Volume 25, Issue 2 (Summer 2024)
jrehab 2024, 25(2): 292-311 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
A’rabi M, Fatorehchy S, Hosseini S A, Bakhshi E, Alavian S. The Effect of Planovalgus on Balance and Motor Function in Children With Cerebral Palsy. jrehab 2024; 25 (2) :292-311
URL: http://rehabilitationj.uswr.ac.ir/article-1-3344-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3344-en.html
Mahsa A’rabi1 

 , Saeid Fatorehchy *2
, Saeid Fatorehchy *2 

 , Seyed Ali Hosseini1
, Seyed Ali Hosseini1 

 , Enayatollah Bakhshi3
, Enayatollah Bakhshi3 

 , Seyedmostafa Alavian4
, Seyedmostafa Alavian4 




 , Saeid Fatorehchy *2
, Saeid Fatorehchy *2 

 , Seyed Ali Hosseini1
, Seyed Ali Hosseini1 

 , Enayatollah Bakhshi3
, Enayatollah Bakhshi3 

 , Seyedmostafa Alavian4
, Seyedmostafa Alavian4 


1- Department of Occupational Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Occupational Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,saeidfatorehchy@yahoo.com
3- Department of Biostatistics and Epidemiology, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Biomechanics, Faculty of Mechanical Engineering, Sharif University of Technology, Tehran, Iran.
2- Department of Occupational Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Department of Biostatistics and Epidemiology, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Biomechanics, Faculty of Mechanical Engineering, Sharif University of Technology, Tehran, Iran.
Keywords: Cerebral palsy (CP), Pes planovalgus, Functional balance, Pain, Range of motion, Muscle strength
Full-Text [PDF 2014 kb]
(945 Downloads)
| Abstract (HTML) (5238 Views)
Full-Text: (1170 Views)
Introduction
Cerebral palsy (CP) is a group of permanent movement and posture disorders that lead to limitations in the performance of activities and occur as a result of non-progressive disorders in the developing brain of a fetus or infant [1]. Brain damage in these children leads to abnormal muscle activity, impaired weight bearing, and limited movement due to muscle shortening, which in turn leads to secondary musculoskeletal and movement problems [2]. One of the most important functional mobility deformities whose treatment is still debated is the planovalgus deformity in children with bilateral spastic CP as one of the most common deformities [3، 4] associated with shortening of the Achilles tendon of the lower limbs and causes pain or other symptoms with increased activity and increased body mass index. These symptoms become more noticeable after the age of 10 years and can last into adulthood, leaving people unable to walk [5]. As a common deformity of the foot, the characteristics of planovalgus include hind foot valgus, midfoot pronation, decreased medial longitudinal arch, and forefoot abduction/supination [6، 7]. Although the primary cause of planovalgus deformity is still unknown, people with this deformity frequently experience pain, functional impairment, and lower limb contracture [7]. According to a 2016 study on CP aimed at improving walking in children with this disorder, the maturation of balance skills in these children was also delayed or reduced compared to typically developing children. Over time, these defects lead to problems in balance and foot center of pressure. Therefore, balance and walking disorders, including asymmetry in the lower limbs, are some of the complications of this phenomenon, which can lead to further dysfunction in ambulatory children with CP [8]. Optimum walking performance comes from using the ground reaction force. Meanwhile, the optimal use of this force requires the proper performance of the ankle’s plantar flexors [9]. According to Miller’s study in 2022, a planovalgus deformity impairs plantar flexor function and ground reaction force by causing structural changes in the foot and ankle. This study shows that the performance level of gross movements of these children alone is the most important factor influencing the progress of radiological indicators in the treatment of planovalgus deformities [10]. The results of research conducted in the field of planovalgus deformity show that early detection of planovalgus deformity is essential to prevent aggravation of leg injuries [11].
Ambulatory children with CP who are referred to medical centers and have planovalgus deformity in the ankles typically use the crutch walking pattern that is most common in these children. Due to spasticity, muscle contractions, and limitation of movement of the joints of the lower limbs, there is a loss of functional capabilities in these children [12]. Although this deformity is known to persist into adulthood, little information has been published regarding the natural history and treatment of planovalgus. Furthermore, there is no clarity regarding the need for non-surgical or surgical treatment [13]. Since the presence of planovalgus deformity can be unilateral in many cases and can affect the functional activities of the lower limbs in walking, mobility, and movement as well as the achievement of maximum functional independence, the extent of children’s participation in activities of daily living leads to problems. Further study and investigation of the planovalgus and its effects on the child’s physical condition and functional and movement abilities to correct the deformity, prevent the progression of the deformity, and ultimately make the lower limbs more stable when walking may lead to an increase in the child’s independence and participation in activities of daily living. Therefore, due to the limited number of studies on planovalgus deformity, its impact on the field of rehabilitation and occupational therapy-related studies, and the lack of access to a study specifically addressing this topic, this study investigates the effects of unilateral planovalgus deformity. Evidence should be presented on the components related to the balance and motor function of children with CP to determine the impact of this deformity on the cases mentioned so that it can be used professionally in the rehabilitation process. Therapists and pediatric orthopedists can benefit from the prevention of secondary musculoskeletal problems in children with cerebral palsy.
Materials and Methods
The current descriptive-analytical research was conducted on an observational basis using the convenient sampling method from September 2022 to February 2023. The inclusion criteria of the study were children with spastic CP in the age group of 8 to 14 years with level one or two of the gross motor function classification scale (GMFCS) [10، 14], diagnosis of unilateral planovalgus deformity by a neurologist and pediatric orthopedist or based on medical records, the lack of obesity (body mass index in the 85th percentile or less) [15], a lack of history of surgery and contractures of the joints of the lower extremities, and sufficient cognitive ability to participate in the study [14]. Meanwhile, the exclusion criteria were parental dissatisfaction with the conduct of the children’s assessments in the study, failure to complete the consent form, the presence of epilepsy and other neurological, psychological, and orthopedic diseases in the child based on the medical examination record and the participation of the child.
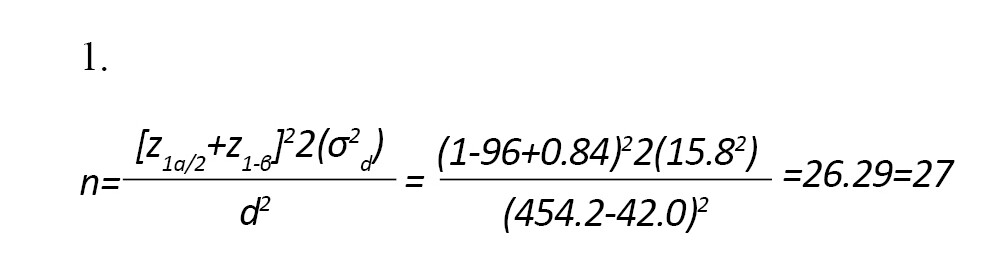
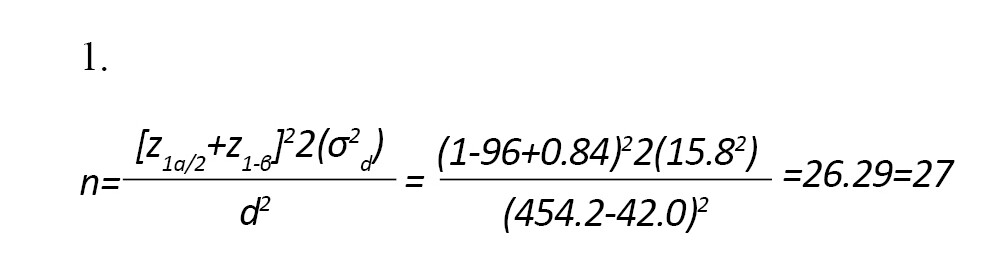
Child’s research occurred parallel to this research. After the research process and assessment method were explained in detail to the participants’ parents, written informed consent was also obtained from them. According to the article by Sung, the minimum sample size was determined from 27 people with a power of 80% and a test error of 5%, using information from similar studies according to Equation 1 [6].
After obtaining ethical approval, the study was carried out in the occupational therapy department of the Mafi system (including the medical centers of the University of Social Welfare and Rehabilitation Sciences) and occupational therapy clinics in Tehran City, Iran. In this study, 9 girls and 18 boys with CP and unilateral planovalgus deformity who could walk independently were examined in one session. Overall, the evaluations took 10 to 15 min. This study included children with CP who were at levels one and two of the gross motor function classification scale to quantify the balance and changes in the center of pressure of the soles of these children through the balance board and the single leg stance balance test. Postural stability and balance can be assessed by analyzing the time coordinate and variable center of pressure measured via the force plate [16]. During the single-leg stance balance test, the subjects were instructed to remain as still as possible on the force plate with the leg being tested [17]. The Nintendo Wii balance board was used in this evaluation, which has 4 pressure sensors with a data acquisition frequency of 100 Hz. The single leg stance balance test, which involves the patient assuming a position of standing on one leg was performed twice for both the leg unaffected by planovalgus deformity and the leg affected by planovalgus deformity, with the most favorable outcome being documented. Primary information was extracted and stored through the software written in the Unity environment and transferred to the Microsoft Excel software. Since all the patients in this study could maintain their balance for 10 s without falling and without the therapist’s help, the raw data of all the patients in the first 10 s of the evaluation were separated and processed by the MATLAB software. The data was filtered with a second-order zero-phase-shift reciprocating Butterworth low-pass filter with a cutoff frequency of 12 Hz. Finally, the center of pressure mean movement index was calculated and reported for each patient [18-22].
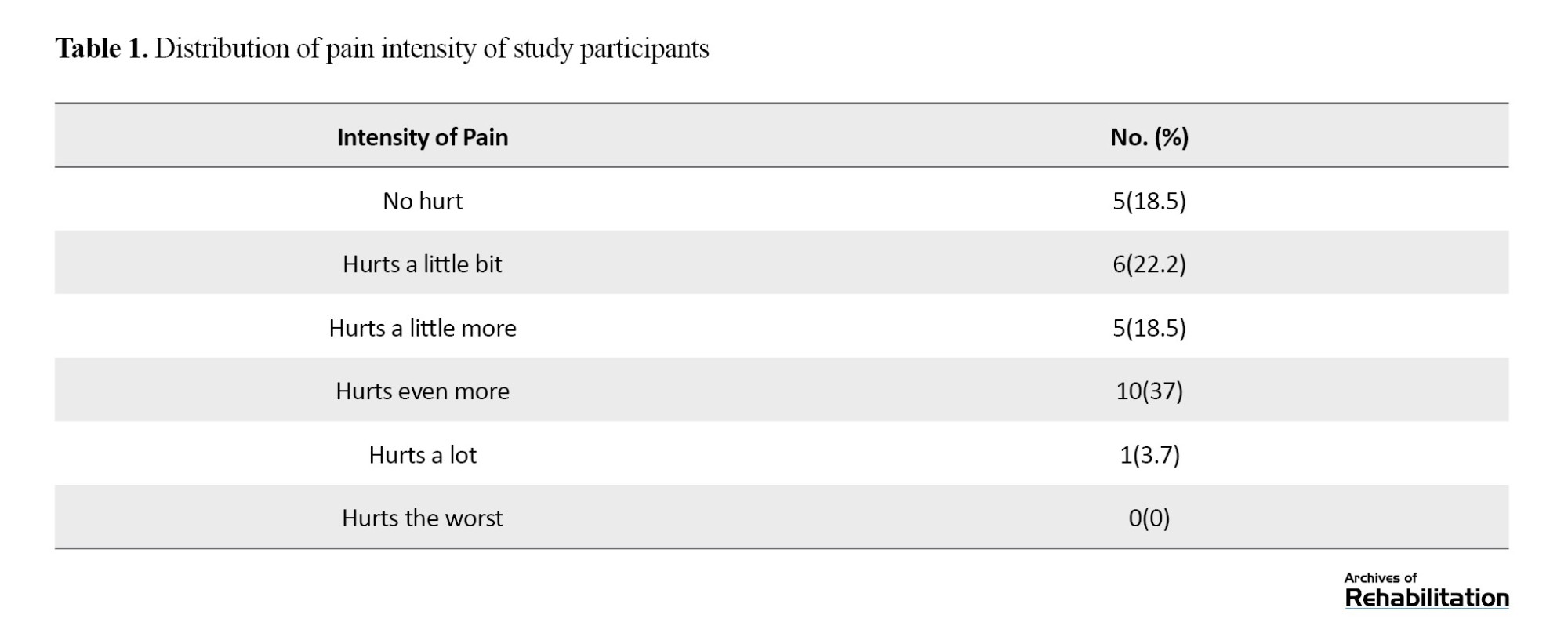
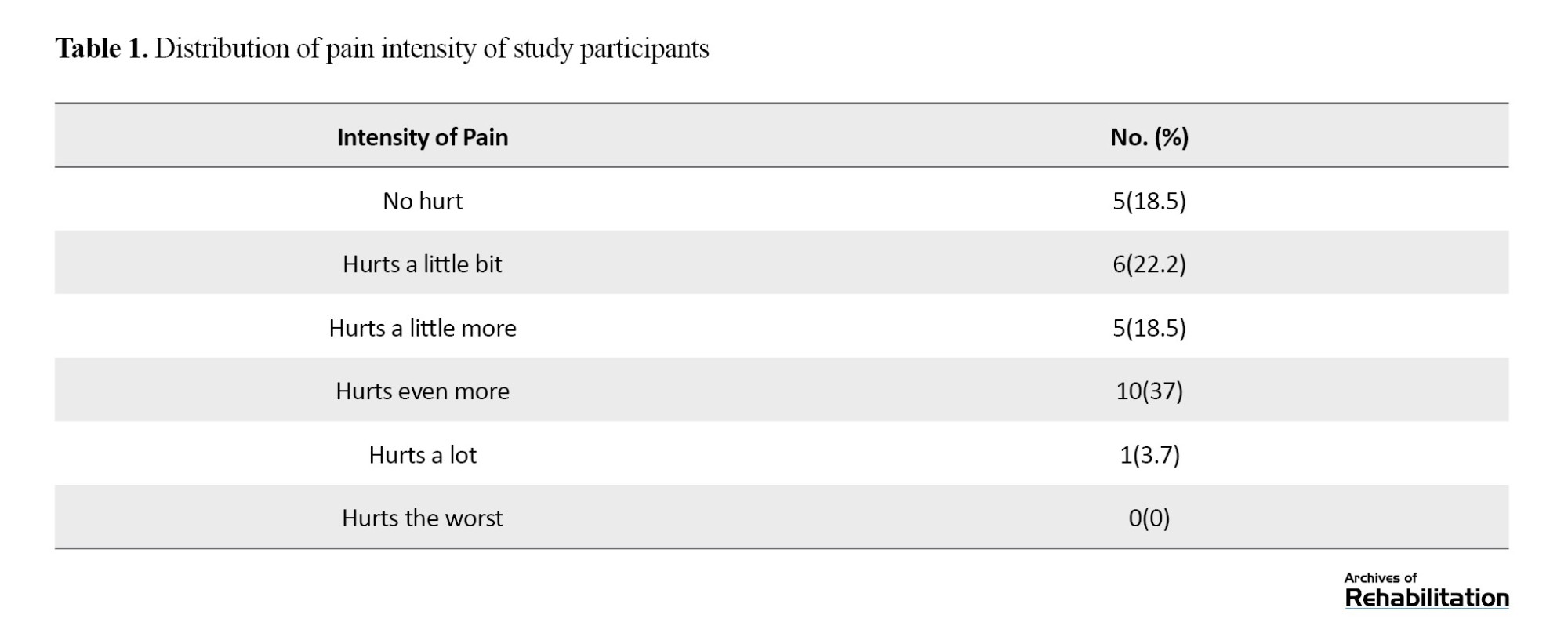
Considering that the motor function of these children depends on the strength of the muscles of the lower limbs and the range of motion of the joints, the presence of pain can appear as a disturbing factor in the performance of the motor function of the lower limbs. Therefore, in this research, the movement function of the lower limb described the strength of the muscles, the range of motion of the lower limb, and the amount of pain of the child in the involved limb [10، 23]. After a brief period of rest, the evaluation of pain was conducted using the Wong-Baker facial scale. This evaluation involved presenting a series of facial expressions on paper to the children. After providing a comprehensive explanation of this scale to the children, they were asked about the intensity of their foot discomfort throughout the day and during their daily activities. Furthermore, they were instructed to assign a numerical value to their pain experience (based on facial depictions) and rate their foot pain on a scale of 0 to 10. The data points were subsequently recorded as described [24، 25]. The results of children’s pain reports are provided in Table 1.
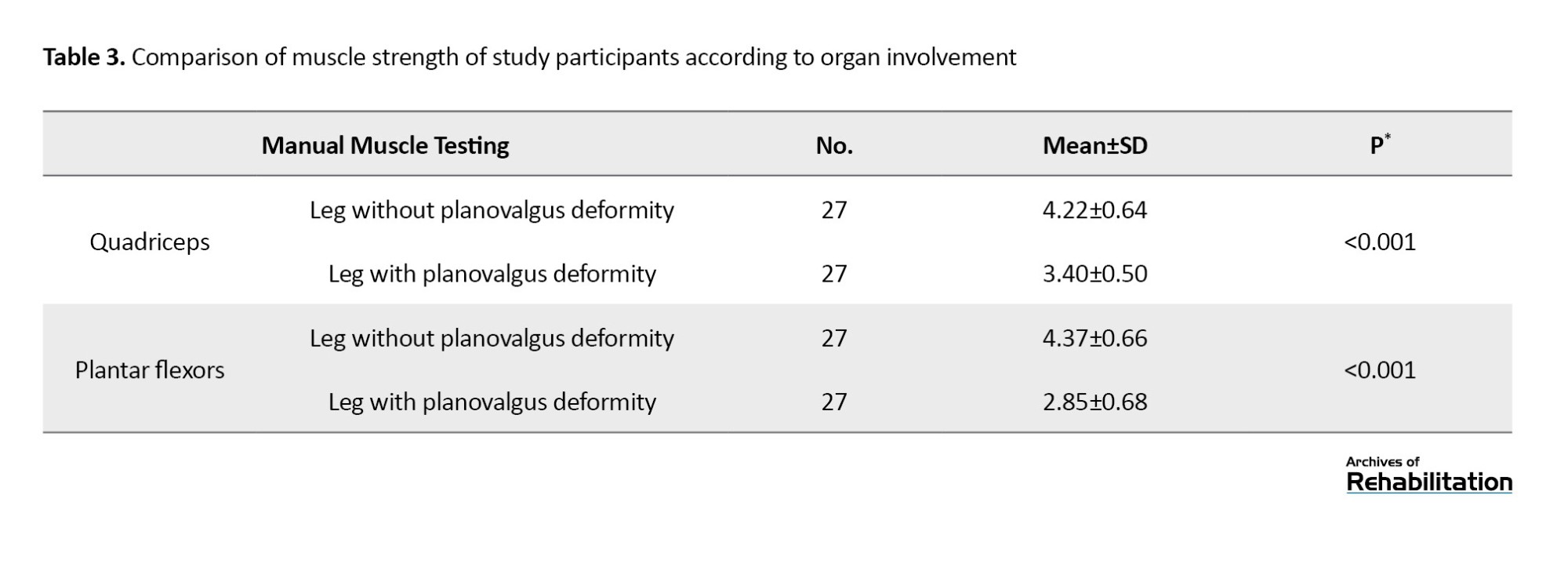
After a short period of rest, the strength of the muscles around the ankle and knee was evaluated by the occupational therapist with a manual test of the strength of the plantar flexor muscles and the quadriceps muscle and was scored from 0 to 5. A modified method of assessing plantar flexor muscle strength was applied using repeated heel raises of one foot, based on the assumption that the subject could perform this movement 25 times or more with good posture (without loss of balance and fatigue). Plantar flexor strength was considered normal regardless of age, gender, or activity level. The strength of the quadriceps muscle was also scored according to the child’s ability to sit with the knee at 90 degrees on the chair perform movement against gravity and apply manual resistance with a static isometric contraction [26، 27].
After the evaluations, the occupational therapist utilized a goniometer to measure the active range of motion of the ankle and knee joint. To measure the active range of motion, the participants were asked to move the mentioned joints in a full range of motion and at their desired speed. The range of motion of knee flexion and extension in the prone position and the range of motion of dorsiflexion and plantarflexion of the ankle while sitting on a high chair with the knee bent at 90 degrees were obtained [28]. Data analysis was done in the SPSS software, version 16.
Screening tool
The gross motor function classification system (GMFCS)
The gross motor function classification scale serves as a valuable tool for promptly assessing the level of mobility and gross motor function in individuals with CP [29]. It is one of the most reliable and well-known criteria for functional classification in children with CP and describes the performance of their gross movements in five levels. It is quick and easy to use [30]. This classification scale is reliable for use by children with CP [31]. The Persian version of this classification scale was developed and revised in 2020 by Dehghan et al. and can be used by rehabilitation and medical professionals as a stable organizational system for classifying people with CP [32] based on the modified version; accordingly, children classified at level I can walk without restrictions, and children classified at level II can walk with limitations. Limitations may include balance or stamina, use of a manual mobility device before age 4, use of handrails on stairs, or inability to run or jump, resulting in the use of wheeled mobility for long distances [30].
Measuring instruments
Single leg stance (balance evaluation test) on the force plate
The single-leg stance on the force plate assessment test is used for static posture and balance control and calculates the time spent standing on each leg and the variation in the center of pressure. This tool is considered a valuable assessment tool for demonstrating fall risk in neurological and musculoskeletal patients and can be used in children and adults [20-22]. Postural stability and balance can be evaluated by analyzing the time coordinate and variable center of pressure measured through the force plate [16].
Wong-Baker faces scale
The Wong-Baker faces scale shows a set of faces. Based on the faces and written descriptions, patients choose the face that best describes their pain level [24، 25، 33]. The validity and reliability of this scale to assess children’s pain was carried out by Alizadeh et al. in 2017 in Iran [34].
Manual muscle testing
The manual muscle testing is popular in clinical work to evaluate muscle strength and is used in many movement disorders, including cerebral palsy. Knowledge about muscle strength in children with CP is important in the treatment decision-making process, and increasing muscle strength in the lower limbs increases walking speed and improves gross motor function. This test has a total of 6 points which are graded from 0 to 5 [35، 36].
Goniometry to measure active range of motion
Goniometry is a common method for evaluating joint range of motion. By placing the fixed and movable arms of the instrument according to specific bony landmarks on both sides of the joint, the full range of joint mobility can be measured in terms of degrees. The most commonly used range of motion standards are published by the American Academy of Orthopedic Surgeons (AAOS) [37].
Results
At first, the Shapiro-Wilk test was used to check the normality of the data. The result of the test showed that the data do not have a normal distribution (P<0.05). Therefore, because the data were not normal, the Wilcoxon non-parametric test was used to compare the variables of active range of motion, muscle strength, and the mean displacement of the center of pressure of the lower limb with planovalgus deformity and without planovalgus deformity in these children.
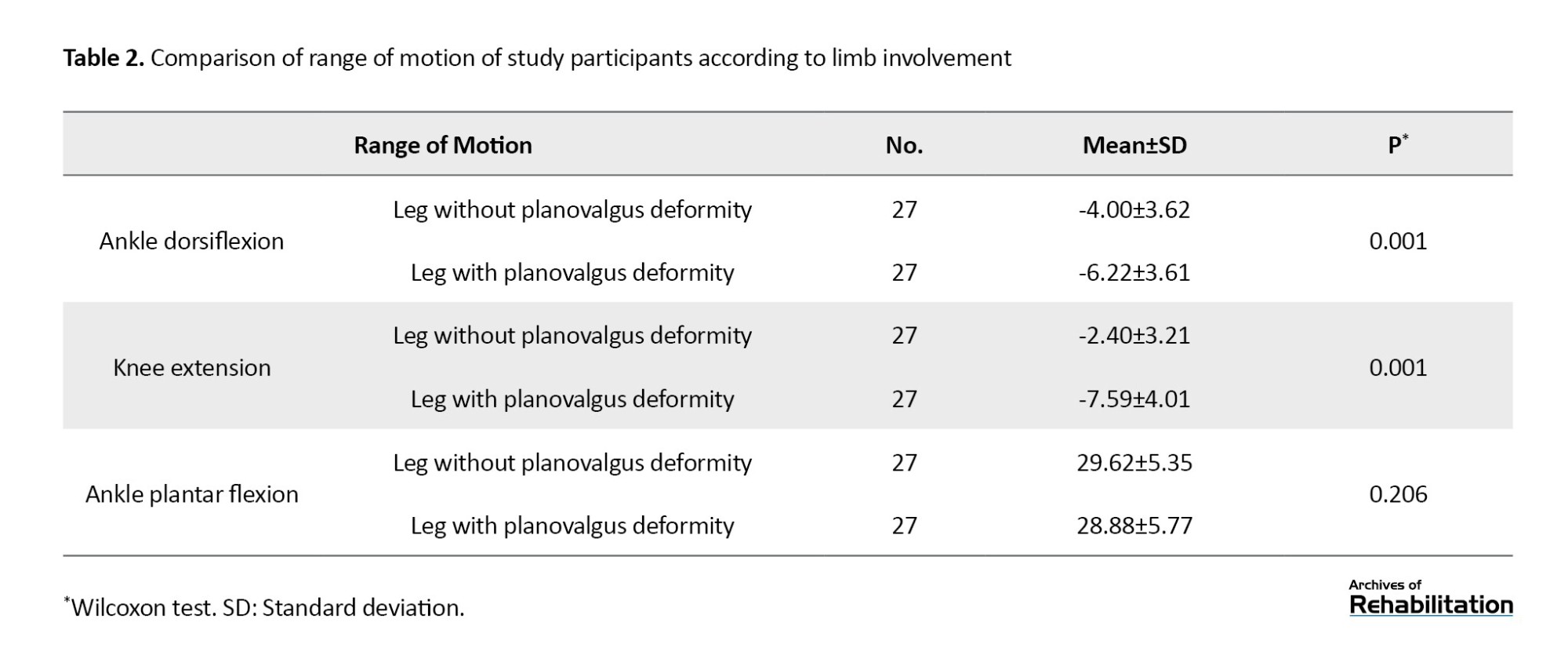
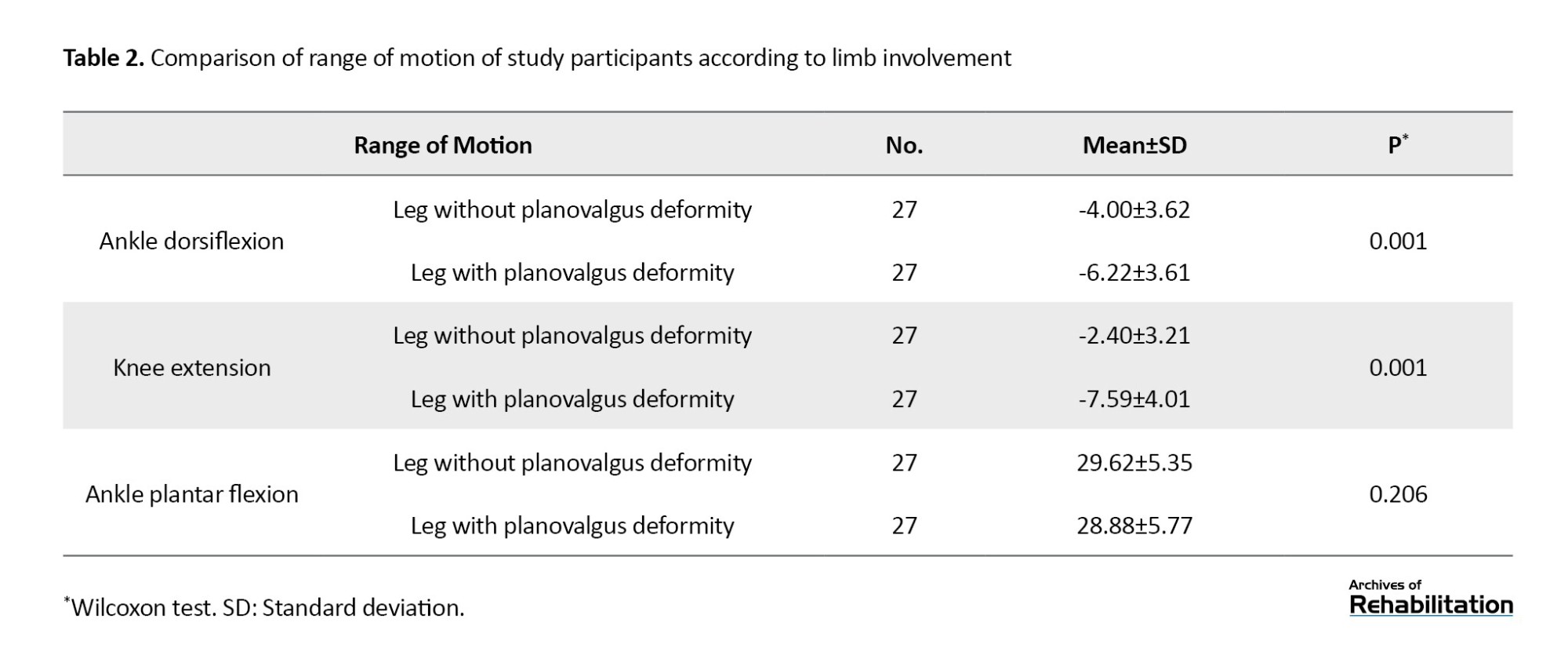
The results of this study showed a statistically significant difference between the mean range of motion of ankle dorsiflexion and knee extension between the two limbs according to the degree of limb involvement (P<0.001). By comparing the limb with and without deformity of ambulatory children with spastic cerebral palsy, planovalgus deformity has significantly reduced the range of motion of active dorsiflexion of the ankle (approximately 2 units) and reduced active extension of the knee in the involved limb. However, there is no statistically significant difference between the mean range of motion of plantar flexion in terms of organ involvement (P>0.001) (Table 2).
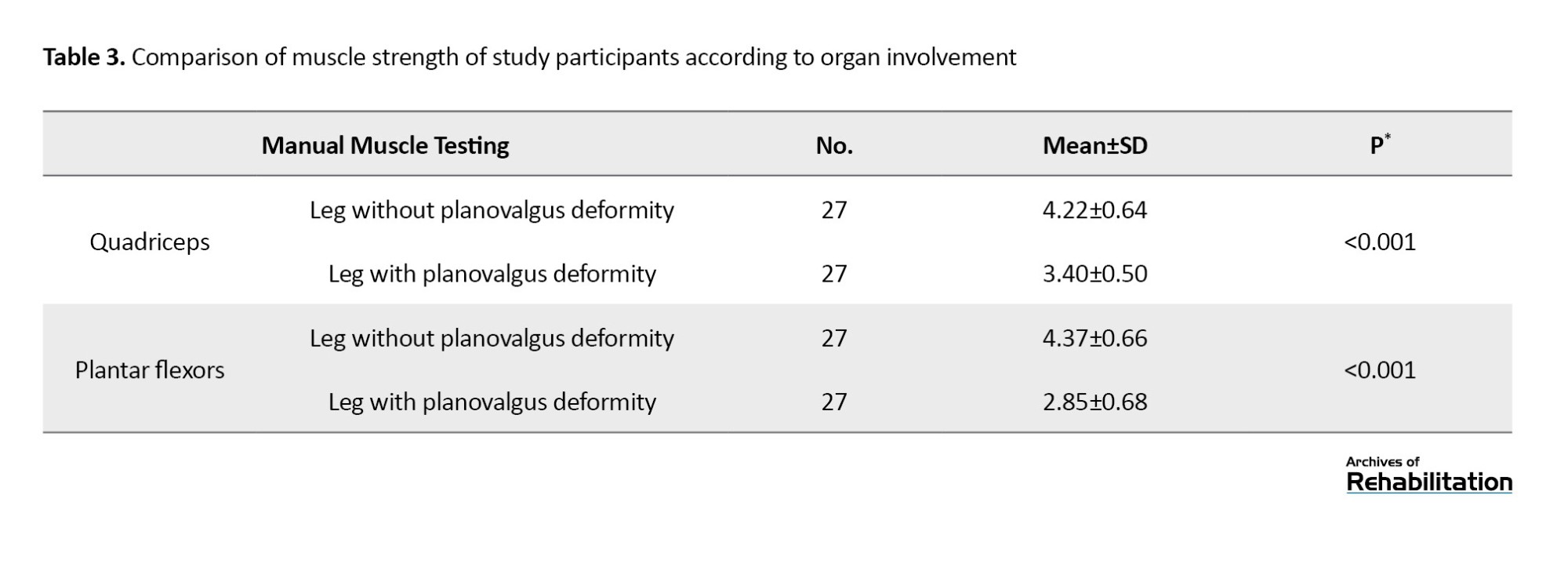
There is a statistically significant difference between the mean strength of quadriceps muscles and ankle plantar flexors of the participants in terms of organ involvement (P<0.001) and planovalgus deformity caused a decrease in the strength of quadriceps muscles and ankle plantar flexors (Table 3).
Also, there is a statistically significant difference between the displacement of the center of pressure of the participants in the study in terms of organ involvement (P<0.001) and the planovalgus deformity significantly affected the displacement of the center of pressure of the foot and caused an increase in the amount of these displacements is in the standing position on one leg (Table 4). The results of the pain report of the children of the statistical population were obtained with a Mean±SD 3.70±2.46, which indicated the feeling of musculoskeletal pain due to the presence of planovalgus deformity (Table 5).

Discussion
This analytical-descriptive study investigated the effect of unilateral planovalgus deformity on the balance and motor function of the affected lower limbs in children with spastic cerebral palsy, based on level I and II of the GMFCS. In this study, the active range of motion of the ankle and knee was measured by the therapist using a goniometer. The results are consistent with the results of studies conducted to date evaluating the range of motion of the ankle and knee joints and its relationship with planovalgus deformity. In the study by Sung et al., in the context of evaluating the difference between the actual dorsiflexion of the ankle and its relationship with the severity of the planovalgus deformity of the foot, the importance of the influence of the planovalgus deformity on the biomechanical structure of the ankle was highlighted [6]. In addition, the results of another study by Eid showed that the range of motion of knee extension in children with CP and diplegia decreases by 50% causing a decrease in stability while walking and an increase in the risk of falling and functional balance problems in children [38]. Accordingly, planovalgus deformity changes the strategy of the hip, knee, and ankle, thus hindering the proper extension of the knee, and affecting the person’s ability to extend the knee properly, which plays a major role in weight bearing [9]. However, in the study of Saraswat (2014), kinematic differences in the planovalgus foot, including excessive ankle eversion (valgus) and plantar flexion, decrease in range of motion of ankle flexion, increase in dorsiflexion and pronation of the midfoot joint were reported. Contrary to clinical expectations, no significant difference was observed in the range of motion of midfoot joint flexion or ankle eversion. Kinetic differences in legs with planovalgus deformity compared to normal growing legs included a decrease in ankle plantarflexion torque, ankle strength, and midfoot joint strength. To compensate for the decreased range of motion of the ankle joint, increased movement in the midfoot joint along with weight bearing often occurs in feet with planovalgus deformity [39]. It is suggested that future studies examine the evidence and magnitude of the impact of planovalgus deformity on hip and spinal joint range of motion in the community of children with CP and planovalgus deformity.
According to the international classification of functioning, disability, and health (ICF), progress in therapeutic interventions that focus on defects, such as increasing muscle strength and range of motion, improve the individual’s activity and participation [40]. In the present study, the muscle strength variable was measured. In the study results of Ganjwala et al. [41], Masaki et al. [42], and the study results of Saraswat et al. [39], a high rate of planovalgus is evident due to the decrease in muscle strength of the knee extensors and soleus muscle associated with plantar flexion performance. In both studies, lower extremity muscle strength decreased in the closed-chain [9]. Hence, changes in the planovalgus in the foot cause biomechanical disturbances, such as the strength and function of the plantar flexors and knee extensors. According to the results of the present study, the strength of the knee extensor and plantar flexor muscles decreased in the leg with planovalgus deformity compared to the leg without deformity. From the beginning of the diagnosis of planovalgus deformity in a child with CP and the ability to walk, it is recommended to pay special attention to the strength of the quadriceps and plantar flexor muscles and to take the necessary measures to strengthen these muscles.
The results of the assessment of balance functions using the Nintendo® Wii fit force plate indicate a significant shift in the center of pressure and an increase in these shifts when standing on one leg compared to the other leg as a result of planovalgus deformity in the affected limb. These results are consistent with the findings of the studies conducted to date to examine the effect of using the Nintendo® Wii fit force plate as a safe, enjoyable, appropriate, and effective method of improving balance indicators in CP patients, which should be added to conventional treatments to improve the balance of these patients [43]. The results of Tang’s study in 2022 also showed a change in foot loading after the progression of CP [44]. These findings are also consistent with the results of the present study. Therefore, preventive interventions for planovalgus deformities can potentially effectively prevent the exacerbation of foot deformities and ultimately lead to timely clinical decision support and play an effective role in facilitating the participation and performance of children with CP in school and society. However, further studies are needed in this field.
The results of pain assessment in children participating in this study are consistent with the results of many studies examining interventions in children with planovalgus deformity. Pain is considered one of the most important factors for children. Because the complications caused by this factor reduce the ability of these children to walk independently and lead to incorrect patterns in the child’s walking process and performance [10، 23]. Therefore, an accurate and correct diagnostic examination of pain in children with planovalgus is critical [45]. Meanwhile, the use of therapeutic assessment tools to better describe pain in clients with planovalgus deformity may be an appropriate guide for experts in the field to select a treatment protocol.
Planovalgus has generated the most debate among pediatric orthopedists due to the high prevalence of this deformity and the increase in alternative treatment methods, the benefits and superiority of which are no longer clear [3]. The current treatment framework for planovalgus deformity should take into account the child’s age and motor performance, as planovalgus deformity occurs in most cases by mid-childhood and worsens over time and entering adolescence [10]. Based on the researcher’s observations during the assessments in the therapeutic environment and the subsequent analysis of the information, the motivation of the therapists and parents of the participants to receive information about the problems after a deformity and how to cope with them was much higher to prevent later problems, such as impairment of the child’s balance skills, which can be caused by impairment of the ankle muscles and joints, including the dorsiflexion and knee extensors. Preventive measures of occupational therapy should be considered regarding the functional abilities and daily activities of these children, and take into account the child’s movement ability, play, academic performance, and participation with peers in society, because if these children are neglected, they may suffer from problems, that prevent them from actively participating in school. Therefore, it is proposed to more comprehensively examine the impact of planovalgus deformity on the balance and motor performance of children with spastic CP with the ability to walk independently and the importance of effective strategies to prevent or minimize injuries associated with planovalgus deformity to examine intervention research more comprehensively.
Conclusion
The results of this study showed that balance and motor function in children with CP can be affected by planovalgus deformity. Changes lead to a decrease in the range of motion of the knee and ankle joints, a decrease in the strength of the muscles of the lower extremities, and an increasing displacement of the plantar pressure center in the affected lower extremity, resulting in pain in children with spastic CP in the ability to walk has been observed. Therefore, non-surgical treatment of these children is warranted, although individualized treatment is recommended in the rehabilitation of these children. At the same time, the results of this study are important for expanding the use of Wii fit in the rehabilitation of CP in terms of assessing the functional balance of these children in our country and providing an appropriate perspective for therapists working in this field.
Study limitations
The limitations of the present study include the lack of gender distribution of study participants and the inability to generalize the results to deformities in adolescents and concurrent deformities in higher joints (knee-thigh and spine).
Ethical Considerations
Compliance with ethical guidelines
The current research was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1401.109). The principle of scientific integrity and the recording of the results of the participant evaluations were recorded without any problems. When collecting data and checking the available sources, attention was paid to the greatest possible trustworthiness and honesty. The participants were informed about the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information. They were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, data validation, review, editing and final approval: Saeid Fatorehchy and Mahsa A’rabi; Data analysis: Enayatollah Bakhshil; Investigation: Saeid Fatorehchy, Mahsa A’rabi, and Seyedmostafa Alavian; Initial draft preparation: Mahsa A’rabi and Seyedmostafa Alavian; Visualization and monitoring: Seyed Ali Hosseini.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Hamidreza Soleimani (occupational therapist) who sincerely gave his time to the research team.
Cerebral palsy (CP) is a group of permanent movement and posture disorders that lead to limitations in the performance of activities and occur as a result of non-progressive disorders in the developing brain of a fetus or infant [1]. Brain damage in these children leads to abnormal muscle activity, impaired weight bearing, and limited movement due to muscle shortening, which in turn leads to secondary musculoskeletal and movement problems [2]. One of the most important functional mobility deformities whose treatment is still debated is the planovalgus deformity in children with bilateral spastic CP as one of the most common deformities [3، 4] associated with shortening of the Achilles tendon of the lower limbs and causes pain or other symptoms with increased activity and increased body mass index. These symptoms become more noticeable after the age of 10 years and can last into adulthood, leaving people unable to walk [5]. As a common deformity of the foot, the characteristics of planovalgus include hind foot valgus, midfoot pronation, decreased medial longitudinal arch, and forefoot abduction/supination [6، 7]. Although the primary cause of planovalgus deformity is still unknown, people with this deformity frequently experience pain, functional impairment, and lower limb contracture [7]. According to a 2016 study on CP aimed at improving walking in children with this disorder, the maturation of balance skills in these children was also delayed or reduced compared to typically developing children. Over time, these defects lead to problems in balance and foot center of pressure. Therefore, balance and walking disorders, including asymmetry in the lower limbs, are some of the complications of this phenomenon, which can lead to further dysfunction in ambulatory children with CP [8]. Optimum walking performance comes from using the ground reaction force. Meanwhile, the optimal use of this force requires the proper performance of the ankle’s plantar flexors [9]. According to Miller’s study in 2022, a planovalgus deformity impairs plantar flexor function and ground reaction force by causing structural changes in the foot and ankle. This study shows that the performance level of gross movements of these children alone is the most important factor influencing the progress of radiological indicators in the treatment of planovalgus deformities [10]. The results of research conducted in the field of planovalgus deformity show that early detection of planovalgus deformity is essential to prevent aggravation of leg injuries [11].
Ambulatory children with CP who are referred to medical centers and have planovalgus deformity in the ankles typically use the crutch walking pattern that is most common in these children. Due to spasticity, muscle contractions, and limitation of movement of the joints of the lower limbs, there is a loss of functional capabilities in these children [12]. Although this deformity is known to persist into adulthood, little information has been published regarding the natural history and treatment of planovalgus. Furthermore, there is no clarity regarding the need for non-surgical or surgical treatment [13]. Since the presence of planovalgus deformity can be unilateral in many cases and can affect the functional activities of the lower limbs in walking, mobility, and movement as well as the achievement of maximum functional independence, the extent of children’s participation in activities of daily living leads to problems. Further study and investigation of the planovalgus and its effects on the child’s physical condition and functional and movement abilities to correct the deformity, prevent the progression of the deformity, and ultimately make the lower limbs more stable when walking may lead to an increase in the child’s independence and participation in activities of daily living. Therefore, due to the limited number of studies on planovalgus deformity, its impact on the field of rehabilitation and occupational therapy-related studies, and the lack of access to a study specifically addressing this topic, this study investigates the effects of unilateral planovalgus deformity. Evidence should be presented on the components related to the balance and motor function of children with CP to determine the impact of this deformity on the cases mentioned so that it can be used professionally in the rehabilitation process. Therapists and pediatric orthopedists can benefit from the prevention of secondary musculoskeletal problems in children with cerebral palsy.
Materials and Methods
The current descriptive-analytical research was conducted on an observational basis using the convenient sampling method from September 2022 to February 2023. The inclusion criteria of the study were children with spastic CP in the age group of 8 to 14 years with level one or two of the gross motor function classification scale (GMFCS) [10، 14], diagnosis of unilateral planovalgus deformity by a neurologist and pediatric orthopedist or based on medical records, the lack of obesity (body mass index in the 85th percentile or less) [15], a lack of history of surgery and contractures of the joints of the lower extremities, and sufficient cognitive ability to participate in the study [14]. Meanwhile, the exclusion criteria were parental dissatisfaction with the conduct of the children’s assessments in the study, failure to complete the consent form, the presence of epilepsy and other neurological, psychological, and orthopedic diseases in the child based on the medical examination record and the participation of the child.
Child’s research occurred parallel to this research. After the research process and assessment method were explained in detail to the participants’ parents, written informed consent was also obtained from them. According to the article by Sung, the minimum sample size was determined from 27 people with a power of 80% and a test error of 5%, using information from similar studies according to Equation 1 [6].
After obtaining ethical approval, the study was carried out in the occupational therapy department of the Mafi system (including the medical centers of the University of Social Welfare and Rehabilitation Sciences) and occupational therapy clinics in Tehran City, Iran. In this study, 9 girls and 18 boys with CP and unilateral planovalgus deformity who could walk independently were examined in one session. Overall, the evaluations took 10 to 15 min. This study included children with CP who were at levels one and two of the gross motor function classification scale to quantify the balance and changes in the center of pressure of the soles of these children through the balance board and the single leg stance balance test. Postural stability and balance can be assessed by analyzing the time coordinate and variable center of pressure measured via the force plate [16]. During the single-leg stance balance test, the subjects were instructed to remain as still as possible on the force plate with the leg being tested [17]. The Nintendo Wii balance board was used in this evaluation, which has 4 pressure sensors with a data acquisition frequency of 100 Hz. The single leg stance balance test, which involves the patient assuming a position of standing on one leg was performed twice for both the leg unaffected by planovalgus deformity and the leg affected by planovalgus deformity, with the most favorable outcome being documented. Primary information was extracted and stored through the software written in the Unity environment and transferred to the Microsoft Excel software. Since all the patients in this study could maintain their balance for 10 s without falling and without the therapist’s help, the raw data of all the patients in the first 10 s of the evaluation were separated and processed by the MATLAB software. The data was filtered with a second-order zero-phase-shift reciprocating Butterworth low-pass filter with a cutoff frequency of 12 Hz. Finally, the center of pressure mean movement index was calculated and reported for each patient [18-22].
Considering that the motor function of these children depends on the strength of the muscles of the lower limbs and the range of motion of the joints, the presence of pain can appear as a disturbing factor in the performance of the motor function of the lower limbs. Therefore, in this research, the movement function of the lower limb described the strength of the muscles, the range of motion of the lower limb, and the amount of pain of the child in the involved limb [10، 23]. After a brief period of rest, the evaluation of pain was conducted using the Wong-Baker facial scale. This evaluation involved presenting a series of facial expressions on paper to the children. After providing a comprehensive explanation of this scale to the children, they were asked about the intensity of their foot discomfort throughout the day and during their daily activities. Furthermore, they were instructed to assign a numerical value to their pain experience (based on facial depictions) and rate their foot pain on a scale of 0 to 10. The data points were subsequently recorded as described [24، 25]. The results of children’s pain reports are provided in Table 1.
After a short period of rest, the strength of the muscles around the ankle and knee was evaluated by the occupational therapist with a manual test of the strength of the plantar flexor muscles and the quadriceps muscle and was scored from 0 to 5. A modified method of assessing plantar flexor muscle strength was applied using repeated heel raises of one foot, based on the assumption that the subject could perform this movement 25 times or more with good posture (without loss of balance and fatigue). Plantar flexor strength was considered normal regardless of age, gender, or activity level. The strength of the quadriceps muscle was also scored according to the child’s ability to sit with the knee at 90 degrees on the chair perform movement against gravity and apply manual resistance with a static isometric contraction [26، 27].
After the evaluations, the occupational therapist utilized a goniometer to measure the active range of motion of the ankle and knee joint. To measure the active range of motion, the participants were asked to move the mentioned joints in a full range of motion and at their desired speed. The range of motion of knee flexion and extension in the prone position and the range of motion of dorsiflexion and plantarflexion of the ankle while sitting on a high chair with the knee bent at 90 degrees were obtained [28]. Data analysis was done in the SPSS software, version 16.
Screening tool
The gross motor function classification system (GMFCS)
The gross motor function classification scale serves as a valuable tool for promptly assessing the level of mobility and gross motor function in individuals with CP [29]. It is one of the most reliable and well-known criteria for functional classification in children with CP and describes the performance of their gross movements in five levels. It is quick and easy to use [30]. This classification scale is reliable for use by children with CP [31]. The Persian version of this classification scale was developed and revised in 2020 by Dehghan et al. and can be used by rehabilitation and medical professionals as a stable organizational system for classifying people with CP [32] based on the modified version; accordingly, children classified at level I can walk without restrictions, and children classified at level II can walk with limitations. Limitations may include balance or stamina, use of a manual mobility device before age 4, use of handrails on stairs, or inability to run or jump, resulting in the use of wheeled mobility for long distances [30].
Measuring instruments
Single leg stance (balance evaluation test) on the force plate
The single-leg stance on the force plate assessment test is used for static posture and balance control and calculates the time spent standing on each leg and the variation in the center of pressure. This tool is considered a valuable assessment tool for demonstrating fall risk in neurological and musculoskeletal patients and can be used in children and adults [20-22]. Postural stability and balance can be evaluated by analyzing the time coordinate and variable center of pressure measured through the force plate [16].
Wong-Baker faces scale
The Wong-Baker faces scale shows a set of faces. Based on the faces and written descriptions, patients choose the face that best describes their pain level [24، 25، 33]. The validity and reliability of this scale to assess children’s pain was carried out by Alizadeh et al. in 2017 in Iran [34].
Manual muscle testing
The manual muscle testing is popular in clinical work to evaluate muscle strength and is used in many movement disorders, including cerebral palsy. Knowledge about muscle strength in children with CP is important in the treatment decision-making process, and increasing muscle strength in the lower limbs increases walking speed and improves gross motor function. This test has a total of 6 points which are graded from 0 to 5 [35، 36].
Goniometry to measure active range of motion
Goniometry is a common method for evaluating joint range of motion. By placing the fixed and movable arms of the instrument according to specific bony landmarks on both sides of the joint, the full range of joint mobility can be measured in terms of degrees. The most commonly used range of motion standards are published by the American Academy of Orthopedic Surgeons (AAOS) [37].
Results
At first, the Shapiro-Wilk test was used to check the normality of the data. The result of the test showed that the data do not have a normal distribution (P<0.05). Therefore, because the data were not normal, the Wilcoxon non-parametric test was used to compare the variables of active range of motion, muscle strength, and the mean displacement of the center of pressure of the lower limb with planovalgus deformity and without planovalgus deformity in these children.
The results of this study showed a statistically significant difference between the mean range of motion of ankle dorsiflexion and knee extension between the two limbs according to the degree of limb involvement (P<0.001). By comparing the limb with and without deformity of ambulatory children with spastic cerebral palsy, planovalgus deformity has significantly reduced the range of motion of active dorsiflexion of the ankle (approximately 2 units) and reduced active extension of the knee in the involved limb. However, there is no statistically significant difference between the mean range of motion of plantar flexion in terms of organ involvement (P>0.001) (Table 2).
There is a statistically significant difference between the mean strength of quadriceps muscles and ankle plantar flexors of the participants in terms of organ involvement (P<0.001) and planovalgus deformity caused a decrease in the strength of quadriceps muscles and ankle plantar flexors (Table 3).
Also, there is a statistically significant difference between the displacement of the center of pressure of the participants in the study in terms of organ involvement (P<0.001) and the planovalgus deformity significantly affected the displacement of the center of pressure of the foot and caused an increase in the amount of these displacements is in the standing position on one leg (Table 4). The results of the pain report of the children of the statistical population were obtained with a Mean±SD 3.70±2.46, which indicated the feeling of musculoskeletal pain due to the presence of planovalgus deformity (Table 5).

Discussion
This analytical-descriptive study investigated the effect of unilateral planovalgus deformity on the balance and motor function of the affected lower limbs in children with spastic cerebral palsy, based on level I and II of the GMFCS. In this study, the active range of motion of the ankle and knee was measured by the therapist using a goniometer. The results are consistent with the results of studies conducted to date evaluating the range of motion of the ankle and knee joints and its relationship with planovalgus deformity. In the study by Sung et al., in the context of evaluating the difference between the actual dorsiflexion of the ankle and its relationship with the severity of the planovalgus deformity of the foot, the importance of the influence of the planovalgus deformity on the biomechanical structure of the ankle was highlighted [6]. In addition, the results of another study by Eid showed that the range of motion of knee extension in children with CP and diplegia decreases by 50% causing a decrease in stability while walking and an increase in the risk of falling and functional balance problems in children [38]. Accordingly, planovalgus deformity changes the strategy of the hip, knee, and ankle, thus hindering the proper extension of the knee, and affecting the person’s ability to extend the knee properly, which plays a major role in weight bearing [9]. However, in the study of Saraswat (2014), kinematic differences in the planovalgus foot, including excessive ankle eversion (valgus) and plantar flexion, decrease in range of motion of ankle flexion, increase in dorsiflexion and pronation of the midfoot joint were reported. Contrary to clinical expectations, no significant difference was observed in the range of motion of midfoot joint flexion or ankle eversion. Kinetic differences in legs with planovalgus deformity compared to normal growing legs included a decrease in ankle plantarflexion torque, ankle strength, and midfoot joint strength. To compensate for the decreased range of motion of the ankle joint, increased movement in the midfoot joint along with weight bearing often occurs in feet with planovalgus deformity [39]. It is suggested that future studies examine the evidence and magnitude of the impact of planovalgus deformity on hip and spinal joint range of motion in the community of children with CP and planovalgus deformity.
According to the international classification of functioning, disability, and health (ICF), progress in therapeutic interventions that focus on defects, such as increasing muscle strength and range of motion, improve the individual’s activity and participation [40]. In the present study, the muscle strength variable was measured. In the study results of Ganjwala et al. [41], Masaki et al. [42], and the study results of Saraswat et al. [39], a high rate of planovalgus is evident due to the decrease in muscle strength of the knee extensors and soleus muscle associated with plantar flexion performance. In both studies, lower extremity muscle strength decreased in the closed-chain [9]. Hence, changes in the planovalgus in the foot cause biomechanical disturbances, such as the strength and function of the plantar flexors and knee extensors. According to the results of the present study, the strength of the knee extensor and plantar flexor muscles decreased in the leg with planovalgus deformity compared to the leg without deformity. From the beginning of the diagnosis of planovalgus deformity in a child with CP and the ability to walk, it is recommended to pay special attention to the strength of the quadriceps and plantar flexor muscles and to take the necessary measures to strengthen these muscles.
The results of the assessment of balance functions using the Nintendo® Wii fit force plate indicate a significant shift in the center of pressure and an increase in these shifts when standing on one leg compared to the other leg as a result of planovalgus deformity in the affected limb. These results are consistent with the findings of the studies conducted to date to examine the effect of using the Nintendo® Wii fit force plate as a safe, enjoyable, appropriate, and effective method of improving balance indicators in CP patients, which should be added to conventional treatments to improve the balance of these patients [43]. The results of Tang’s study in 2022 also showed a change in foot loading after the progression of CP [44]. These findings are also consistent with the results of the present study. Therefore, preventive interventions for planovalgus deformities can potentially effectively prevent the exacerbation of foot deformities and ultimately lead to timely clinical decision support and play an effective role in facilitating the participation and performance of children with CP in school and society. However, further studies are needed in this field.
The results of pain assessment in children participating in this study are consistent with the results of many studies examining interventions in children with planovalgus deformity. Pain is considered one of the most important factors for children. Because the complications caused by this factor reduce the ability of these children to walk independently and lead to incorrect patterns in the child’s walking process and performance [10، 23]. Therefore, an accurate and correct diagnostic examination of pain in children with planovalgus is critical [45]. Meanwhile, the use of therapeutic assessment tools to better describe pain in clients with planovalgus deformity may be an appropriate guide for experts in the field to select a treatment protocol.
Planovalgus has generated the most debate among pediatric orthopedists due to the high prevalence of this deformity and the increase in alternative treatment methods, the benefits and superiority of which are no longer clear [3]. The current treatment framework for planovalgus deformity should take into account the child’s age and motor performance, as planovalgus deformity occurs in most cases by mid-childhood and worsens over time and entering adolescence [10]. Based on the researcher’s observations during the assessments in the therapeutic environment and the subsequent analysis of the information, the motivation of the therapists and parents of the participants to receive information about the problems after a deformity and how to cope with them was much higher to prevent later problems, such as impairment of the child’s balance skills, which can be caused by impairment of the ankle muscles and joints, including the dorsiflexion and knee extensors. Preventive measures of occupational therapy should be considered regarding the functional abilities and daily activities of these children, and take into account the child’s movement ability, play, academic performance, and participation with peers in society, because if these children are neglected, they may suffer from problems, that prevent them from actively participating in school. Therefore, it is proposed to more comprehensively examine the impact of planovalgus deformity on the balance and motor performance of children with spastic CP with the ability to walk independently and the importance of effective strategies to prevent or minimize injuries associated with planovalgus deformity to examine intervention research more comprehensively.
Conclusion
The results of this study showed that balance and motor function in children with CP can be affected by planovalgus deformity. Changes lead to a decrease in the range of motion of the knee and ankle joints, a decrease in the strength of the muscles of the lower extremities, and an increasing displacement of the plantar pressure center in the affected lower extremity, resulting in pain in children with spastic CP in the ability to walk has been observed. Therefore, non-surgical treatment of these children is warranted, although individualized treatment is recommended in the rehabilitation of these children. At the same time, the results of this study are important for expanding the use of Wii fit in the rehabilitation of CP in terms of assessing the functional balance of these children in our country and providing an appropriate perspective for therapists working in this field.
Study limitations
The limitations of the present study include the lack of gender distribution of study participants and the inability to generalize the results to deformities in adolescents and concurrent deformities in higher joints (knee-thigh and spine).
Ethical Considerations
Compliance with ethical guidelines
The current research was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1401.109). The principle of scientific integrity and the recording of the results of the participant evaluations were recorded without any problems. When collecting data and checking the available sources, attention was paid to the greatest possible trustworthiness and honesty. The participants were informed about the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information. They were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, data validation, review, editing and final approval: Saeid Fatorehchy and Mahsa A’rabi; Data analysis: Enayatollah Bakhshil; Investigation: Saeid Fatorehchy, Mahsa A’rabi, and Seyedmostafa Alavian; Initial draft preparation: Mahsa A’rabi and Seyedmostafa Alavian; Visualization and monitoring: Seyed Ali Hosseini.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Hamidreza Soleimani (occupational therapist) who sincerely gave his time to the research team.
References
- te Velde A, Morgan C, Novak I, Tantsis E, Badawi N. Early diagnosis and classification of cerebral palsy: An historical perspective and barriers to an early diagnosis. Journal of Clinical Medicine. 2019; 8(10):1599. [DOI:10.3390/jcm8101599] [PMID] [PMCID]
- Song S, Lee K, Jung S, Park S, Cho H, Lee G. Effect of horizontal whole-body vibration training on trunk and lower-extremity muscle tone and activation, balance, and gait in a child with cerebral palsy. The American Journal of Case Reports. 2018; 19:1292-300. [DOI:10.12659/AJCR.910468] [PMID] [PMCID]
- Sees JP, Miller F. Overview of foot deformity management in children with cerebral palsy. Journal of Children's Orthopaedics. 2013; 7(5):373-7. [DOI:10.1007/s11832-013-0509-4] [PMID] [PMCID]
- Raposo MR, Ricardo D, Teles J, Veloso AP, João F. Gait analysis in children with cerebral palsy: Are plantar pressure insoles a reliable tool? Sensors. 2022; 22(14):5234. [DOI:10.3390/s22145234] [PMID] [PMCID]
- Kim HY, Shin HS, Ko JH, Cha YH, Ahn JH, Hwang JY. Gait analysis of symptomatic flatfoot in children: An observational study. Clinics in Orthopedic Surgery. 2017; 9(3):363-73. [DOI:10.4055/cios.2017.9.3.363] [PMID] [PMCID]
- Sung KH, Chung CY, Lee KM, Kwon KB, Lee JH, Park MS. Discrepancy between true ankle dorsiflexion and gait kinematics and its association with severity of planovalgus foot deformity. BMc Musculoskeletal Disorders. 2020; 21(1):250. [DOI:10.1186/s12891-020-03285-3] [PMID] [PMCID]
- Kim NT, Lee YT, Park MS, Lee KM, Kwon OS, Sung KH. Changes in the bony alignment of the foot after tendo-Achilles lengthening in patients with planovalgus deformity. Journal of Orthopaedic Surgery and Research. 2021; 16(1):118. [DOI:10.1186/s13018-021-02272-1] [PMID] [PMCID]
- Rumberg F, Bakir MS, Taylor WR, Haberl H, Sarpong A, Sharankou I, et al. The effects of selective dorsal rhizotomy on balance and symmetry of gait in children with cerebral palsy. Plos One. 2016; 11(4):e0152930. [DOI:10.1371/journal.pone.0152930] [PMID] [PMCID]
- Levangie PK, Norkin CC. Joint structure and function: A comprehensive analysis. Philadelphia: F.A. Davis; 2011. [Link]
- Miller F Planovalgus foot deformity in cerebral palsy. Berlin: Springer; 2020. [DOI:10.1007/978-3-319-74558-9_144]
- Lashkouski U, Ihnatouski M, Pauk J, Daunoraviciene K. Correction of planovalgus deformity through rotational reinsertion of the lateral layers of the achilles tendons in ambulatory children with cerebral palsy. The Journal of Foot and Ankle Surgery. 2019; 58(3):528-33. [DOI:10.1053/j.jfas.2018.11.001] [PMID]
- Kadhim M, Miller F. Crouch gait changes after planovalgus foot deformity correction in ambulatory children with cerebral palsy. Gait & Posture. 2014; 39(2):793-8. [DOI:10.1016/j.gaitpost.2013.10.020] [PMID]
- Galán-Olleros M, Ramírez-Barragán A, Rodríguez-Zamorano P, Egea-Gámez RM, Serrano JI, Martínez-Caballero I. Long-term impact of planovalgus foot on activities of daily living in patients with down syndrome. Journal of Pediatric Orthopedics. 2023; 43(4):259-267. [DOI:10.1097/BPO.0000000000002354] [PMID]
- Gatica-Rojas V, Cartes-Velásquez R, Guzmán-Muñoz E, Méndez-Rebolledo G, Soto-Poblete A, Pacheco-Espinoza AC, et al. Effectiveness of a nintendo wii balance board exercise programme on standing balance of children with cerebral palsy: A randomised clinical trial protocol. Contemporary Clinical Trials Communications. 2017; 6:17-21. [DOI:10.1016/j.conctc.2017.02.008] [PMID] [PMCID]
- Kumar S, Kelly AS. Review of childhood obesity: From epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clinic Proceedings. 2017; 92(2):251-65. [DOI:10.1016/j.mayocp.2016.09.017] [PMID]
- Karlsson A, Frykberg G. Correlations between force plate measures for assessment of balance. Clinical Biomechanics. 2000; 15(5):365-9. [DOI:10.1016/S0268-0033(99)00096-0] [PMID]
- Ross SE, Guskiewicz KM, Gross MT, Yu B. Balance measures for discriminating between functionally unstable and stable ankles. Medicine and Science in Sports and Exercices. 2009; 41(2):399-407. [DOI:10.1249/MSS.0b013e3181872d89] [PMID]
- Clark RA, Bryant AL, Pua Y, McCrory P, Bennell K, Hunt M. Validity and reliability of the nintendo wii balance board for assessment of standing balance. Gait & Posture. 2010; 31(3):307-10. [DOI:10.1016/j.gaitpost.2009.11.012] [PMID]
- Bonnechère B, Jansen B, Omelina L, Sholukha V, Van Sint Jan S. Validation of the balance board for clinical evaluation of balance during serious gaming rehabilitation exercises. Telemedicine Journal and E-Health. 2016; 22(9):709-17. [DOI:10.1089/tmj.2015.0230] [PMID]
- Zhang C, Talaber A, Truong M, Vargas BB. K-D balance: An objective measure of balance in tandem and double leg stances. Digital Health. 2019; 5:2055207619885573. [DOI:10.1177/2055207619885573] [PMID] [PMCID]
- Hunt MA, McManus FJ, Hinman RS, Bennell KL. Predictors of single-leg standing balance in individuals with medial knee osteoarthritis. Arthritis Care & Research. 2010; 62(4):496-500. [DOI:10.1002/acr.20046] [PMID]
- Bonora G, Mancini M, Carpinella I, Chiari L, Ferrarin M, Nutt JG, et al. Investigation of anticipatory postural adjustments during one-leg stance using inertial sensors: Evidence from subjects with parkinsonism. Frontiers in Neurology. 2017; 8:361. [DOI:10.3389/fneur.2017.00361] [PMID] [PMCID]
- Miller F. Foot deformities impact on cerebral palsy gait. In: Bachrach S, Lennon N, O'Neil ME, editors. Cerebral palsy. Berlin: Springer; 2020. [DOI:10.1007/978-3-319-74558-9_201]
- Tomlinson D, von Baeyer CL, Stinson JN, Sung L. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics. 2010; 126(5):e1168-98. [DOI:10.1542/peds.2010-1609] [PMID]
- Casey J, Rosenblad A, Rodby-Bousquet E. Postural asymmetries, pain, and ability to change position of children with cerebral palsy in sitting and supine: A cross-sectional study. Disability and Rehabilitation. 2022; 44(11):2363-71. [DOI:10.1080/09638288.2020.1834628] [PMID]
- Jan MH, Chai HM, Lin YF, Lin JC, Tsai LY, Ou YC, et al. Effects of age and sex on the results of an ankle plantar-flexor manual muscle test. Physical Therapy. 2005; 85(10):1078-84. [DOI:10.1093/ptj/85.10.1078] [PMID]
- Lin HT, Hsu AT, Chang JH, Chien CS, Chang GL. Comparison of EMG activity between maximal manual muscle testing and cybex maximal isometric testing of the quadriceps femoris. Journal of the Formosan Medical Association. 2008; 107(2):175-80. [DOI:10.1016/S0929-6646(08)60131-X] [PMID]
- Jung H, Yamasaki M. Association of lower extremity range of motion and muscle strength with physical performance of community-dwelling older women. Journal of Physiological Anthropology. 2016; 35(1):30. [DOI:10.1186/s40101-016-0120-8] [PMID] [PMCID]
- Einspieler C, Bos AF, Krieber-Tomantschger M, Alvarado E, Barbosa VM, Bertoncelli N, et al. Cerebral palsy: Early markers of clinical phenotype and functional outcome. Journal of Clinical Medicine. 2019; 8(10):1616. [DOI:10.3390/jcm8101616] [PMID] [PMCID]
- Paulson A, Vargus-Adams J. Overview of four functional classification systems commonly used in cerebral palsy. Children. 2017; 4(4):30. [DOI:10.3390/children4040030] [PMID] [PMCID]
- Piscitelli D, Vercelli S, Meroni R, Zagnoni G, Pellicciari L. Reliability of the gross motor function classification system and the manual ability classification system in children with cerebral palsy in Tanzania. Developmental Neurorehabilitation. 2019; 22(2):80-86. [DOI:10.1080/17518423.2017.1342710] [PMID]
- Dehghan L, Abdolvahab M, Bagheri H, Dalvand H, Faghih Zade S. [Inter rater reliability of Persian version of gross motor function classification system expanded and revised in patients with cerebral palsy (Persian)]. Daneshvar Medicine. 2020; 18(6):37-44. [Link]
- Garra G, Singer AJ, Taira BR, Chohan J, Cardoz H, Chisena E, et al. Validation of the wong-baker FACES pain rating scale in pediatric emergency department patients. Academic Emergency Medicine. 2010; 17(1):50-4. [DOI:10.1111/j.1553-2712.2009.00620.x] [PMID]
- Alizadeh Z, Paymard A, Khalili A, Hejr HJAoTM, Health P. A systematic review of pain assessment method in children. Annals of Tropical Medicine and Public Health. 2017; 10(4):847-9. [DOI:10.4103/ATMPH.ATMPH_155_17]
- Manikowska F, Chen BP, Jóźwiak M, Lebiedowska MK. Validation of manual muscle testing (MMT) in children and adolescents with cerebral palsy. NeuroRehabilitation. 2018; 42(1):1-7. [DOI:10.3233/NRE-172179] [PMID]
- Naqvi U, Sherman AL. Muscle strength grading. Treasure Island: StatPearls Publishing; 2021. [Link]
- Soucie JM, Wang C, Forsyth A, Funk S, Denny M, Roach KE, et al. Range of motion measurements: reference values and a database for comparison studies. Haemophilia. 2011; 17(3):500-7. [DOI:10.1111/j.1365-2516.2010.02399.x] [PMID]
- Eid MA, Aly SM, Mohamed RA. Effect of twister wrap orthosis on foot pressure distribution and balance in diplegic cerebral palsy. Journal of Musculoskeletal & Neuronal Interactions. 2018; 18(4):543-50. [PMID] [PMCID]
- Saraswat P, MacWilliams BA, Davis RB, D'Astous JL. Kinematics and kinetics of normal and planovalgus feet during walking. Gait & Posture. 2014; 39(1):339-45. [DOI:10.1016/j.gaitpost.2013.08.003] [PMID]
- Moreau NG, Bodkin AW, Bjornson K, Hobbs A, Soileau M, Lahasky K. Effectiveness of rehabilitation interventions to improve gait speed in children with cerebral palsy: Systematic review and meta-analysis. Physical Therapy. 2016; 96(12):1938-54. [DOI:10.2522/ptj.20150401] [PMID] [PMCID]
- Ganjwala D, Shah H. Management of the knee problems in spastic cerebral palsy. Indian Journal of Orthopaedics. 2019; 53(1):53-62. [DOI:10.4103/ortho.IJOrtho_339_17] [PMID] [PMCID]
- Masaki M, Sugawara K, Iizuka Y, Uchikawa Y, Isobe H, Hattori F, et al. Comparison of the degree of pes planovalgus and muscle mass of the ankle joint and foot muscles between children with Down syndrome and children with typical development. Journal of Biomechanics. 2021; 122:110482. [DOI:10.1016/j.jbiomech.2021.110482] [PMID]
- Tarakci D, Ozdincler AR, Tarakci E, Tutuncuoglu F, Ozmen M. Wii-based balance therapy to improve balance function of children with cerebral palsy: A pilot study. Journal of Physical Therapy Science. 2013; 25(9):1123-7. [DOI:10.1589/jpts.25.1123] [PMID] [PMCID]
- Chow TH. Traceable features of static plantar pressure characteristics and foot postures in college students with hemiplegic cerebral palsy. Journal of Personalized Medicine. 2022; 12(3):394. [DOI:10.3390/jpm12030394] [PMID] [PMCID]
- Pardus K, Stencel-Gabriel K, Kurdyś P, Konwant D, Nowak U. Analysis of selected methods of diagnostics and physiotherapy of pes plano-valgus in children. Journal of Education, Health and Sport. 2022; 12(11):18-22. [DOI:10.12775/JEHS.2022.12.11.002]
Type of Study: Original |
Subject:
Occupational Therapy
Received: 22/08/2023 | Accepted: 7/02/2024 | Published: 11/07/2024
Received: 22/08/2023 | Accepted: 7/02/2024 | Published: 11/07/2024
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |