Volume 25, Issue 4 (Winter 2025)
jrehab 2025, 25(4): 824-847 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nemati Z, Jalali M, Sanjari M A, Bagherifard A. The Effect of Hybrid Knee Brace on Kinesiophobia, Proprioception, and Coping Ability After Acute Anterior Cruciate Ligament Rupture: A Pilot Randomized Trial. jrehab 2025; 25 (4) :824-847
URL: http://rehabilitationj.uswr.ac.ir/article-1-3415-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3415-en.html
1- Department of Orthotics and Prosthetics, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Department of Orthotics and Prosthetics, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,jalali.m@iums.ac.ir
3- Department of Basic Rehabilitation Sciences, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafa Yahyaeian Orthopedics Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthotics and Prosthetics, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Basic Rehabilitation Sciences, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafa Yahyaeian Orthopedics Hospital, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 3351 kb]
(621 Downloads)
| Abstract (HTML) (5380 Views)
Full-Text: (907 Views)
Introduction
The anterior cruciate ligament rupture (ACL) is a common knee joint injury. This injury results in anterior laxity of the tibiofemoral joint, leading to repeated knee instability and early-onset osteoarthritis [1]. After an injury, some people can return to the activity level before the injury, which is called copers. However, some are unable to resume previous activities due to recurrent knee giving way and kinesiophobia. They are classified as non-copers and are potential candidates for ligament reconstruction surgery [2]. To assess an individual’s capacity for adaptation to the injury, Fitzgerald et al. developed a screening test based on the dynamic stability of the knee joint during various activities [3]. Those achieving a satisfactory score on this test are categorized as copers to the injury, while those failing to do so are placed in the non-coper group [3]. The criteria for satisfactory performance include achieving at least 80% of the score on the 6-m jump test [4], scoring at least 80% on the KOS-ADL (knee outcome survey’s activities of daily living scale) questionnaire, attaining a minimum of 60 points on the Global rating of knee function [5], and experiencing a maximum of one episode of knee giving-way since the time of injury [6].
One of the factors influencing the ability to adapt to injury in these individuals is neuromuscular coordination [7], which is disrupted by the loss of afferent feedback from the ACL [8]. The absence of feedback also leads to a reduction in knee proprioception [9], which is a primary contributor to knee instability in injury non-adaptive patients [10]. To improve the neuromuscular system, perturbation training is typically performed on balance boards once acute symptoms subside, involving anterior-posterior and internal-external perturbations as well as multi-directional perturbations [11]. However, such interventions are not conducted due to the instability experienced during the acute injury phase [12]. Since skin receptors around the knee transmit vital information regarding joint position and movements, stimulating these receptors can partially compensate for the proprioceptive deficit resulting from ligament rupture [13].
To enhance neuromuscular function and dynamic stability, stimulating joint capsule receptors and muscles surrounding the knee can also be beneficial [14، 15]. Studies indicate that knee braces have effects such as increasing knee proprioception through skin contact [16] and applying pressure on underlying muscles and the joint capsule [17، 18], consequently altering the timing and movement patterns of lower limb muscles [19]. Strutzenberger and Delincé et al. reported that using flexible structures like elastic sleeves in individuals with complete ACL ruptures leads to improved proprioception [20، 21] and increased brain activity in the primary sensorimotor cortex, responsible for processing sensory input, thus enhancing the proprioception. Therefore, knee braces and elastic sleeves can enhance knee proprioception and neuromuscular function in individuals with complete ACL rupture [22].
Another factor influencing the ability to adapt to injury following an ACL rupture is kinesiophobia. Individuals who successfully adapt to the injury typically exhibit lower levels of kinesiophobia [23]. While psychological factors also play a role in the development of kinesiophobia [24], increasing the mechanical stability of the knee can help mitigate it [22، 23]. Brisson et al. demonstrated that knee braces could enhance knee stability post-ACL rupture [25]. Similarly, Harput et al.’s study indicates that employing a knee brace after ligament reconstruction surgery reduced kinesiophobia [22]. Based on the existing literature, no study has investigated the effect of brace usage during the acute phase following an ACL rupture on enhancing coping rates. Therefore, this study aims to explore the impact of employing a hybrid knee brace (Figure 1), comprising a custom-made functional brace and an elastic sleeve, on kinesiophobia, proprioception, and its overall effect on the ability to adapt to the injury during the acute stage following an ACL rupture.

Materials and Methods
The present study is a single-blind randomized clinical trial conducted on 30 individuals with acute ACL rupture. The samples were selected based on availability and randomly assigned using permutation blocks (four blocks of four) into control and experimental groups [26]. Participants remained unaware of the process and the existence of the other group. The sample size was determined using G*Power software version 3.1.9.2, with a confidence level of 95%, a power of 80%, and an effect size of 0.8, which was derived from a similar study [27]. This calculation yielded 13 individuals in each group. However, to account for a potential 15% drop in the sample, the number increased to 15 individuals in each group. Ethical approval for this study was obtained from the Iran University of Medical Sciences Ethics Committee and registered in the Iranian Registry of Clinical Trial (IRCT). All participants provided informed consent by signing the consent form before participating in the study.
A specialized knee surgeon selected samples from the knee orthopedic clinic at Shafa Yahyaeian Orthopedics Hospital, Tehran City, Iran. Subsequently, they were randomly assigned into two groups: control (without orthosis) and experimental (with orthosis). Both groups followed an identical physiotherapy program, consisting of 10 sessions to increase knee range of motion, reduce swelling, and perform strengthening exercises for the quadriceps and hamstring muscles. These sessions were conducted uniformly by an experienced therapist for both groups. At the initial physiotherapy sessions, individuals experiencing swelling were treated with compression bandaging to reduce swelling.
If necessary, devices like transcutaneous electrical nerve stimulation and pulsed ultrasound were utilized. Since quadriceps muscles undergo inhibition after ACL rupture, early strengthening of these muscles is crucial. However, hamstring muscles should also be strengthened as these muscles act as antagonists to the ACL. Quadriceps muscle strengthening was conducted using devices such as a Faradic or functional electrical stimulation device and Q-set exercises. The exercises provided to patients at this stage consisted of closed and open kinetic chain exercises [28، 29]. During the first two weeks, exercises within the range of 30 to 60 degrees of knee flexion were performed. Patellar bone mobilization was performed to increase the knee’s range of motion. In the following two weeks, exercises were performed within a larger range of motion. Upon completing the physiotherapy sessions, the physiotherapist provided a satisfactory status report regarding muscle strength, area swelling, and sufficient range of motion for patients to undergo functional tests.
The inclusion criteria of this study encompassed patients aged 18 to 40 years who presented with an isolated and unilateral tear of the ACL, confirmed through magnetic resonance imaging (MRI). These individuals should have maintained a moderate activity level before the injury, indicated by a score of 3-5 on the Tegner scale [30]. Furthermore, they should have no history of fractures or surgeries in the knee area and no prior damage to the ACL or other ligaments of the knee joint. The exclusion criteria comprised individuals who experienced pain or inflammation in the knee during functional tests or those who declined to continue cooperating with the study’s rehabilitation protocol.
The participants underwent evaluation in two sessions. During the first session, they completed the KOS-ADL questionnaire [5], the global rating of knee function [31], and the Tampa questionnaire [32]. The KOS-ADL scale is a self-report tool designed to assess performance limitations in patients experiencing various knee conditions, including ligament and meniscus injuries, patellofemoral pain, and knee osteoarthritis. This questionnaire comprises sections for measuring symptoms and functional limitations during daily activities. Specifically, the section related to daily activities measurement consists of 14 questions. Six questions pertain to the impact of impairment on the ability to perform daily activities, while the remaining 8 focus on the effect of knee impairment on specific tasks. Each question offers five response options, scored from 0 to 5. A score of 0 denotes no difficulty in performing the activity, while a score of 5 indicates inability to perform the activity. The maximum achievable score is 70. The total score is converted to a percentage by dividing by 70 and multiplying by 100. The validity and reliability of this questionnaire were investigated by Irrgang et al. in 1998 [33].
Additionally, a study conducted by Salvati et al. demonstrated that the Persian version of this questionnaire is valid and reliable for use in Iranian society [34]. The global rating of knee function represents the current performance of the knee in comparison to its state before the injury. It is assessed using the visual analog scale (VAS), ranging from 0 to 100 [31].
The Tampa questionnaire assesses the pain associated with fear, accompanied by avoidance and restriction of behavior, movement, and physical activities initiated by the individual. It comprises 17 questions rated on a 4-point Likert scale with responses ranging from 1= “completely disagree” to 4= “completely agree.” Upon completion by the patient, a total score between 17 and 68 is calculated. Scores below 37 indicate a low kinesiophobia, while scores exceeding 37 suggest a high kinesiophobia. The minimum clinically important difference for kinesiophobia is reported to be a 4-point reduction [35]. The Persian translation of the Tampa questionnaire was conducted by Jafari et al., who measured and evaluated the psychometric properties of the Persian version. The results indicated that the Persian version of the Tampa kinesiophobia scale is valid and reliable for Iranian society [36].
Four weeks after enrollment in the study, the participants were summoned to the Research Institute of Physical Education and Sports Sciences under the Ministry of Science, Research and Technology in Tehran to undergo functional tests. Adaptation to the injury was assessed through a screening test, while the sense of joint position was evaluated using the Biodex dynamometer device [37]. The screening test comprised 4 conditions: achieving a score of at least 80% on the six-meter jump test, obtaining a score of at least 80% on the daily activities questionnaire, attaining a score of at least 60% on the overall knee function assessment, experiencing at least one instance of knee instability following the initiation of treatment [3].
The joint position sense was assessed using the Biodex System Pro 3 dynamometer (Shirley, New York, USA), initially in the healthy knee and subsequently in the injured knee. This device has been validated and proven reliable for measuring joint position sense [37]. Proper positioning of the individual in the Biodex machine involved aligning the knee’s movement axis with the dynamometer’s mechanical axis. Additionally, the dynamometer seat was adjusted to an 85-degree flexion angle, and the knee’s range of motion was set from full extension to 90 degrees of flexion. The end of the knee connecting lever was positioned above the ankles and secured with a strap. The individual’s torso was also stabilized using shoulder, waist, and thigh straps. Before commencing the test, leg torque produced at a 30-degree knee flexion angle was recorded to negate the effects of gravity. Furthermore, to minimize the influence of other muscles, the individual maintained crossed arms on the chest [38]. For the joint position test with closed eyes, the knee was passively moved from 90° flexion to 60° flexion using the lever arm of the device and returned to the initial position after 4 seconds. Subsequently, participants were instructed to reproduce the bending angle with their eyes closed actively. Following two experimental repetitions, three tests were recorded for each side.
The hybrid brace used in the experimental group consisted of a functional brace and an elastic sleeve (Figure 1). The functional component comprised a posterior femoral cuff and an anterior shin cuff of 2.5-mm thick polypropylene. These components were designed to enhance anterior-posterior stability and were custom-made for each patient based on limb measurements. In individuals with ACL rupture, anterior and posterior instability leads to anterior tibial displacement relative to the femur during walking [10، 39]. Thus, positioning the shin cuff anteriorly and the thigh cuff posteriorly prevents this displacement. The midpoint between the hip trochanter and the external condyle of the femur corresponded to the location of the femoral cuff, while the midpoint between the head of the fibula and the lateral malleolus aligned with the position of the tibial cuff. The polycentric knee joint, constructed from aluminum and featuring a gear model, allows free joint movement. This joint was aligned with the knee’s movement axis, ensuring optimal functionality. From a lateral perspective, the knee brace’s joint location is aligned with the knee’s anatomical axis.
Additionally, elastic straps were employed to minimize functional knee brace slippage. The elastic straps, capable of greater stretch than non-elastic ones, provide increased orthotic adhesion, thereby reducing downward slippage. The ACL plays a significant role in controlling valgus force and preventing instability on the medial side of the knee joint [40]. Consequently, ACL damage results in internal knee joint instability. The external load of the knee brace counteracts valgus force and mitigates internal instability post-ACL rupture [41، 42]. This outcome is achieved by applying three pressure points generated by the upper and lower ends of the lateral upright and the knee pad’s mutual force on the inner aspect of the knee (Figure 1). The orthotic joint was linked to the upper and lower cuff via lateral upright in this brace. Strap tension varied to accommodate proper suspension and individual tolerance levels, as indicated by skin redness assessment 15 minutes after brace removal. The applied pressure was deemed appropriate if redness disappeared within 20 minutes [43]. Underneath the functional brace, patients wore a Tynor® neoprene sleeve that provided complete contact with the knee, exerting pressure on underlying structures. Sleeve size was determined individually by measuring knee circumference and utilizing the sleeve guide. Patients were instructed to wear the hybrid brace for a minimum of four hours daily and record the duration of use.
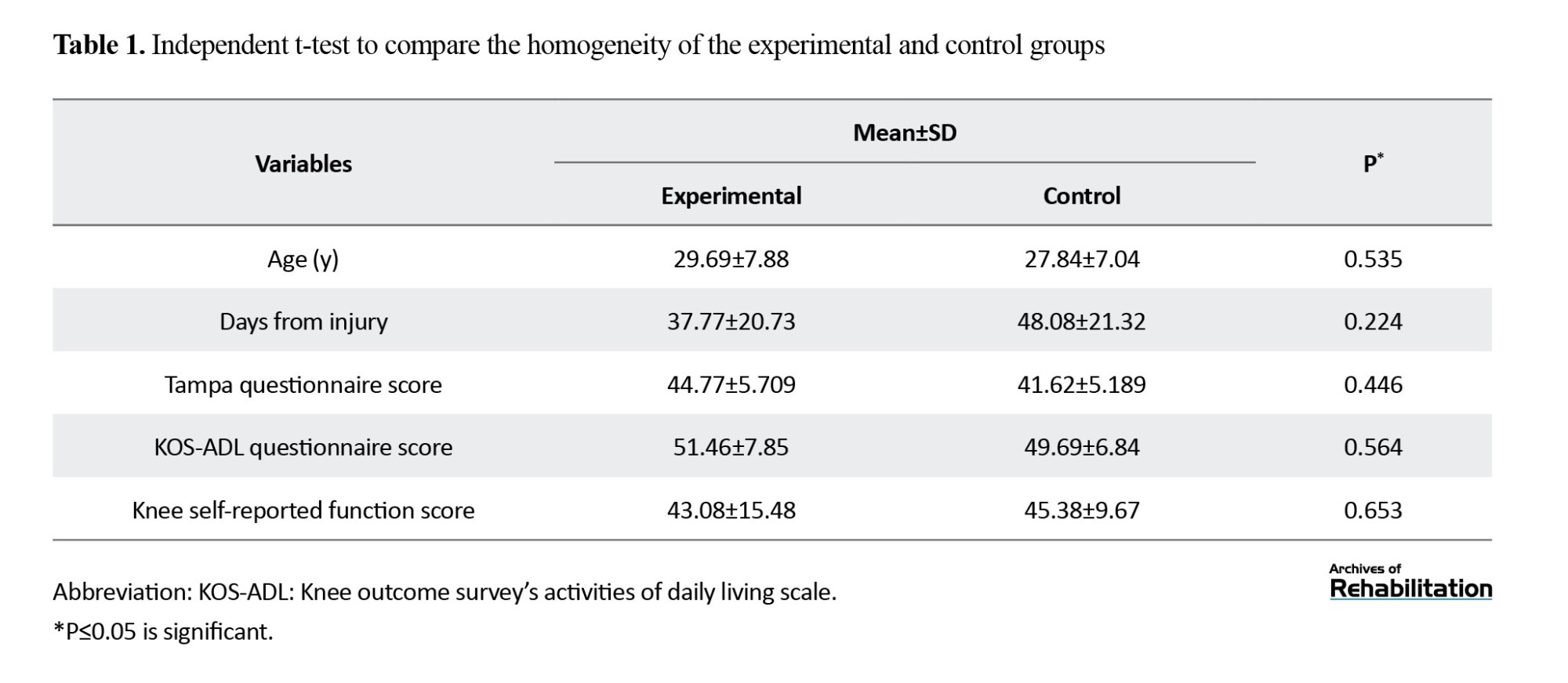
SPSS statistical software, version 22 was employed for data analysis, with the normality of data distribution assessed using the Shapiro-Wilk test. All data exhibited normal distribution except for the performance report, which was normalized by excluding one outlier data point. An independent t test was utilized to assess the homogeneity of the two groups concerning age, scores on the Tampa and daily activity questionnaires, and the global rating of knee function scores at the study’s outset.
Mixed within-between analysis of variance (ANOVA) was employed to evaluate the KOS-ADL questionnaire, global rating of knee function report, and Tampa questionnaire within and between groups. The Chi-square test was conducted to compare the proportion of copers and non-copers. The Spearman correlation test was employed to investigate the relationship between coping ability and proprioception and the association between kinesiophobia and proprioception. A significance level of 0.05 was established.
Furthermore, an independent t test was conducted to compare the absolute joint position sense error, which was used to measure joint position sense, between the test, control, and coper and non-coper groups.
Results
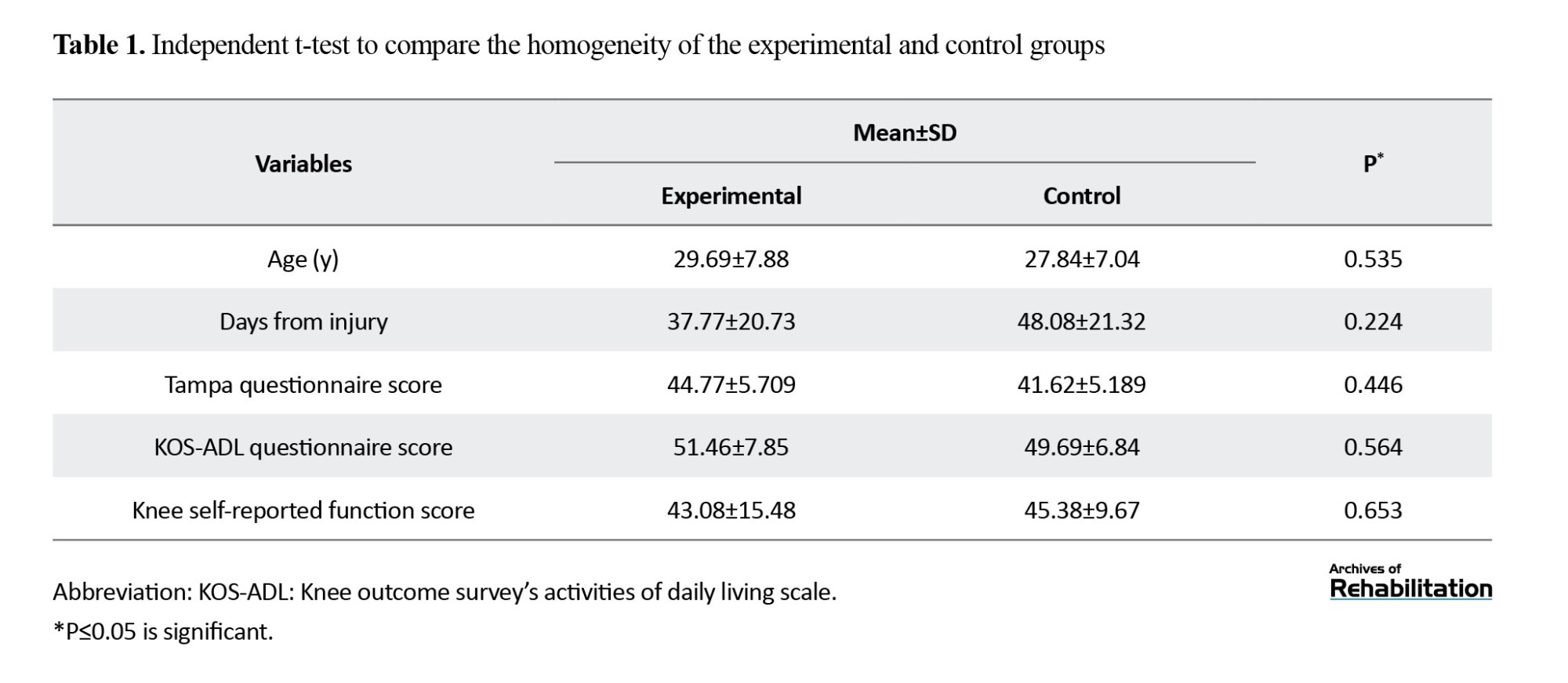
The study included 30 individuals diagnosed with isolated ACL tears. However, two individuals were excluded from the study because they did not utilize a brace, while the other two were excluded for failing to attend all physiotherapy sessions. Consequently, 26 individuals were chosen to partake in the study, divided into two groups, with 13 participants in each group. Before the study’s commencement, the two groups were matched based on age, time of injury, fear of movement level, daily activity, and knee function, as outlined in Table 1.
The Effects of Using a Hybrid Brace on Kinesiophobia, Knee Function, and Daily Activities
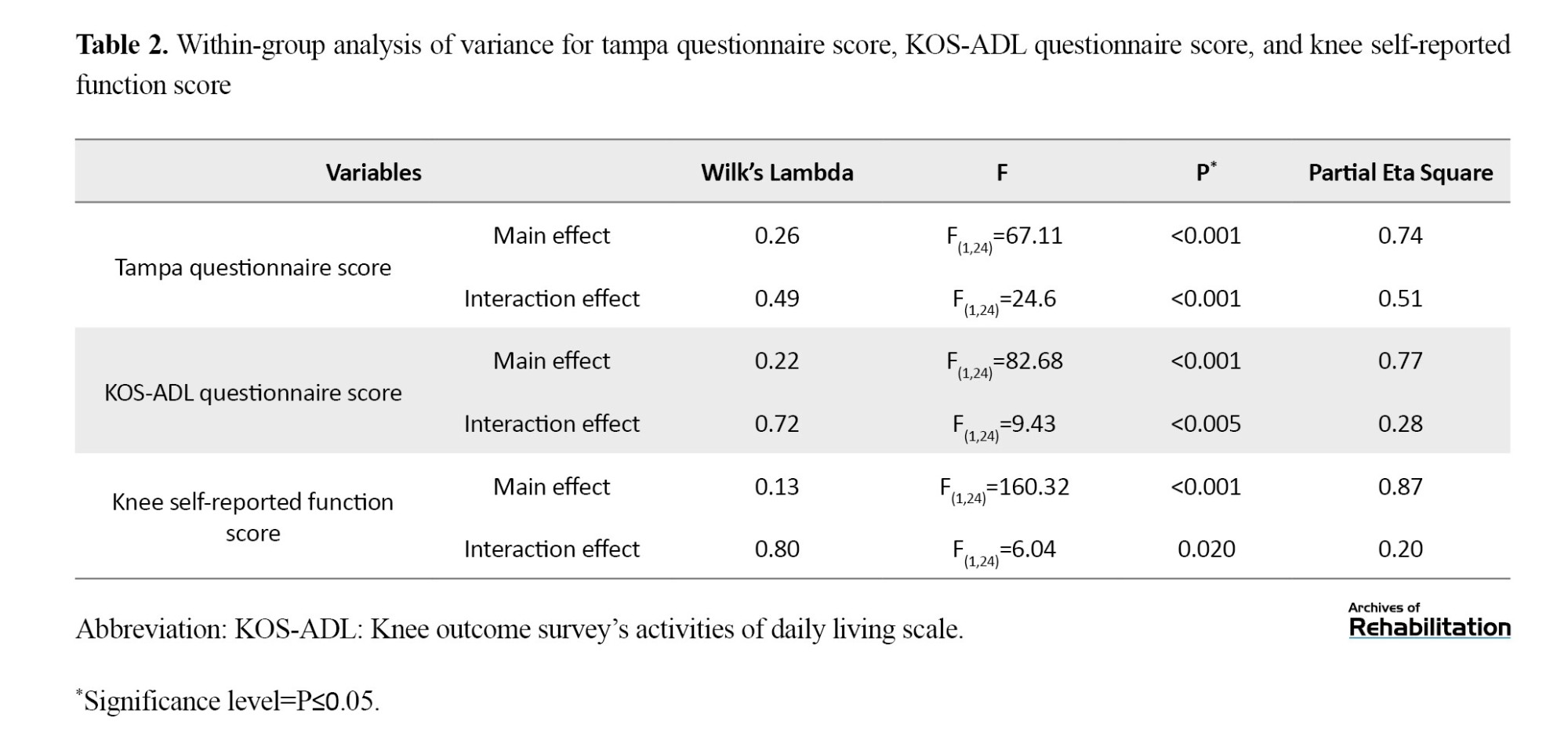
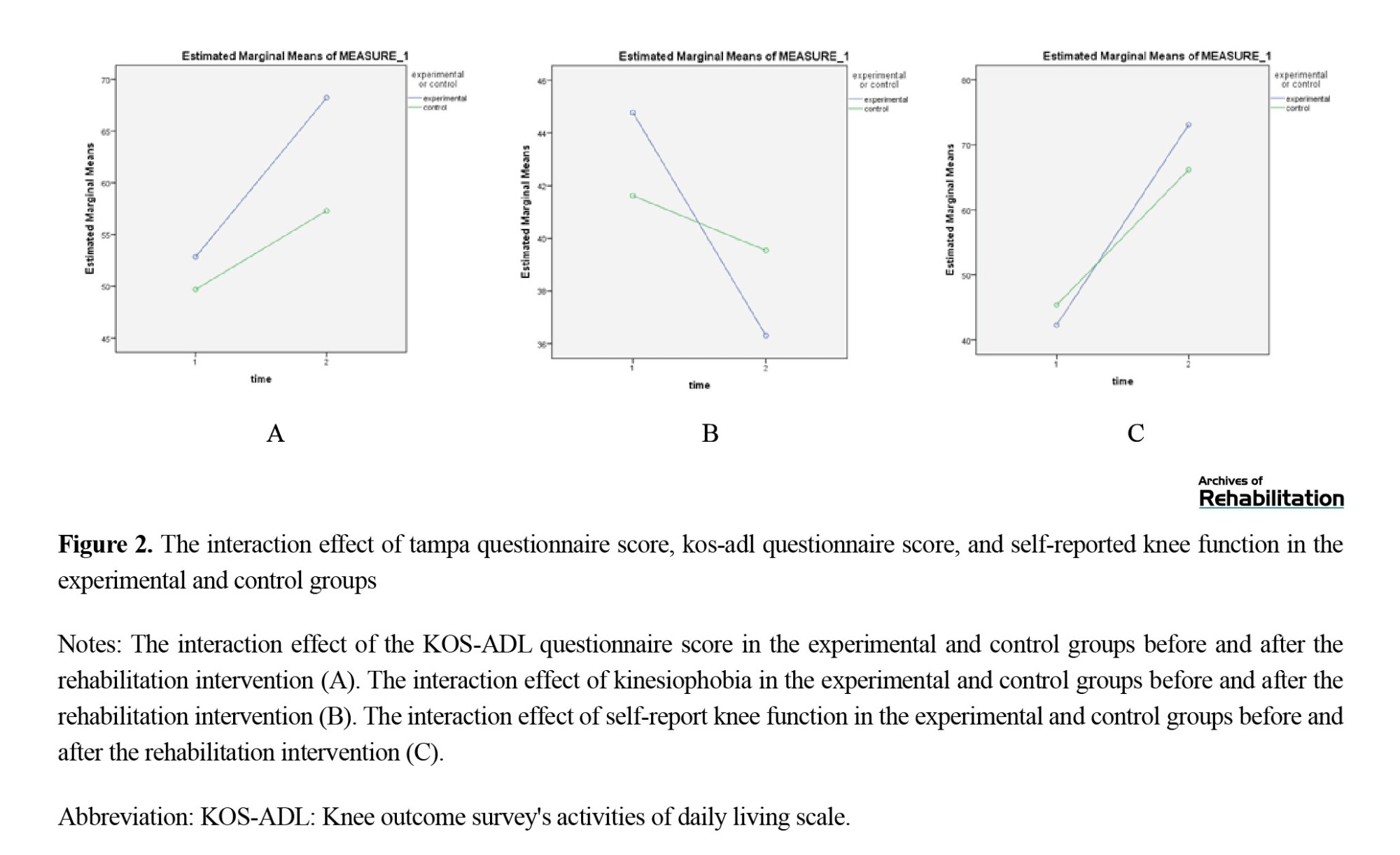
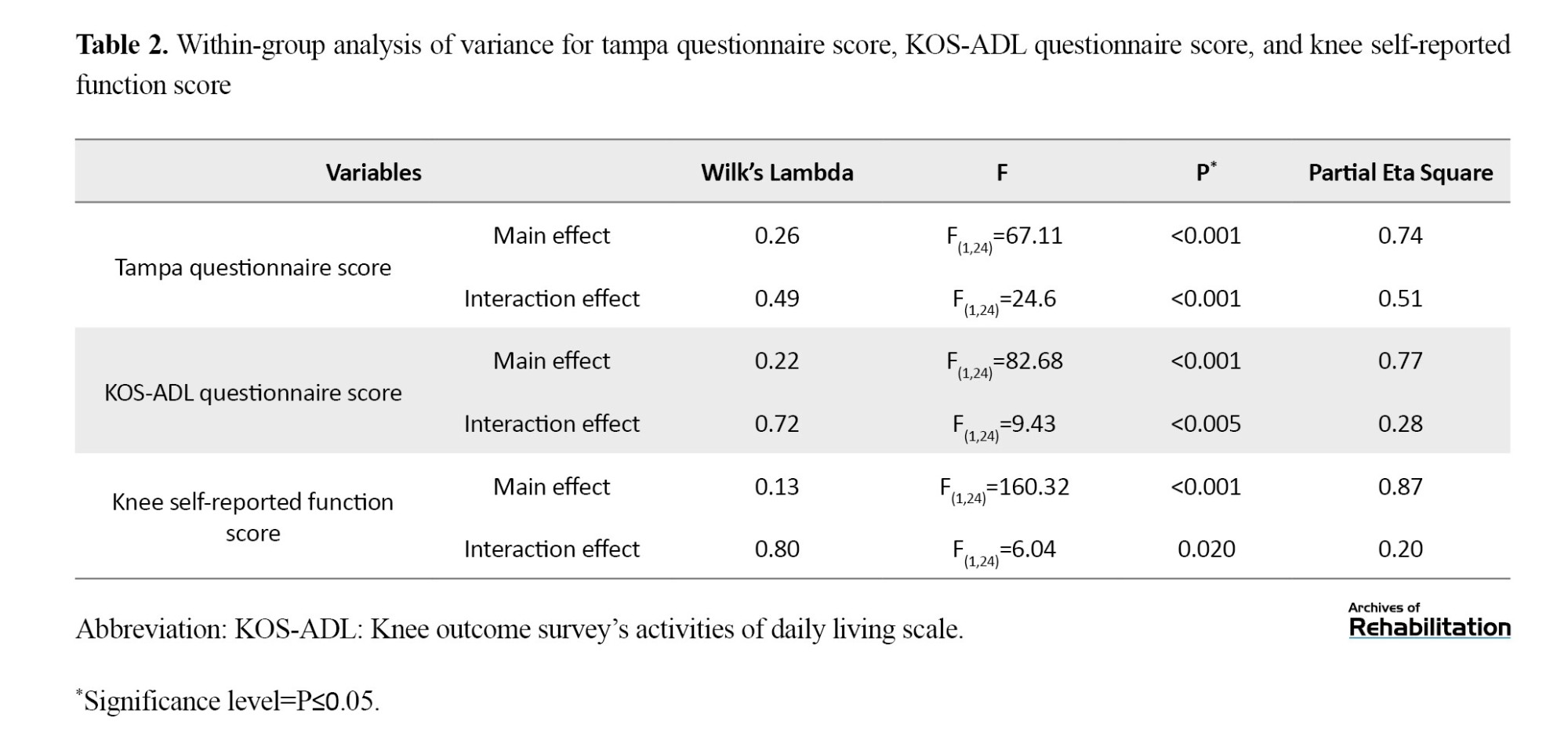
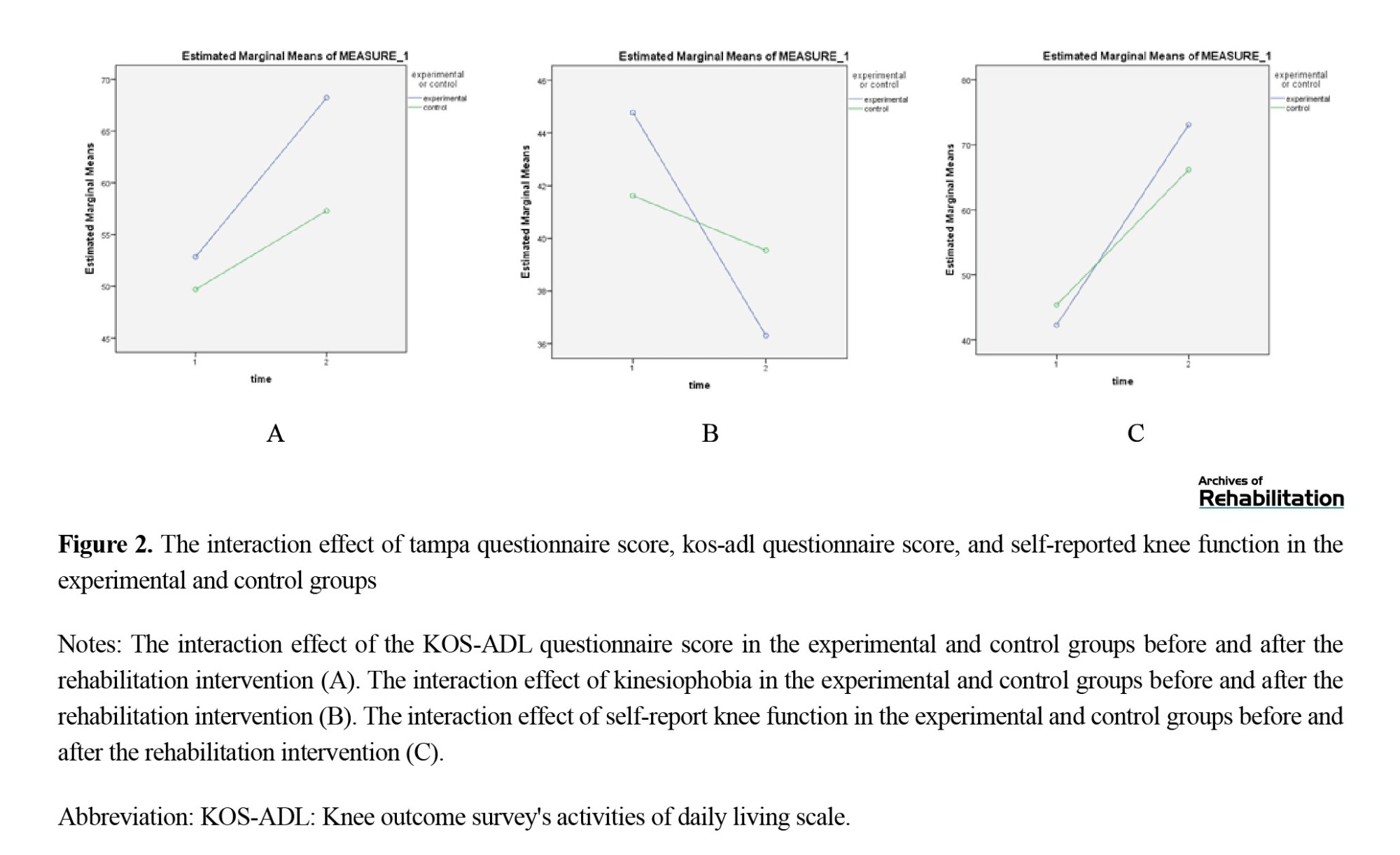
A mixed within-between analysis of variance was conducted to assess the impact of utilizing a hybrid knee orthosis on kinesiophobia, knee function, and daily activities. The within-group analysis of variance results indicated a significant difference between pre- and post-intervention outcomes across all three variables, with improvements observed in the scores of each variable following the intervention in both groups (demonstrating a significant main effect of the variables). Additionally, the interaction effect of all three variables (Tampa questionnaire, daily activities measurement questionnaire, and knee self-reported performance) was found to be significant in both groups (Table 2), indicating that the positive changes in all three variables were more pronounced in the test group compared to the control group (Figure 2).
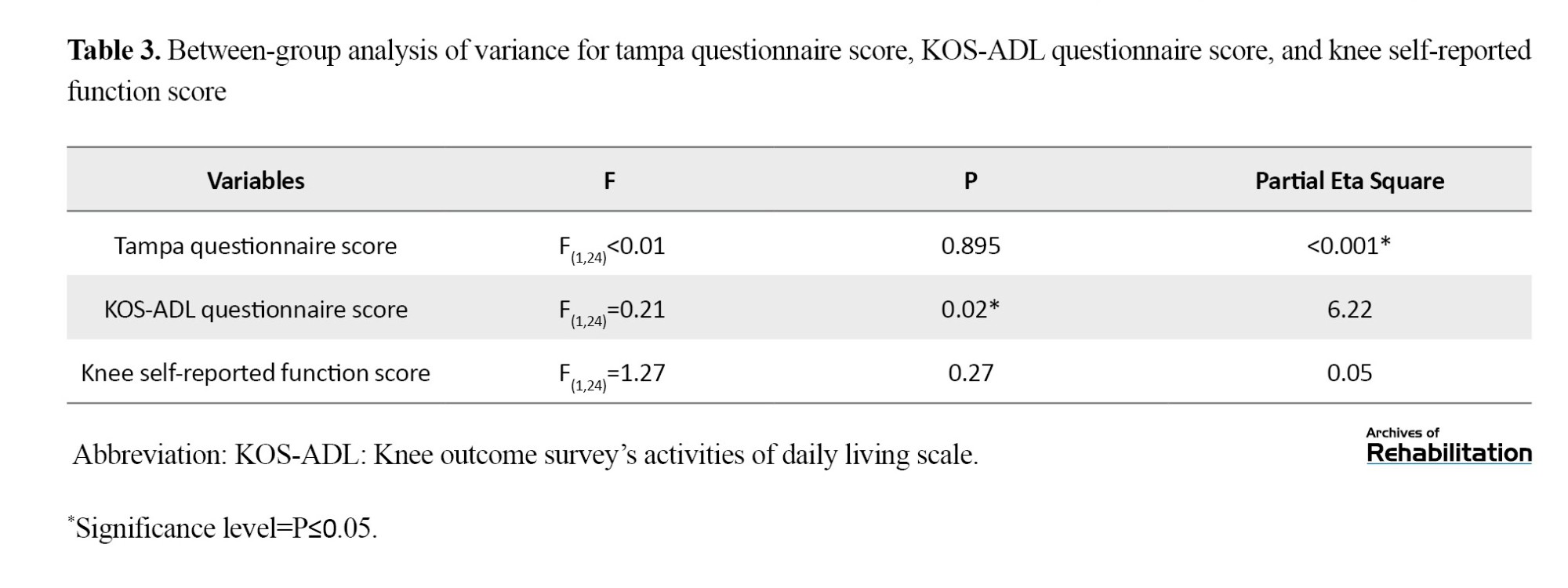
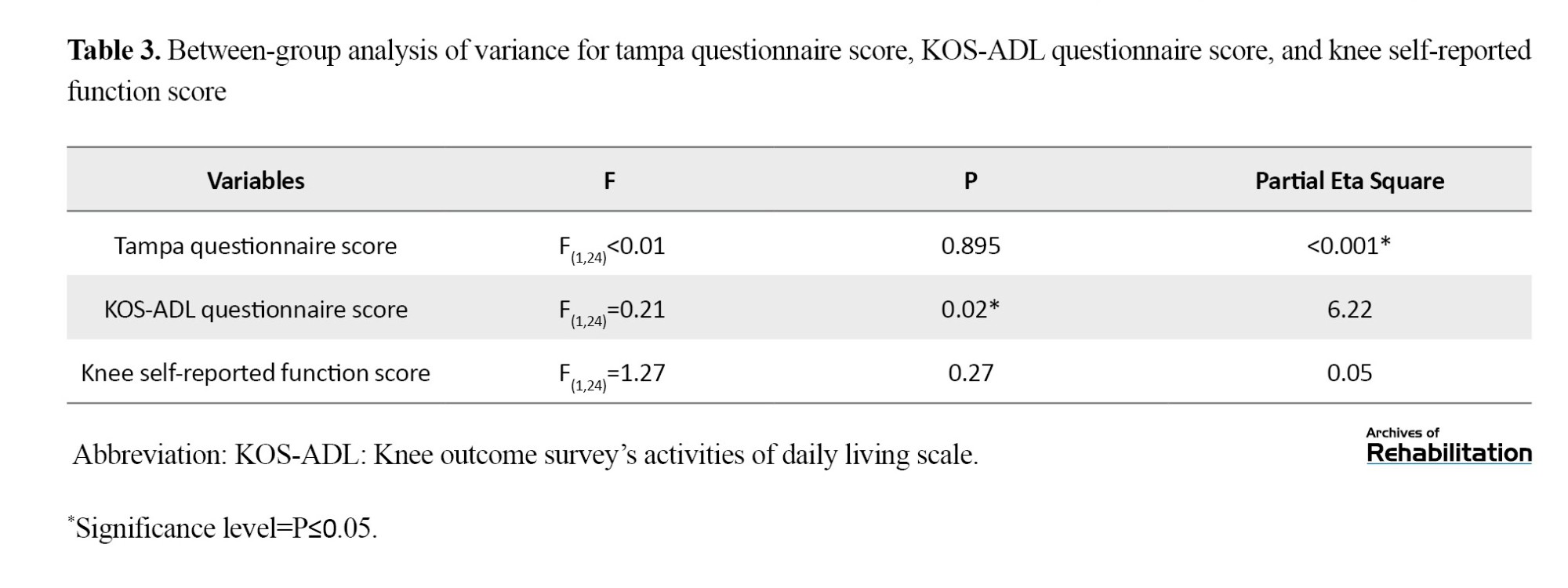
Regarding between-group analysis concerning kinesiophobia and knee function, no significant differences were observed between the two groups (Table 3). However, regarding the score of the daily activities questionnaire, a significant difference was noted between the two groups (P=0.020) (Table 3).
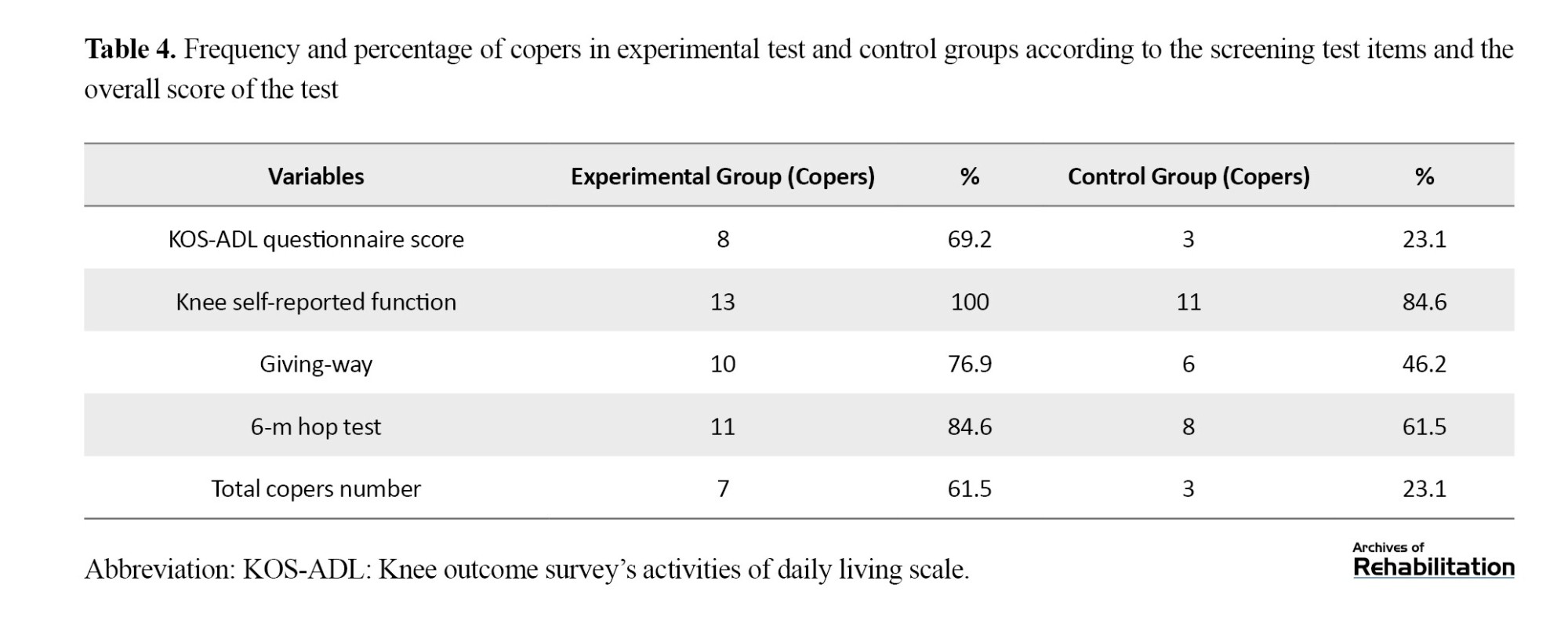
Determining the Frequency and Percentage of Copers in Each Group, Separately For Each Component of the Screening Test, and the Final Score of the Test
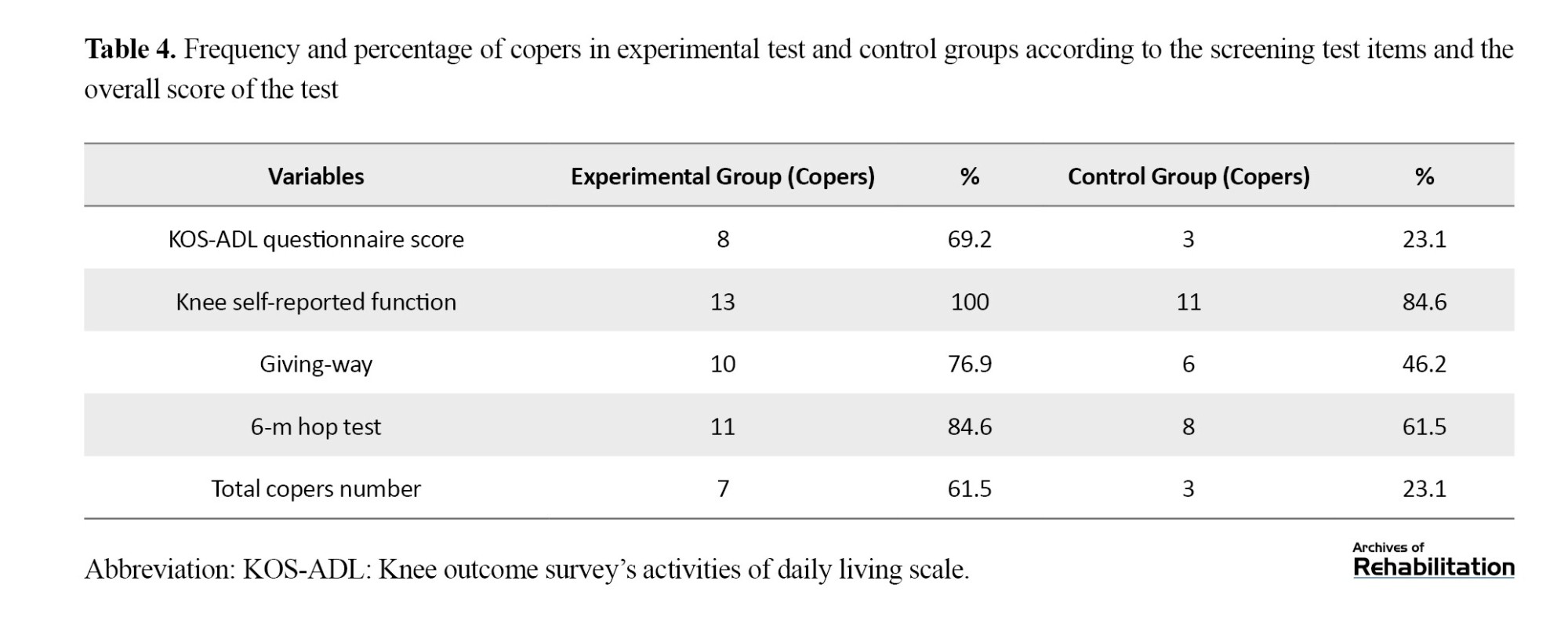
Table 3 displays the frequency and percentage of copers in each group, separately by each component of the screening test, along with the final score. Eight individuals in the test group and 3 in the control group exhibited coping (61.5% vs 23.1%) (Table 4).
In Table 5, the relationship between the proportion of copers based on each test and the proportion of copers based on all the tests is reported using the Chi-square test. According to this Table, the score of the KOS-ADL questionnaire exhibits the highest correlation with the final result of the screening test (φ= 0.92).
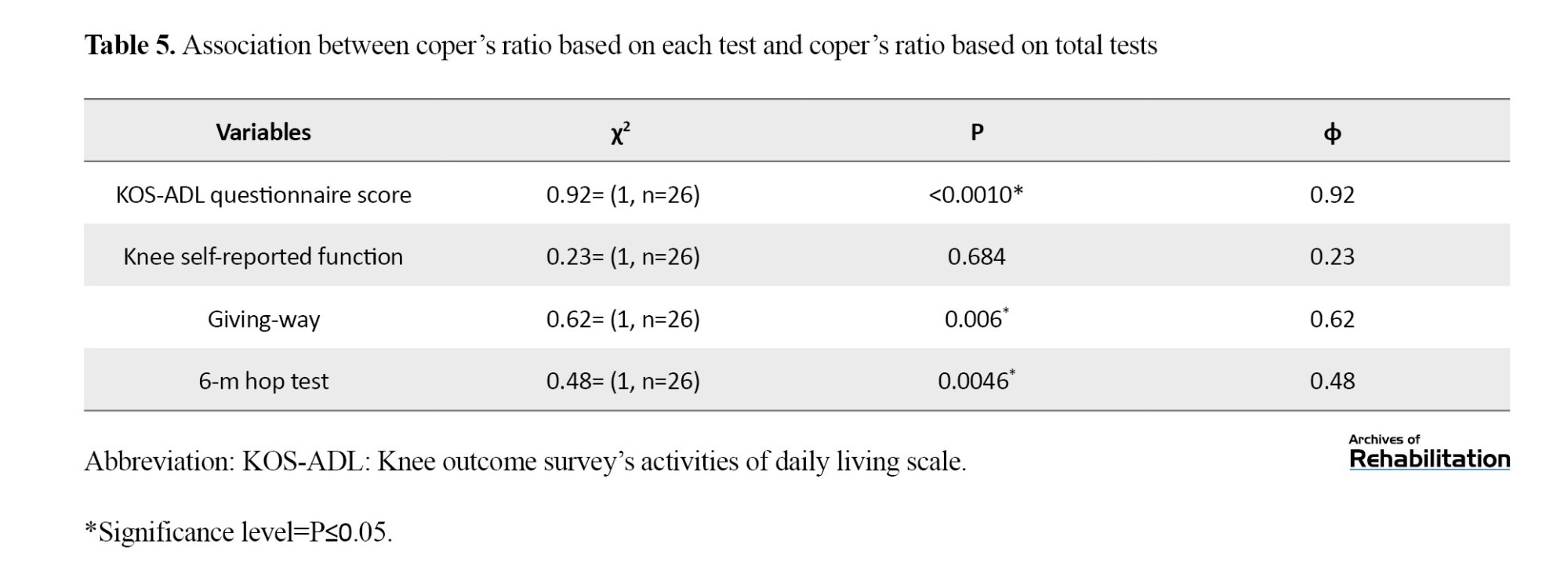
The results presented in Table 5 indicate that the highest correlation between the components of the screening test and the final result of the screening test, indicative of compatibility with the injury, is associated with the score of the KOS-ADL questionnaire, with a coefficient of 0.92. Conversely, the lowest correlation is linked to the knee self-reported performance, with a coefficient of 0.23.
Analysis of the Absolute Joint Position Sense Error Between Experimental and Control Groups and Between Coper and Non-coper Groups With Injury
To assess joint position sense, the absolute value of the difference between each individual’s reconstructed angle and the target angle (60 degrees knee flexion) was calculated, termed the absolute joint position sense error. An independent t test was conducted to compare the absolute joint position sense error between the experimental and control groups (Table 6). The test results indicated a significant difference between the two groups, with the absolute joint position sense error being lower in the experimental group. This result suggests that individuals in the experimental group can better reconstruct the target angle and have a more refined proprioception than the control group.
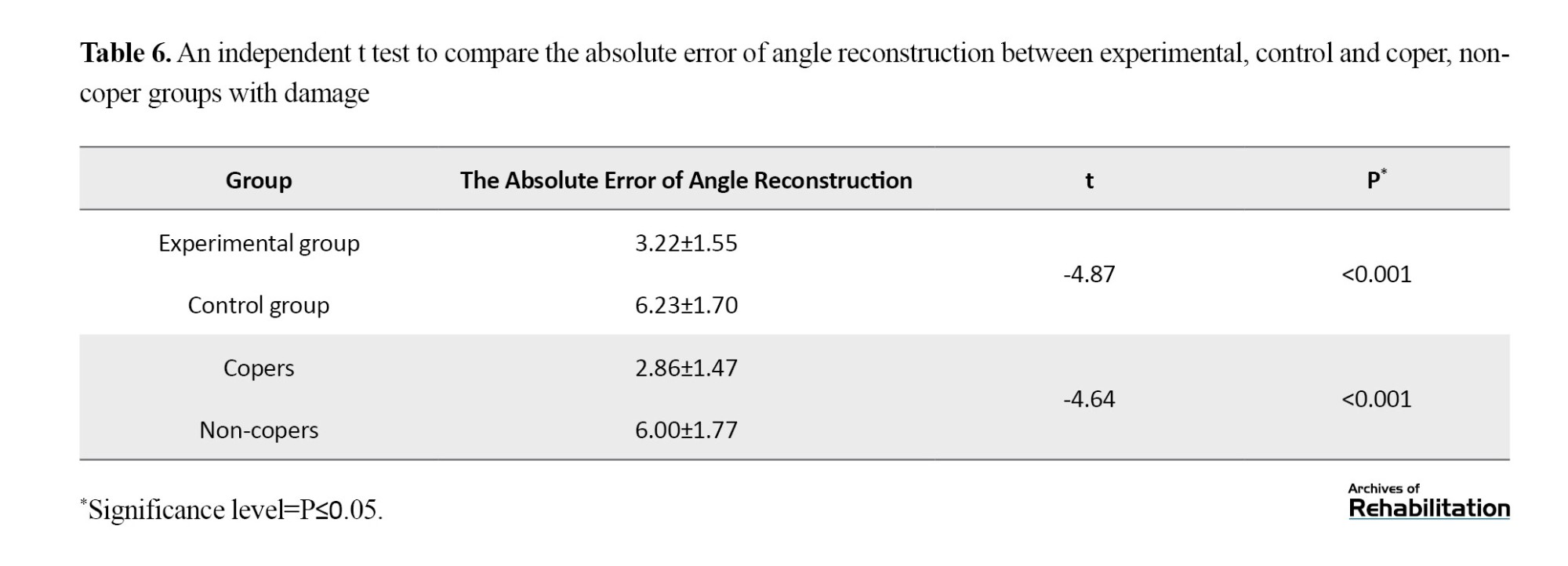
Moreover, a significant difference was observed between the coper and non-coper groups, with the absolute joint position sense error being lower in the coper group. This outcome signifies the superior ability of individuals in the coper group to reconstruct the target angle and a heightened sense of proprioception in this group (Table 4).
The Spearman correlation test was employed to assess the relationship between the average absolute joint position sense error and kinesiophobia. Additionally, the Pearson correlation test was utilized to examine the relationship between the average absolute joint position sense error and adaptation to injury. The results of these tests are summarized in Table 7.
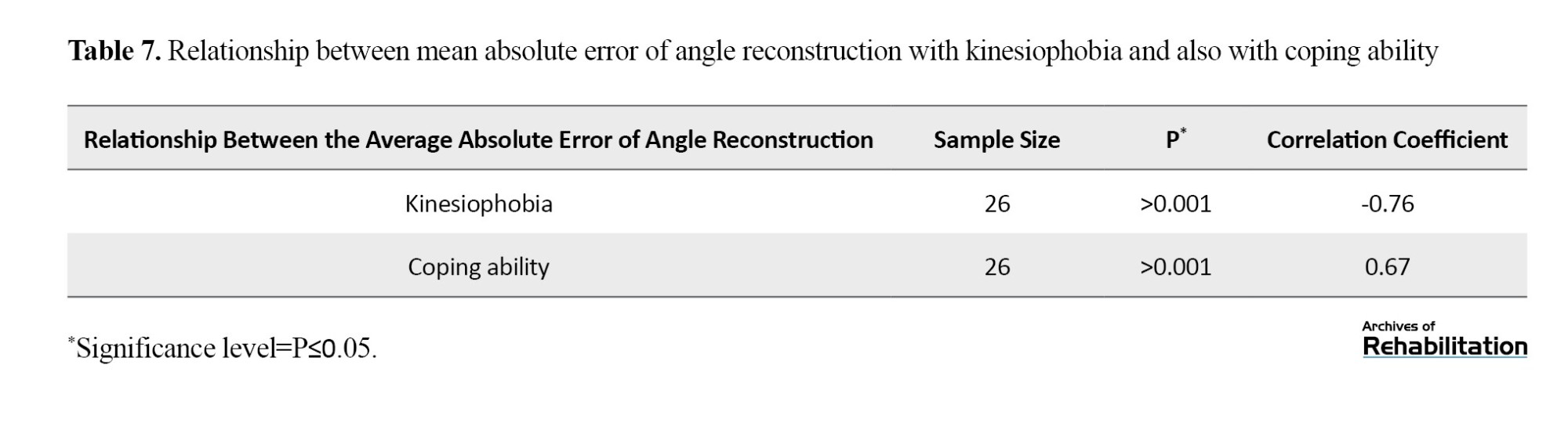
Table 7 indicates a strong inverse relationship between proprioception and kinesiophobia. Individuals who exhibited less kinesiophobia demonstrated a heightened proprioception, suggesting a more accurate proprioceptive ability. Additionally, a strong correlation was observed between proprioception and coping ability. Individuals who displayed greater coping ability exhibited higher proprioceptive sensitivity.
Notably, no side effects were observed in the experimental group due to using knee braces throughout the study period.
Discussion
Following an ACL tear, copers may resume previous activities without undergoing ligament reconstruction surgery. However, non-copers, due to instability and recurrent knee giving-way episodes, often require ligament reconstruction surgery. Given that no immediate rehabilitation intervention is typically performed post-rupture to enhance adaptation to the injury, the objective of our study was to investigate the efficacy of using a suitable knee brace following ACL rupture. Our study focused on using a hybrid knee brace, comprising an elastic sleeve and a functional knee brace, which, in addition to not interfering with the recovery of acute symptoms, can help increase adaptation to the injury. Results indicated that individuals who used the hybrid knee brace demonstrated greater improvement in parameters related to adaptation to injury and fear of injury than the control group. Moreover, the hybrid knee brace group exhibited better knee joint proprioception than the control group. This finding suggests that using a hybrid knee brace may mitigate the risk of repeated injuries and contribute to improved outcomes following ACL rupture.
The study’s findings revealed that the number of individuals adapted to the injury was higher in the experimental group, which used the hybrid knee brace for 4 weeks. Although 61.5% of participants in the experimental group and 23.1% in the control group were potential copers based on the screening test, the difference between the two groups was not statistically significant, possibly due to the small sample size. This study agrees with previous research indicating that improving neuromuscular control contributes to greater coping ability [44, 45].
Based on the studies conducted by Méndez-Bouza, Diermeier et al., the reason for this is the reduction of muscle co-contraction during walking and the normalization of knee kinematics, which increased knee stability. Furthermore, the correlations between the subgroups of the screening test and the final result of compatibility with injury were examined to identify the subgroup’s result closest to the overall outcome. Subgroup points included 1) achieving at least 80% of the 6-meter hop test score [4], 2) achieving at least 80% of the KOS-ADL questionnaire score [5], 3) achieving at least 60 points for the global knee function rating, and 4) experiencing a maximum of one knee giving-way episode since the time of injury [3]. The analysis revealed the highest correlation between scores of the KOS-ADL questionnaire and the final screening examination result. This finding suggests that if the screening test is not feasible, determining compatibility with injury can still be achieved using only the KOS-ADL questionnaire. Assessing patient-reported outcomes in screening examinations is crucial as they reflect an individual’s perspective on the injury or treatment’s impact on daily life and functioning. These outcomes significantly influence patient satisfaction. Although no significant difference was observed in the number of copers between the two groups, scores in both groups indicated that the experimental group performed better in the daily activities and knee self-report questionnaire scores. These parameters are closely related to the International Classification of Functioning, Disability, and Health (ICF), essential for patients and therapists [46، 47].
Another notable finding of this study revealed that subjects in the experimental group exhibited a superior sense of knee joint position and could reconstruct knee angles with less error than the target angle. This result is consistent with studies by Murata and Focke, which demonstrated that knee braces enhanced knee joint proprioception [48-51]. The hybrid brace likely enhances proprioception by stimulating the joint capsule and skin in the knee area, thereby strengthening sensory input and increasing knee sensation [52، 53]. Moreover, the study revealed a strong inverse relationship between the absolute joint position sense error and kinesiophobia. As fear of movement decreases, the error in angle reconstruction also decreases. This finding aligns with studies indicating that disturbances in proprioception contribute to the development of kinesiophobia [54-56].
Additionally, Harput et al. demonstrated the positive effects of knee braces and taping on kinesiophobia post-surgical treatment, attributed to increased knee stability [22]. However, some studies do not support the mechanical efficacy of knee braces on knees with damaged cruciate ligaments, suggesting that braces primarily improve proprioception [57]. Maybe the existing functional braces technologies may not effectively restore normal knee biomechanics or improve long-term patient outcomes. Furthermore, this study identified a strong relationship between coping ability and absolute joint position sense error, consistent with prior research [58-60] indicating that better proprioception correlates with improved adaptation to injury.
Conclusion
In conclusion, employing a hybrid knee brace, which combines an elastic sleeve and a functional brace, can improve proprioception, daily activity questionnaire scores, and knee self-reported performance scores following acute ACL injury. Enhanced proprioception is associated with greater coping ability, with a higher proportion of individuals using the knee brace demonstrating adaptation to the injury. This study highlights the potential benefits of utilizing a hybrid knee brace in managing ACL injuries, suggesting that it may be valuable in promoting recovery and rehabilitation following such injuries. By enhancing proprioceptive feedback and supporting knee stability, the hybrid knee brace offers a promising approach to improving functional outcomes and facilitating return to pre-injury activities. Further research and clinical trials may provide additional insights into the effectiveness and long-term benefits of using hybrid knee braces in ACL injury rehabilitation.
The study has several limitations that should be acknowledged. Firstly, the small sample size and the inclusion of participants with isolated, unilateral ACL tears limit the generalizability of the findings, particularly to individuals with ACL injuries accompanied by damage to other structures such as collateral ligaments or menisci. Future studies with larger and more diverse study samples must validate the results across a broader spectrum of ACL injury presentations. Secondly, this study only assessed the short-term effects of the hybrid knee brace intervention. Long-term follow-up evaluations are necessary to assess the durability of the intervention’s effects over time. A suggestion for future research is to conduct a longitudinal study with a follow-up period of at least 2 months to track symptoms and evaluate the persistence of treatment effects.
Additionally, this study did not fully explore factors such as patient adherence to brace usage, compliance with rehabilitation protocols, and potential confounding variables. Future research could investigate these factors to understand their influence on treatment outcomes better. Furthermore, while the study focused on the benefits of the hybrid knee brace intervention, potential adverse effects or limitations associated with its use were not thoroughly examined. Future studies should include comprehensive assessments of potential adverse events or drawbacks associated with the intervention.
In conclusion, while the findings of this study provide valuable insights into the potential benefits of using a hybrid knee brace in ACL injury rehabilitation, further research with larger sample sizes, longer follow-up periods, and comprehensive assessments of treatment adherence and potential adverse effects is warranted to strengthen the evidence base and inform clinical practice effectively.
Ethical Considerations
Compliance with ethical guidelines
This article has been approved by the Ethics Committee of Iran University of Medical Sciences (code: .IR.IUMS REC.1397.049). In this study, after providing necessary explanations about the research process, ensuring the confidentiality of information, and observing the right to leave the study, written consent was obtained from all participants.
Funding
This article was extracted from the PhD thesis of Zahra Nemati, funded by the Rehabilitation Research Center of Iran University of Medical Sciences (Grant number: 97-4-6-14006).
Authors' contributions
Conceptualization: Zahra Nemati and Maryam Jalali; Methodology: Zahra Nemati, Maryam Jalali, and Abolfazl Bagherifard; Validation: Zahra Nemati, Maryam Jalali, Mohammad Ali Sanjari; Investigation, review, and draft writing: Zahra Nemati; Editing & review, and supervision: Maryam Jalali, Mohammad Ali Sanjari and Abolfazl Bagherifard; Project administration and funding acquisition: Maryam Jalali.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Dr. Hooman Yahyazadeh and the staff of the Knee Clinic at Shafa Yahyaian Hospital for their cooperation in referring the patients, and all participants for their cooperation in this study.
References
The anterior cruciate ligament rupture (ACL) is a common knee joint injury. This injury results in anterior laxity of the tibiofemoral joint, leading to repeated knee instability and early-onset osteoarthritis [1]. After an injury, some people can return to the activity level before the injury, which is called copers. However, some are unable to resume previous activities due to recurrent knee giving way and kinesiophobia. They are classified as non-copers and are potential candidates for ligament reconstruction surgery [2]. To assess an individual’s capacity for adaptation to the injury, Fitzgerald et al. developed a screening test based on the dynamic stability of the knee joint during various activities [3]. Those achieving a satisfactory score on this test are categorized as copers to the injury, while those failing to do so are placed in the non-coper group [3]. The criteria for satisfactory performance include achieving at least 80% of the score on the 6-m jump test [4], scoring at least 80% on the KOS-ADL (knee outcome survey’s activities of daily living scale) questionnaire, attaining a minimum of 60 points on the Global rating of knee function [5], and experiencing a maximum of one episode of knee giving-way since the time of injury [6].
One of the factors influencing the ability to adapt to injury in these individuals is neuromuscular coordination [7], which is disrupted by the loss of afferent feedback from the ACL [8]. The absence of feedback also leads to a reduction in knee proprioception [9], which is a primary contributor to knee instability in injury non-adaptive patients [10]. To improve the neuromuscular system, perturbation training is typically performed on balance boards once acute symptoms subside, involving anterior-posterior and internal-external perturbations as well as multi-directional perturbations [11]. However, such interventions are not conducted due to the instability experienced during the acute injury phase [12]. Since skin receptors around the knee transmit vital information regarding joint position and movements, stimulating these receptors can partially compensate for the proprioceptive deficit resulting from ligament rupture [13].
To enhance neuromuscular function and dynamic stability, stimulating joint capsule receptors and muscles surrounding the knee can also be beneficial [14، 15]. Studies indicate that knee braces have effects such as increasing knee proprioception through skin contact [16] and applying pressure on underlying muscles and the joint capsule [17، 18], consequently altering the timing and movement patterns of lower limb muscles [19]. Strutzenberger and Delincé et al. reported that using flexible structures like elastic sleeves in individuals with complete ACL ruptures leads to improved proprioception [20، 21] and increased brain activity in the primary sensorimotor cortex, responsible for processing sensory input, thus enhancing the proprioception. Therefore, knee braces and elastic sleeves can enhance knee proprioception and neuromuscular function in individuals with complete ACL rupture [22].
Another factor influencing the ability to adapt to injury following an ACL rupture is kinesiophobia. Individuals who successfully adapt to the injury typically exhibit lower levels of kinesiophobia [23]. While psychological factors also play a role in the development of kinesiophobia [24], increasing the mechanical stability of the knee can help mitigate it [22، 23]. Brisson et al. demonstrated that knee braces could enhance knee stability post-ACL rupture [25]. Similarly, Harput et al.’s study indicates that employing a knee brace after ligament reconstruction surgery reduced kinesiophobia [22]. Based on the existing literature, no study has investigated the effect of brace usage during the acute phase following an ACL rupture on enhancing coping rates. Therefore, this study aims to explore the impact of employing a hybrid knee brace (Figure 1), comprising a custom-made functional brace and an elastic sleeve, on kinesiophobia, proprioception, and its overall effect on the ability to adapt to the injury during the acute stage following an ACL rupture.

Materials and Methods
The present study is a single-blind randomized clinical trial conducted on 30 individuals with acute ACL rupture. The samples were selected based on availability and randomly assigned using permutation blocks (four blocks of four) into control and experimental groups [26]. Participants remained unaware of the process and the existence of the other group. The sample size was determined using G*Power software version 3.1.9.2, with a confidence level of 95%, a power of 80%, and an effect size of 0.8, which was derived from a similar study [27]. This calculation yielded 13 individuals in each group. However, to account for a potential 15% drop in the sample, the number increased to 15 individuals in each group. Ethical approval for this study was obtained from the Iran University of Medical Sciences Ethics Committee and registered in the Iranian Registry of Clinical Trial (IRCT). All participants provided informed consent by signing the consent form before participating in the study.
A specialized knee surgeon selected samples from the knee orthopedic clinic at Shafa Yahyaeian Orthopedics Hospital, Tehran City, Iran. Subsequently, they were randomly assigned into two groups: control (without orthosis) and experimental (with orthosis). Both groups followed an identical physiotherapy program, consisting of 10 sessions to increase knee range of motion, reduce swelling, and perform strengthening exercises for the quadriceps and hamstring muscles. These sessions were conducted uniformly by an experienced therapist for both groups. At the initial physiotherapy sessions, individuals experiencing swelling were treated with compression bandaging to reduce swelling.
If necessary, devices like transcutaneous electrical nerve stimulation and pulsed ultrasound were utilized. Since quadriceps muscles undergo inhibition after ACL rupture, early strengthening of these muscles is crucial. However, hamstring muscles should also be strengthened as these muscles act as antagonists to the ACL. Quadriceps muscle strengthening was conducted using devices such as a Faradic or functional electrical stimulation device and Q-set exercises. The exercises provided to patients at this stage consisted of closed and open kinetic chain exercises [28، 29]. During the first two weeks, exercises within the range of 30 to 60 degrees of knee flexion were performed. Patellar bone mobilization was performed to increase the knee’s range of motion. In the following two weeks, exercises were performed within a larger range of motion. Upon completing the physiotherapy sessions, the physiotherapist provided a satisfactory status report regarding muscle strength, area swelling, and sufficient range of motion for patients to undergo functional tests.
The inclusion criteria of this study encompassed patients aged 18 to 40 years who presented with an isolated and unilateral tear of the ACL, confirmed through magnetic resonance imaging (MRI). These individuals should have maintained a moderate activity level before the injury, indicated by a score of 3-5 on the Tegner scale [30]. Furthermore, they should have no history of fractures or surgeries in the knee area and no prior damage to the ACL or other ligaments of the knee joint. The exclusion criteria comprised individuals who experienced pain or inflammation in the knee during functional tests or those who declined to continue cooperating with the study’s rehabilitation protocol.
The participants underwent evaluation in two sessions. During the first session, they completed the KOS-ADL questionnaire [5], the global rating of knee function [31], and the Tampa questionnaire [32]. The KOS-ADL scale is a self-report tool designed to assess performance limitations in patients experiencing various knee conditions, including ligament and meniscus injuries, patellofemoral pain, and knee osteoarthritis. This questionnaire comprises sections for measuring symptoms and functional limitations during daily activities. Specifically, the section related to daily activities measurement consists of 14 questions. Six questions pertain to the impact of impairment on the ability to perform daily activities, while the remaining 8 focus on the effect of knee impairment on specific tasks. Each question offers five response options, scored from 0 to 5. A score of 0 denotes no difficulty in performing the activity, while a score of 5 indicates inability to perform the activity. The maximum achievable score is 70. The total score is converted to a percentage by dividing by 70 and multiplying by 100. The validity and reliability of this questionnaire were investigated by Irrgang et al. in 1998 [33].
Additionally, a study conducted by Salvati et al. demonstrated that the Persian version of this questionnaire is valid and reliable for use in Iranian society [34]. The global rating of knee function represents the current performance of the knee in comparison to its state before the injury. It is assessed using the visual analog scale (VAS), ranging from 0 to 100 [31].
The Tampa questionnaire assesses the pain associated with fear, accompanied by avoidance and restriction of behavior, movement, and physical activities initiated by the individual. It comprises 17 questions rated on a 4-point Likert scale with responses ranging from 1= “completely disagree” to 4= “completely agree.” Upon completion by the patient, a total score between 17 and 68 is calculated. Scores below 37 indicate a low kinesiophobia, while scores exceeding 37 suggest a high kinesiophobia. The minimum clinically important difference for kinesiophobia is reported to be a 4-point reduction [35]. The Persian translation of the Tampa questionnaire was conducted by Jafari et al., who measured and evaluated the psychometric properties of the Persian version. The results indicated that the Persian version of the Tampa kinesiophobia scale is valid and reliable for Iranian society [36].
Four weeks after enrollment in the study, the participants were summoned to the Research Institute of Physical Education and Sports Sciences under the Ministry of Science, Research and Technology in Tehran to undergo functional tests. Adaptation to the injury was assessed through a screening test, while the sense of joint position was evaluated using the Biodex dynamometer device [37]. The screening test comprised 4 conditions: achieving a score of at least 80% on the six-meter jump test, obtaining a score of at least 80% on the daily activities questionnaire, attaining a score of at least 60% on the overall knee function assessment, experiencing at least one instance of knee instability following the initiation of treatment [3].
The joint position sense was assessed using the Biodex System Pro 3 dynamometer (Shirley, New York, USA), initially in the healthy knee and subsequently in the injured knee. This device has been validated and proven reliable for measuring joint position sense [37]. Proper positioning of the individual in the Biodex machine involved aligning the knee’s movement axis with the dynamometer’s mechanical axis. Additionally, the dynamometer seat was adjusted to an 85-degree flexion angle, and the knee’s range of motion was set from full extension to 90 degrees of flexion. The end of the knee connecting lever was positioned above the ankles and secured with a strap. The individual’s torso was also stabilized using shoulder, waist, and thigh straps. Before commencing the test, leg torque produced at a 30-degree knee flexion angle was recorded to negate the effects of gravity. Furthermore, to minimize the influence of other muscles, the individual maintained crossed arms on the chest [38]. For the joint position test with closed eyes, the knee was passively moved from 90° flexion to 60° flexion using the lever arm of the device and returned to the initial position after 4 seconds. Subsequently, participants were instructed to reproduce the bending angle with their eyes closed actively. Following two experimental repetitions, three tests were recorded for each side.
The hybrid brace used in the experimental group consisted of a functional brace and an elastic sleeve (Figure 1). The functional component comprised a posterior femoral cuff and an anterior shin cuff of 2.5-mm thick polypropylene. These components were designed to enhance anterior-posterior stability and were custom-made for each patient based on limb measurements. In individuals with ACL rupture, anterior and posterior instability leads to anterior tibial displacement relative to the femur during walking [10، 39]. Thus, positioning the shin cuff anteriorly and the thigh cuff posteriorly prevents this displacement. The midpoint between the hip trochanter and the external condyle of the femur corresponded to the location of the femoral cuff, while the midpoint between the head of the fibula and the lateral malleolus aligned with the position of the tibial cuff. The polycentric knee joint, constructed from aluminum and featuring a gear model, allows free joint movement. This joint was aligned with the knee’s movement axis, ensuring optimal functionality. From a lateral perspective, the knee brace’s joint location is aligned with the knee’s anatomical axis.
Additionally, elastic straps were employed to minimize functional knee brace slippage. The elastic straps, capable of greater stretch than non-elastic ones, provide increased orthotic adhesion, thereby reducing downward slippage. The ACL plays a significant role in controlling valgus force and preventing instability on the medial side of the knee joint [40]. Consequently, ACL damage results in internal knee joint instability. The external load of the knee brace counteracts valgus force and mitigates internal instability post-ACL rupture [41، 42]. This outcome is achieved by applying three pressure points generated by the upper and lower ends of the lateral upright and the knee pad’s mutual force on the inner aspect of the knee (Figure 1). The orthotic joint was linked to the upper and lower cuff via lateral upright in this brace. Strap tension varied to accommodate proper suspension and individual tolerance levels, as indicated by skin redness assessment 15 minutes after brace removal. The applied pressure was deemed appropriate if redness disappeared within 20 minutes [43]. Underneath the functional brace, patients wore a Tynor® neoprene sleeve that provided complete contact with the knee, exerting pressure on underlying structures. Sleeve size was determined individually by measuring knee circumference and utilizing the sleeve guide. Patients were instructed to wear the hybrid brace for a minimum of four hours daily and record the duration of use.
SPSS statistical software, version 22 was employed for data analysis, with the normality of data distribution assessed using the Shapiro-Wilk test. All data exhibited normal distribution except for the performance report, which was normalized by excluding one outlier data point. An independent t test was utilized to assess the homogeneity of the two groups concerning age, scores on the Tampa and daily activity questionnaires, and the global rating of knee function scores at the study’s outset.
Mixed within-between analysis of variance (ANOVA) was employed to evaluate the KOS-ADL questionnaire, global rating of knee function report, and Tampa questionnaire within and between groups. The Chi-square test was conducted to compare the proportion of copers and non-copers. The Spearman correlation test was employed to investigate the relationship between coping ability and proprioception and the association between kinesiophobia and proprioception. A significance level of 0.05 was established.
Furthermore, an independent t test was conducted to compare the absolute joint position sense error, which was used to measure joint position sense, between the test, control, and coper and non-coper groups.
Results
The study included 30 individuals diagnosed with isolated ACL tears. However, two individuals were excluded from the study because they did not utilize a brace, while the other two were excluded for failing to attend all physiotherapy sessions. Consequently, 26 individuals were chosen to partake in the study, divided into two groups, with 13 participants in each group. Before the study’s commencement, the two groups were matched based on age, time of injury, fear of movement level, daily activity, and knee function, as outlined in Table 1.
The Effects of Using a Hybrid Brace on Kinesiophobia, Knee Function, and Daily Activities
A mixed within-between analysis of variance was conducted to assess the impact of utilizing a hybrid knee orthosis on kinesiophobia, knee function, and daily activities. The within-group analysis of variance results indicated a significant difference between pre- and post-intervention outcomes across all three variables, with improvements observed in the scores of each variable following the intervention in both groups (demonstrating a significant main effect of the variables). Additionally, the interaction effect of all three variables (Tampa questionnaire, daily activities measurement questionnaire, and knee self-reported performance) was found to be significant in both groups (Table 2), indicating that the positive changes in all three variables were more pronounced in the test group compared to the control group (Figure 2).
Regarding between-group analysis concerning kinesiophobia and knee function, no significant differences were observed between the two groups (Table 3). However, regarding the score of the daily activities questionnaire, a significant difference was noted between the two groups (P=0.020) (Table 3).
Determining the Frequency and Percentage of Copers in Each Group, Separately For Each Component of the Screening Test, and the Final Score of the Test
Table 3 displays the frequency and percentage of copers in each group, separately by each component of the screening test, along with the final score. Eight individuals in the test group and 3 in the control group exhibited coping (61.5% vs 23.1%) (Table 4).
In Table 5, the relationship between the proportion of copers based on each test and the proportion of copers based on all the tests is reported using the Chi-square test. According to this Table, the score of the KOS-ADL questionnaire exhibits the highest correlation with the final result of the screening test (φ= 0.92).
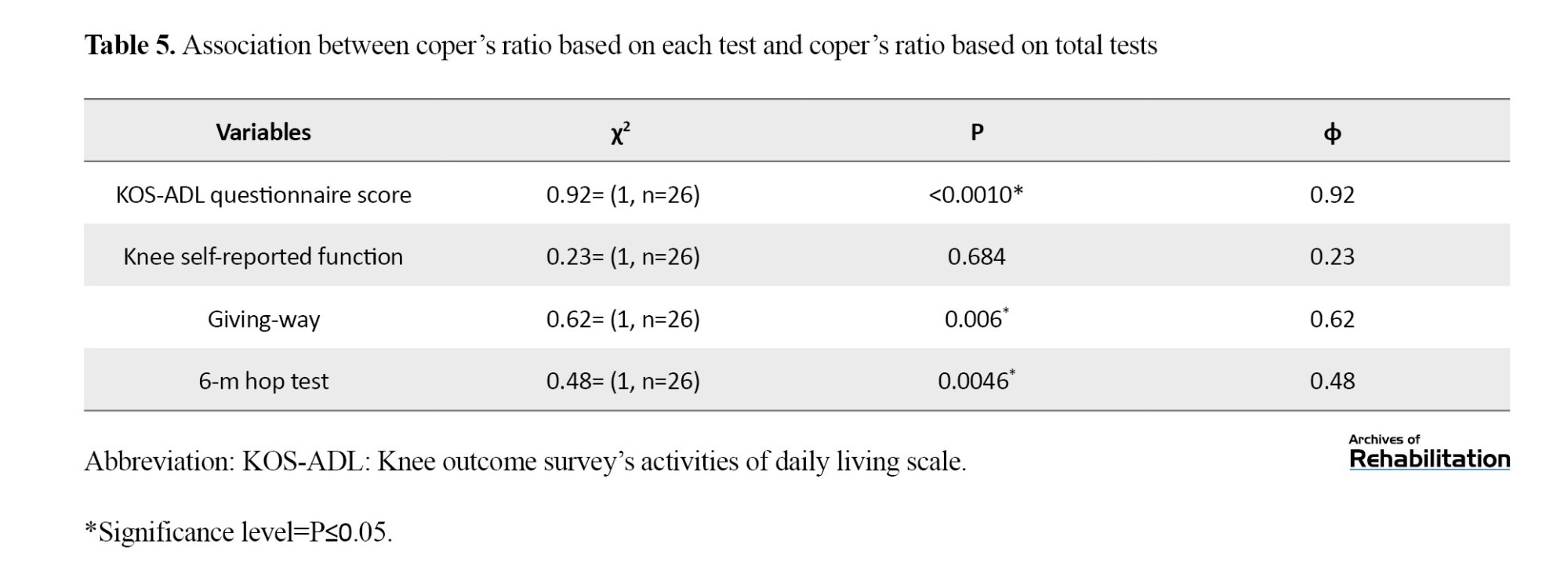
The results presented in Table 5 indicate that the highest correlation between the components of the screening test and the final result of the screening test, indicative of compatibility with the injury, is associated with the score of the KOS-ADL questionnaire, with a coefficient of 0.92. Conversely, the lowest correlation is linked to the knee self-reported performance, with a coefficient of 0.23.
Analysis of the Absolute Joint Position Sense Error Between Experimental and Control Groups and Between Coper and Non-coper Groups With Injury
To assess joint position sense, the absolute value of the difference between each individual’s reconstructed angle and the target angle (60 degrees knee flexion) was calculated, termed the absolute joint position sense error. An independent t test was conducted to compare the absolute joint position sense error between the experimental and control groups (Table 6). The test results indicated a significant difference between the two groups, with the absolute joint position sense error being lower in the experimental group. This result suggests that individuals in the experimental group can better reconstruct the target angle and have a more refined proprioception than the control group.
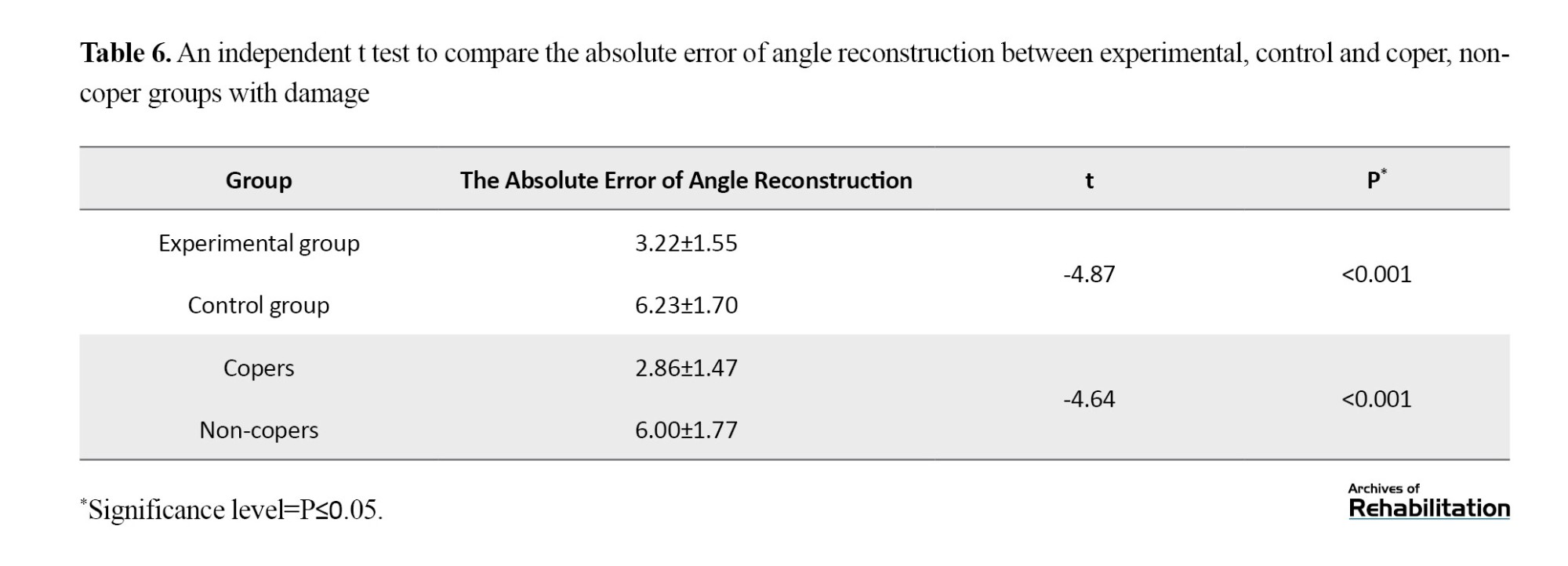
Moreover, a significant difference was observed between the coper and non-coper groups, with the absolute joint position sense error being lower in the coper group. This outcome signifies the superior ability of individuals in the coper group to reconstruct the target angle and a heightened sense of proprioception in this group (Table 4).
The Spearman correlation test was employed to assess the relationship between the average absolute joint position sense error and kinesiophobia. Additionally, the Pearson correlation test was utilized to examine the relationship between the average absolute joint position sense error and adaptation to injury. The results of these tests are summarized in Table 7.
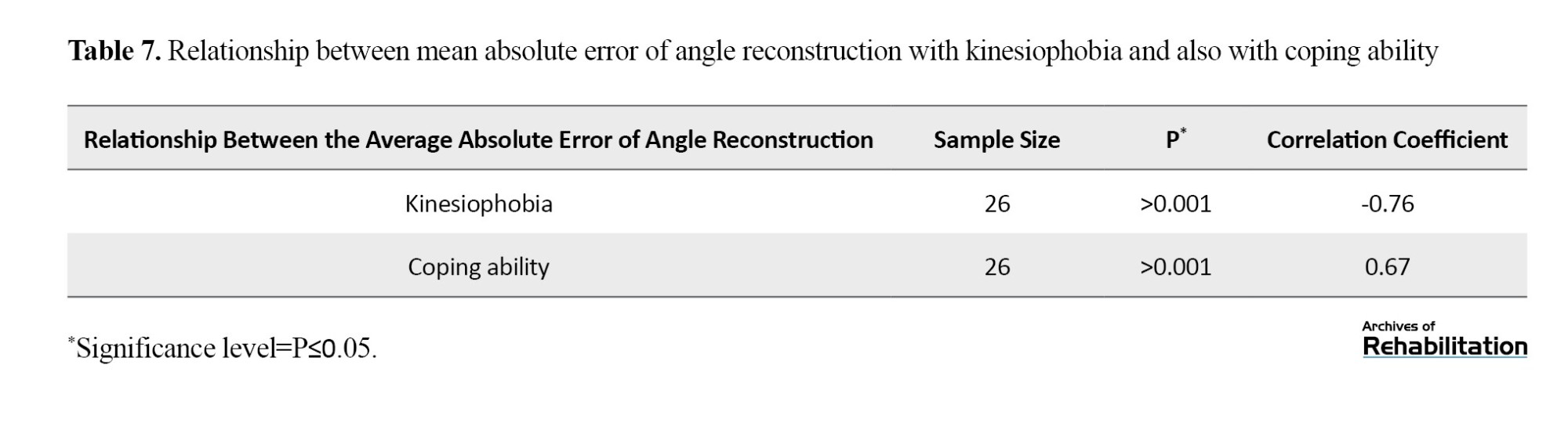
Table 7 indicates a strong inverse relationship between proprioception and kinesiophobia. Individuals who exhibited less kinesiophobia demonstrated a heightened proprioception, suggesting a more accurate proprioceptive ability. Additionally, a strong correlation was observed between proprioception and coping ability. Individuals who displayed greater coping ability exhibited higher proprioceptive sensitivity.
Notably, no side effects were observed in the experimental group due to using knee braces throughout the study period.
Discussion
Following an ACL tear, copers may resume previous activities without undergoing ligament reconstruction surgery. However, non-copers, due to instability and recurrent knee giving-way episodes, often require ligament reconstruction surgery. Given that no immediate rehabilitation intervention is typically performed post-rupture to enhance adaptation to the injury, the objective of our study was to investigate the efficacy of using a suitable knee brace following ACL rupture. Our study focused on using a hybrid knee brace, comprising an elastic sleeve and a functional knee brace, which, in addition to not interfering with the recovery of acute symptoms, can help increase adaptation to the injury. Results indicated that individuals who used the hybrid knee brace demonstrated greater improvement in parameters related to adaptation to injury and fear of injury than the control group. Moreover, the hybrid knee brace group exhibited better knee joint proprioception than the control group. This finding suggests that using a hybrid knee brace may mitigate the risk of repeated injuries and contribute to improved outcomes following ACL rupture.
The study’s findings revealed that the number of individuals adapted to the injury was higher in the experimental group, which used the hybrid knee brace for 4 weeks. Although 61.5% of participants in the experimental group and 23.1% in the control group were potential copers based on the screening test, the difference between the two groups was not statistically significant, possibly due to the small sample size. This study agrees with previous research indicating that improving neuromuscular control contributes to greater coping ability [44, 45].
Based on the studies conducted by Méndez-Bouza, Diermeier et al., the reason for this is the reduction of muscle co-contraction during walking and the normalization of knee kinematics, which increased knee stability. Furthermore, the correlations between the subgroups of the screening test and the final result of compatibility with injury were examined to identify the subgroup’s result closest to the overall outcome. Subgroup points included 1) achieving at least 80% of the 6-meter hop test score [4], 2) achieving at least 80% of the KOS-ADL questionnaire score [5], 3) achieving at least 60 points for the global knee function rating, and 4) experiencing a maximum of one knee giving-way episode since the time of injury [3]. The analysis revealed the highest correlation between scores of the KOS-ADL questionnaire and the final screening examination result. This finding suggests that if the screening test is not feasible, determining compatibility with injury can still be achieved using only the KOS-ADL questionnaire. Assessing patient-reported outcomes in screening examinations is crucial as they reflect an individual’s perspective on the injury or treatment’s impact on daily life and functioning. These outcomes significantly influence patient satisfaction. Although no significant difference was observed in the number of copers between the two groups, scores in both groups indicated that the experimental group performed better in the daily activities and knee self-report questionnaire scores. These parameters are closely related to the International Classification of Functioning, Disability, and Health (ICF), essential for patients and therapists [46، 47].
Another notable finding of this study revealed that subjects in the experimental group exhibited a superior sense of knee joint position and could reconstruct knee angles with less error than the target angle. This result is consistent with studies by Murata and Focke, which demonstrated that knee braces enhanced knee joint proprioception [48-51]. The hybrid brace likely enhances proprioception by stimulating the joint capsule and skin in the knee area, thereby strengthening sensory input and increasing knee sensation [52، 53]. Moreover, the study revealed a strong inverse relationship between the absolute joint position sense error and kinesiophobia. As fear of movement decreases, the error in angle reconstruction also decreases. This finding aligns with studies indicating that disturbances in proprioception contribute to the development of kinesiophobia [54-56].
Additionally, Harput et al. demonstrated the positive effects of knee braces and taping on kinesiophobia post-surgical treatment, attributed to increased knee stability [22]. However, some studies do not support the mechanical efficacy of knee braces on knees with damaged cruciate ligaments, suggesting that braces primarily improve proprioception [57]. Maybe the existing functional braces technologies may not effectively restore normal knee biomechanics or improve long-term patient outcomes. Furthermore, this study identified a strong relationship between coping ability and absolute joint position sense error, consistent with prior research [58-60] indicating that better proprioception correlates with improved adaptation to injury.
Conclusion
In conclusion, employing a hybrid knee brace, which combines an elastic sleeve and a functional brace, can improve proprioception, daily activity questionnaire scores, and knee self-reported performance scores following acute ACL injury. Enhanced proprioception is associated with greater coping ability, with a higher proportion of individuals using the knee brace demonstrating adaptation to the injury. This study highlights the potential benefits of utilizing a hybrid knee brace in managing ACL injuries, suggesting that it may be valuable in promoting recovery and rehabilitation following such injuries. By enhancing proprioceptive feedback and supporting knee stability, the hybrid knee brace offers a promising approach to improving functional outcomes and facilitating return to pre-injury activities. Further research and clinical trials may provide additional insights into the effectiveness and long-term benefits of using hybrid knee braces in ACL injury rehabilitation.
The study has several limitations that should be acknowledged. Firstly, the small sample size and the inclusion of participants with isolated, unilateral ACL tears limit the generalizability of the findings, particularly to individuals with ACL injuries accompanied by damage to other structures such as collateral ligaments or menisci. Future studies with larger and more diverse study samples must validate the results across a broader spectrum of ACL injury presentations. Secondly, this study only assessed the short-term effects of the hybrid knee brace intervention. Long-term follow-up evaluations are necessary to assess the durability of the intervention’s effects over time. A suggestion for future research is to conduct a longitudinal study with a follow-up period of at least 2 months to track symptoms and evaluate the persistence of treatment effects.
Additionally, this study did not fully explore factors such as patient adherence to brace usage, compliance with rehabilitation protocols, and potential confounding variables. Future research could investigate these factors to understand their influence on treatment outcomes better. Furthermore, while the study focused on the benefits of the hybrid knee brace intervention, potential adverse effects or limitations associated with its use were not thoroughly examined. Future studies should include comprehensive assessments of potential adverse events or drawbacks associated with the intervention.
In conclusion, while the findings of this study provide valuable insights into the potential benefits of using a hybrid knee brace in ACL injury rehabilitation, further research with larger sample sizes, longer follow-up periods, and comprehensive assessments of treatment adherence and potential adverse effects is warranted to strengthen the evidence base and inform clinical practice effectively.
Ethical Considerations
Compliance with ethical guidelines
This article has been approved by the Ethics Committee of Iran University of Medical Sciences (code: .IR.IUMS REC.1397.049). In this study, after providing necessary explanations about the research process, ensuring the confidentiality of information, and observing the right to leave the study, written consent was obtained from all participants.
Funding
This article was extracted from the PhD thesis of Zahra Nemati, funded by the Rehabilitation Research Center of Iran University of Medical Sciences (Grant number: 97-4-6-14006).
Authors' contributions
Conceptualization: Zahra Nemati and Maryam Jalali; Methodology: Zahra Nemati, Maryam Jalali, and Abolfazl Bagherifard; Validation: Zahra Nemati, Maryam Jalali, Mohammad Ali Sanjari; Investigation, review, and draft writing: Zahra Nemati; Editing & review, and supervision: Maryam Jalali, Mohammad Ali Sanjari and Abolfazl Bagherifard; Project administration and funding acquisition: Maryam Jalali.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Dr. Hooman Yahyazadeh and the staff of the Knee Clinic at Shafa Yahyaian Hospital for their cooperation in referring the patients, and all participants for their cooperation in this study.
References
- Wang LJ, Zeng N, Yan ZP, Li JT, Ni GX. Post-traumatic osteoarthritis following ACL injury. Arthritis Research & Therapy. 2020; 22(1):57. [DOI:10.1186/s13075-020-02156-5] [PMID]
- Ptasinski AM, Dunleavy M, Adebayo T, Gallo RA. Returning athletes to sports following anterior cruciate ligament tears. Current Reviews in Musculoskeletal Medicine. 2022; 15(6):616-28. [DOI:10.1007/s12178-022-09782-3] [PMID]
- Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surgery, Sports Traumatology, Arthroscopy. 2000; 8(2):76-82. [DOI:10.1007/s001670050190] [PMID]
- Sonesson S, Gauffin H, Kvist J. Early knee status affects self-reported knee function 1 year after non-surgically treated anterior cruciate ligament injury. Physical Therapy in Sport. 2021; 50:173-83. [DOI:10.1016/j.ptsp.2021.05.007] [PMID]
- Ataeian M, Shafizadegan Z, Rahnemai-Azar AA, Irrgang JJ, Rezaeian ZS. Development of the Persian version of knee outcome survey activities for daily living scale. Iranian Journal of Medical Sciences. 2020; 45(6):434-43. [PMID]
- Musahl V, Diermeier T, de Sa D, Karlsson J. ACL surgery: When to do it? Knee Surgery, Sports Traumatology, Arthroscopy : Official Journal of the ESSKA. 2020; 28(7):2023-26. [DOI:10.1007/s00167-020-06117-y] [PMID]
- Ward SH, Perraton L, Bennell K, Pietrosimone B, Bryant AL. Deficits in quadriceps force control after anterior cruciate ligament injury: Potential central mechanisms. Journal of Athletic Training. 2019; 54(5):505-12. [DOI:10.4085/1062-6050-414-17] [PMID]
- Criss CR, Melton MS, Ulloa SA, Simon JE, Clark BC, France CR, et al. Rupture, reconstruction, and rehabilitation: A multi-disciplinary review of mechanisms for central nervous system adaptations following anterior cruciate ligament injury. The Knee. 2021; 30:78-89. [DOI:10.1016/j.knee.2021.03.009] [PMID]
- Tayfur B, Charuphongsa C, Morrissey D, Miller SC. Neuromuscular function of the knee joint following knee injuries: Does it ever get back to normal? A systematic review with meta-analyses. Sports Medicine. 2021; 51(2):321-38. [DOI:10.1007/s40279-020-01386-6] [PMID]
- Manchado I, Alvarez D, Motta LM, Blanco G, Saavedra P, Garcés GL. Correlation among knee muscle strength and self-reported outcomes score, anterior tibial displacement, and time post-injury in Non-Coper anterior cruciate ligament deficient patients: a cross-sectional study. International Journal of Environmental Research and Public Health. 2021; 18(24):13303. [DOI:10.3390/ijerph182413303] [PMID]
- Nawasreh Z, Logerstedt D, Marmon A, Snyder-Mackler L. Clinical and biomechanical efficacies of mechanical perturbation training after anterior cruciate ligament rupture. Journal of Sport Rehabilitation. 2019; 28(8):877-86. [DOI:10.1123/jsr.2017-0363] [PMID]
- Paterno MV. Non-operative care of the patient with an ACL-deficient knee. Current Reviews in Musculoskeletal Medicine. 2017; 10(3):322-7. [DOI:10.1007/s12178-017-9431-6] [PMID]
- Macefield VG. The roles of mechanoreceptors in muscle and skin in human proprioception. Current Opinion in Physiology. 2021; 21:48-56. [DOI:10.1016/j.cophys.2021.03.003]
- Sliz D, Smith A, Wiebking C, Northoff G, Hayley S. Neural correlates of a single-session massage treatment. Brain Imaging and Behavior. 2012; 6(1):77-87. [DOI:10.1007/s11682-011-9146-z] [PMID]
- David E, Amasay T, Ludwig K, Shapiro S. The effect of foam rolling of the hamstrings on proprioception at the knee and hip joints. International Journal of Exercise Science. 2019; 12(1):343-54. [DOI:10.70252/GDKN8044] [PMID]
- Beynnon BD, Good L, Risberg MA. The effect of bracing on proprioception of knees with anterior cruciate ligament injury. Journal of Orthopaedic & Sports Physical Therapy. 2002; 32(1):11-5. [DOI:10.2519/jospt.2002.32.1.11] [PMID]
- Herrington L, Simmonds C, Hatcher J. The effect of a neoprene sleeve on knee joint position sense. Research in Sports Medicine. 2005; 13(1):37-46. [DOI:10.1080/15438620590922077] [PMID]
- Palm HG, Brattinger F, Stegmueller B, Achatz G, Riesner HJ, Friemert B. Effects of knee bracing on postural control after anterior cruciate ligament rupture. The Knee. 2012; 19(5):664-71. [DOI:10.1016/j.knee.2011.07.011] [PMID]
- Mohd Sharif NA, Goh SL, Usman J, Wan Safwani WKZ. Biomechanical and functional efficacy of knee sleeves: A literature review. Physical Therapy in Sport. 2017; 28:44-52. [DOI:10.1016/j.ptsp.2017.05.001] [PMID]
- Strutzenberger G, Braig M, Sell S, Boes K, Schwameder H. Effect of brace design on patients with ACL-ruptures. International Journal of Sports Medicine. 2012; 33(11):934-9. [DOI:10.1055/s-0032-1304634] [PMID]
- Delincé P, Ghafil D. Anterior cruciate ligament tears: Conservative or surgical treatment? A critical review of the literature. Knee Surgery, Sports Traumatology, Arthroscopy. 2012; 20(1):48-61. [DOI:10.1007/s00167-011-1614-x] [PMID]
- Harput G, Ulusoy B, Ozer H, Baltaci G, Richards J. External supports improve knee performance in anterior cruciate ligament reconstructed individuals with higher kinesiophobia levels. The Knee. 2016; 23(5):807-12. [DOI:10.1016/j.knee.2016.05.008] [PMID]
- Hartigan EH, Lynch AD, Logerstedt DS, Chmielewski TL, Snyder-Mackler L. Kinesiophobia after anterior cruciate ligament rupture and reconstruction: noncopers versus potential copers. Journal of Orthopaedic & Sports Physical Therapy. 2013; 43(11):821-32. [DOI:10.2519/jospt.2013.4514] [PMID]
- Ardern CL, Kvist J, Webster KE. Psychological aspects of anterior cruciate ligament injuries. Operative Techniques in Sports Medicine. 2016; 24(1):77-83. [DOI:10.1053/j.otsm.2015.09.006]
- Brisson N, Lamontagne M. The efficacy of functional knee braces in stabilizing anterior cruciate ligament defficiency knees: A review. Journal of Orthopedics. 2014;6(1):1-12.
- Jüni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ. 2001; 323(7303):42-6. [DOI:10.1136/bmj.323.7303.42] [PMID]
- Moksnes H, Snyder-Mackler L, Risberg MA. Individuals with an anterior cruciate ligament-deficient knee classified as noncopers may be candidates for nonsurgical rehabilitation. journal of Orthopaedic & Sports Physical Therapy. 2008; 38(10):586-95. [DOI:10.2519/jospt.2008.2750] [PMID]
- American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. Pennsylvania: Wolters Kluwer Health; 2013. [Link]
- Brotzman SB, Manske RC. Clinical orthopaedic rehabilitation e-book: An evidence-based approach-expert consult. Amsterdam: Elsevier Health Sciences; 2011. [Link]
- Negahban H, Mostafaee N, Sohani SM, Mazaheri M, Goharpey S, Salavati M, et al. Reliability and validity of the Tegner and Marx activity rating scales in Iranian patients with anterior cruciate ligament injury. Disability and Rehabilitation. 2011; 33(22-23):2305-10. [DOI:10.3109/09638288.2011.570409] [PMID]
- Koca F, Fältström A, Cristiani R, Stålman A. Comparison of knee function and activity level between bilateral and unilateral ACL reconstruction: A matched-group analysis with minimum 5-year follow-up. Orthopaedic Journal of Sports Medicine. 2022; 10(4):23259671221083576. [DOI:10.1177/23259671221083576] [PMID]
- Huang H, Nagao M, Arita H, Shiozawa J, Nishio H, Kobayashi Y, et al. Reproducibility, responsiveness and validation of the Tampa Scale for Kinesiophobia in patients with ACL injuries. Health and quality of life outcomes. 2019; 17(1):150. [DOI:10.1186/s12955-019-1217-7] [PMID]
- Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee.The Journal of Bone and Joint Surgery. American volume 1998; 80(8):1132-45. [DOI:10.2106/00004623-199808000-00006] [PMID]
- Salavati M, Mazaheri M, Negahban H, Sohani S, Ebrahimian M, Ebrahimi I, et al. Validation of a Persian-version of Knee injury and Osteoarthritis Outcome Score (KOOS) in Iranians with knee injuries. Osteoarthritis and Cartilage. 2008; 16(10):1178-82. [DOI:10.1016/j.joca.2008.03.004] [PMID]
- Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: A shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005; 117(1-2):137-44. [DOI:10.1016/j.pain.2005.05.029] [PMID]
- Jafari H, Ebrahimi I, Salavati M, Kamali M, Fata L. [Psychometric properties of Iranian version of Tampa Scale for Kinesiophobia in low back pain patients (Persian)]. Archives of Rehabilitation. 2010; 11(1):15-22. [Link]
- Drouin JM, Valovich-mcLeod TC, Shultz SJ, Gansneder BM, Perrin DH. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. European Journal of Applied Physiology. 2004; 91(1):22-9. [DOI:10.1007/s00421-003-0933-0] [PMID]
- Tsepis E, Giakas G, Vagenas G, Georgoulis A. Frequency content asymmetry of the isokinetic curve between ACL deficient and healthy knee. Journal of Biomechanics. 2004; 37(6):857-64. [DOI:10.1016/j.jbiomech.2003.11.009] [PMID]
- Atarod M, Frank CB, Shrive NG. Kinematic and kinetic interactions during normal and ACL-deficient gait: A longitudinal in vivo study. Annals of Biomedical Engineering. 2014; 42(3):566-78. [DOI:10.1007/s10439-013-0914-3] [PMID]
- Matsumoto H, Suda Y, Otani T, Niki Y, Seedhom BB, Fujikawa K. Roles of the anterior cruciate ligament and the medial collateral ligament in preventing valgus instability. Journal of Orthopaedic Science. 2001; 6(1):28-32. [DOI:10.1007/s007760170021] [PMID]
- Rishiraj N, Taunton JE, Lloyd-Smith R, Woollard R, Regan W, Clement D. The potential role of prophylactic/functional knee bracing in preventing knee ligament injury. Sports Medicine. 2009; 39(11):937-60. [DOI:10.2165/11317790-000000000-00000] [PMID]
- Rishiraj N, Taunton JE, Lloyd-Smith R, Regan W, Niven B, Woollard R. Functional knee brace use effect on peak vertical ground reaction forces during drop jump landing. Knee Surgery, Sports Traumatology, Arthroscopy. 2012; 20(12):2405-12. [DOI:10.1007/s00167-012-1911-z] [PMID]
- Webster JB, Murphy DP. Atlas of orthoses and assistive devices. Philadelphia: Elsevier Health Sciences; 2019. [Link]
- Méndez-Bouza M, Alonso-Calvete A, Abalo-Núñez R. Efficacy of perturbation-based balance training in anterior cruciate ligament tears. A systematic review. Apunts Sports Medicine. 2023; 58(218):100411. [DOI:10.1016/j.apunsm.2023.100411]
- Diermeier T, Rothrauff BB, Engebretsen L, Lynch AD, Ayeni OR, Paterno MV, et al. Treatment after anterior cruciate ligament injury: Panther symposium ACL Treatment Consensus Group. British Journal of Sports Medicine. 2020; 8(6):2325967120931097. [DOI:10.1177/2325967120931097] [PMID]
- Arundale AJ, Bizzini M, Giordano A, Hewett TE, Logerstedt DS, Mandelbaum B, et al. Exercise-based knee and anterior cruciate ligament injury prevention. The Journal of Orthopaedic and Sports Physical Therapy. 2018; 48(9):A1-42. [DOI:10.2519/jospt.2018.0303] [PMID]
- Logerstedt DS, Scalzitti D, Risberg MA, Engebretsen L, Webster KE, Feller J, et al. Knee stability and movement coordination impairments: Knee ligament sprain revision 2017. The Journal of Orthopaedic and Sports Physical Therapy. 2017; 47(11):A1-47. [DOI:10.2519/jospt.2017.0303] [PMID]
- Focke A, Steingrebe H, Möhler F, Ringhof S, Sell S, Potthast W, et al. Effect of different knee braces in ACL-deficient patients. Frontiers in Bioengineering and Biotechnology. 2020; 8:964. [DOI:10.3389/fbioe.2020.00964] [PMID]
- Pierrat B, Oullion R, Molimard J, Navarro L, Combreas M, Avril S, et al. Characterisation of in-vivo mechanical action of knee braces regarding their anti-drawer effect. The Knee. 2015; 22(2):80-7. [DOI:10.1016/j.knee.2014.12.001] [PMID]
- Linczeski Z. A systematic review: The effect of prophylactic braces on reducing risk factors related to ACL injury in athletes. [MA thesis]. Michigan: Northern Michigan University; 2022. [Link]
- Murata K, Kanemura N, Kokubun T, Fujino T, Morishita Y, Onitsuka K, et al. Controlling joint instability delays the degeneration of articular cartilage in a rat model. Osteoarthritis and Cartilage. 2017; 25(2):297-308. [DOI:10.1016/j.joca.2016.10.011] [PMID]
- Edin B. Cutaneous afferents provide information about knee joint movements in humans. The Journal of Physiology. 2001; 531(1):289-97. [DOI:10.1111/j.1469-7793.2001.0289j.x] [PMID]
- Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clinical Orthopaedics and Related Research. 2002; 402:76-94. [DOI:10.1097/00003086-200209000-00008] [PMID]
- Okur I, Taspinar B, Kilit TP, Okur EO, Taspinar F. Musculoskeletal system disorders and kinesiophobia in type 2 diabetes: A case-control study. The Australian Journal of Rehabilitation Counselling. 2021; 27(1):41-9. [DOI:10.1017/jrc.2021.1]
- Reddy RS, Meziat-Filho N, Ferreira AS, Tedla JS, Kandakurti PK, Kakaraparthi VN. Comparison of neck extensor muscle endurance and cervical proprioception between asymptomatic individuals and patients with chronic neck pain. Journal of Bodywork and Movement Therapies. 2021; 26:180-6. [DOI:10.1016/j.jbmt.2020.12.040] [PMID]
- Mazaheri M, Heidari E, Mostamand J, Negahban H, van Dieen JH. Competing effects of pain and fear of pain on postural control in low back pain? Spine. 2014; 39(25):E1518-23. [DOI:10.1097/BRS.0000000000000605] [PMID]
- Smith SD, LaPrade RF, Jansson KS, Årøen A, Wijdicks CA. Functional bracing of ACL injuries: Current state and future directions. Knee Surgery, Sports Traumatology, Arthroscopy: Official Journal of the ESSKA. 2014; 22(5):1131-41. [DOI:10.1007/s00167-013-2514-z] [PMID]
- Thoma LM, Grindem H, Logerstedt D, Axe M, Engebretsen L, Risberg MA, et al. Coper classification early after ACL rupture changes with progressive neuromuscular and strength training and is associated with two-year success: The Delaware-Oslo ACL Cohort Study. The American Journal of Sports Medicine. 2019; 47(4):807-14. [DOI:10.1177/0363546519825500] [PMID]
- Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. Journal of Orthopaedic Research. 2009; 27(6):724-9. [DOI:10.1002/jor.20754] [PMID]
- Failla MJ, Logerstedt DS, Grindem H, Axe MJ, Risberg MA, Engebretsen L, et al. Does extended preoperative rehabilitation influence outcomes 2 years after ACL reconstruction? A comparative effectiveness study between the MOON and Delaware-Oslo ACL cohorts. The American Journal of Sports Medicine. 2017; 45(5):NP9. [DOI:10.1177/0363546516652594] [PMID]
Type of Study: Original |
Subject:
Orthotics & Prosthetics
Received: 12/12/2023 | Accepted: 22/04/2024 | Published: 1/01/2025
Received: 12/12/2023 | Accepted: 22/04/2024 | Published: 1/01/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |