Volume 25, Issue 2 (Summer 2024)
jrehab 2024, 25(2): 336-355 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mardani-Kivi M, Kamrani Moghadam S, Izadi A, Kazemnejad Leili E, Asadi K. Investigating the Best Time of Weight Bearing After Anterior Cruciate Ligament Reconstruction (Immediate or Delayed): A Randomized Clinical. jrehab 2024; 25 (2) :336-355
URL: http://rehabilitationj.uswr.ac.ir/article-1-3359-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3359-en.html
Mohsen Mardani-Kivi1 

 , Sina Kamrani Moghadam1
, Sina Kamrani Moghadam1 

 , Amin Izadi2
, Amin Izadi2 

 , Ehsan Kazemnejad Leili3
, Ehsan Kazemnejad Leili3 

 , Kamran Asadi *4
, Kamran Asadi *4 




 , Sina Kamrani Moghadam1
, Sina Kamrani Moghadam1 

 , Amin Izadi2
, Amin Izadi2 

 , Ehsan Kazemnejad Leili3
, Ehsan Kazemnejad Leili3 

 , Kamran Asadi *4
, Kamran Asadi *4 


1- Department of Orthopaedic, Orthopaedic Research Center, Faculty of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Orthopaedics, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Statistics, Faculty of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Orthopaedic, Orthopaedic Research Center, Faculty of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,kam_asadi@yahoo.com
2- Department of Orthopaedics, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Statistics, Faculty of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Orthopaedic, Orthopaedic Research Center, Faculty of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,
Keywords: Anterior cruciate ligament (ACL), Weight-bearing (WB), Rehabilitation, Partial weight-bearing
Full-Text [PDF 2078 kb]
(1038 Downloads)
| Abstract (HTML) (6016 Views)
Full-Text: (1752 Views)
Introduction
An anterior cruciate ligament (ACL) tear is the most common knee injury. The age- and sex-adjusted annual incidence rate (1990-2010) of ACL tears is 68.6 per 100 000 in the US [1]. Cruciate ligament ruptures are reported to be 10 times as common in athletes as in the general population [2، 3]. Reconstructing this ligament yields favorable outcomes in 75% to 97% of patients [4-6]. Advances in ACL reconstruction (ACLR) techniques and maintaining its stability have provided many adaptations in the protection of the reconstructed ligament by limiting knee extension, weight bearing (WB), and return to post-surgical activities for faster recovery. In other words, these advances and techniques enable faster rehabilitation and return of the initial range of motion and WB [7، 8].
Reports range from immediate WB to delayed WB of up to eight weeks. WB reduces knee effusion and facilitates isometric activity of the muscles around the knee. It also increases the compression and nutrition of the articular cartilage, maintains the strength of the subchondral bone, and reduces fibrosis around the patella [9-12]. However, early WB causes graft and knee instability and widens the bone tunnel compared to delayed WB post-ACLR [13، 14].
Surgeons have not reached a consensus regarding the optimal rehabilitation protocol and the best WB time after ACLR in the acute phase after surgery [15]. Recent articles have shown no benefit for brace use after ACLR in terms of pain and stability [16-19], and previous systematic reviews have reported the safety of rapid rehabilitation, early WB, and increased initial range of motion for patients [20، 21]. Due to the ambiguity of the results of previous studies about WB after ACLR, this clinical trial determines the effect of WB time (immediate or delayed) on clinical functional outcomes after ACLR with a larger sample size than previous studies.
Material and Methods
Study design
This was a single-blind clinical trial conducted in 2022 at Poursina Hospital in Rasht City, Iran. Patients with 18 to 50 years of age with complete ACL tear were included. A complete ACL tear was diagnosed by the Lachman test of +3 by an orthopedist and confirmed by knee magnetic resonance imaging. Patients with a history of any knee surgery, a history of ACL tear of the opposite knee, damage to other ligaments, any meniscus repair, abnormal knee radiography, and symptomatic ankle or hip were excluded. After providing informed consent, the patients were randomly divided into two groups. Group one included patients who were allowed to have full WB post-surgery without using a brace based on their ability and desire. Group 2 comprised patients who were asked to use a brace and have partial WB for 1 month after the surgery and full WB after a month.
Clinical evaluation and data collection
Data related to age, sex, body mass index, level of exercise (regular, irregular, none), time of returning to exercise, and the quality of returning to exercise (based on the patient’s self-report) were recorded. The Lachman test, anterior knee pain, and kneeling pain were precisely recorded in the patients’ files 1 month after the surgery. Knee function was evaluated using the international knee documentation committee (IKDC), subjective knee evaluation score, and knee injury and osteoarthritis outcome score (KOOS) questionnaires before surgery, and 1, 3, and 6 months after surgery.
Data analysis
The Fisher exact test and the chi-square test were used to compare the qualitative variables in the two groups. Repeated measures analysis of variance and the Friedman test were run to study the changes in the scores in the measurement intervals. The significance level was considered P˂0.05. All data were analyzed using the SPSS software, version 20.
Sampling method and group allocation
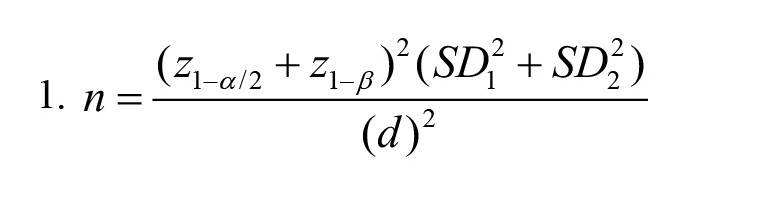
The participants were selected by consecutive sampling from patients presenting to the orthopedic department. We used the consecutive sampling method and all patients presenting to the orthopedic department who met the inclusion criteria were enrolled. The sample size was calculated at 84 patients (42 patients in each group) based on the study by Tajima et al. [22] with 95% confidence interval and 90% test power in the two-tailed test and standard deviation of the two groups at 3.4 and 1.3, respectively, and considering the statistical difference 2 scores based on the Lysholm score and Equation 1 were determined for the selected 84 patients.
Eligible patients were allocated to each group through block randomization using the Random Allocation software with 21 blocks of 4. After generating the list, a specific code was assigned to each person to identify them; therefore, based on the random sequence list and patients’ referrals, 42 patients were placed in group 1 and 42 patients in group 2. This list was kept in a sealed envelope in the Orthopedic Research Center, and after the start of the study, it was opened and read daily.
Blinding
A third person who was blinded to sampling and the type of therapeutic intervention evaluated the patients.
Surgical procedure
For all the patients, routine diagnostic arthroscopy was first performed to confirm ACL tear and find any other intra-articular pathology. Then, a 3-cm anteromedial incision was made to the tibia approximately 4 cm distal to the joint surface and 3 cm medial to the tibial tuberosity, and pes anserine was exposed by subcutaneous dissection. A subperiosteal dissection was performed up to the tendon insertion on the tibial crest to maintain maximum length. Semitendinosus and gracilis tendons were separated from the proximal muscle belly with a 10-mm tendon stripper, and a four-layer graft was used for ACLR. The femoral tunnel was reamed through arthroscopy with the anteromedial portal technique, and then, the tibial tunnel was inserted. The femoral side was fixated by an EndoButton and the tibial side was fixated by a MISBIO® absorbable interference screw.
Rehabilitation protocol
The two-week rehabilitation program was based on a combination of exercises, including range of motion, muscle strengthening, walking, physical therapy, muscle stretching, and balance and proprioceptive exercises. The first week focused on foot, ankle, and quadriceps exercises. The patient was allowed to bend the knee up to 30 degrees at the end of the first week and 45 degrees at the end of the second week. Quadriceps exercises continued and knee bending increased to 90 degrees in the third week. In the fourth week, knee bending up to 120 degrees was allowed in the form of air cycling (5 min, 3 times a day). In the fifth week, the same exercises were performed with greater knee flexion (more than 120 degrees), and in the sixth week, full range of motion exercises were performed in squats with the help of quadriceps exercises. Rehabilitation started at 3 months with squatting and running. At month 6, the patient returned to sports after evaluation. Patients in group 1 were allowed to bear full weight 24 h after surgery up to the limit without restrictions, and in group 2, they had partial WB using a brace for one month and then they were allowed to bear full weight.
Results
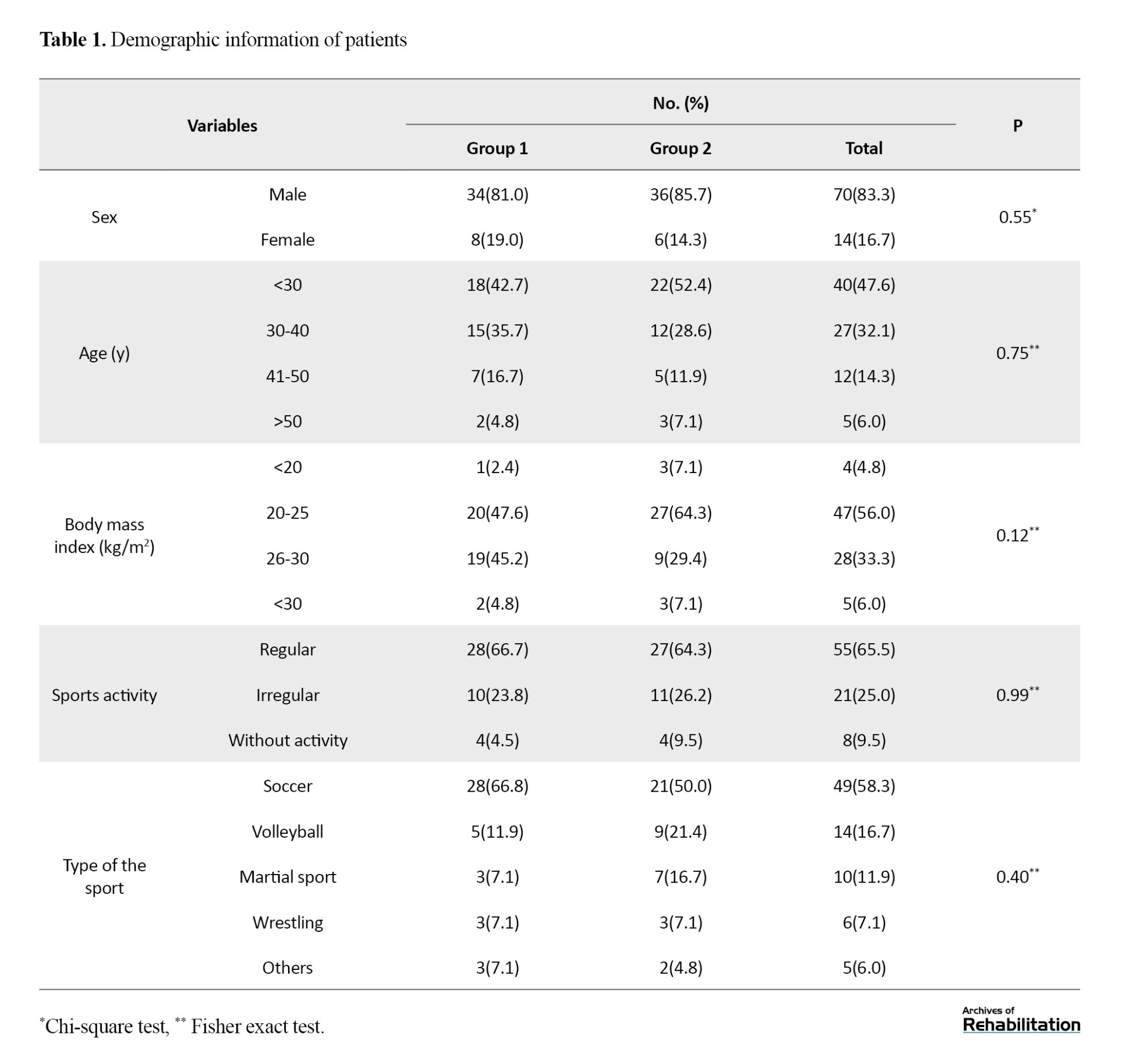
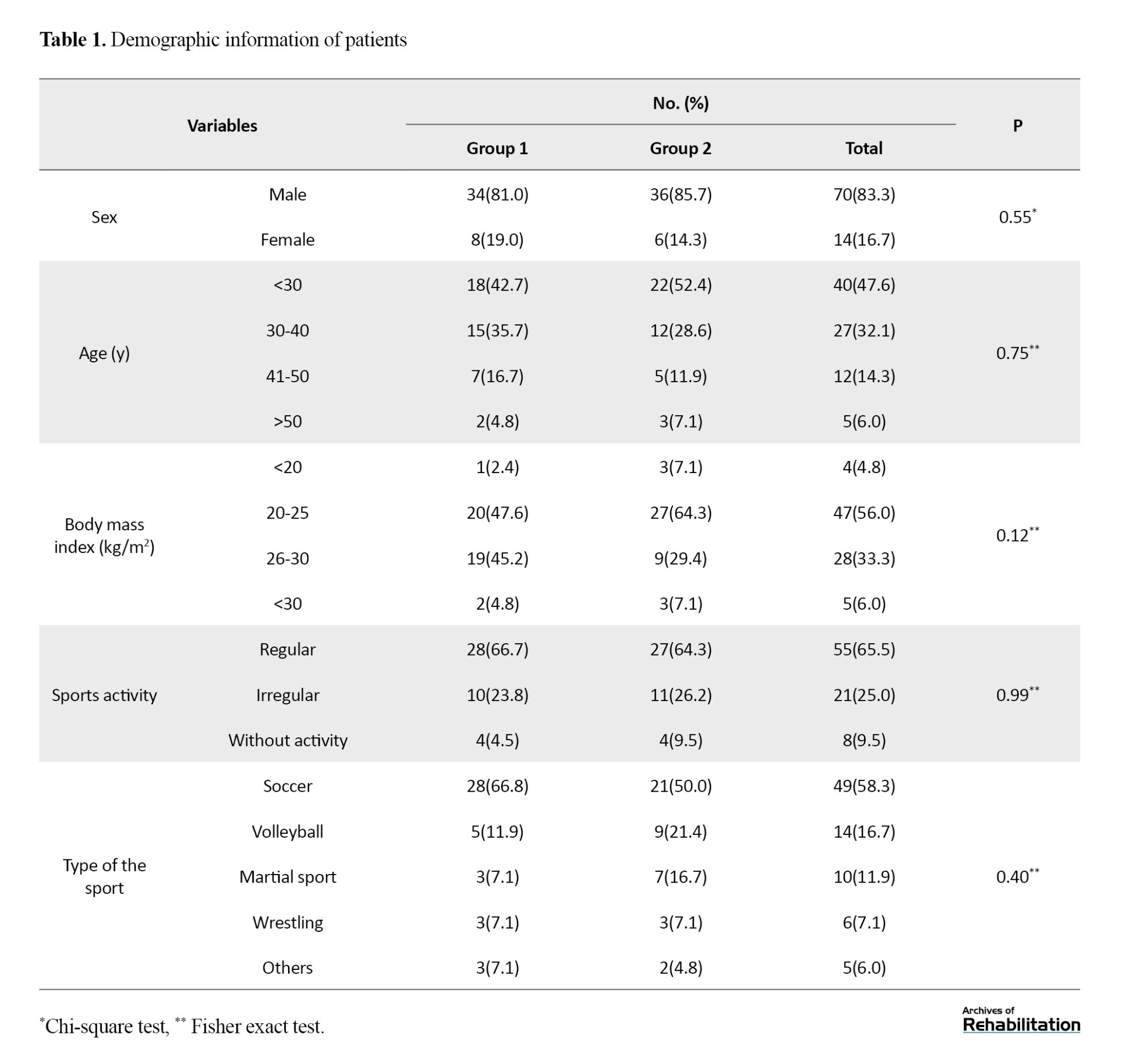
Table 1 presents patients’ basic information by group. There was no significant difference in age, sex, body mass index, exercise, and type of exercise between the two groups.
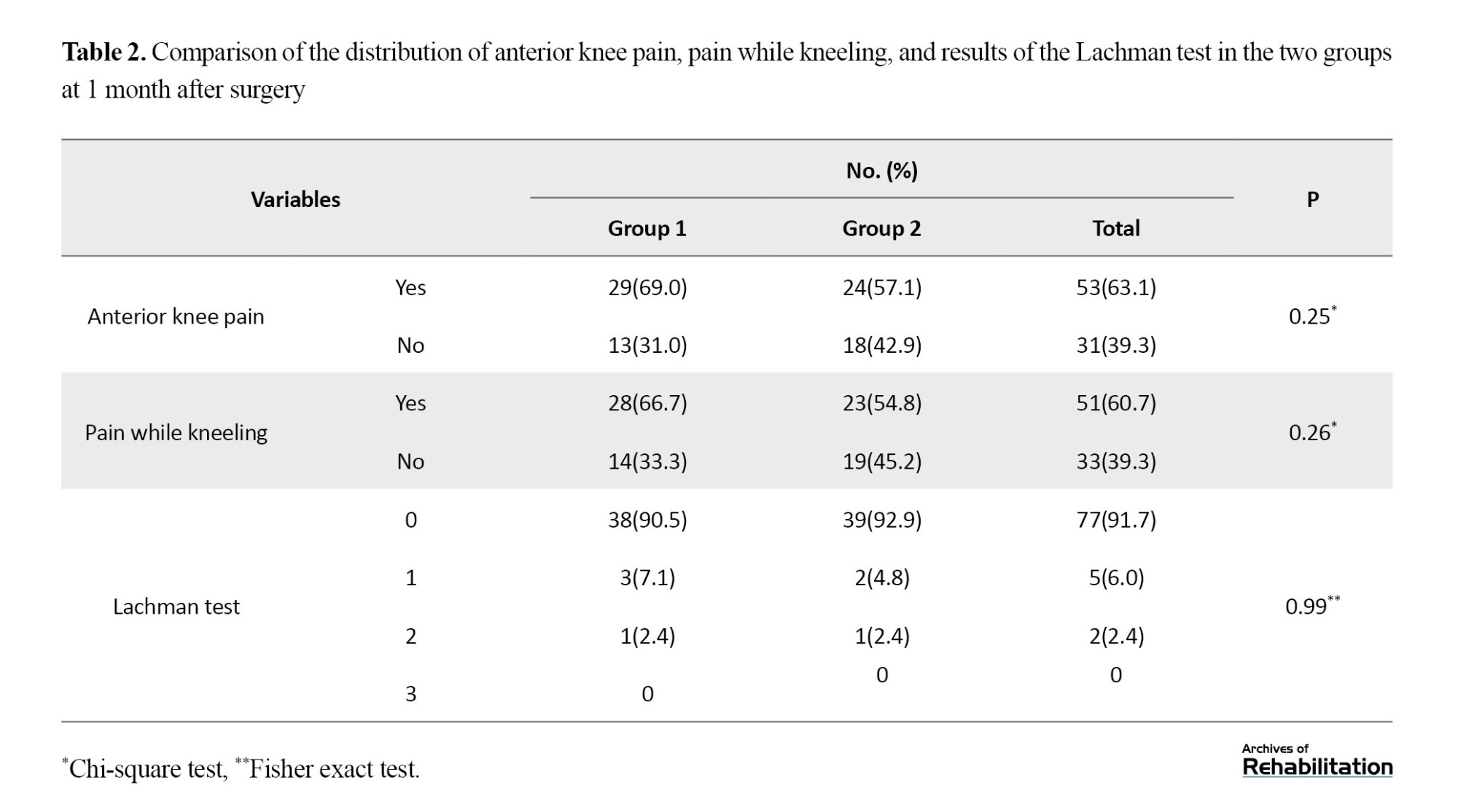
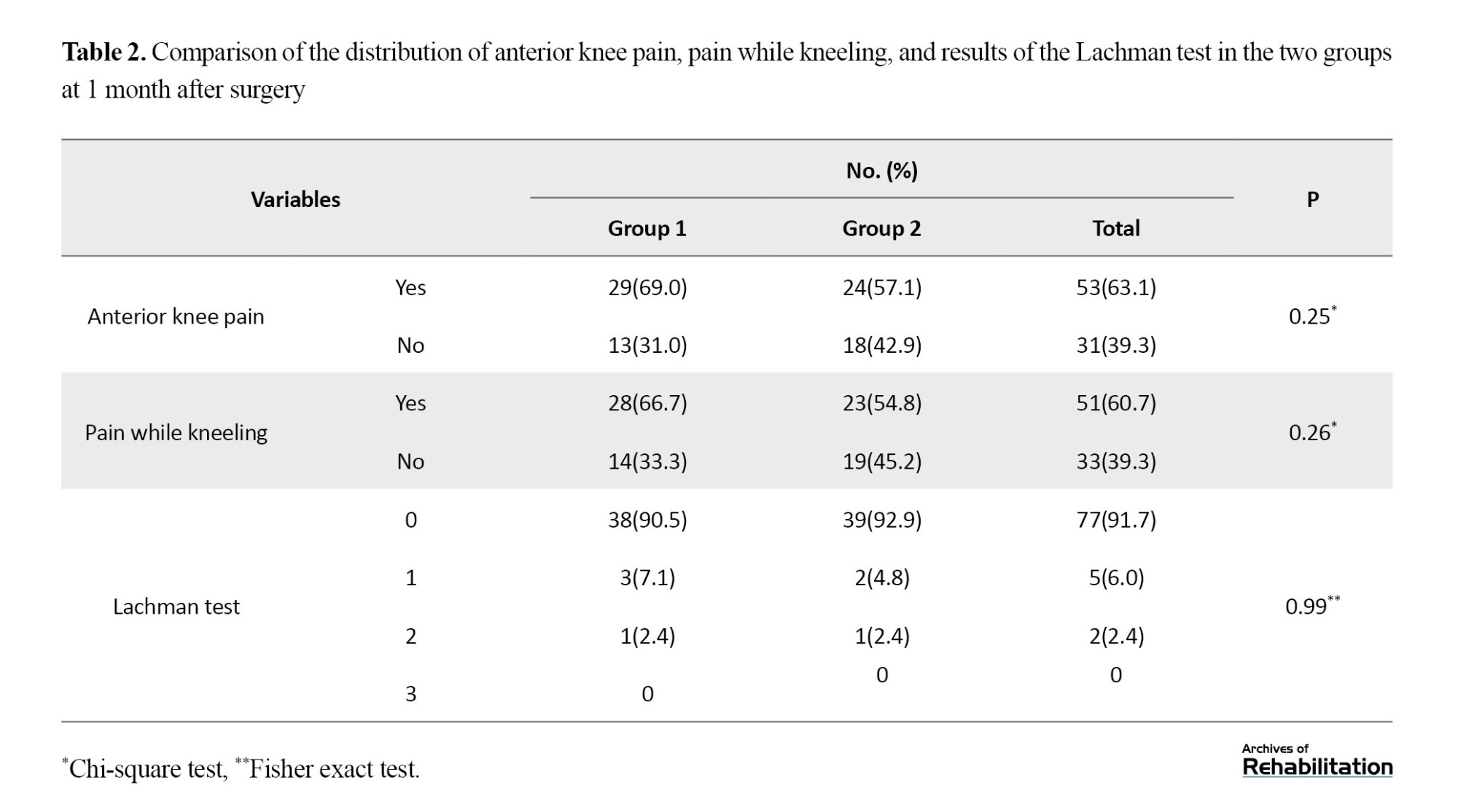
There was no significant difference in anterior knee pain and kneeling pain 1month after the surgery between the two groups. The Lachman test was also similar 1 month post-surgery between the two groups (Table 2).
There was no statistically significant difference between the two groups in terms of Lysholm score at any of the measurement time points (P>0.05). The results of the Friedman test in comparing the Lysholm score at different measurement time points in each group were significant (P<0.001); accordingly, the Lysholm score was reported higher 6 months after the operation compared to other time points. In other words, all patients improved over time.
The amount of IKDC and KOOS at time points of 1, 3, and 6 months is shown in Table 3. Accordingly, the trend of changes in IKDC and KOOS scores from before the operation to 6 months after the operation in both study groups had a significant upward trend, so time had a significant effect on improving IKDC score (power of 1 and Partial Eta Squared=0.894) and KOOS score (power of 0.962, Partial Eta Squared=0.962). Hence, the mean score increased, or the functional scores of the knee in both groups improved significantly with time (P<0.001). The mean scores of IKDC and KOOS were not statistically different between the two groups during the study, and the changes did not differ between the two groups as well (P=0.229 and P=0.385, respectively). Also, there was no significant interaction between the study groups and the measurement time points in the mean scores of IKDC and KOOS. In other words, the interaction between groups and time is not statistically significant (P=0.152 and P=0.136, respectively).
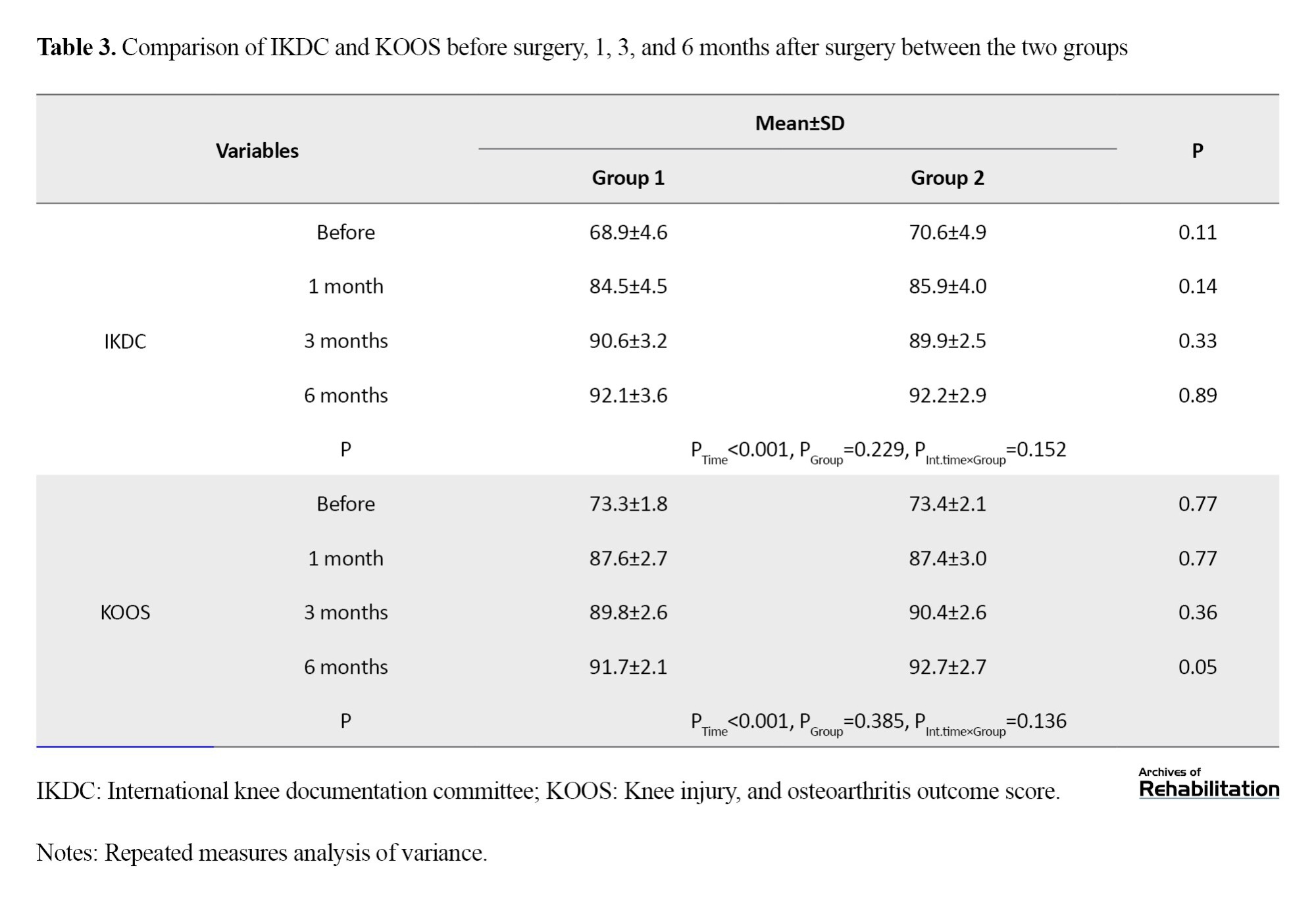
Figure 1 and Figure 2 show the changes in the average functional scores of the knee in the three time points post-surgery.
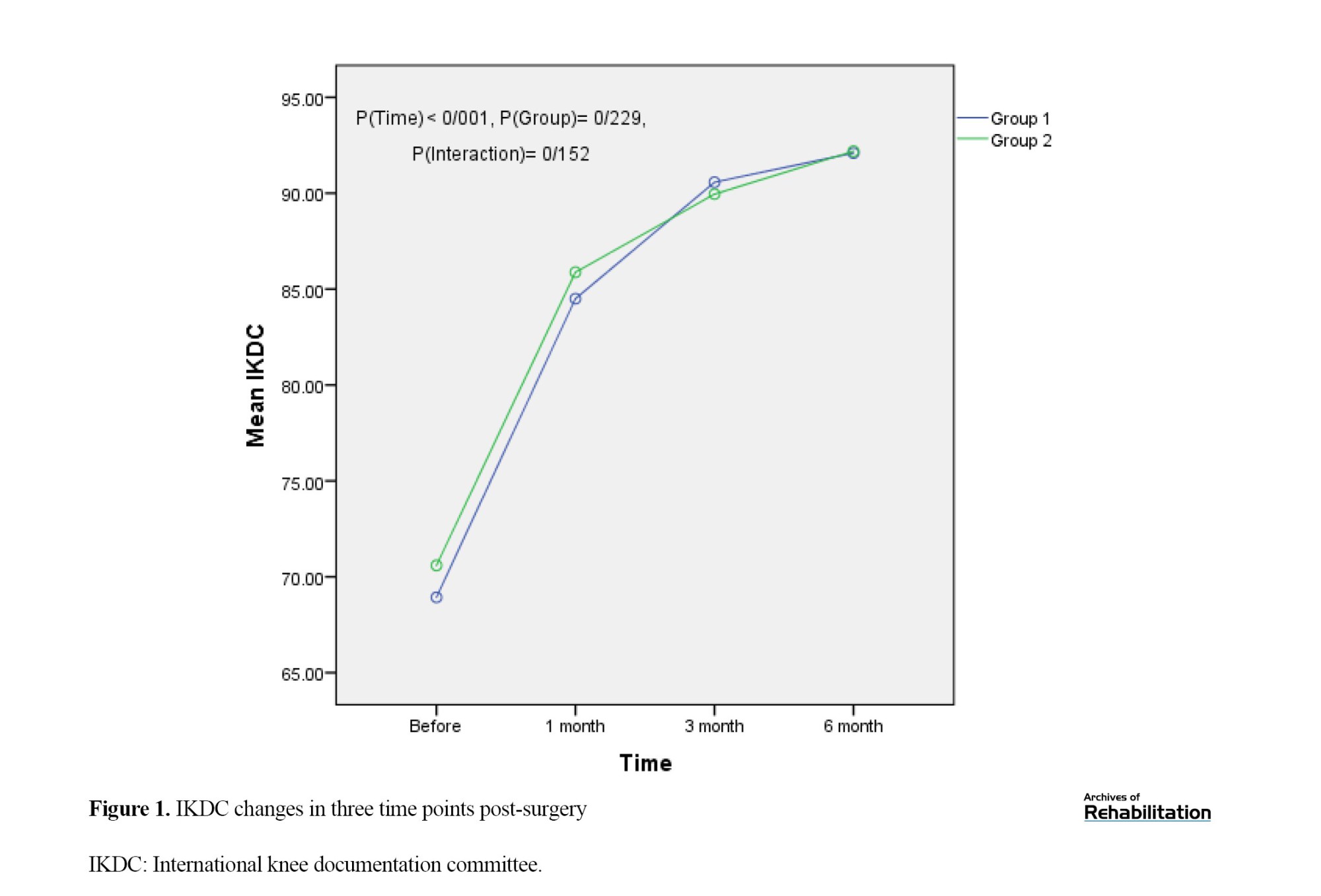
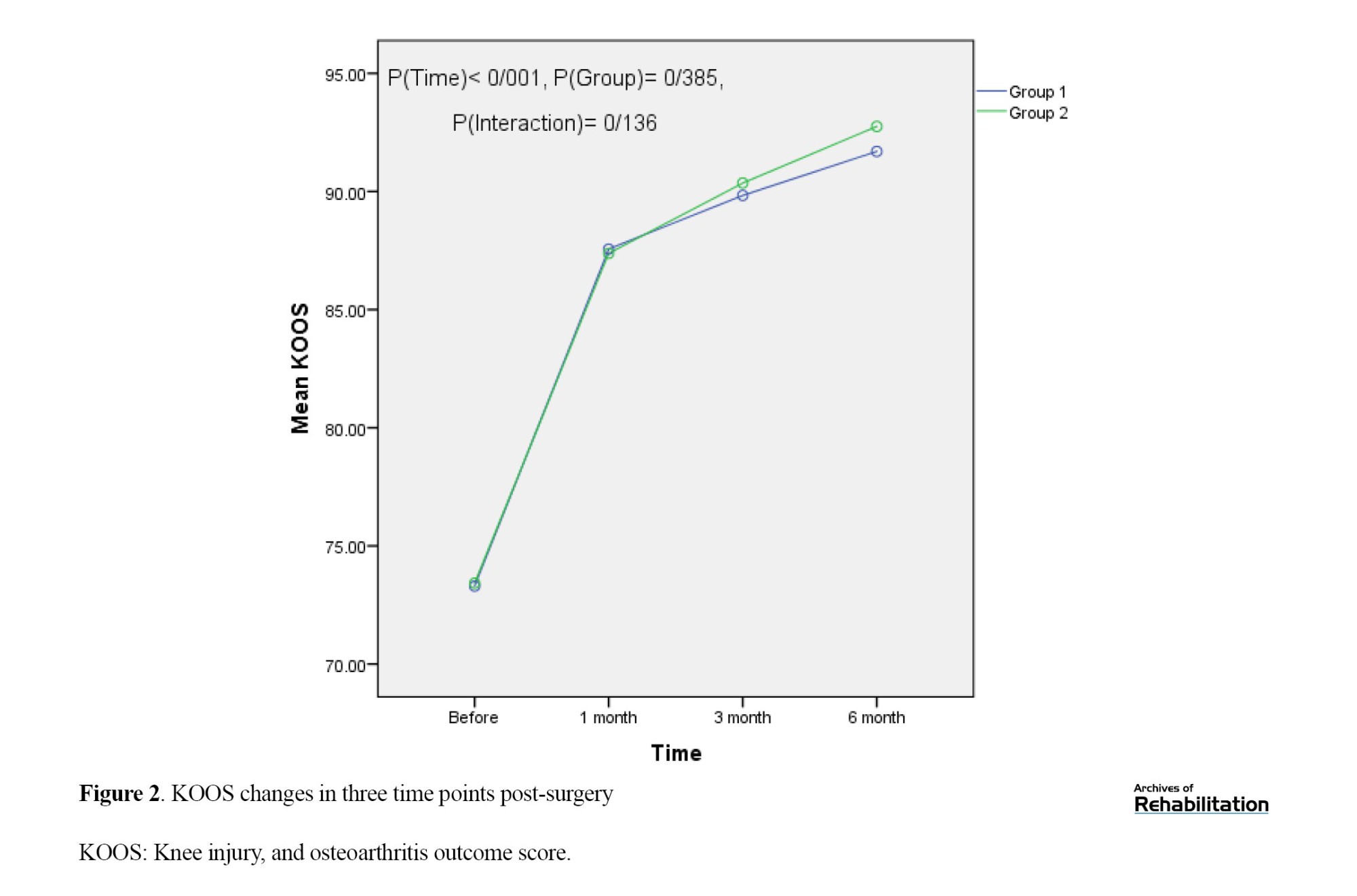
According to Figure 1, the IKDC score was not significantly different between the two groups before the operation. The mean IKDC score was higher in the full weight-bearing group than in the partial group three months after the operation and descriptively lower than at other time points. After 6 months, the two groups were descriptively closer with a 0.1 difference between their mean scores. Furthermore, the mean scores increased more sharply one month after the operation while the trend slowed down later. Figure 2 shows that before the operation, KOOS scores were not significantly different between the two groups. The mean score was 0.2 points higher in the full-weight group one month after the operation, and the two groups were close to each other and at the same point. Then the partial group descriptively scored higher than the full group with time, but this difference was not significant (P=0.136). Also, the slope of the graph is steeper one month after the operation, and then it slows down.
Discussion
ACLR is one of the most common surgeries in athletes. There is no consensus among surgeons regarding postoperative WB and its duration. In this study, the results of WB immediately after surgery without restrictions compared to partial WB with braces in the first-month post-surgery in patients with ACLR were investigated. The results revealed no significant difference between the two groups in terms of the evaluation parameters (IKDC, KOOS, and Lysholm) at different time points.
Early restoration of knee extension range of motion and early WB have been possible for more than 20 years and are the current standard of care after isolated ACLR [23]. There are consistent recommendations in rehabilitation guidelines, noting that knee mobility and strength/neuromuscular training should be started as early as possible. Wright et al. (2015) [24] and van Melick et al. (2016) [25] reported that initial knee exercises after ACL tear should be performed with full WB. On the other hand, Logerstedt et al. (2017) recommended that full post-operative WB along with exercises should start immediately after the surgery if tolerated [23].
Descriptively, pain while kneeling and pain in the front of the knee one month after surgery was less in group 2, which may be the reason for the descriptive difference due to the time of weighting. However, it was not statistically significant. The clinical outcomes of ACLR significantly improved in each group during the study time, and ACL repair similarly produced good results in both weight-bearing situations. In other words, functional clinical scores (IKDC, KOOS, and Lysholm) of the knee post-ACLR in the two groups of full and partial WB did not differ. In a study by Alsaad et al., there was no functional difference between immediate and delayed WB after ACLR, which is in line with our study [26]. Meanwhile, Di Miceli et al. concluded that bracing and delayed WB after ACLR had a negative effect on long-term functional outcomes and patients in the ACLR group who underwent full WB without a brace for four weeks after surgery scored significantly better in IKDC than patients who used a brace and delayed full WB. Their finding is inconsistent with our study [27]. Tajima et al. reported that the duration of non-WB in patients after ACLR does not differ from their clinical outcomes; in other words, there was no difference between patients who did not bear weight for one week and patients who did not bear weight for two weeks post-surgery [22]. Fan et al. showed that the IKDC score was higher in patients who had accelerated WB, but there was no statistical difference for Lysholm and KOOS scores at a follow-up of 2 years [14]. Differences in sample size and duration of follow-up, surgical method, and type of transplant may be the reason for the difference in the results of the studies. The multicenter ACL revision study group reported that full WB without support is not a risk factor affecting two-year outcomes, and WB can be initiated immediately after surgery [15]. According to the recommendations of the clinical guidelines of the American Physical Therapy Association, initial WB does not harm knee stability and function after ACLR [23].
Studies that are against early WB hold that early WB causes knee instability. A review of radiological results reported that early WB widens the femoral tunnel [22]. Taketomi stated that the pressure when putting weight on the graft deepens the femoral tunnel, and the graft-retaining wall becomes closer due to tension and causes knee instability [28]. However, most of the studies state that the widening of the bone tunnel does not clinically cause laxity of the graft [29، 30]. The results of a systematic review published in 2022 showed that early WB leads to more laxity and widening of the bone tunnel than delayed WB, which clinically does not affect the functional results, and they recommended that clinicians should choose post-operative rehabilitation programs carefully [14].
The strengths of the current study include its methodology and design as a randomized controlled clinical trial with a control group, randomization, and blinding, which reduced the potential for bias. Furthermore, we used consolidated standards of reporting trials checklist.
Conclusion
The short-term clinical and functional outcomes of WB immediately post-surgery without restrictions compared to partial WB with a brace after ACLR do not differ from each other. The present study showed that immediate WB in a rehabilitation protocol after ACL reconstruction is not harmful and does not have any adverse effect on the results, so, there is no need to use a brace immediately after surgery, and patients can bear full weight if they can tolerate it.
Study limitations
This study faced some limitations. Although we made every effort to consider all the confounding variables in the two groups, we could not examine all these variables, such as genetic status, activity intensity, compliance with rehabilitation recommendations, and post-surgery physiotherapy. Another limitation was the limited follow-up of less than two years, as in many other similar studies. The functional clinical results of the knee after ACLR did not differ in the two study groups; however, different results may be obtained in longer follow-ups. Therefore, decision-making in this case should be done with caution. In addition, the studies on this issue have been very limited with a small statistical population. It is recommended to conduct more studies with a larger sample size and longer follow-up in the future.
Ethical Considerations
Compliance with ethical guidelines
The study was fully explained to the participants and written informed consent was obtained before the study. All methods were performed following ethical approval and relevant guidelines and regulations in the study setting. The participants had the right to withdraw from the research. Also, the patients were informed that all information would remain confidential and no one would disclose it unless it was at the patient’s request. The study protocol was approved by the Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.1400.493) and registered in the Iranian Clinical Trial System (IRCT) (Code: IRCT20110809007274N17).
Funding
The present article was extracted from the residency dissertation of Sina Kamrani Moghadam, approved by Department of Orthopedics, School of Medicine, Guilan University of Medical Sciences and was supported by the Deputy of Research and Technology of Guilan University of Medical Sciences.
Authors' contributions
Conceptualization, methodology, and validation: Mohsen Mardani-Kivi, Kamran Asadi, and Sina Kamrani Moghadam; Research and data collection: Mohsen Mardani-Kivi, Sina Kamrani Moghadam, and Amin Izadi; Data analysis: Ehsan Kazemnejad Leili; Sources: Mohsen Mardani-Kivi, Kamran Asadi, Sina Kamrani Moghadam, and Amin Izadi; Writing and final approval: Mohsen Mardani-Kivi, Kamran Asadi, Sina Kamrani Moghadam, Amin Izadi, and Ehsan Kazemnejad Leili; Supervision: Mohsen Mardani-Kivi and Kamran Asadi.
Conflict of interest
The authors declared no conflict of interest.
An anterior cruciate ligament (ACL) tear is the most common knee injury. The age- and sex-adjusted annual incidence rate (1990-2010) of ACL tears is 68.6 per 100 000 in the US [1]. Cruciate ligament ruptures are reported to be 10 times as common in athletes as in the general population [2، 3]. Reconstructing this ligament yields favorable outcomes in 75% to 97% of patients [4-6]. Advances in ACL reconstruction (ACLR) techniques and maintaining its stability have provided many adaptations in the protection of the reconstructed ligament by limiting knee extension, weight bearing (WB), and return to post-surgical activities for faster recovery. In other words, these advances and techniques enable faster rehabilitation and return of the initial range of motion and WB [7، 8].
Reports range from immediate WB to delayed WB of up to eight weeks. WB reduces knee effusion and facilitates isometric activity of the muscles around the knee. It also increases the compression and nutrition of the articular cartilage, maintains the strength of the subchondral bone, and reduces fibrosis around the patella [9-12]. However, early WB causes graft and knee instability and widens the bone tunnel compared to delayed WB post-ACLR [13، 14].
Surgeons have not reached a consensus regarding the optimal rehabilitation protocol and the best WB time after ACLR in the acute phase after surgery [15]. Recent articles have shown no benefit for brace use after ACLR in terms of pain and stability [16-19], and previous systematic reviews have reported the safety of rapid rehabilitation, early WB, and increased initial range of motion for patients [20، 21]. Due to the ambiguity of the results of previous studies about WB after ACLR, this clinical trial determines the effect of WB time (immediate or delayed) on clinical functional outcomes after ACLR with a larger sample size than previous studies.
Material and Methods
Study design
This was a single-blind clinical trial conducted in 2022 at Poursina Hospital in Rasht City, Iran. Patients with 18 to 50 years of age with complete ACL tear were included. A complete ACL tear was diagnosed by the Lachman test of +3 by an orthopedist and confirmed by knee magnetic resonance imaging. Patients with a history of any knee surgery, a history of ACL tear of the opposite knee, damage to other ligaments, any meniscus repair, abnormal knee radiography, and symptomatic ankle or hip were excluded. After providing informed consent, the patients were randomly divided into two groups. Group one included patients who were allowed to have full WB post-surgery without using a brace based on their ability and desire. Group 2 comprised patients who were asked to use a brace and have partial WB for 1 month after the surgery and full WB after a month.
Clinical evaluation and data collection
Data related to age, sex, body mass index, level of exercise (regular, irregular, none), time of returning to exercise, and the quality of returning to exercise (based on the patient’s self-report) were recorded. The Lachman test, anterior knee pain, and kneeling pain were precisely recorded in the patients’ files 1 month after the surgery. Knee function was evaluated using the international knee documentation committee (IKDC), subjective knee evaluation score, and knee injury and osteoarthritis outcome score (KOOS) questionnaires before surgery, and 1, 3, and 6 months after surgery.
Data analysis
The Fisher exact test and the chi-square test were used to compare the qualitative variables in the two groups. Repeated measures analysis of variance and the Friedman test were run to study the changes in the scores in the measurement intervals. The significance level was considered P˂0.05. All data were analyzed using the SPSS software, version 20.
Sampling method and group allocation
The participants were selected by consecutive sampling from patients presenting to the orthopedic department. We used the consecutive sampling method and all patients presenting to the orthopedic department who met the inclusion criteria were enrolled. The sample size was calculated at 84 patients (42 patients in each group) based on the study by Tajima et al. [22] with 95% confidence interval and 90% test power in the two-tailed test and standard deviation of the two groups at 3.4 and 1.3, respectively, and considering the statistical difference 2 scores based on the Lysholm score and Equation 1 were determined for the selected 84 patients.
Eligible patients were allocated to each group through block randomization using the Random Allocation software with 21 blocks of 4. After generating the list, a specific code was assigned to each person to identify them; therefore, based on the random sequence list and patients’ referrals, 42 patients were placed in group 1 and 42 patients in group 2. This list was kept in a sealed envelope in the Orthopedic Research Center, and after the start of the study, it was opened and read daily.
Blinding
A third person who was blinded to sampling and the type of therapeutic intervention evaluated the patients.
Surgical procedure
For all the patients, routine diagnostic arthroscopy was first performed to confirm ACL tear and find any other intra-articular pathology. Then, a 3-cm anteromedial incision was made to the tibia approximately 4 cm distal to the joint surface and 3 cm medial to the tibial tuberosity, and pes anserine was exposed by subcutaneous dissection. A subperiosteal dissection was performed up to the tendon insertion on the tibial crest to maintain maximum length. Semitendinosus and gracilis tendons were separated from the proximal muscle belly with a 10-mm tendon stripper, and a four-layer graft was used for ACLR. The femoral tunnel was reamed through arthroscopy with the anteromedial portal technique, and then, the tibial tunnel was inserted. The femoral side was fixated by an EndoButton and the tibial side was fixated by a MISBIO® absorbable interference screw.
Rehabilitation protocol
The two-week rehabilitation program was based on a combination of exercises, including range of motion, muscle strengthening, walking, physical therapy, muscle stretching, and balance and proprioceptive exercises. The first week focused on foot, ankle, and quadriceps exercises. The patient was allowed to bend the knee up to 30 degrees at the end of the first week and 45 degrees at the end of the second week. Quadriceps exercises continued and knee bending increased to 90 degrees in the third week. In the fourth week, knee bending up to 120 degrees was allowed in the form of air cycling (5 min, 3 times a day). In the fifth week, the same exercises were performed with greater knee flexion (more than 120 degrees), and in the sixth week, full range of motion exercises were performed in squats with the help of quadriceps exercises. Rehabilitation started at 3 months with squatting and running. At month 6, the patient returned to sports after evaluation. Patients in group 1 were allowed to bear full weight 24 h after surgery up to the limit without restrictions, and in group 2, they had partial WB using a brace for one month and then they were allowed to bear full weight.
Results
Table 1 presents patients’ basic information by group. There was no significant difference in age, sex, body mass index, exercise, and type of exercise between the two groups.
There was no significant difference in anterior knee pain and kneeling pain 1month after the surgery between the two groups. The Lachman test was also similar 1 month post-surgery between the two groups (Table 2).
There was no statistically significant difference between the two groups in terms of Lysholm score at any of the measurement time points (P>0.05). The results of the Friedman test in comparing the Lysholm score at different measurement time points in each group were significant (P<0.001); accordingly, the Lysholm score was reported higher 6 months after the operation compared to other time points. In other words, all patients improved over time.
The amount of IKDC and KOOS at time points of 1, 3, and 6 months is shown in Table 3. Accordingly, the trend of changes in IKDC and KOOS scores from before the operation to 6 months after the operation in both study groups had a significant upward trend, so time had a significant effect on improving IKDC score (power of 1 and Partial Eta Squared=0.894) and KOOS score (power of 0.962, Partial Eta Squared=0.962). Hence, the mean score increased, or the functional scores of the knee in both groups improved significantly with time (P<0.001). The mean scores of IKDC and KOOS were not statistically different between the two groups during the study, and the changes did not differ between the two groups as well (P=0.229 and P=0.385, respectively). Also, there was no significant interaction between the study groups and the measurement time points in the mean scores of IKDC and KOOS. In other words, the interaction between groups and time is not statistically significant (P=0.152 and P=0.136, respectively).
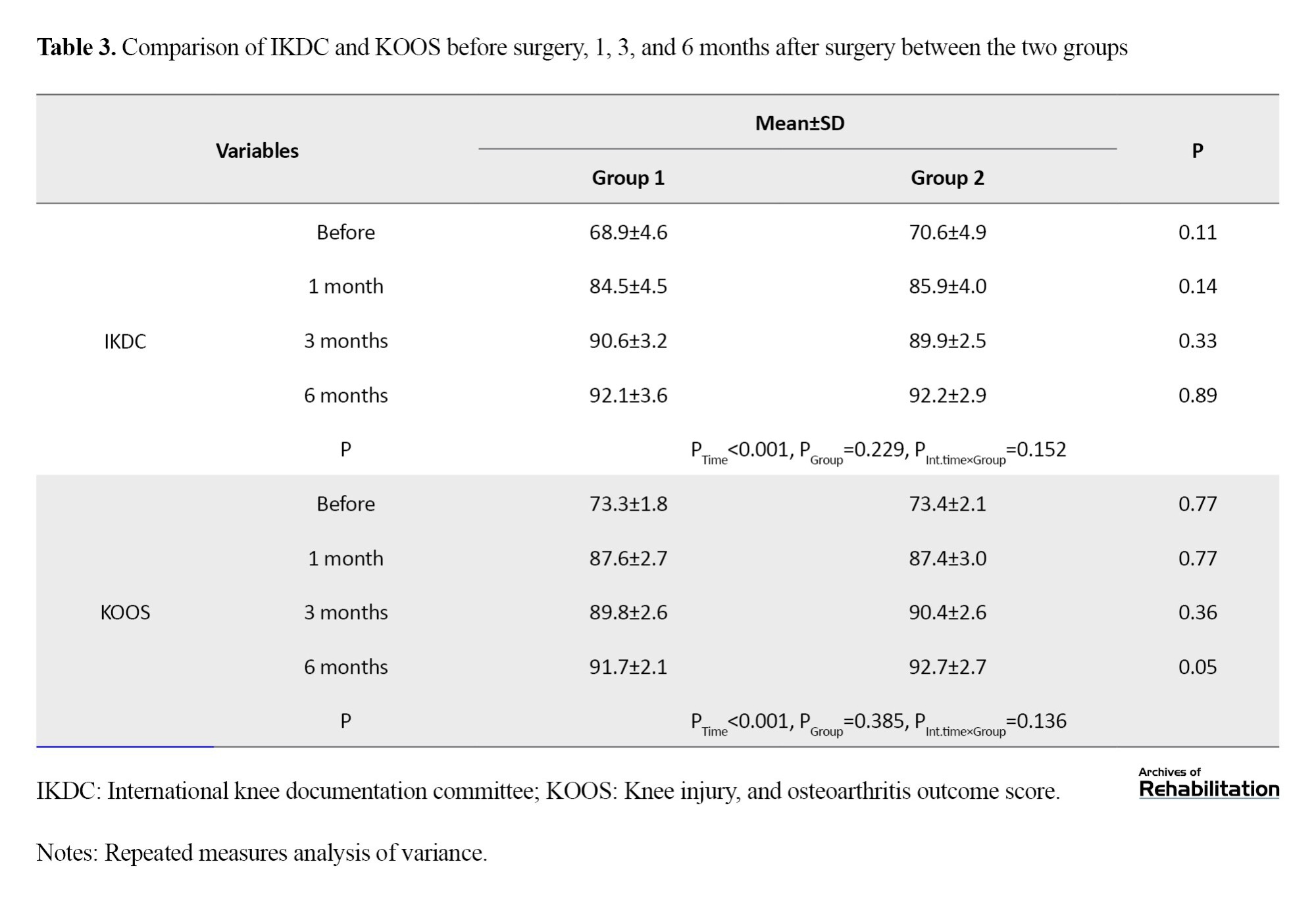
Figure 1 and Figure 2 show the changes in the average functional scores of the knee in the three time points post-surgery.
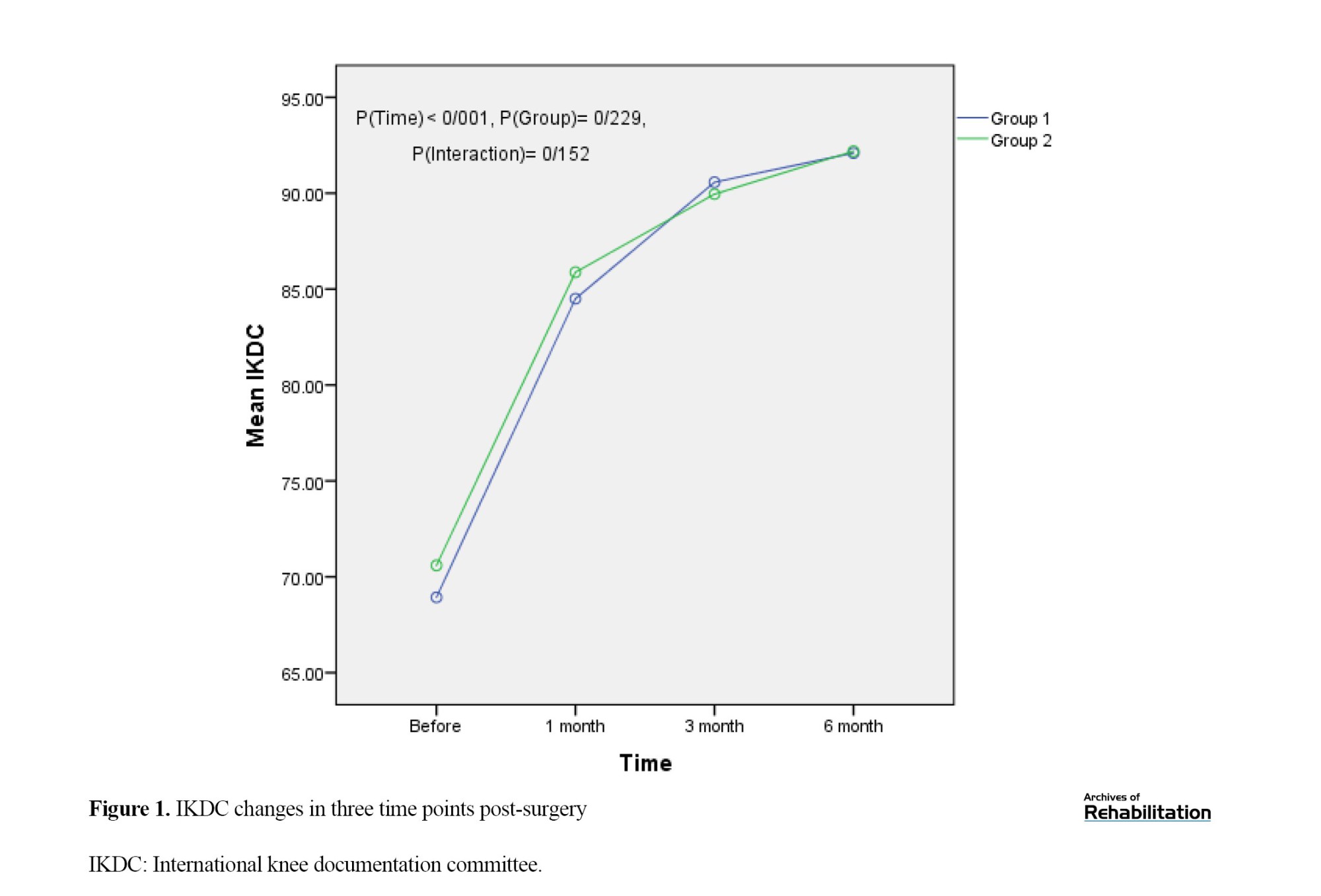
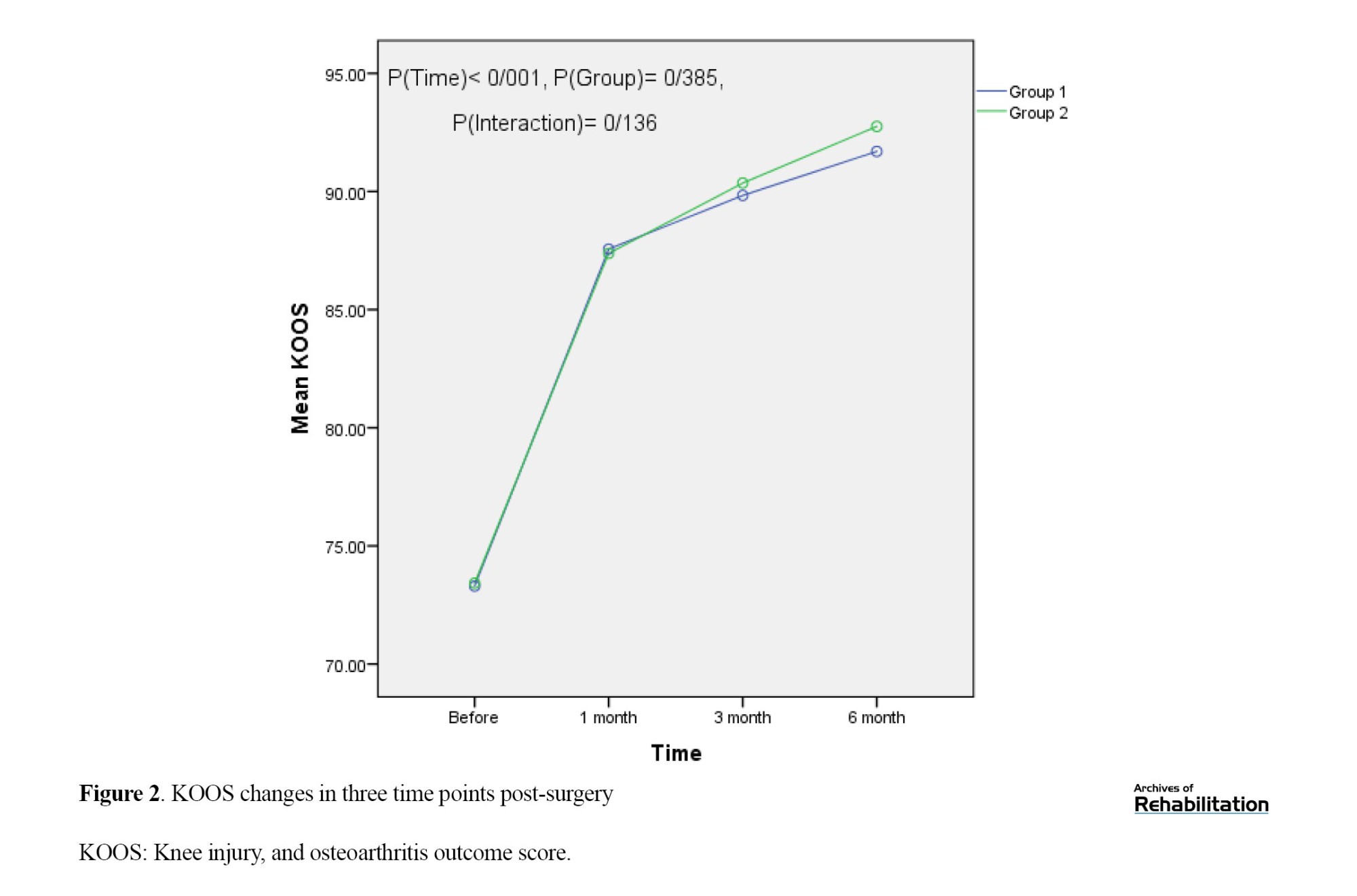
According to Figure 1, the IKDC score was not significantly different between the two groups before the operation. The mean IKDC score was higher in the full weight-bearing group than in the partial group three months after the operation and descriptively lower than at other time points. After 6 months, the two groups were descriptively closer with a 0.1 difference between their mean scores. Furthermore, the mean scores increased more sharply one month after the operation while the trend slowed down later. Figure 2 shows that before the operation, KOOS scores were not significantly different between the two groups. The mean score was 0.2 points higher in the full-weight group one month after the operation, and the two groups were close to each other and at the same point. Then the partial group descriptively scored higher than the full group with time, but this difference was not significant (P=0.136). Also, the slope of the graph is steeper one month after the operation, and then it slows down.
Discussion
ACLR is one of the most common surgeries in athletes. There is no consensus among surgeons regarding postoperative WB and its duration. In this study, the results of WB immediately after surgery without restrictions compared to partial WB with braces in the first-month post-surgery in patients with ACLR were investigated. The results revealed no significant difference between the two groups in terms of the evaluation parameters (IKDC, KOOS, and Lysholm) at different time points.
Early restoration of knee extension range of motion and early WB have been possible for more than 20 years and are the current standard of care after isolated ACLR [23]. There are consistent recommendations in rehabilitation guidelines, noting that knee mobility and strength/neuromuscular training should be started as early as possible. Wright et al. (2015) [24] and van Melick et al. (2016) [25] reported that initial knee exercises after ACL tear should be performed with full WB. On the other hand, Logerstedt et al. (2017) recommended that full post-operative WB along with exercises should start immediately after the surgery if tolerated [23].
Descriptively, pain while kneeling and pain in the front of the knee one month after surgery was less in group 2, which may be the reason for the descriptive difference due to the time of weighting. However, it was not statistically significant. The clinical outcomes of ACLR significantly improved in each group during the study time, and ACL repair similarly produced good results in both weight-bearing situations. In other words, functional clinical scores (IKDC, KOOS, and Lysholm) of the knee post-ACLR in the two groups of full and partial WB did not differ. In a study by Alsaad et al., there was no functional difference between immediate and delayed WB after ACLR, which is in line with our study [26]. Meanwhile, Di Miceli et al. concluded that bracing and delayed WB after ACLR had a negative effect on long-term functional outcomes and patients in the ACLR group who underwent full WB without a brace for four weeks after surgery scored significantly better in IKDC than patients who used a brace and delayed full WB. Their finding is inconsistent with our study [27]. Tajima et al. reported that the duration of non-WB in patients after ACLR does not differ from their clinical outcomes; in other words, there was no difference between patients who did not bear weight for one week and patients who did not bear weight for two weeks post-surgery [22]. Fan et al. showed that the IKDC score was higher in patients who had accelerated WB, but there was no statistical difference for Lysholm and KOOS scores at a follow-up of 2 years [14]. Differences in sample size and duration of follow-up, surgical method, and type of transplant may be the reason for the difference in the results of the studies. The multicenter ACL revision study group reported that full WB without support is not a risk factor affecting two-year outcomes, and WB can be initiated immediately after surgery [15]. According to the recommendations of the clinical guidelines of the American Physical Therapy Association, initial WB does not harm knee stability and function after ACLR [23].
Studies that are against early WB hold that early WB causes knee instability. A review of radiological results reported that early WB widens the femoral tunnel [22]. Taketomi stated that the pressure when putting weight on the graft deepens the femoral tunnel, and the graft-retaining wall becomes closer due to tension and causes knee instability [28]. However, most of the studies state that the widening of the bone tunnel does not clinically cause laxity of the graft [29، 30]. The results of a systematic review published in 2022 showed that early WB leads to more laxity and widening of the bone tunnel than delayed WB, which clinically does not affect the functional results, and they recommended that clinicians should choose post-operative rehabilitation programs carefully [14].
The strengths of the current study include its methodology and design as a randomized controlled clinical trial with a control group, randomization, and blinding, which reduced the potential for bias. Furthermore, we used consolidated standards of reporting trials checklist.
Conclusion
The short-term clinical and functional outcomes of WB immediately post-surgery without restrictions compared to partial WB with a brace after ACLR do not differ from each other. The present study showed that immediate WB in a rehabilitation protocol after ACL reconstruction is not harmful and does not have any adverse effect on the results, so, there is no need to use a brace immediately after surgery, and patients can bear full weight if they can tolerate it.
Study limitations
This study faced some limitations. Although we made every effort to consider all the confounding variables in the two groups, we could not examine all these variables, such as genetic status, activity intensity, compliance with rehabilitation recommendations, and post-surgery physiotherapy. Another limitation was the limited follow-up of less than two years, as in many other similar studies. The functional clinical results of the knee after ACLR did not differ in the two study groups; however, different results may be obtained in longer follow-ups. Therefore, decision-making in this case should be done with caution. In addition, the studies on this issue have been very limited with a small statistical population. It is recommended to conduct more studies with a larger sample size and longer follow-up in the future.
Ethical Considerations
Compliance with ethical guidelines
The study was fully explained to the participants and written informed consent was obtained before the study. All methods were performed following ethical approval and relevant guidelines and regulations in the study setting. The participants had the right to withdraw from the research. Also, the patients were informed that all information would remain confidential and no one would disclose it unless it was at the patient’s request. The study protocol was approved by the Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.1400.493) and registered in the Iranian Clinical Trial System (IRCT) (Code: IRCT20110809007274N17).
Funding
The present article was extracted from the residency dissertation of Sina Kamrani Moghadam, approved by Department of Orthopedics, School of Medicine, Guilan University of Medical Sciences and was supported by the Deputy of Research and Technology of Guilan University of Medical Sciences.
Authors' contributions
Conceptualization, methodology, and validation: Mohsen Mardani-Kivi, Kamran Asadi, and Sina Kamrani Moghadam; Research and data collection: Mohsen Mardani-Kivi, Sina Kamrani Moghadam, and Amin Izadi; Data analysis: Ehsan Kazemnejad Leili; Sources: Mohsen Mardani-Kivi, Kamran Asadi, Sina Kamrani Moghadam, and Amin Izadi; Writing and final approval: Mohsen Mardani-Kivi, Kamran Asadi, Sina Kamrani Moghadam, Amin Izadi, and Ehsan Kazemnejad Leili; Supervision: Mohsen Mardani-Kivi and Kamran Asadi.
Conflict of interest
The authors declared no conflict of interest.
References
- Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. The American Journal of Sports Medicine. 2016; 44(6):1502-7. [DOI:10.1177/0363546516629944] [PMID]
- Chen G, Wang S. Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: a meta-analysis of randomized controlled trials. International Journal of Clinical and Experimental Medicine. 2015; 8(9):14604-14. [PMID] [PMCID]
- Goshima K, Kitaoka K, Nakase J, Tsuchiya H. Familial predisposition to anterior cruciate ligament injury. Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology. 2014; 1(2):62-6. [DOI:10.1016/j.asmart.2014.02.002]
- Grassi A, Ardern CL, Marcheggiani Muccioli GM, Neri MP, Marcacci M, Zaffagnini S. Does revision ACL reconstruction measure up to primary surgery? A meta-analysis comparing patient-reported and clinician-reported outcomes, and radiographic results. British Journal of Sports Medicine. 2016; 50(12):716-24. [DOI:10.1136/bjsports-2015-094948] [PMID]
- Jenny JY, Clement X. Patient-based decision for resuming activity after ACL reconstruction: A single-centre experience. European Journal of Orthopaedic Surgery & Traumatology. 2016; 26(8):929-35. [DOI:10.1007/s00590-016-1861-0] [PMID]
- Geib TM, Shelton WR, Phelps RA, Clark L. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: Intermediate-term outcome. Arthroscopy. 2009; 25(12):1408-14. [DOI:10.1016/j.arthro.2009.06.004] [PMID]
- Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. The American Journal of Sports Medicine. 1997; 25(6):786-95. [DOI:10.1177/036354659702500610] [PMID]
- Shelbourne KD, Klotz C. What I have learned about the ACL: Utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. Journal of Orthopaedic Science. 2006; 11(3):318-25. [DOI:10.1007/s00776-006-1007-z] [PMID] [PMCID]
- Rizer M, Foremny GB, Rush A, 3rd, Singer AD, Baraga M, Kaplan LD, et al. Anterior cruciate ligament reconstruction tunnel size: causes of tunnel enlargement and implications for single versus two-stage revision reconstruction. Skeletal Radiology. 2017; 46(2):161-9. [DOI:10.1007/s00256-016-2535-z] [PMID]
- Harput G, Howard JS, Mattacola C. Comparison of muscle activation levels between healthy individuals and persons who have undergone anterior cruciate ligament reconstruction during different phases of weight-bearing exercises. The Journal of Orthopaedic and Sports Physical Therapy. 2016; 46(11):984-92. [DOI:10.2519/jospt.2016.5896] [PMID]
- Sritharan P, Schache AG, Culvenor AG, Perraton LG, Bryant AL, Crossley KM. Between-limb differences in patellofemoral joint forces during running at 12 to 24 months after unilateral anterior cruciate ligament reconstruction. The American Journal of Sports Medicine. 2020; 48(7):1711-9. [DOI:10.1177/0363546520914628] [PMID]
- Lin PE, Sigward SM. Influence of hamstrings on knee moments during loading response of gait in individuals following ACL reconstruction. Journal of Orthopaedic Research. 2020; 38(2):378-86.[DOI:10.1002/jor.24465] [PMID]
- Tyler TF, McHugh MP, Gleim GW, Nicholas SJ. The effect of immediate weightbearing after anterior cruciate ligament reconstruction. Clinical Orthopaedics and Related Research. 1998; (357):141-8. [DOI:10.1097/00003086-199812000-00019] [PMID]
- Fan Z, Yan J, Zhou Z, Gao Y, Tang J, Li Y, et al. Delayed versus accelerated weight-bearing rehabilitation protocol following anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Journal of Rehabilitation Medicine. 2022; 54:jrm00260. [DOI:10.2340/jrm.v53.1438] [PMID] [PMCID]
- MARS Group. Rehabilitation predictors of clinical outcome following revision ACL reconstruction in the MARS cohort. The Journal of Bone and Joint Surgery. American volume. 2019; 101(9):779-86. [DOI:10.2106/JBJS.18.00397] [PMID] [PMCID]
- Bordes P, Laboute E, Bertolotti A, Dalmay JF, Puig P, Trouve P, et al. No beneficial effect of bracing after anterior cruciate ligament reconstruction in a cohort of 969 athletes followed in rehabilitation. Annals of Physical and Rehabilitation Medicine. 2017; 60(4):230-6. [DOI:10.1016/j.rehab.2017.02.001] [PMID]
- Mayr HO, Stüeken P, Münch EO, Wolter M, Bernstein A, Suedkamp NP, et al. Brace or no-brace after ACL graft? Four-year results of a prospective clinical trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2014; 22(5):1156-62. [DOI:10.1007/s00167-013-2564-2] [PMID]
- Lindström M, Wredmark T, Wretling ML, Henriksson M, Felländer-Tsai L. Post-operative bracing after ACL reconstruction has no effect on knee joint effusion. A prospective, randomized study. The Knee. 2015; 22(6):559-64. [DOI:10.1016/j.knee.2015.04.015] [PMID]
- Wright RW, Fetzer GB. Bracing after ACL reconstruction: A systematic review. Clinical Orthopaedics and Related Research. 2007; 455:162-8. [DOI:10.1097/BLO.0b013e31802c9360] [PMID]
- Kruse LM, Gray B, Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: A systematic review. The Journal of Bone and Joint Surgery. 2012; 94(19):1737-48. [DOI:10.2106/JBJS.K.01246] [PMID] [PMCID]
- Wright RW, Preston E, Fleming BC, Amendola A, Andrish JT, Bergfeld JA, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: Part II: Open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. The Journal of Knee Surgery. 2008; 21(3):225-34. [DOI:10.1055/s-0030-1247823] [PMID] [PMCID]
- Tajima T, Yamaguchi N, Nagasawa M, Morita Y, Nakamura Y, Chosa E. Early weight-bearing after anterior cruciate ligament reconstruction with hamstring grafts induce femoral bone tunnel enlargement: A prospective clinical and radiographic study. BMC Musculoskeletal Disorders. 2019; 20(1):274. [DOI:10.1186/s12891-019-2653-6] [PMID] [PMCID]
- Logerstedt DS, Scalzitti D, Risberg MA, Engebretsen L, Webster KE, Feller J, et al. Knee stability and movement coordination impairments: Knee ligament sprain revision 2017. The Journal of Orthopaedic and Sports Physical Therapy. 2017 ; 47(11):A1-47. [DOI:10.2519/jospt.2017.0303] [PMID]
- Wright RW, Haas AK, Anderson J, Calabrese G, Cavanaugh J, Hewett TE, et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. sports health. 2015; 7(3):239-43. [DOI:10.1177/1941738113517855] [PMID] [PMCID]
- van Melick N, van Cingel RE, Brooijmans F, Neeter C, van Tienen T, Hullegie W, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. British Journal of Sports Medicine. 2016; 50(24):1506-15. [DOI:10.1136/bjsports-2015-095898] [PMID]
- Alsaad MA, Alsaffa AH, Alharris MA. Comparison between immediate and delayed weight bearing in arthroscopically assisted anterior cruciate ligament reconstruction. Al-Anbar Medical Journal. 2019; 15(2):30-4. [DOI:10.33091/amj.2019.170896]
- Di Miceli R, Marambio CB, Zati A, Monesi R, Benedetti MG. Do knee bracing and delayed weight bearing affect mid-term functional outcome after anterior cruciate ligament reconstruction? Joints. 2017; 5(4):202-6. [DOI:10.1055/s-0037-1606617] [PMID] [PMCID]
- Taketomi S. Editorial commentary: Tunnel widening after anterior cruciate ligament reconstruction may increase laxity and complicate revision. Arthroscopy. 2021; 37(8):2564-6. [DOI:10.1016/j.arthro.2021.04.013] [PMID]
- Clatworthy MG, Annear P, Bulow JU, Bartlett RJ. Tunnel widening in anterior cruciate ligament reconstruction: A prospective evaluation of hamstring and patella tendon grafts. Knee Surgery, Sports Traumatology, Arthroscopy. 1999; 7(3):138-45. [DOI:10.1007/s001670050138] [PMID]
- Linn RM, Fischer DA, Smith JP, Burstein DB, Quick DC. Achilles tendon allograft reconstruction of the anterior cruciate ligament-deficient knee. The American Journal of Sports Medicine. 1993; 21(6):825-31. [DOI:10.1177/036354659302100611] [PMID]
Type of Study: Original |
Subject:
Rehabilitation Management
Received: 9/09/2023 | Accepted: 8/05/2024 | Published: 1/07/2024
Received: 9/09/2023 | Accepted: 8/05/2024 | Published: 1/07/2024
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |