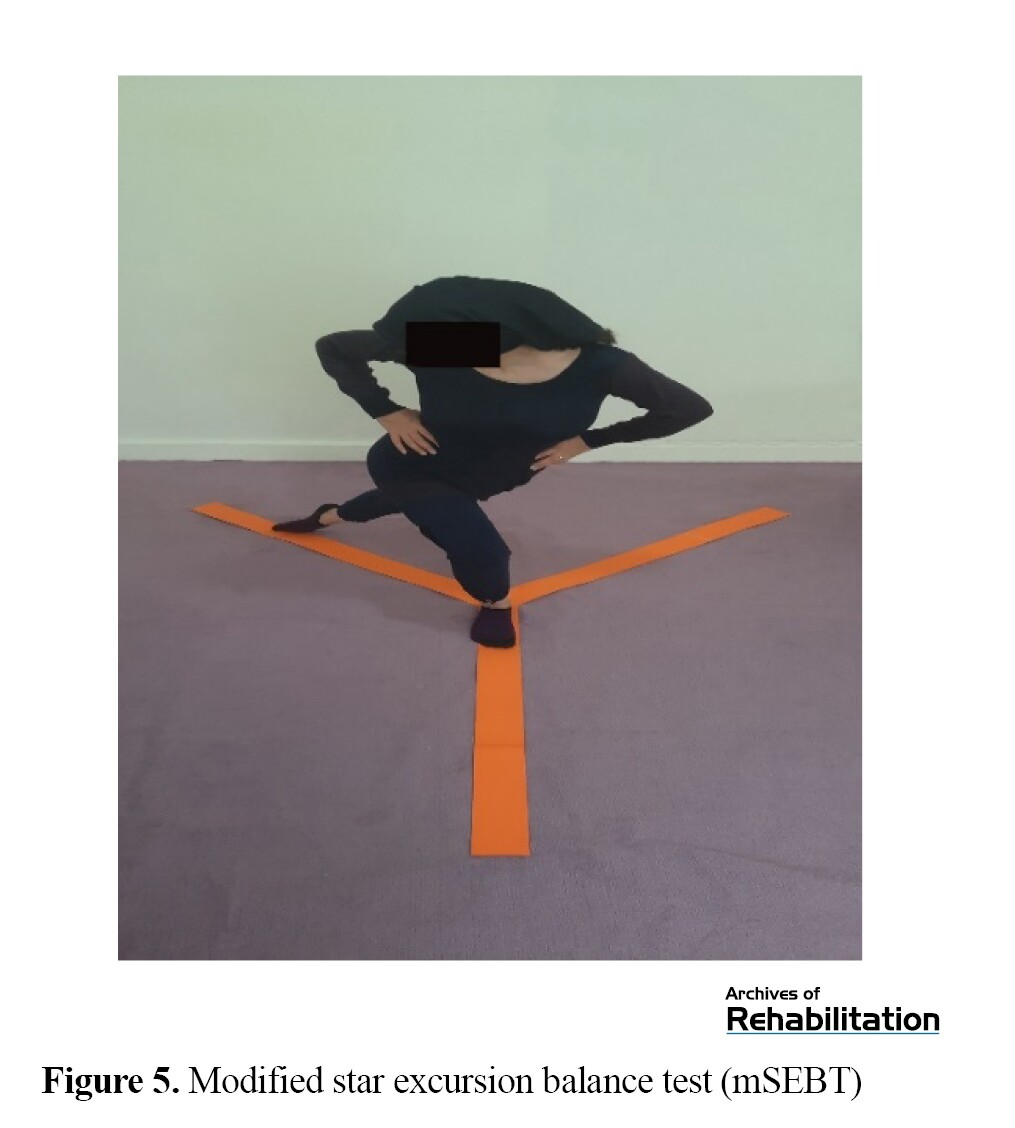
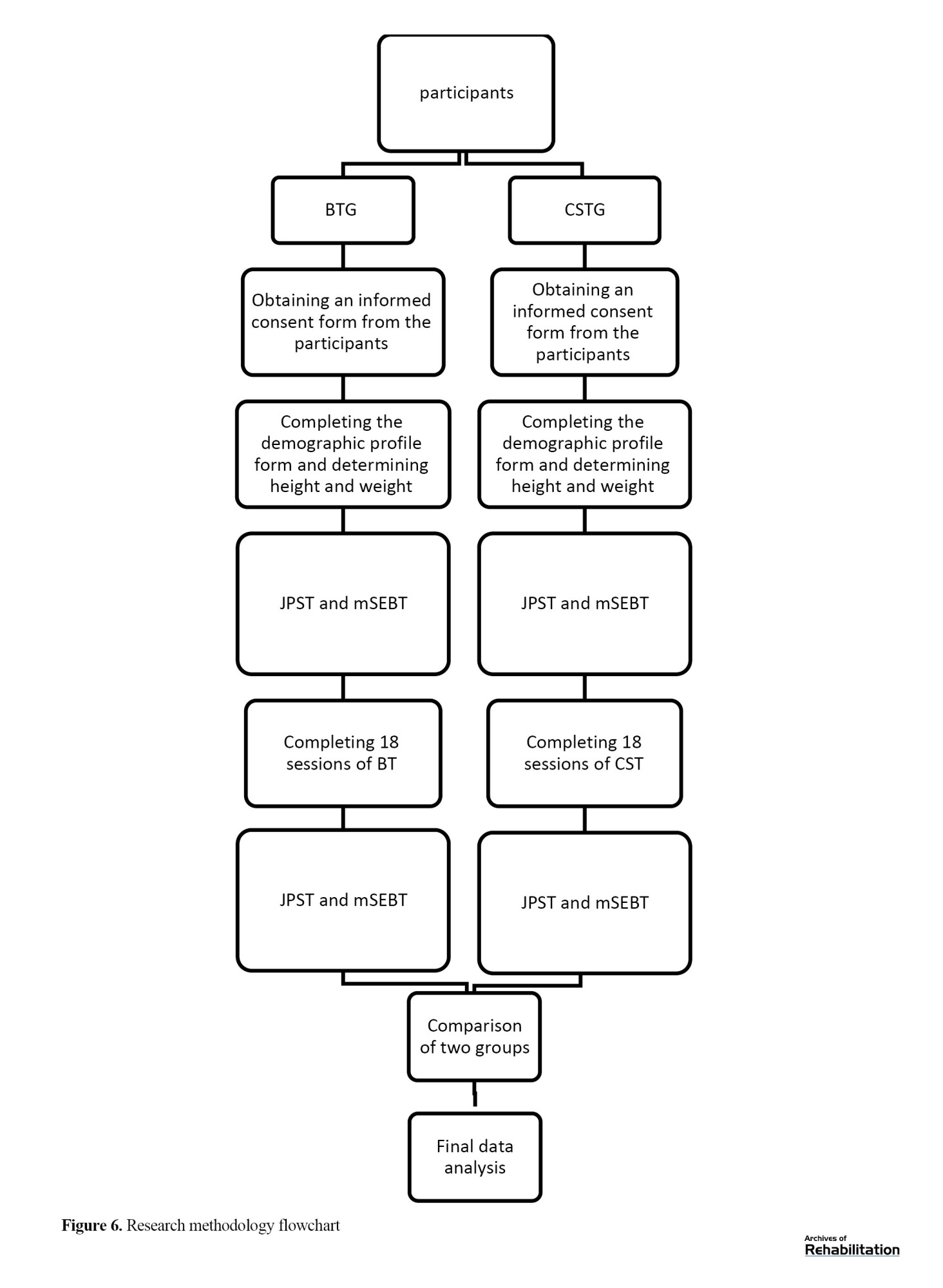
The test required the participants to maintain contact between their hands and pelvic area. The maximal touched length was identified during the trials by marking a point on the tape line and measuring it from the center of the grid [22]. The maximum reaching distance was normalized by calculating the mean reaching distance in four repetitions and dividing it by the leg length of the person measured earlier. A higher normalized score indicated better dynamic balance. Lower limb length was calculated based on the measurement between the anterior superior iliac spine and the medial malleolus tibia. If the subject could not maintain her balance on the support leg during the trial, the researcher would ignore the trial and repeat the test [7, 15]. The mSEBT has previously shown strong consistency within the same tester, as evidenced by a high ICC of 0.67 to 0.96 (Figure 6) [34].
Statistical Analysis
Levene’s test indicated that the equality of variances assumption was upheld for all variables (P<0.05). The distribution of scores was found to be normal according to the Shapiro-Wilk test (P<0.05). The assessment of improvement within the group was done using a paired t test for the JPST (30 and 60 degrees) and the mSEBT (Ant, PM, and PL directions). The improvement between different groups was evaluated using an independent t test. A P value of ≤0.05 was considered significant. All analyses were conducted utilizing SPSS software, version 22.
Results
General Characteristics
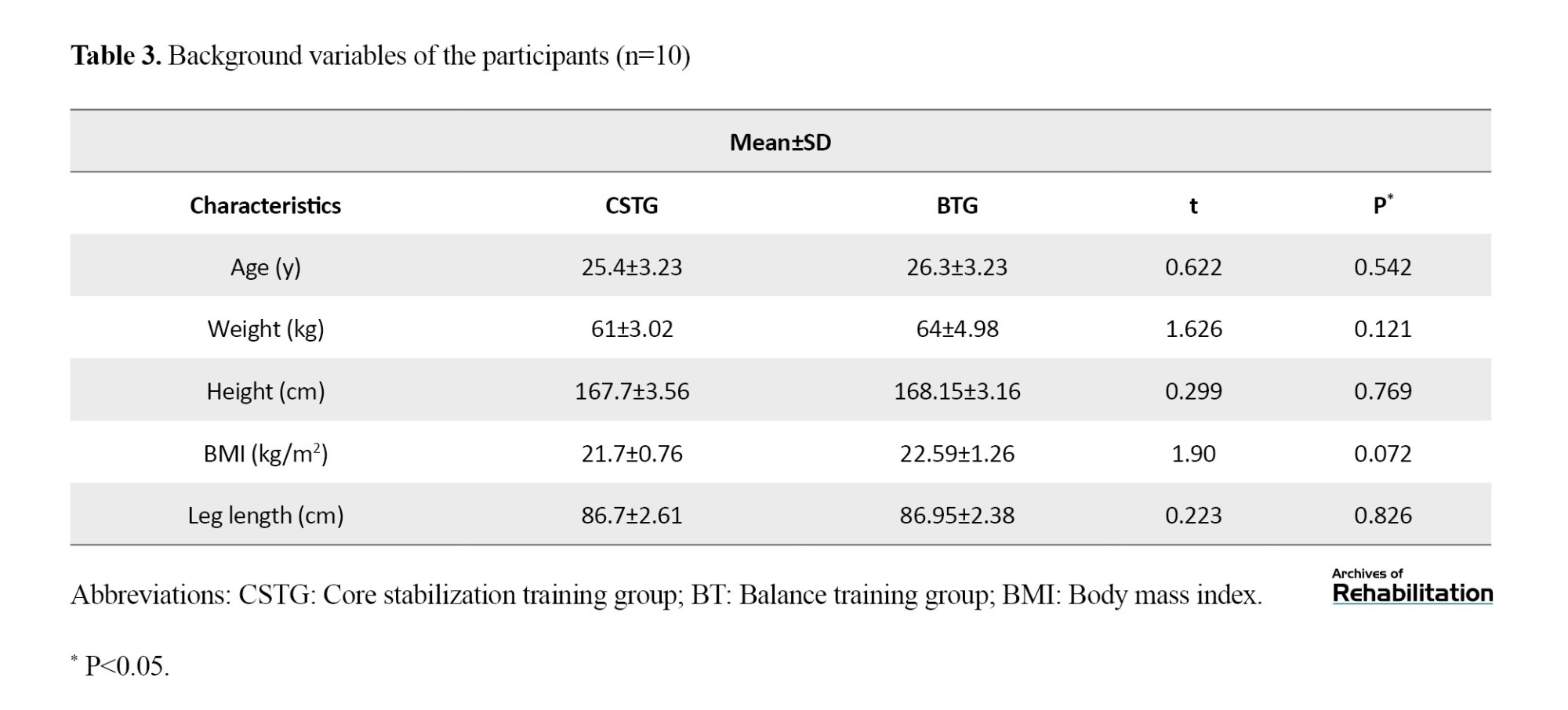
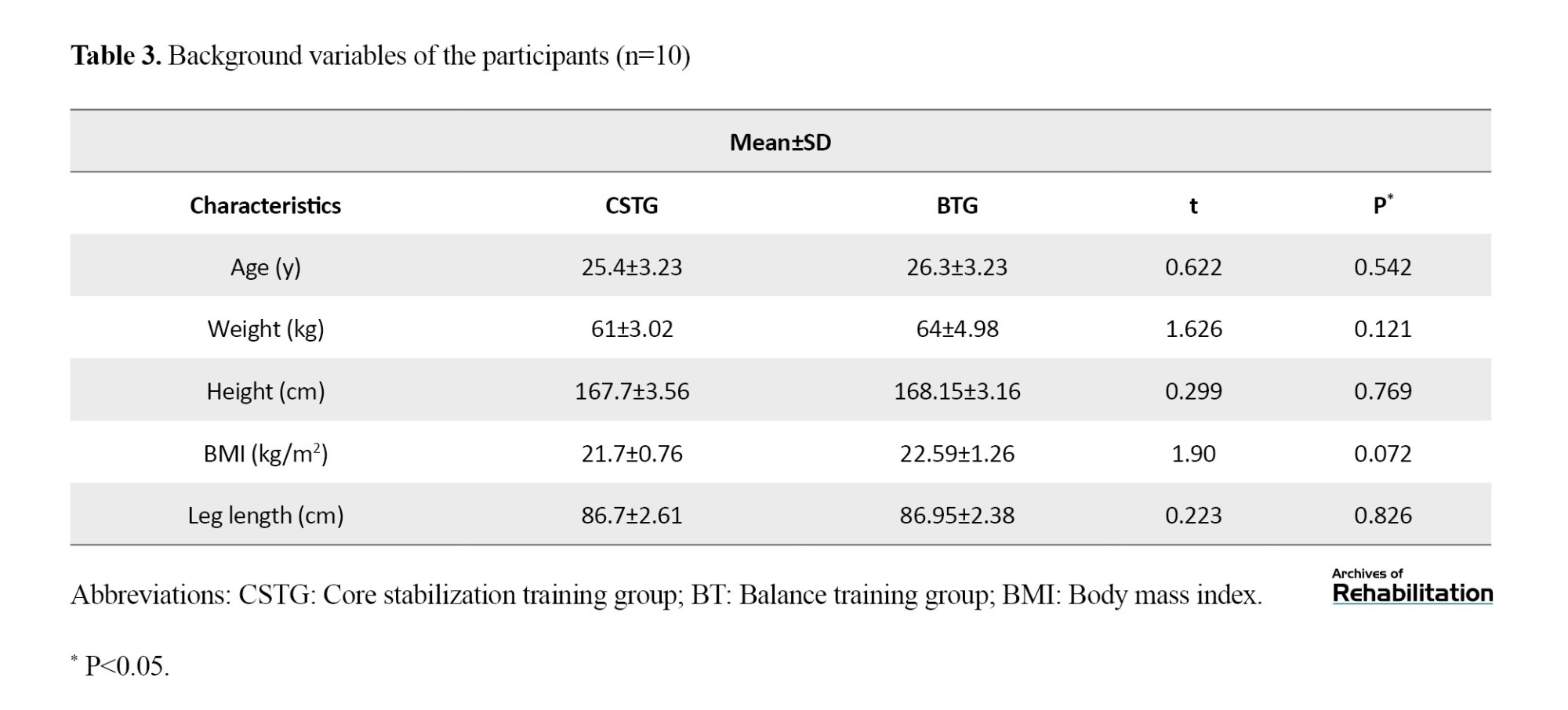
Twenty participants (nCSTG=10, nBTG=10) completed the study. Table 3 shows the average and standard deviation (SD) for the participants’ demographic details, such as age, height, weight, body mass index (BMI), and leg length. Comparing the demographic data between the two experimental groups revealed no significant difference (P>0.05).
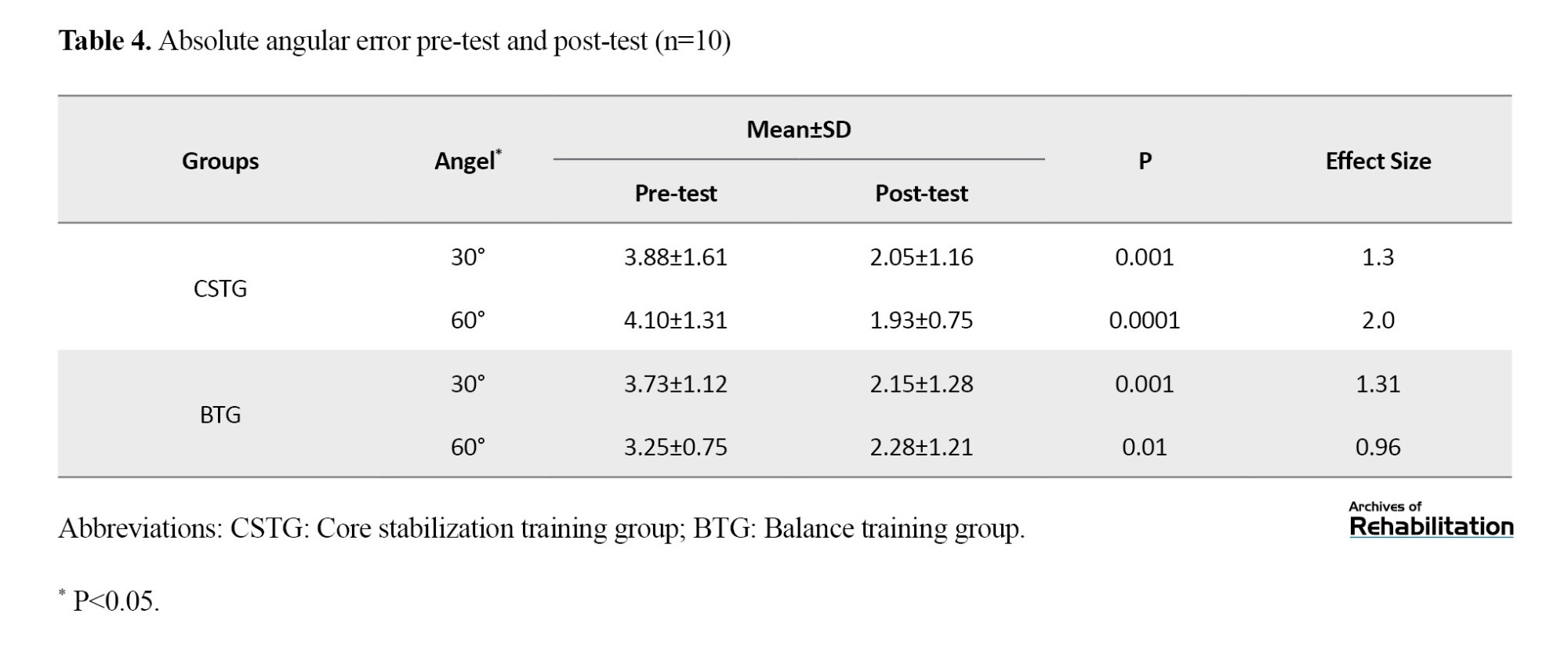
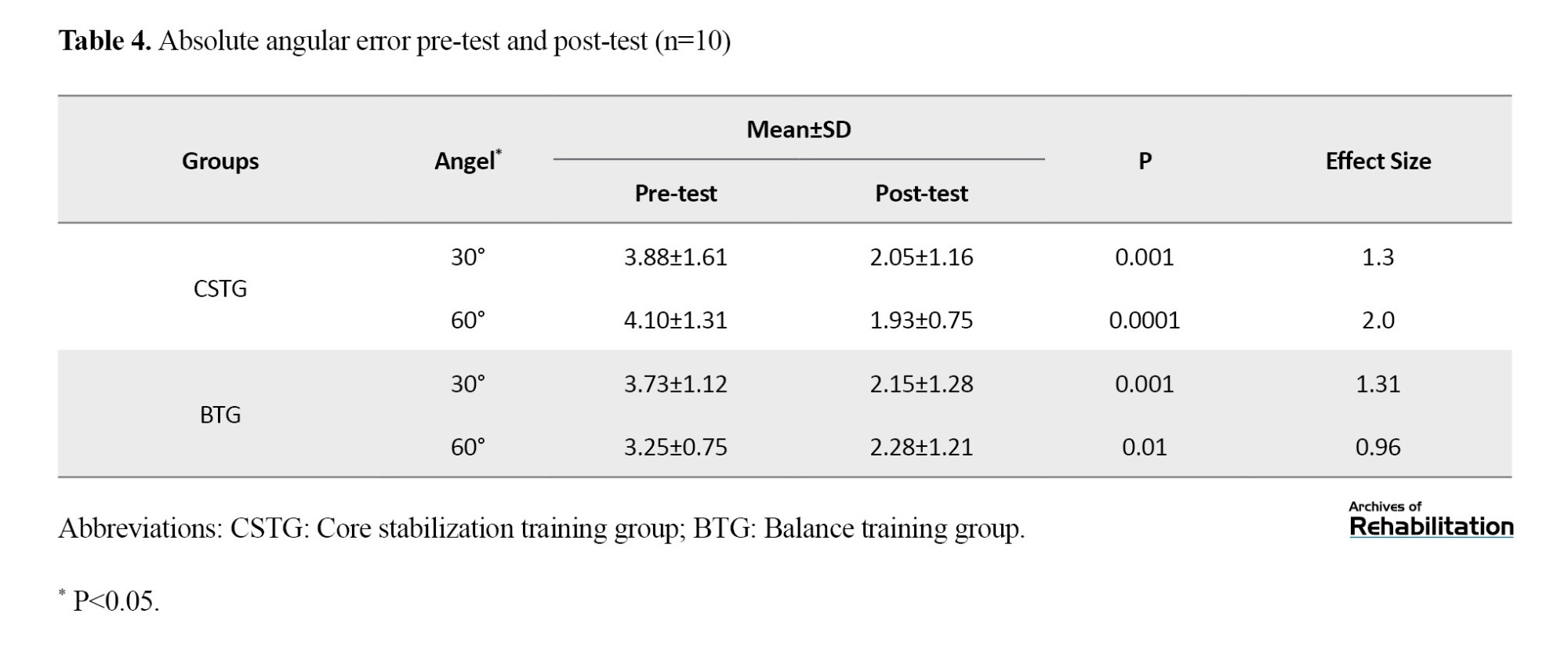
Within-Group Analysis
Analysis within the groups for JPST revealed that both training groups (CSTG and BTG) experienced a significant decrease in the absolute angular error at 30° and 60° (P<0.05). The results for proprioception absolute error in the initial and final tests for the groups can be found in Table 4.
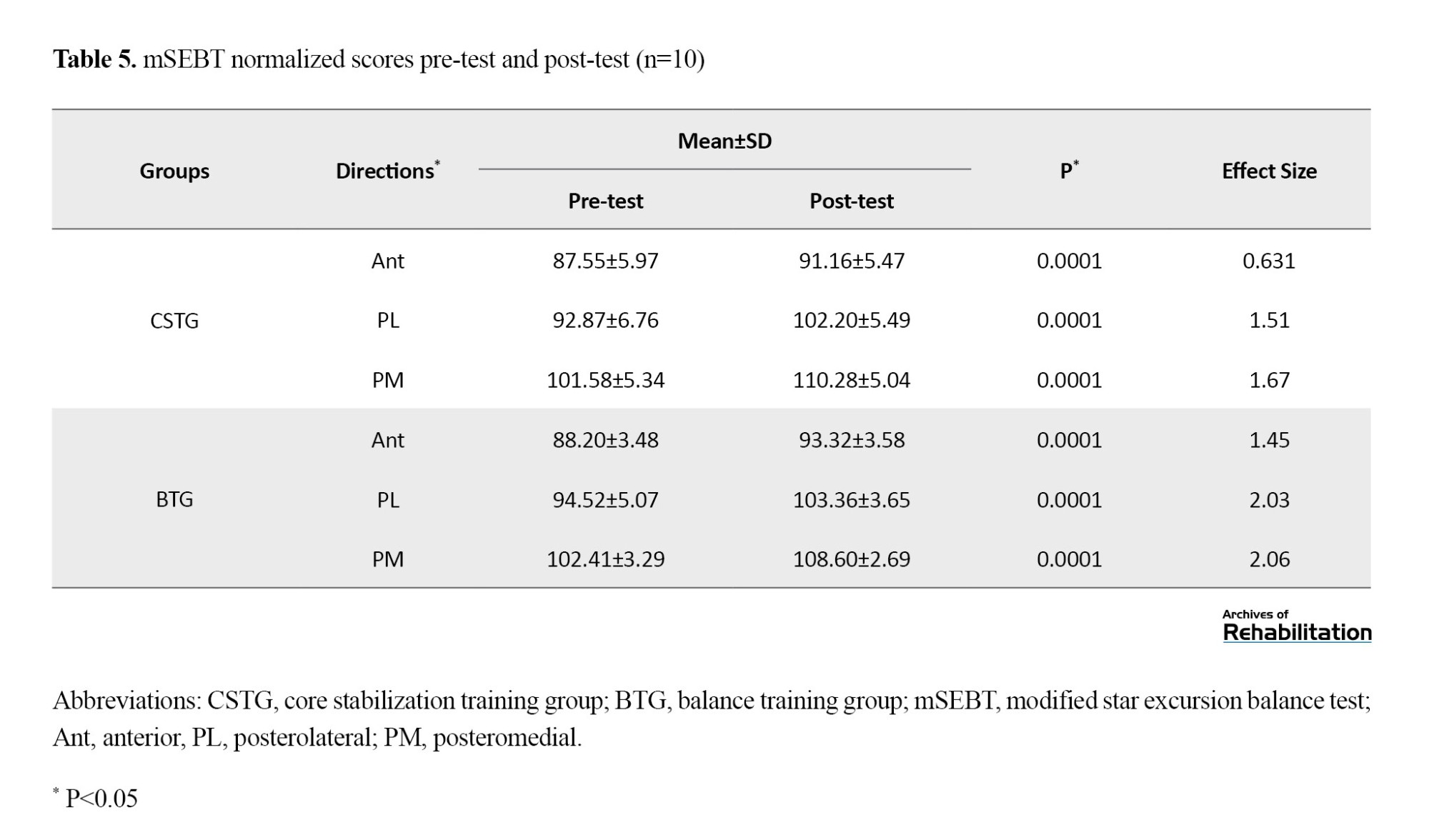
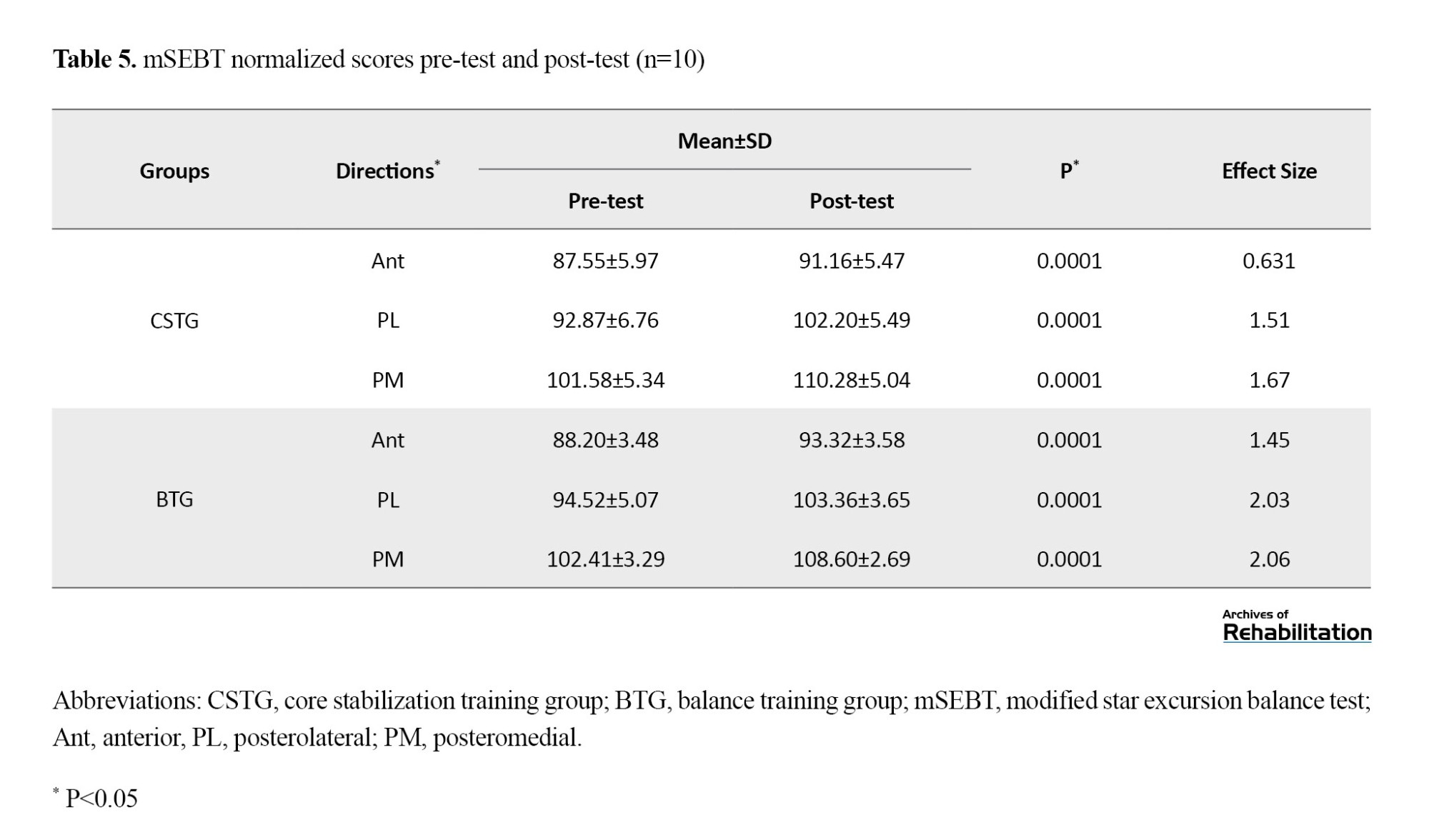
Within-group analysis for mSEBT showed that both training groups (CSTG and BTG) experienced a significant increase in the distance of reaching in three (Ant, PM, and PL) directions (P<0.05). The average mSEBT scores during the pretest and posttest for the groups can be found in Table 5.
Between-Group Analysis
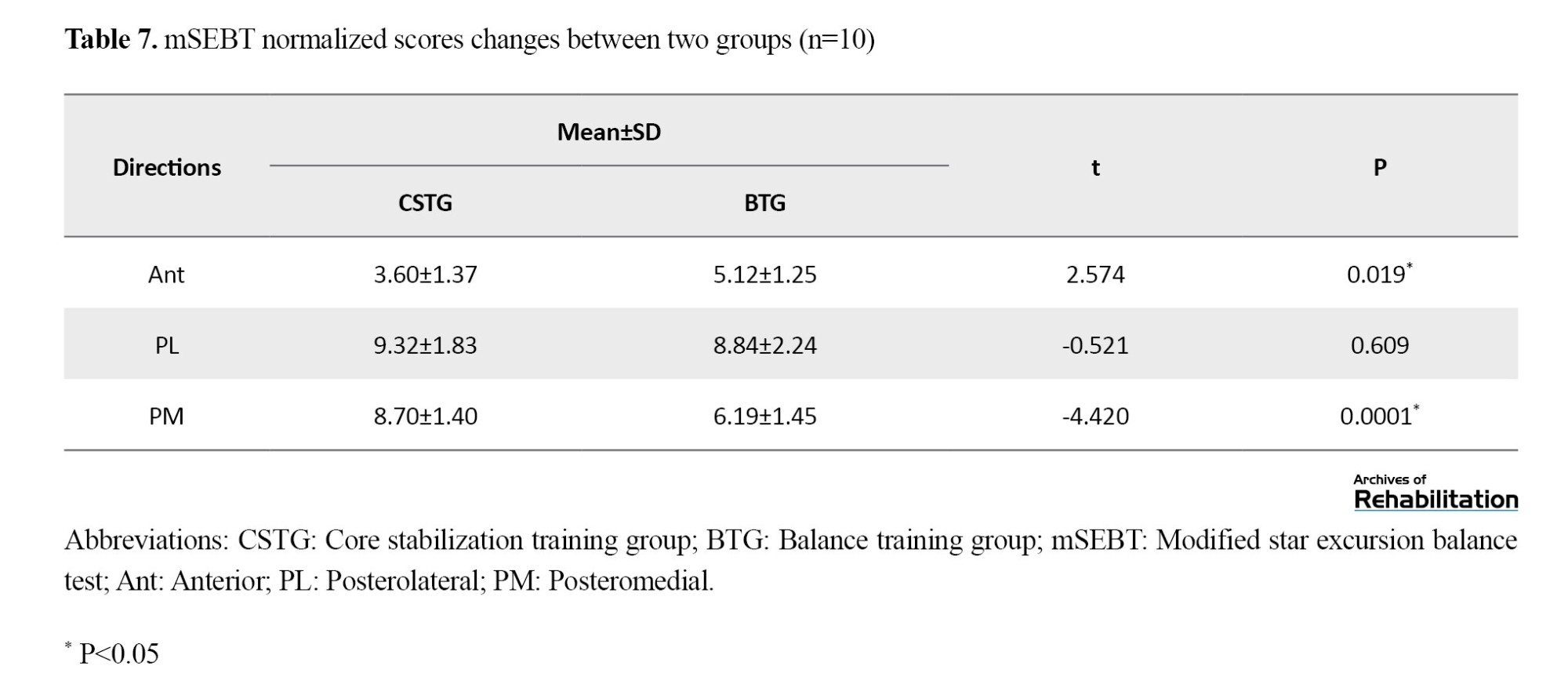
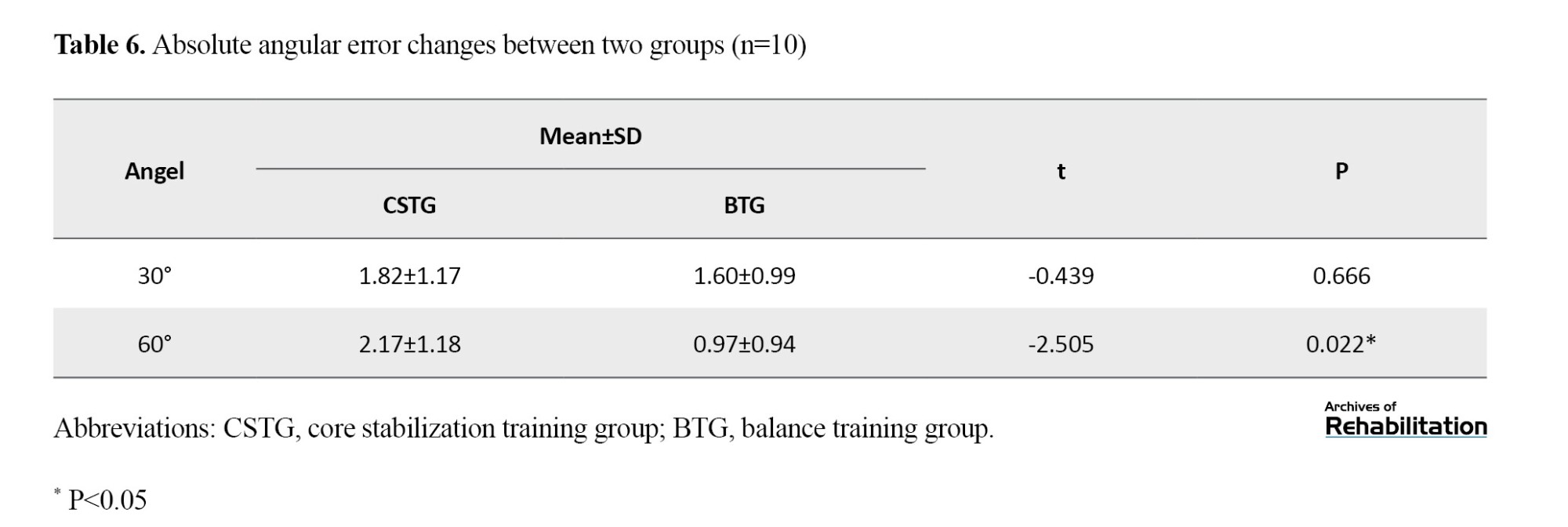
The analysis comparing the two groups in JPST indicated no statistically significant variance at the mean of absolute angular error reduction for position 30° (P>0.05). However, the mean of absolute error reduction for position 60° showed a significant statistical difference (P<0.05) that the mean of changes in the CSTG was significantly higher than BTG. The means of proprioception absolute error changes between the two groups are presented in Table 6.
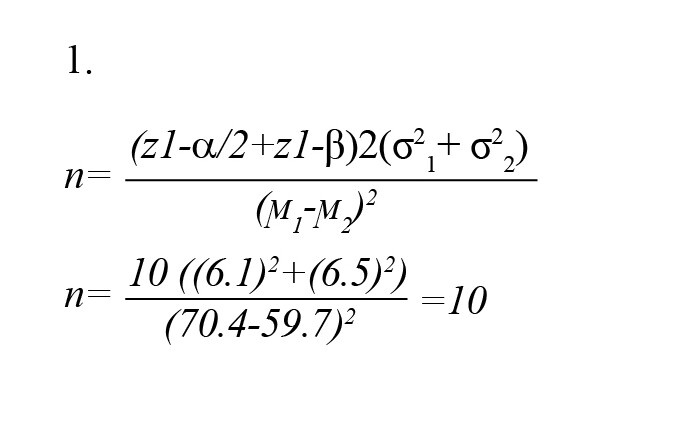
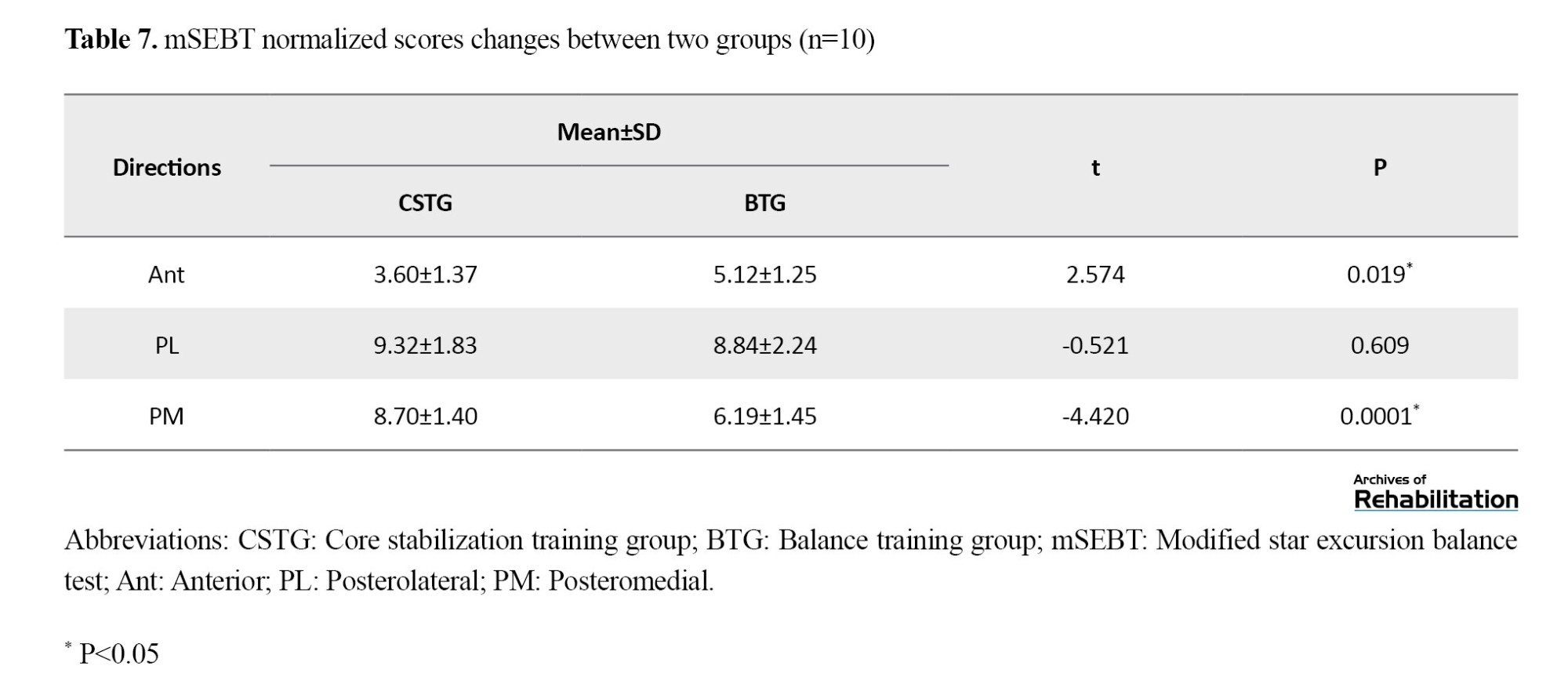
Between-group analysis for mSEBT exhibited no significant variance between the different values in the PL direction (P>0.05), and the mean changes in the CSTG were higher than BTG. However, significant differences were found in the Ant and PM directions (P<0.05). The average modifications in the Ant direction were higher in the CSTG than in BTG, and the mean changes in the PM direction were higher in the BTG than in CSTG. The means of mSEBT score changes between the two groups are presented in Table 7.
Discussion
The Effect of CST and BT on Outcome Measures
This study examined the effect of a 6-week CST and BT program on dynamic balance and knee proprioception in female soccer players. The BT and CST groups showed significant enhancements in knee proprioception and dynamic balance. Many articles have already been conducted on CST’s effect on dynamic balance [35, 36]. Most of these articles have reported the positive effects of this exercise. For example, in his research, Gribble showed that a 6-week training program focused on core stabilization can improve maximal reach distances in healthy individuals when performing the SEBT [37]. On the other hand, this study contradicts Sato and Mokha’s findings on CST in runners: SEBT did not significantly improve after 6 weeks, but 5000 m times improved compared to the control group [38]. However, the number of articles investigating CST’s effect on knee proprioception is limited. The results of this research support the discoveries of Mutlu et al., who concluded that sedentary individuals who engaged in 10 weeks of instability resistance training using body weight displayed improved knee proprioception [17].
Comparing the Effect of CST and BT on Outcome Measures
According to our study, CSTG showed greater improvement than BTG regarding the PM reach distance of mSEBT and JPST at 60 degrees. On the other hand, BTG showed more improvement than CSTG in the Ant reach distance of mSEBT. However, when we analyzed both groups, no substantial difference was observed with the mean reduction of the absolute error at 30 degrees and the mean improvement of reach distance of mSEBT in the PL direction. In summary, the CSTG showed more improvement in proprioception than the BTG, while BT had a greater effect on the Ant direction in the mSEBT. On the other hand, CST had a greater effect on the posterior directions of mSEBT.
This study supports Aggarwal et al.’s findings that both CST and BT programs improved balance performance, but the CSTG had greater improvement than the BTG [39]. Unfortunately, the number of articles that have compared the effect of CST with BT on knee proprioception is scarce. This is one of the reasons for the novelty of the subject of this article, and it is suggested that more research be done in the field of finding the best type of exercise therapy in the field of multiple factors to minimize the likelihood of harm in sports players.
Possible Mechanisms of the Effect of CST and BT on Outcome Measures
Several variables could enhance JPST in CSTG and BTG. Despite the constant number of peripheral receptors, training might alter proprioception through central mechanisms [40]. Using physioball and wobble boards can create an unstable environment that can activate proprioceptors to help maintain balance and detect body position [41, 42]. Instability can lead to changes in balance, which, in turn, can lead to alterations in the length of the muscle-tendon unit, as well as in tension and neuromuscular activity. These changes can then affect one’s ability to perceive and react to alterations in balance [43-45]. Performing closed kinetic chain exercises, such as standing and kneeling on physioballs, involves movements that use multiple joints and planes. These movements help engage proprioceptors, which play a role in determining joint direction and position [46]. CST and BT can enhance the responsiveness of the feedback pathway, reduce the time taken to initiate movements, and enhance the accuracy of the sense of position [47]. Practicing on surfaces that are not stable could lead to an increase in co-contractile activity. This increase can help enhance motor control and balance [48]. Greater antagonist activity can be induced by resisting plantar flexion and leg extension in unstable conditions compared to stable conditions [49].
These mechanisms mentioned in both types of CST and BT can improve knee proprioception, but the reason why CST had a better effect on improving knee proprioception may be due to the presence of an additional mechanism, ie, the lumbosacral junction connects the spine to the lower extremities during sports. A stable core is essential for transferring force from the upper body to the lower body [50]. Core muscle stability may optimize lower extremity function and improve balance [51]. Strengthening core muscles improves body position and movement, leading to better proprioception. Core stability exercises can enhance joint proprioception in the lower limbs [52].
Also, CST can potentially improve spinal segment management and deep stabilizing muscles’ simultaneous contraction, ultimately leading to improved center of gravity management and optimal lumbopelvic control. Additionally, training the trunk muscles can improve lower extremity function and balance control by increasing neural recruitment patterns and activating the nervous system, promoting the concurrency of motor units, and reducing neural inhibitory reflexes during SEBT. The reason SEBT reach distance improves may be due to the activation of deep local muscles happening earlier than the activation of global abdominal muscles during lower extremity movement. Activating the spinal stabilizers early on establishes a firm foundation for lower body movement, enhancing the spine’s stiffness. It is possible that the training of deep stabilizers in CSTG contributed to creating such a stable base [53].
Study Limitations
The study is restricted by the minimal involvement of female athletes due to the spread of the coronavirus. Another constraint of this research is the age range of the participants examined (20–30 years); it is unclear whether all results occur younger or older than the study period. Another limitation of this research is assessing the dominant foot; it is better to perform the tests on the right and left foot and compare them. Also, it is better to use an isokinetic device to measure proprioception, which controls the speed and the sense of force and movement. This research did not involve extended follow-up and only focused on women, without comparing results with men. More research should be conducted on different groups of people in the future. Finally, it is better to conduct future studies with a follow-up period.
Conclusion
After evaluating the findings of this research, we can make the following inference: both CST and BT can effectively improve knee proprioception and dynamic balance in female amateur soccer players.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were performed after the study was approved by the Scientific Board and Ethics Committee of the School of Rehabilitation, Tehran University of Medical Sciences (Ethics committee reference number: IR.TUMS.FNM.REC.1399.012).
Funding
The present paper was extracted from the Master’s thesis of the first author, Department of Physiotherapy, School of Rehabilitation, Tehran University of Medical Sciences.
Authors' contributions
The authors contributed equally to preparing this paper.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the distance runners who participated in this study.
References
Women are more likely to be injured in sports than men due to their anatomical, hormonal, biomechanical, and neuromuscular differences [1]. Factors that raise the possibility of sports injuries generally include proprioceptive disorder, scar tissue formation, and pathological variations in joint range of motion [2]. In these cases, proprioception is crucial because it protects against movement injuries and plays a role in establishing joint constancy and natural coordination of movements [3، 4]. Joint position sense is a subset of proprioception, involving the awareness and ability to reconstruct the angle of a joint after movement [5, 6]. Proprioception plays a big part in the awareness and unawareness of the senses, spontaneous detection of movements, coordination and learning of movement, posture, and balance [5]. Soccer players need a significant dynamic balance to act rightly and reduce the risk of injury during fast and cutting movements. The capability to maintain body stability while standing is called static balance, and while moving, it is called dynamic balance. Dynamic balance involves some degree of predictable movement near the center of gravity [7-9]. There are a few points in this regard. Among different sports, soccer is one of the most risky sports [10] as this sport is called “knee injury disease” [11]. Proprioception becomes more important in athletes, especially soccer players because the highest level of performance is expected from them [12]. Among the joints of the human body, the knee is one of the richest joints with proprioceptive receptors, and has the extensor and flexor muscles, which are the largest in the body, also have the largest number of muscle spindles [13].
Physiotherapists are searching for effective ways to return joint proprioception to a normal state to provide optimal stability and mobility in static and dynamic situations. Proprioception can be influenced by various factors, including age, injuries, diseases, and physical activity [14]. No definite therapeutic exercise method currently improves proprioception [15, 16]. Still, several exercises have been suggested to improve proprioception, such as balance training (BT) [14], closed chain exercises, plyometric, and core stability training (CST) [9, 17]. Hübscher stated in his study that more comparative studies should be conducted to determine the best exercises to reduce the risk of injury in different sports [18]. In the past, numerous studies have demonstrated that CST has an impressive role in enhancing athletic efficiency, progressing balance, and decreasing the risk of sports injuries [19, 20]. Despite the importance of proprioception, very few studies have evaluated the effect of CST on proprioception, and most of the effects of BT or a combination of exercises on improving proprioception have been researched. Despite the theoretical advantages proposed for each exercise, few studies have compared these methods. Additionally, there is not enough information about the most effective training method and the benefits of each training alone. Therefore, this research was conducted to compare the impact of CST with BT, which is more commonly used to improve proprioception. Considering that no research has been done to compare the consequence of CST and BT on knee proprioception in female soccer players, this study aims to determine the impact of these two exercise methods on knee proprioception and dynamic balance of healthy female athletes and also to compare the effects of these exercises with each other.
Materials and Methods
Trial Design
The design of this research was an interventional study.
Blinding
This research was single-blinded (participants were blind to the type of intervention of their training group).
Sample Size
A comparison equation of averages was used to conduct a sample calculation to determine the sample size. The equation originated from the mean reach distance assessed in the star excursion balance test (SEBT) as part of the data in Filipa et al.’s research [20]. The mean difference for improvement was 10%, and the standard deviation was 7.5%. A significance level 0.05 was adopted, and the correlation power was set at 80% [21]. Thus, the sample consisted of 10 women in each group (Equation 1).
Study Participants
After permission from the Ethics Committee (IR.TUMS.FNM.REC.1399.012), 20 female soccer athletes completed the study. Most participants were selected from the female athletes participating in the sports complexes and volunteered to participate in this study. For inclusion in the study, athletes had to meet the following criteria: female gender, aged between 20 and 30 years, and participating in an unprofessional level of soccer [16]. The exclusion criteria were as follows: having had lower limb or lumbar-spine problems or had an operation in the last half year; experienced neurological, vestibular, or visual disorders within the previous 6 months; were presently participating in another training program; did not finish the interventions and evaluations; or attended less than 80% of the exercise meetings (16 out of 18 sessions) [21].
Randomization
The subjects were split into two groups utilizing the sealed envelope technique: 10 in the core stabilization training group (CSTG) and 10 in the balance training group (BTG). A summary of the research objectives was presented to participants, and they signed the informed consent form.
Outcome Measures
Information regarding the participant’s age, height, weight, and leg length were gathered. Knee proprioception was measured by using the joint position sense test (JPST) [9], and dynamic balance was measured by using the modified star excursion balance test (mSEBT) one week before and immediately after the 6-week interventions [22].
Intervention
The subjects completed the CST or BT program three times a week. They practiced on the days that were part of their regular schedule. The training program lasted around 30 minutes per session for 6 weeks, totaling 18 sessions. Considering that the participants in this study were blind, they performed the exercises separately and under the supervision of the physiotherapist.
The Core Stability Training Program
The participants engaged in a six-week exercise program with the investigator, meeting thrice weekly for up to half an hour. The CST program comprises three exercises designed to increase the trunk muscles’ power and enhance neuromuscular coordination [23-26]. The CST program protocol is based on the training program set in Jeffreys’ research [27]. The exercise program had three levels, each with different types of exercises. The first level involved stationary exercises, then low motions in an unsteady setting were achieved gradually. Participants in the second level engaged in stationary contractions in an unsteady setting and transitioned to active motions in a steadier environment. In the third level, participants performed motion on uneven surfaces while also incorporating resistance. The type of exercises was changed and improved every week, and each training session was 30 minutes long. The session began with a 10-minute warm-up, including a 5-minute walk and static stretching for the major muscle groups. Despite learning new activities each week, specific exercises built upon the previous weeks by incorporating a new action or changing the surface [22]. The protocol is described in Table 1 in the attachment and is shown in Figure 1.
Balance Training Program
The program involved three weekly sessions and was designed based on scientifically validated BT protocols from previous studies [28]. The program consisted of a 5-phase BT approach, with details outlined in Figure 2 and Table 2.
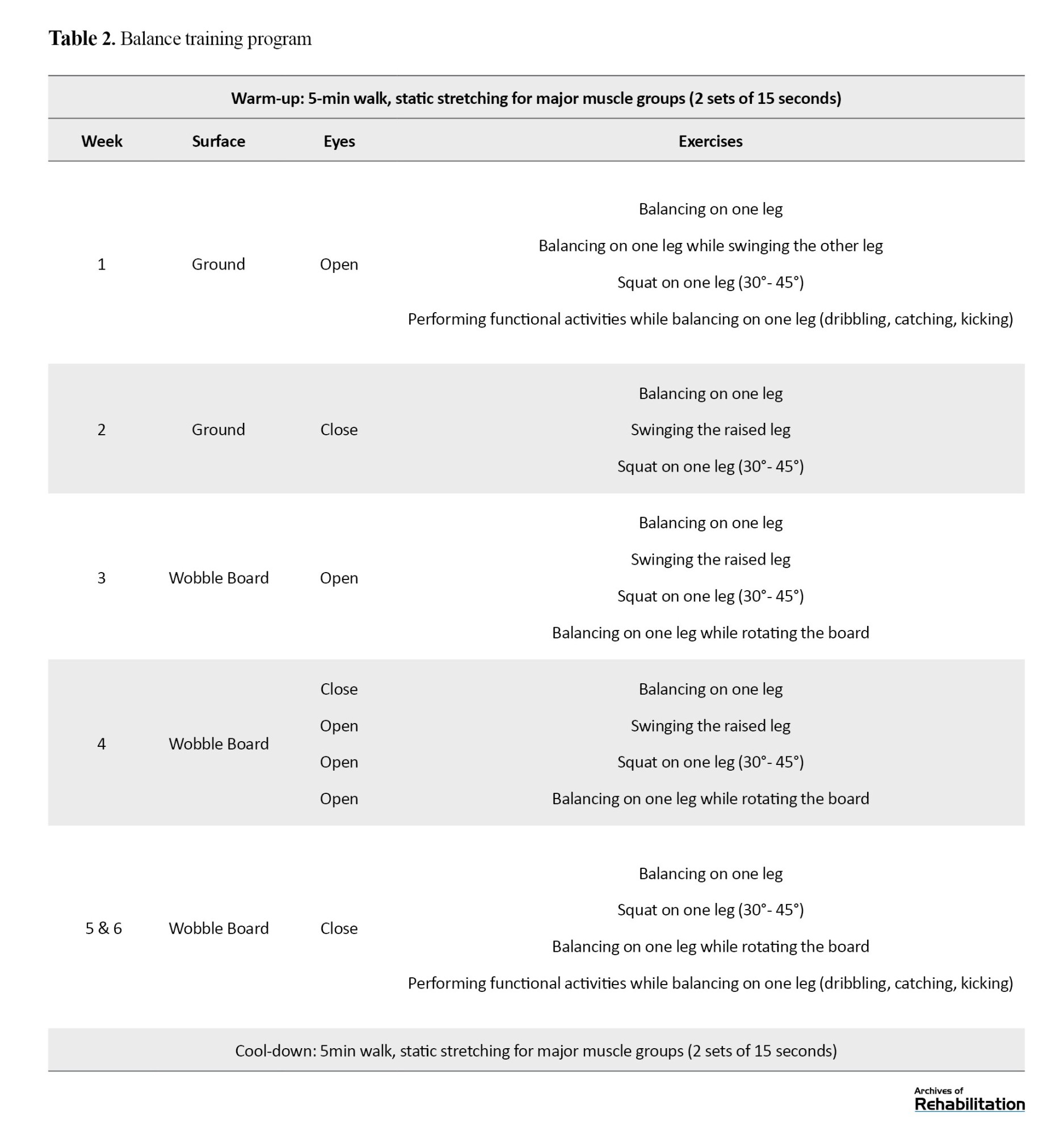
During each phase, exercises were carried out for up to half a minute, and there was a half-minute rest interval between each exercise. The exercises were improved every week. The difficulty of the exercises was changed by opening and closing the eyes and doing the exercise on the floor or wobbleboard. The protocol of these exercises in the first week was that the person maintained her balance on one leg while using her sense of sight and standing on the ground. Progress was made to the point that in the sixth week, balance exercises were performed by standing on one leg on the balance board with eyes closed and functional movements of the upper leg. All exercises were performed for up to 30 seconds during all phases, with 30 seconds of rest in between, during which the legs were alternated [28].
Proprioception Test
To measure knee joint position sense, the error rate in the JPST was evaluated using skin markers, digital photography, and ImageJ software .[9] A previous study showed an intraclass correlation coefficient (ICC) of 0.910 for this method of JPS assessment [29]. Nikon’s 24-megapixel digital camera model D5600 was used to take photographs of the joint positions in this study (Figure 3). Before starting the assessments, the reliability of this digital camera was assessed by computing ICC= 0.99.
This study evaluated the dominant leg; the angles of 30 and 60 degrees of knee flexion were considered the target angles [30]. Reflective markers were placed before the assessment. To attach the first marker, we connected an imaginary line from the greater trochanter of the femur to the external joint line of the knee and placed a skin marker on the upper third of this line. The second marker was attached to the neck of the fibula, and the third marker to the upper part of the external malleolus. Then, the person was sitting on a chair and in a position where the knee was bent at 90 degrees, and the fourth marker was attached to the upper part of the popliteal fold in alignment with the upper edge of the patella [31]. The method of JPST in this research was passive-active and was performed while sitting. During the test, the subjects sat comfortably on the edge of a bed, with their legs hanging freely without touching the ground and their eyes closed. The camera was 80 cm away from the participant’s knee and positioned parallel to the knee’s axis (Figure 4).
The following process was used to conduct the test. First, the person administering the test moved the leg gradually (at a speed of about 10 degree/s) from the starting position (90° knee flexion) to the test positions (30° or 60° knee flexion) using a goniometer. Second, the person administering the test took a photo of the subject from the reference angle. Third, the subject was required to maintain the test position for 5 seconds actively. This process was repeated 5 times to learn the target angle. Finally, the participant actively tried to move the foot to the target angle. Lastly, for each target angle, the participants tried to make that angle 5 times, and the examiner took a picture of each of these times. Then, all photos, including those taken from the examiner’s and participants’ angles, were transferred to ImageJ software, and the exact number of these angles was calculated. Next, the amount of angle reconstructed by the participant was deducted from the angle made by the examiner. The obtained number was recorded as an absolute error. Then, it was averaged from 5 repetitions and recorded as the average absolute error in each target angle. Based on articles, ImageJ shows high reliability (ICC=0.96) when assessing knee flexion angles [32]. Absolute error is the signless arithmetic difference between test and response angles [33].
Dynamic Balance Test
The mSEBT was done to assess dynamic balance. To perform the mSEBT, the participants were placed in the center of the figure of Y, which was drawn on the ground in three directions: anterior (Ant), posteromedial (PM), and posterolateral (PL). As shown in figure 5, the test was performed so that the participants stood on the dominant leg, moved the other leg as far as they could along the determined line, and touched the tip of the toe on the ground. Subsequently, they were instructed to return the extended leg to a stable stance on both legs while the dominant leg should not be moved. This condition was repeated four times in each direction. The order of obtaining the directions was such that if the person’s right leg was dominant, the test was done clockwise, and if the left leg was dominant, it was done counterclockwise.
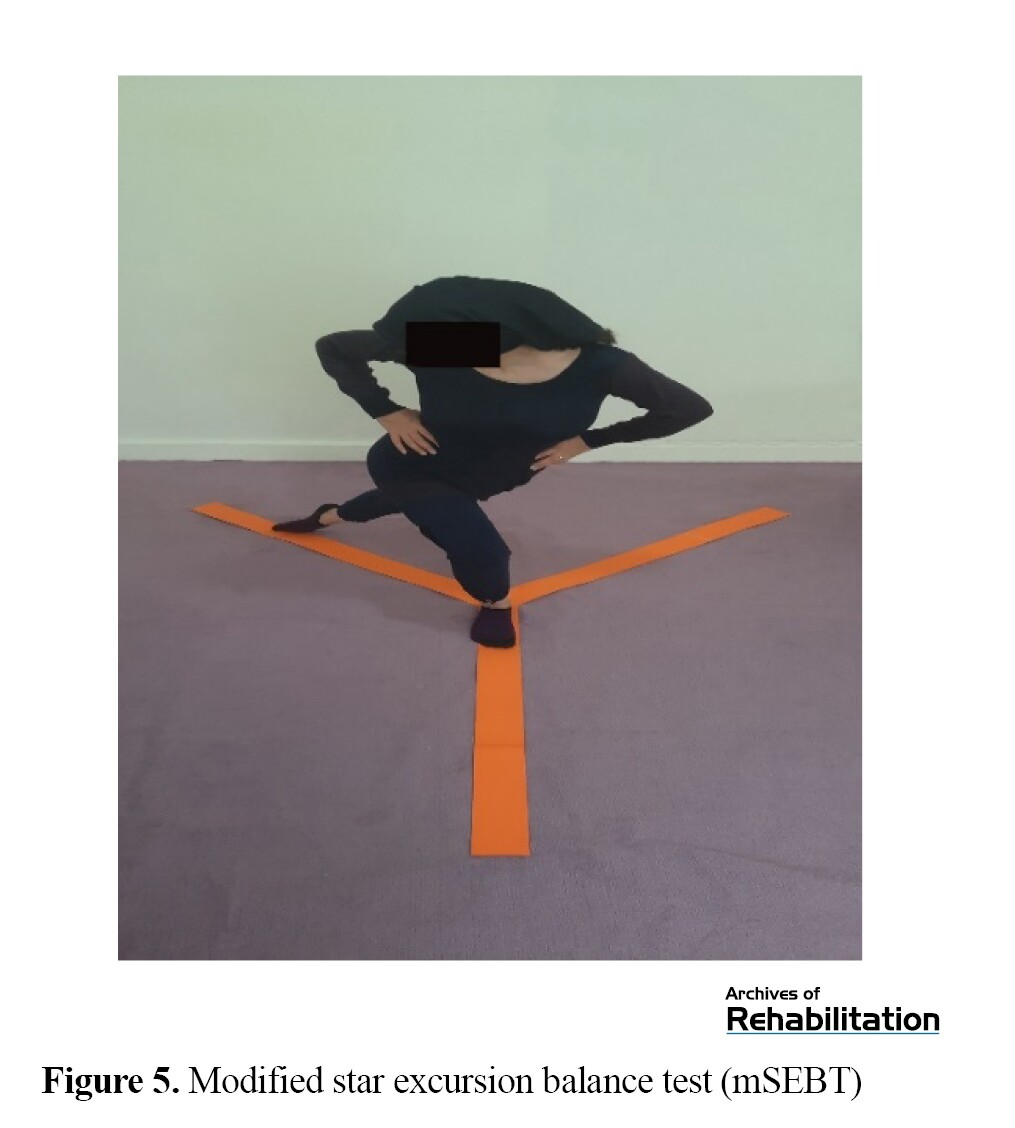
The test required the participants to maintain contact between their hands and pelvic area. The maximal touched length was identified during the trials by marking a point on the tape line and measuring it from the center of the grid [22]. The maximum reaching distance was normalized by calculating the mean reaching distance in four repetitions and dividing it by the leg length of the person measured earlier. A higher normalized score indicated better dynamic balance. Lower limb length was calculated based on the measurement between the anterior superior iliac spine and the medial malleolus tibia. If the subject could not maintain her balance on the support leg during the trial, the researcher would ignore the trial and repeat the test [7, 15]. The mSEBT has previously shown strong consistency within the same tester, as evidenced by a high ICC of 0.67 to 0.96 (Figure 6) [34].
Statistical Analysis
Levene’s test indicated that the equality of variances assumption was upheld for all variables (P<0.05). The distribution of scores was found to be normal according to the Shapiro-Wilk test (P<0.05). The assessment of improvement within the group was done using a paired t test for the JPST (30 and 60 degrees) and the mSEBT (Ant, PM, and PL directions). The improvement between different groups was evaluated using an independent t test. A P value of ≤0.05 was considered significant. All analyses were conducted utilizing SPSS software, version 22.
Results
General Characteristics
Twenty participants (nCSTG=10, nBTG=10) completed the study. Table 3 shows the average and standard deviation (SD) for the participants’ demographic details, such as age, height, weight, body mass index (BMI), and leg length. Comparing the demographic data between the two experimental groups revealed no significant difference (P>0.05).
Within-Group Analysis
Analysis within the groups for JPST revealed that both training groups (CSTG and BTG) experienced a significant decrease in the absolute angular error at 30° and 60° (P<0.05). The results for proprioception absolute error in the initial and final tests for the groups can be found in Table 4.
Within-group analysis for mSEBT showed that both training groups (CSTG and BTG) experienced a significant increase in the distance of reaching in three (Ant, PM, and PL) directions (P<0.05). The average mSEBT scores during the pretest and posttest for the groups can be found in Table 5.
Between-Group Analysis
The analysis comparing the two groups in JPST indicated no statistically significant variance at the mean of absolute angular error reduction for position 30° (P>0.05). However, the mean of absolute error reduction for position 60° showed a significant statistical difference (P<0.05) that the mean of changes in the CSTG was significantly higher than BTG. The means of proprioception absolute error changes between the two groups are presented in Table 6.
Between-group analysis for mSEBT exhibited no significant variance between the different values in the PL direction (P>0.05), and the mean changes in the CSTG were higher than BTG. However, significant differences were found in the Ant and PM directions (P<0.05). The average modifications in the Ant direction were higher in the CSTG than in BTG, and the mean changes in the PM direction were higher in the BTG than in CSTG. The means of mSEBT score changes between the two groups are presented in Table 7.
Discussion
The Effect of CST and BT on Outcome Measures
This study examined the effect of a 6-week CST and BT program on dynamic balance and knee proprioception in female soccer players. The BT and CST groups showed significant enhancements in knee proprioception and dynamic balance. Many articles have already been conducted on CST’s effect on dynamic balance [35, 36]. Most of these articles have reported the positive effects of this exercise. For example, in his research, Gribble showed that a 6-week training program focused on core stabilization can improve maximal reach distances in healthy individuals when performing the SEBT [37]. On the other hand, this study contradicts Sato and Mokha’s findings on CST in runners: SEBT did not significantly improve after 6 weeks, but 5000 m times improved compared to the control group [38]. However, the number of articles investigating CST’s effect on knee proprioception is limited. The results of this research support the discoveries of Mutlu et al., who concluded that sedentary individuals who engaged in 10 weeks of instability resistance training using body weight displayed improved knee proprioception [17].
Comparing the Effect of CST and BT on Outcome Measures
According to our study, CSTG showed greater improvement than BTG regarding the PM reach distance of mSEBT and JPST at 60 degrees. On the other hand, BTG showed more improvement than CSTG in the Ant reach distance of mSEBT. However, when we analyzed both groups, no substantial difference was observed with the mean reduction of the absolute error at 30 degrees and the mean improvement of reach distance of mSEBT in the PL direction. In summary, the CSTG showed more improvement in proprioception than the BTG, while BT had a greater effect on the Ant direction in the mSEBT. On the other hand, CST had a greater effect on the posterior directions of mSEBT.
This study supports Aggarwal et al.’s findings that both CST and BT programs improved balance performance, but the CSTG had greater improvement than the BTG [39]. Unfortunately, the number of articles that have compared the effect of CST with BT on knee proprioception is scarce. This is one of the reasons for the novelty of the subject of this article, and it is suggested that more research be done in the field of finding the best type of exercise therapy in the field of multiple factors to minimize the likelihood of harm in sports players.
Possible Mechanisms of the Effect of CST and BT on Outcome Measures
Several variables could enhance JPST in CSTG and BTG. Despite the constant number of peripheral receptors, training might alter proprioception through central mechanisms [40]. Using physioball and wobble boards can create an unstable environment that can activate proprioceptors to help maintain balance and detect body position [41, 42]. Instability can lead to changes in balance, which, in turn, can lead to alterations in the length of the muscle-tendon unit, as well as in tension and neuromuscular activity. These changes can then affect one’s ability to perceive and react to alterations in balance [43-45]. Performing closed kinetic chain exercises, such as standing and kneeling on physioballs, involves movements that use multiple joints and planes. These movements help engage proprioceptors, which play a role in determining joint direction and position [46]. CST and BT can enhance the responsiveness of the feedback pathway, reduce the time taken to initiate movements, and enhance the accuracy of the sense of position [47]. Practicing on surfaces that are not stable could lead to an increase in co-contractile activity. This increase can help enhance motor control and balance [48]. Greater antagonist activity can be induced by resisting plantar flexion and leg extension in unstable conditions compared to stable conditions [49].
These mechanisms mentioned in both types of CST and BT can improve knee proprioception, but the reason why CST had a better effect on improving knee proprioception may be due to the presence of an additional mechanism, ie, the lumbosacral junction connects the spine to the lower extremities during sports. A stable core is essential for transferring force from the upper body to the lower body [50]. Core muscle stability may optimize lower extremity function and improve balance [51]. Strengthening core muscles improves body position and movement, leading to better proprioception. Core stability exercises can enhance joint proprioception in the lower limbs [52].
Also, CST can potentially improve spinal segment management and deep stabilizing muscles’ simultaneous contraction, ultimately leading to improved center of gravity management and optimal lumbopelvic control. Additionally, training the trunk muscles can improve lower extremity function and balance control by increasing neural recruitment patterns and activating the nervous system, promoting the concurrency of motor units, and reducing neural inhibitory reflexes during SEBT. The reason SEBT reach distance improves may be due to the activation of deep local muscles happening earlier than the activation of global abdominal muscles during lower extremity movement. Activating the spinal stabilizers early on establishes a firm foundation for lower body movement, enhancing the spine’s stiffness. It is possible that the training of deep stabilizers in CSTG contributed to creating such a stable base [53].
Study Limitations
The study is restricted by the minimal involvement of female athletes due to the spread of the coronavirus. Another constraint of this research is the age range of the participants examined (20–30 years); it is unclear whether all results occur younger or older than the study period. Another limitation of this research is assessing the dominant foot; it is better to perform the tests on the right and left foot and compare them. Also, it is better to use an isokinetic device to measure proprioception, which controls the speed and the sense of force and movement. This research did not involve extended follow-up and only focused on women, without comparing results with men. More research should be conducted on different groups of people in the future. Finally, it is better to conduct future studies with a follow-up period.
Conclusion
After evaluating the findings of this research, we can make the following inference: both CST and BT can effectively improve knee proprioception and dynamic balance in female amateur soccer players.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were performed after the study was approved by the Scientific Board and Ethics Committee of the School of Rehabilitation, Tehran University of Medical Sciences (Ethics committee reference number: IR.TUMS.FNM.REC.1399.012).
Funding
The present paper was extracted from the Master’s thesis of the first author, Department of Physiotherapy, School of Rehabilitation, Tehran University of Medical Sciences.
Authors' contributions
The authors contributed equally to preparing this paper.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the distance runners who participated in this study.
References
- Kiani A, Hellquist E, Ahlqvist K, Gedeborg R, Michaëlsson K, Byberg L. Prevention of soccer-related knee injuries in teenaged girls. Archives of Internal Medicine. 2010; 170(1):43-9. [DOI:10.1001/archinternmed.2009.289] [PMID]
- Bahr R, Holme I. Risk factors for sports injuries-a methodological approach. British Journal of Sports Medicine. 2003; 37(5):384-92. [DOI:10.1136/bjsm.37.5.384] [PMID]
- Bayramoglu M, Toprak R, Sozay S. Effects of osteoarthritis and fatigue on proprioception of the knee joint. Archives of Physical Medicine and Rehabilitation. 2007; 88(3):346-50. [DOI:10.1016/j.apmr.2006.12.024] [PMID]
- Thacker SB, Stroup DF, Branche CM, Gilchrist J, Goodman RA, Porter Kelling E. Prevention of knee injuries in sports. A systematic review of the literature. Journal of Sports Medicine and Physical Fitness. 2003; 43(2):165-79. [PMID]
- Evetovich TK, Nauman NJ, Conley DS, Todd JB. Effect of static stretching of the biceps brachii on torque, electromyography, and mechanomyography during concentric isokinetic muscle actions. The Journal of Strength & Conditioning Research. 2003; 17(3):484-8. [Link]
- Magalhães T, Ribeiro F, Pinheiro A, Oliveira J. Warming-up before sporting activity improves knee position sense. Physical Therapy in Sport. 2010; 11(3):86-90. [DOI:10.1016/j.ptsp.2010.06.001]
- Tayshete I, Akre M, Ladgaonkar Sh, Kumar A. Comparison of effect of proprioceptive training and core muscle strengthening on the balance ability of adolescent taekwondo athletes. International Journal of Health Sciences and Research. 2020; 10(6):268-79. [Link]
- Rahim AF, Sari GM, Rejeki PS. Difference influence of core stability exercise and ankle proprioceptive exercise toward dynamic balance on young adult overweight. Proceedings of the 2nd Health Science International Conference (HSIC 2019). 2020; 27-30. [Link]
- Alikhani R, Shahrjerdi S, Golpaigany M, Kazemi M. The effect of a six-week plyometric training on dynamic balance and knee proprioception in female badminton players. The Journal of The Canadian Chiropractic Association. 2019; 63(3):144-53. [PMID]
- Wong P, Hong Y. Soccer injury in the lower extremities. British Journal of Sports Medicine. 2005; 39(8):473-82. [DOI:10.1136/bjsm.2004.015511] [PMID]
- Ronga M, Grassi FA, Manelli A, Bulgheroni P. Tissue engineering techniques for the treatment of a complex knee injury. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2006; 22(5):576.e1-3. [DOI:10.1016/j.arthro.2005.12.050] [PMID]
- Rahnama N, Bambaeichi E, Daneshjoo A. The epidemiology of knee injuries in Iranian male professional soccer players. Sport Sciences for Health. 2009; 5(1):9-14. [DOI:10.1007/s11332-009-0070-1]
- Brodal P. The central nervous system. Oxford: Oxford University Press; 2010. [Link]
- Esmailnia M, Khalkhali Zavieh M, Naeimi SS. [Effect of balance exercises on lower limb joint proprioception: systematic review (Review Article) (Persian)]. Scientific Journal of Rehabilitation Medicine. 2017; 6(3):266-73. [Link]
- Daneshjoo A, Mokhtar AH, Rahnama N, Yusof A. The effects of comprehensive warm-up programs on proprioception, static and dynamic balance on male soccer players. Plos One. 2012; 7(12):e51568. [DOI:10.1371/journal.pone.0051568] [PMID]
- Pánics G, Tállay A, Pavlik A, Berkes I. Effect of proprioception training on knee joint position sense in female team handball players. British Journal of Sports Medicine. 2008. 42(6):472-6. [DOI:10.1136/bjsm.2008.046516] [PMID]
- Cuğ M, Ak E, Ozdemir RA, Korkusuz F, Behm DG. The effect of instability training on knee joint proprioception and core strength. Journal of Sports Science & Medicine. 2012; 11(3):468-74. [PMID]
- Hübscher M, Zech A, Pfeifer K, Hänsel F, Vogt L, Banzer W. Neuromuscular training for sports injury prevention: A systematic review. Medicine & Science in Sports & Exercise. 2010; 42(3):413-21. [PMID]
- Akuthota V, Ferreiro A, Moore T, Fredericson M. Core stability exercise principles. Current Sports Medicine Reports. 2008; 7(1):39-44. [PMID]
- Priyanka P, Nilima B, Parag S, Ashok S. Effects of lumbar core stability exercise programme on knee pain, range of motion, and function post anterior cruciate ligament reconstruction. Journal of Orthopaedics, Trauma and Rehabilitation. 2017; 23(1):39-44. [DOI:10.1016/j.jotr.2016.10.003]
- Filipa A, Byrnes R, Paterno MV, Myer GD, Hewett TE. Neuromuscular training improves performance on the star excursion balance test in young female athletes. Journal of Orthopaedic & Sports Physical Therapy. 2010; 40(9):551-8. [DOI:10.2519/jospt.2010.3325] [PMID]
- Sandrey MA, Mitzel JG. Improvement in dynamic balance and core endurance after a 6-week core-stability-training program in high school track and field athletes. Journal of Sport Rehabilitation. 2013; 22(4):264-71. [DOI:10.1123/jsr.22.4.264] [PMID]
- King M. Core stability: Creating a foundation for functional rehabilitation. Athletic Therapy Today. 2000; 5(2):6-13. [DOI:10.1123/att.5.2.6]
- Samson KM. The effects of a five-week core stabilization-training program on dynamic balance in tennis athletes. [MA thesis]. Virginia: West Virginia University; 2005. [Link]
- Fredericson M, Moore T. Muscular balance, core stability, and injury prevention for middle- and long-distance runners. Physical Medicine and Rehabilitation Clinics of North America. 2005; 16(3):669-89. [DOI:10.1016/j.pmr.2005.03.001] [PMID]
- Lust KR, Sandrey MA, Bulger SM, Wilder N. The effects of 6-week training programs on throwing accuracy, proprioception, and core endurance in baseball. Journal of Sport Rehabilitation. 2009; 18(3):407-26. [PMID]
- Jeffreys I. Developing a progressive core stability program. Strength & Conditioning Journal. 2002; 24(5):65-6. [DOI:10.1519/00126548-200210000-00017]
- McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. The American Journal of Sports Medicine. 2006; 34(7):1103-11. [DOI:10.1177/0363546505284191] [PMID]
- Pour Kazemi F, Naseri N, Bagheri H, Fakhari Z. [Reliability of a system consists of skin markers, digital photography, and AutoCAD software for measuring the knee angles (Persian)]. Journal of Modern Rehabilitation. 2009; 2(3 and 4):19-24. [Link]
- Levangie PK, Norkin CC. Joint structure and function: A comprehensive analysis. Philadelphia: FA. Davis Company; 2011. [Link]
- Lafortune MA, Lambert C , Lake M. Skin marker displacement at the knee joint. Journal of Biomechanics. 1993; 26(3):299. [DOI:10.1016/0021-9290(93)90408-7]
- Kim HY. The examination of reliability of lower limb joint angles with free software imageJ. Journal of the Ergonomics Society of Korea. 2015; 34(6):583 -95. [DOI:10.5143/JESK.2015.34.6.583]
- Romero-Franco N, Jiménez-Reyes P. Effects of warm-up and fatigue on knee joint position sense and jump performance. Journal of Motor Behavior. 2017; 49(2):117-22. [PMID]
- Onofrei RR, Amaricai E, Petroman R, Suciu O. Relative and absolute within-session reliability of the modified Star Excursion Balance Test in healthy elite athletes. PeerJ. 2019; 7:e6999. [DOI:10.7717/peerj.6999] [PMID]
- Cabanas-Valdés R, Boix-Sala L, Grau-Pellicer M, Guzmán-Bernal JA, Caballero-Gómez FM, Urrútia G. The effectiveness of additional core stability exercises in improving dynamic sitting balance, gait and functional rehabilitation for subacute stroke patients (CORE-Trial): Study protocol for a randomized controlled trial. International Journal of Environmental Research and Public Health. 2021; 18(12):6615. [PMID]
- Bahrami F, Sabbagh Langeroudi M. [Comparison of the effects of core stability and trampoline exercises on static and dynamic balance, and ankle proprioception in female volleyball players with chronic ankle instability (Persian)]. Journal of Sport Biomechanics. 2023; 9(2):140-54. [DOI:10.61186/JSportBiomech.9.2.140]
- Kahle NL, Gribble PP. Care stability training in dynamic balance testing among young, healthy adults. Athletic Training & Sports Health Care. 2009; 1(2):65-73. [DOI:10.3928/19425864-20090301-03]
- Sato K, Mokha M. Does core strength training influence running kinetics, lower-extremity stability, and 5000-M performance in runners? Journal of Strength and Conditioning Research. 2009; 23(1):133-40. [DOI:10.1519/JSC.0b013e31818eb0c5] [PMID]
- Ashton-Miller JA, Wojtys EM, Huston LJ, Fry-Welch D. Can Proprioception Really Be Improved By Exercises? Knee Surgery, Sports Traumatology, Arthroscopy. 2001; 9(3):128-36. [PMID]
- Cooke JD. The role of stretch reflexes during active movements. Brain Research. 1980; 181(2):493-7. [DOI:10.1016/0006-8993(80)90636-8] [PMID]
- Verhagen EA, van Tulder M, van der Beek AJ, Bouter LM, van Mechelen W. An economic evaluation of a proprioceptive balance board training programme for the prevention of ankle sprains in volleyball. British Journal of Sports Medicine. 2005; 39(2):111-5. [DOI:10.1136/bjsm.2003.011031] [PMID]
- Anderson K, Behm DG. The impact of instability resistance training on balance and stability. Sports Medicine. 2005; 35(1):43-53. [PMID]
- Heitkamp HC, Horstmann T, Mayer F, Weller J, Dickhuth HH. Gain in strength and muscular balance after balance training. International Journal of Sports Medicine. 2001; 22(04):285-90. [DOI:10.1055/s-2001-13819] [PMID]
- Magnusson SP, Simonsen EB, Aagaard P, Kjaer M. Biomechanical responses to repeated stretches in human hamstring muscle in vivo. The American Journal of Sports Medicine. 1996; 24(5):622-8. [DOI:10.1177/036354659602400510] [PMID]
- Rogol IM, Ernst G, Perrin DH. Open and closed kinetic chain exercises improve shoulder joint reposition sense equally in healthy subjects. Journal of Athletic Training. 1998; 33(4):315-8. [PMID]
- Mirjamali E, Minoonejad H, Seidi F, Samadi, H. (2019). [Comparison of the effects of core stability training on stable and unstable levels on the static and dynamic balance of female athletes with trunk dysfunction (Persian)]. The Scientific Journal of Rehabilitation Medicine. 2019; 8(1):61-70. [DOI:10.22037/jrm.2018.111331.1920]
- Sparkes R, Behm DG. Training adaptations associated with an 8-week instability resistance training program with recreationally active individuals. The Journal of Strength & Conditioning Research. 2010; 24(7):1931-41. [DOI:10.1519/JSC.0b013e3181df7fe4] [PMID]
- Engelhorn R. Agonist and antagonist muscle EMG activity pattern changes with skill acquisition. Research Quarterly for Exercise and Sport. 1983; 54(4):315-23. [DOI:10.1080/02701367.1983.10605315]
- Willardson JM. Core stability training for healthy athletes: A different paradigm for fitness professionals. National Strength and Conditioning Association. 2007; 29(6):42-9. [Link]
- Kumar S, Sharma VP, Shikla R, Dev R, Pal Singh Negi M. Assessment of back and abdominal pressure, sexual frequency and quality of life. International Journal of Therapy and Rehabilitation. 2009; 16(11):615-24. [DOI:10.12968/ijtr.2009.16.11.44943]
- Balba AE, Alaa IE, Ahmed H, Mohammed MM. Effect of core stability training on knee proprioception after anterior cruciate ligament reconstruction. The Medical Journal of Cairo University. 2018; 86(March):231-40. [DOI:10.21608/mjcu.2018.55091]
- Hadadnezhad M, Rajabi R, Alizadeh MH, Letafatkar A. [Does core stability predispose female athletes to lower extremity injuries? (Persian)] Journal of Research in Rehabilitation Sciences. 2010; 6(2):89-98. [Link]
- Aggarwal A, Zutshi K, Munjal J, Kumar S, Sharma V. Comparing stabilization training with balance training in recreationally active individuals. International Journal of Therapy and Rehabilitation. 2010; 17(5):244-53. [DOI:10.12968/ijtr.2010.17.5.47843]
Type of Study: Original |
Subject:
Physical Therapy
Received: 8/03/2024 | Accepted: 17/08/2024 | Published: 1/01/2025
Received: 8/03/2024 | Accepted: 17/08/2024 | Published: 1/01/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |