Volume 25, Issue 1 (Spring 2024)
jrehab 2024, 25(1): 158-179 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mirbagheri S S, Aminian G, Bahramizadeh M, Dalvand H, Farahmand F, Vahedi M. Design and Evaluation of Dynamic Movement Orthosis on Functional Parameters in a Child With Spastic Diplegia Cerebral Palsy. jrehab 2024; 25 (1) :158-179
URL: http://rehabilitationj.uswr.ac.ir/article-1-3316-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3316-en.html
Sedigheh Sadat Mirbagheri1 

 , Gholamreza Aminian1
, Gholamreza Aminian1 

 , Mahmood Bahramizadeh *2
, Mahmood Bahramizadeh *2 

 , Hamid Dalvand3
, Hamid Dalvand3 

 , Farzam Farahmand4
, Farzam Farahmand4 

 , Mohsen Vahedi5
, Mohsen Vahedi5 




 , Gholamreza Aminian1
, Gholamreza Aminian1 

 , Mahmood Bahramizadeh *2
, Mahmood Bahramizadeh *2 

 , Hamid Dalvand3
, Hamid Dalvand3 

 , Farzam Farahmand4
, Farzam Farahmand4 

 , Mohsen Vahedi5
, Mohsen Vahedi5 


1- Department of Orthotic and Prosthetic, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran., department of orthothic and prosthetic, university of social welfare and rehabilitation sciences
2- Department of Orthotic and Prosthetic, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,ma.bahramizadeh@uswr.ac.ir
3- Department of Occupational Therapy, School of Rehabilitation, Tehran University, Tehran, Iran., Department of Occupational Therapy, School of Rehabilitation, Tehran University, Tehran, Iran
4- Department of Mechanical Engineering, Faculty of Mechanical Engineering, Sharif University of Technology, Tehran, Iran., Department of Mechanical Engineering, Sharif University of Technology
5- Department of Biostatistics and Epidemiology, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran., Department of Biostatistics and Epidemiology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
2- Department of Orthotic and Prosthetic, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Department of Occupational Therapy, School of Rehabilitation, Tehran University, Tehran, Iran., Department of Occupational Therapy, School of Rehabilitation, Tehran University, Tehran, Iran
4- Department of Mechanical Engineering, Faculty of Mechanical Engineering, Sharif University of Technology, Tehran, Iran., Department of Mechanical Engineering, Sharif University of Technology
5- Department of Biostatistics and Epidemiology, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran., Department of Biostatistics and Epidemiology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Full-Text [PDF 3210 kb]
(1130 Downloads)
| Abstract (HTML) (2959 Views)
Full-Text: (1563 Views)
Introduction
Cerebral palfsy (CP) is the most common cause of motor disability in childhood [1]; its prevalence has been reported from 1.5 to 4 per 1000 live births worldwide [2] and 2.06 per 1000 births in Iran [3]. Three-fourths (77.4%) of children with CP are spastic type [2]. Spasticity with muscle weakness limits the ability to move in these children. Among the most common walking patterns in children with CP is the crouch walking pattern using the Roda criteria [7], the excessive knee flexion pattern (66%), and excessive hip flexion and adduction (57%) [8]. Walking with knee flexion leads to increased joint stress in the tibiofemoral and patellofemoral joints [9], patella fracture stress [10], pain, and muscle fatigue [11].
Using orthotic methods is necessary to limit the excessive flexion of the lower limb joints during walking. Limitation of joint flexion reduces secondary adaptations and improves walking performance and quality of life. Using neurophysiological principles, Lycra dynamic orthoses have recently been developed as a therapeutic modality for children with CP [16]. Lycra orthoses are not directly comparable to ankle foot orthoses (AFO). These orthoses are flexible, synthetic, neoprene, and Lycra garments. They are designed to be customized based on the measurements of the child’s body and can include any part of the body affected by spasticity. The action mechanism of these elastic orthoses is such that increasing the pressure on specific muscle groups may increase proprioceptiveness and facilitate joint movements [22]. Also, by raising awareness of the body position, these elastic orthoses are effective in biomechanics and body alignment [20]
Watson et al. suggested that dynamic movement orthoses may help support unstable body areas and increase sensory feedback in neurological conditions with prolonged stretching of shortened muscles and modulation of redundant and inefficient movements [23]. In examining the effect of various orthoses on walking with a crouch pattern, most studies have examined rigid orthoses, such as floor reaction AFO. Although they have shown improvements in knee kinematics, no evidence exists about the comfort and acceptance of these orthoses. A high percentage of not using these orthoses has been reported due to their design and application, lack of comfort, inability to wear orthoses with desired shoes, and participation in various formal and informal activities as they are rigid and bulky [26]. However, descriptive evidence maintains the acceptance and comfort of dynamic orthoses for children with CP [27].
So far, no study has investigated the effect of reinforced soft orthoses in the knee and wrist area in this category of children with CP. This study was conducted to design a dynamic movement orthosis with an additional structure in the knee and wrist to improve the biomechanical alignment of the lower limb joints.
Materials and Methods
This research was a fundamental and applied study of the design and construction of the single subject design. The interaction design (A-B-BC-A) type of study was conducted in two design and evaluation stages. This study was conducted in Hamedan City, Iran, in 2022 in the Tavana Occupational Therapy Clinic. The preparation of materials and fabrication of orthosis was conducted by Teb Va Sanat Orthopedic Equipment Company in Tehran City, Iran, supervised by orthotics and prosthetics researchers of the research team.
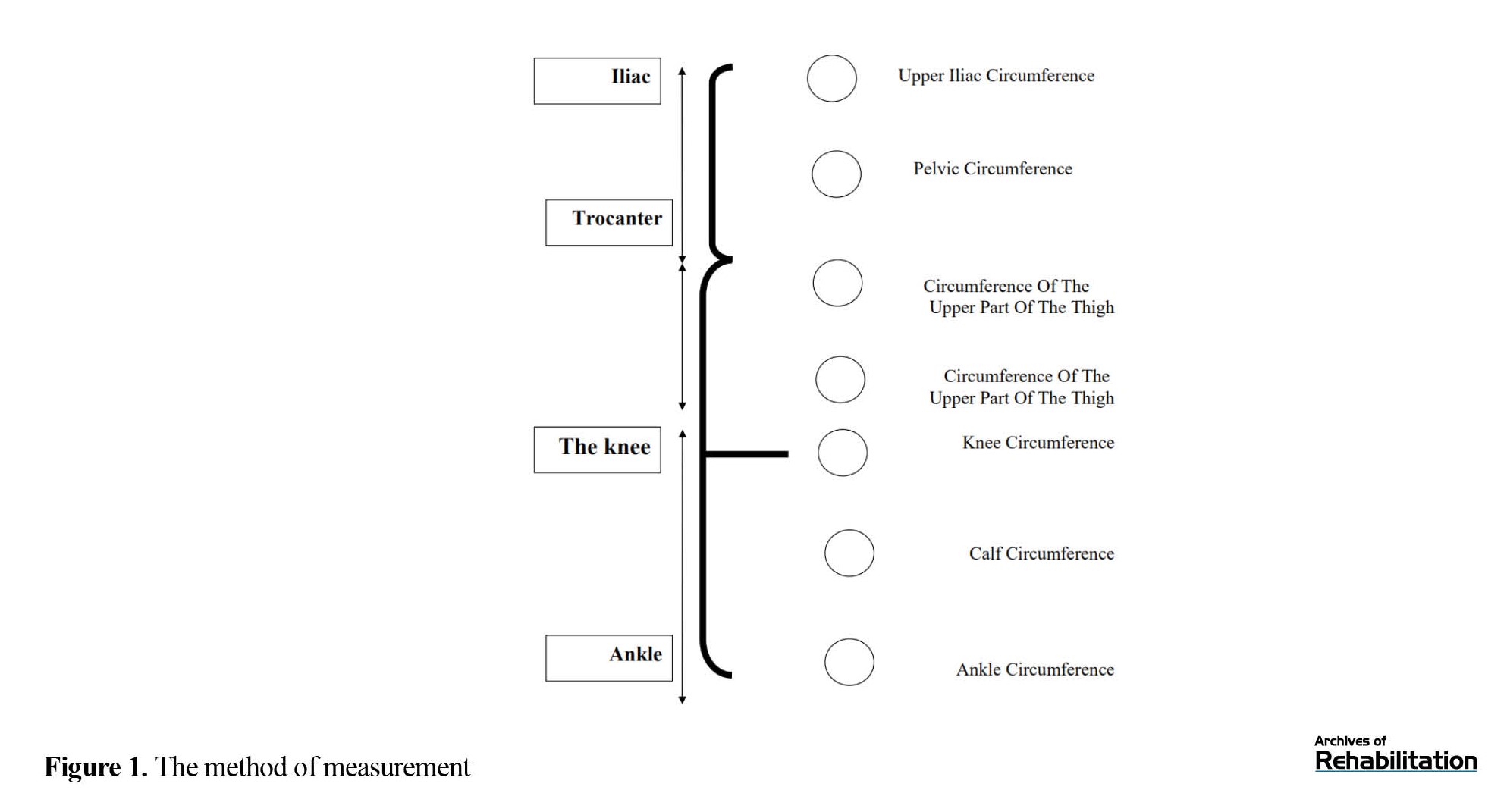
In the first stage, according to the mechanism, thigh, and fitness of the orthosis (which are among the effective factors of the orthosis), the initial plan was an orthosis containing the lower limb (pants) made of neoprene (Ancient Eagle.CR30.SBR70) by measuring specific areas on the limb (Figure 1) [28]. To improve the biomechanical alignment of the lower limb in CP children with crouch patterns and to increase stability in the sagittal plane in the knee region, reinforcement pieces were considered in the initial orthosis in the knee area. Also, to correct the biomechanical alignment of the lower limb in the closed chain of motion, an ankle piece, like ankle supports with spring reinforcement pieces and a stabilizing elastic piece tied around the ankle in the shape of “8” was used (Figure 2). The reason for choosing the spring as a reinforcement piece in the knee joint is the dynamic nature of the orthosis. In other words, the purpose of designing such an orthosis for children with CP was to use soft materials for ease of wearing compared to hard orthoses and allow joint movement. However, due to the time-consuming manufacturing process and the difficulty of wearing or removing the orthosis with the addition of spring pieces in the knee area, despite the installation of side zippers in the torso and legs, after checking on a sample with the desired criteria of the study, the second design was considered to optimize this design.
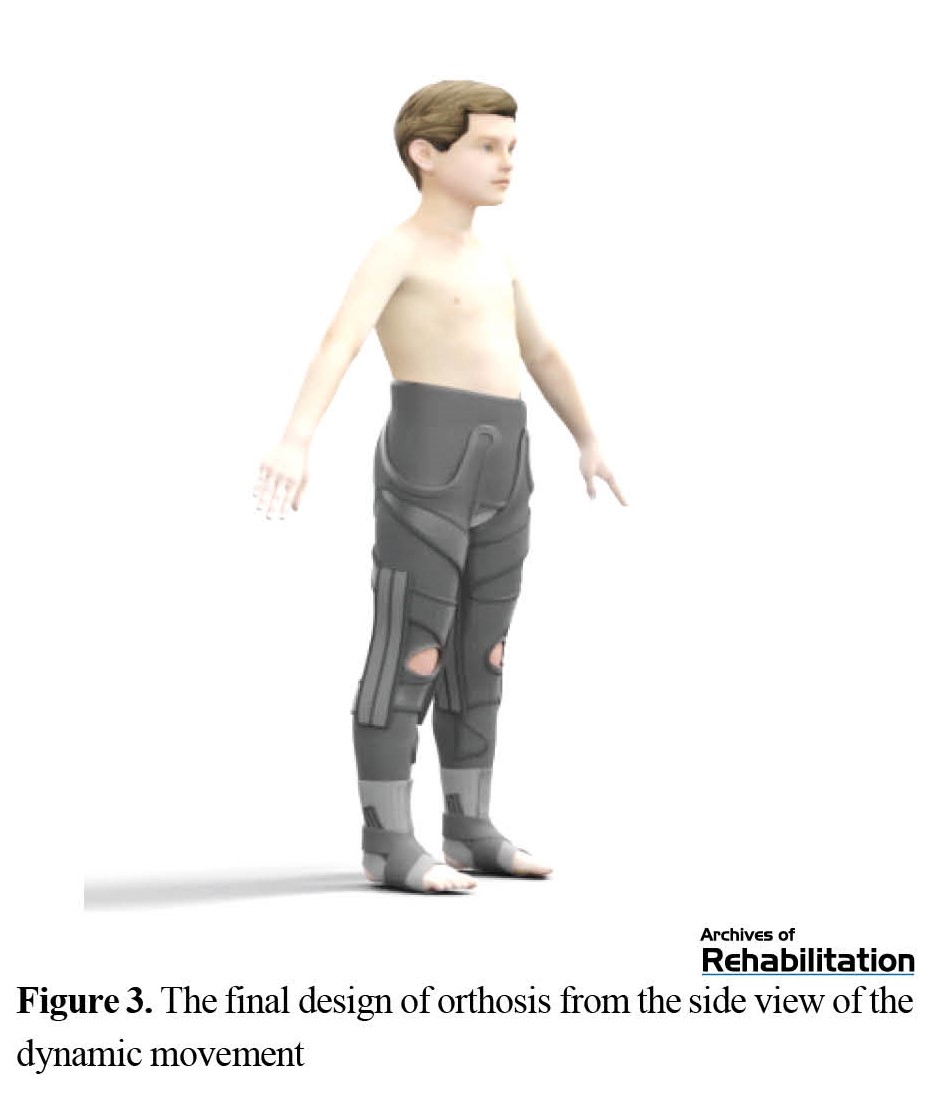
In the second design, to reduce the time of the manufacturing process, the ability to adjust the orthosis to individual sizes was provided by changing the type of elastic material and inserting straps in the thigh and leg area. The elastic material used in the second design was another type of neoprene with the adhesive property of a rough strap. Each part of the orthosis had goals. According to hip joint flexion in children with crouch patterns, the lumbar part was inserted by the related part of the body to correct the alignment of the body and hip joint by applying pressure and tension to this area. Straps in the thigh area to apply pressure on the spastic muscles, especially the adductor muscles, and the strap in the leg area under the patella were installed to apply extensor torque on the knee, similar to the one in floor reaction AFO. Four springs were placed around each knee joint, which could be separated in this study to compare the state without orthosis spring and the state of Buffner. Two springs and a supporting elastic in the wrist area were also installed around the wrist joint to create stability and maintain better alignment in the biomechanical closed chain. The pattern was designed to correspond to two sizes for 6- to 12-year-old children. This orthosis was designed using the advanced Marvelous software for clothing design (Figure 3).
Advantages of the new design
The advantages of the new design are as follows: The capability to measure in two sizes for children 6 to 12 years old, which are different in terms of the height of the lower limbs, and shortening the custom manufacturing process; the capability to adjust the environmental pressure through the thigh and leg straps and solve the problem of the tight or loose orthosis in the previous design; facilitation in putting on and taking off and making it easier to go to the bathroom compared to the previous design and design of jumpsuit clothes. After the second design was prepared, the second phase began.
The second stage included evaluation and validation of the final orthosis with single case experimental design and interaction design (A-B-BC-A) for the study sample. The study participants included a child with spastic diplegia CP [29] aged 6 to 12 years, level one or two of the gross motor function classification system expanded and revised (GMFCS E&R) and crouch walking pattern, who did not need external aids, such as a walker, to walk [29, 30]. The subject could walk at least 10 m without support [18]. The inclusion criteria were appropriate cooperation from the child and family [31], no history of orthopedic surgery in the last 9 months [18, 31, 32], and no history of epilepsy and respiratory diseases [20]. Meanwhile, the exclusion criteria were passing less than 9 months from the last botulinum toxin injection and the presence of proven deformity in the lower limb. The evaluations began after obtaining written and oral consent from the child’s family.
The basic phase (A1) was the control period. In each phase, the participant was subjected to the usual occupational therapy treatments three times a week, and the values of the functional tests: The 10-m walking test (10MWT), time up and go (TUG), and modified Ashworth scale (MAS). To evaluate right and left hamstring spasticity, the Canadian occupational performance measure (COPM) was conducted twice a week for one month (4 weeks). The results of the evaluations were recorded by a senior expert in occupational therapy who was present in the study process. After the basic phase, the intended design had two phases of intervention: The first intervention included dynamic movement orthosis (B), and the second was dynamic movement orthosis with knee springs and wristbands (BC), which were randomly selected. The method of wearing the orthosis in the intervention phases was such that to prevent the effect of wearing shoes and orthoses, it was worn for at least 5 h at home and at a time other than sleeping and without shoes or sandals. The post-intervention phase (A2) included the follow-up phase, which was also 4 weeks long, and similar to the baseline phase, the child underwent occupational therapy exercises. Also, the performance tests were conducted twice a week.
Results
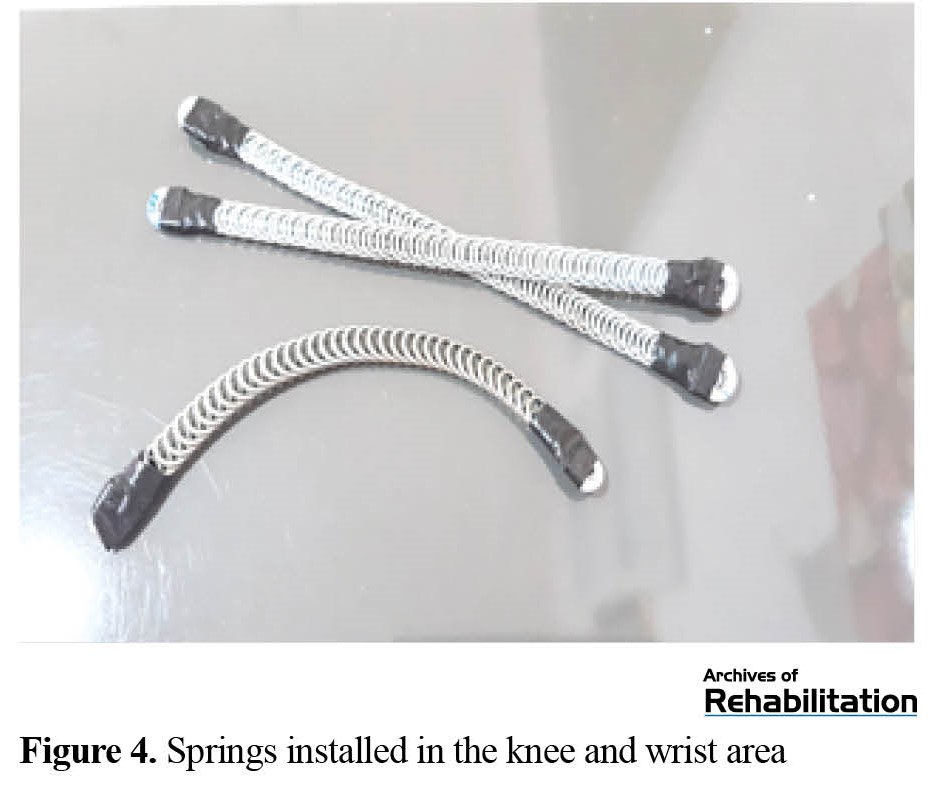
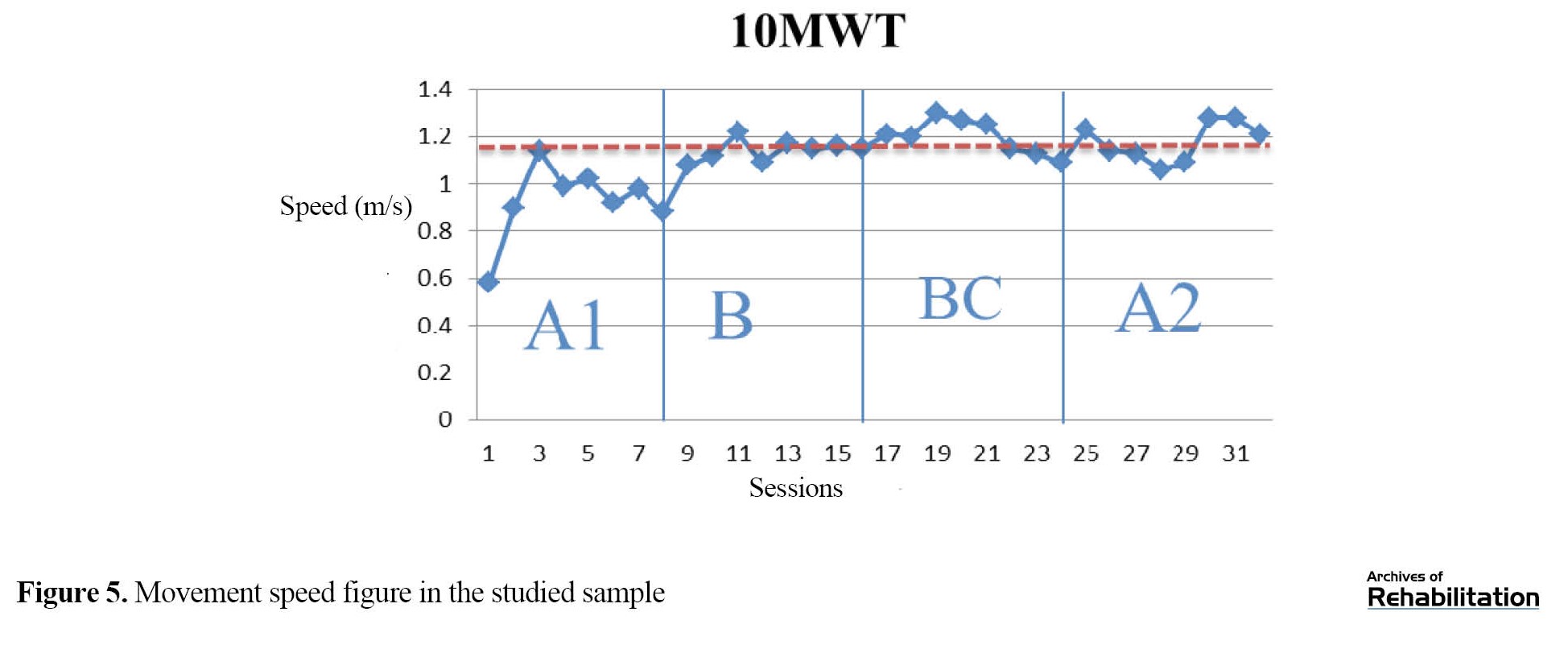
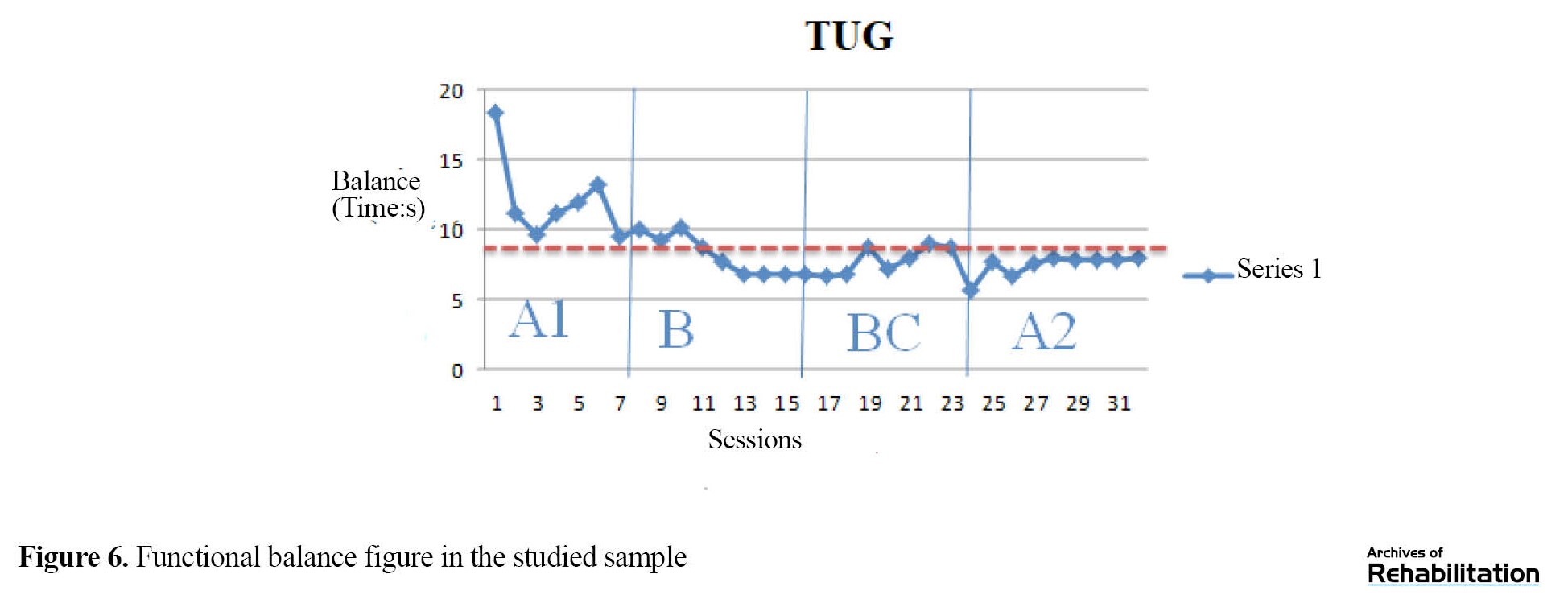
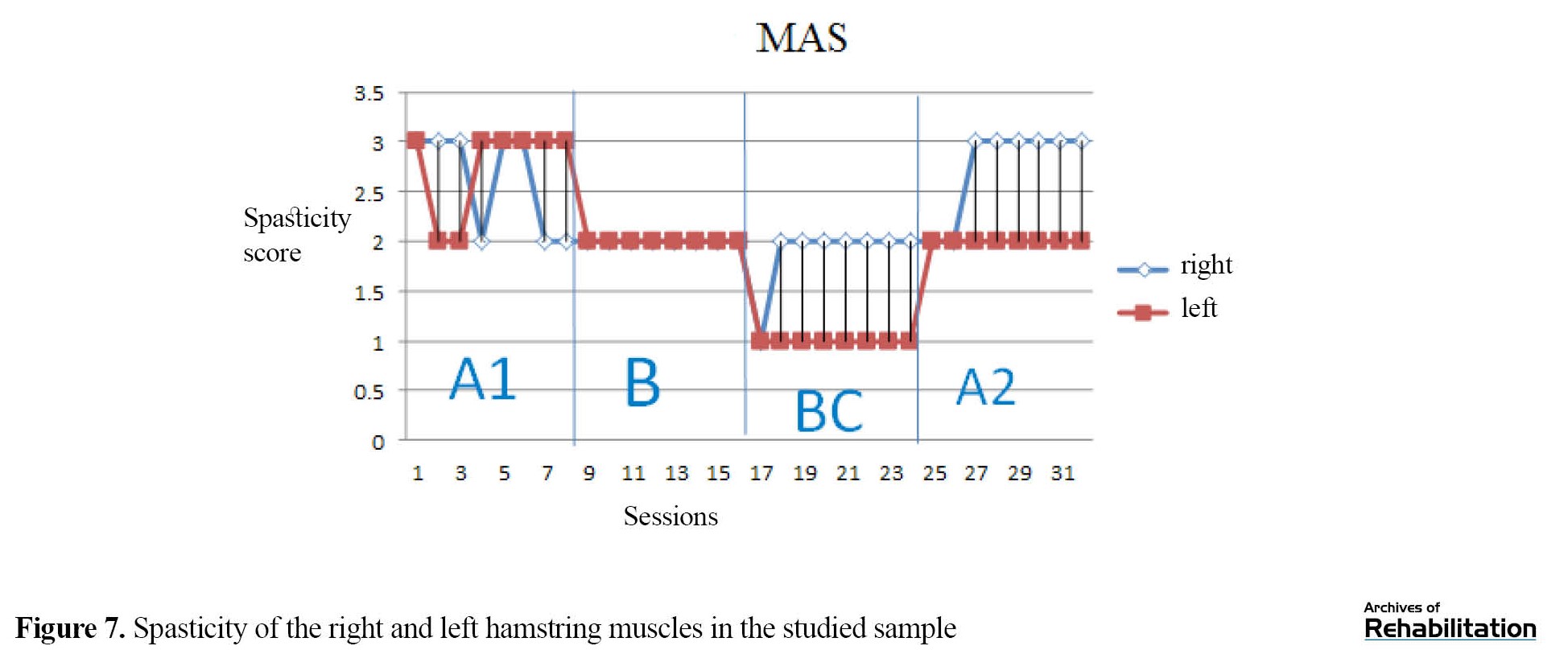
Among dynamic orthoses (garments), this dynamic movement orthosis was the first and only orthosis that used dynamic reinforcement pieces in the knee and ankle joints. The springs used are made of steel wire with a thickness of 12 mm. Also, these springs are doubled springs with a width of one centimeter that have been rolled (Figure 4). The study participant was an 8-year-old boy with Gross motor function classification system Expanded & Revised (GMFCS E&R), height of 135 cm, and weight of 50 kg. The participant’s walking speed and balance with 10MWT and TUG scales and right and left hamstring spasticity changes with an MAS were evaluated. At the end of each phase, the COPM was used to check the occupational performance and satisfaction with the child’s occupational performance. Figures 5, 6, and 7 depict the speed, balance, and spasticity of the hamstring muscles of the right and left leg of the child.
The interpretation of the effectiveness of the provided interventions based on the data non-overlapping statistics is as follows: Percentage of non-overlapping data (PND) of 90%, very effective interventions; PND of 70%-90%, effective interventions; PND of 50%-70%, ambiguity in treatment effectiveness; PND of 50% or less, ineffective treatment. In the interpretation of the effectiveness of the interventions, the Cohen d and the Hedges g effect size indices were also examined. According to a study, values less than 0.87 indicate small effect sizes, between 0.87 and 2.67 medium, and above 2.67 large [33].
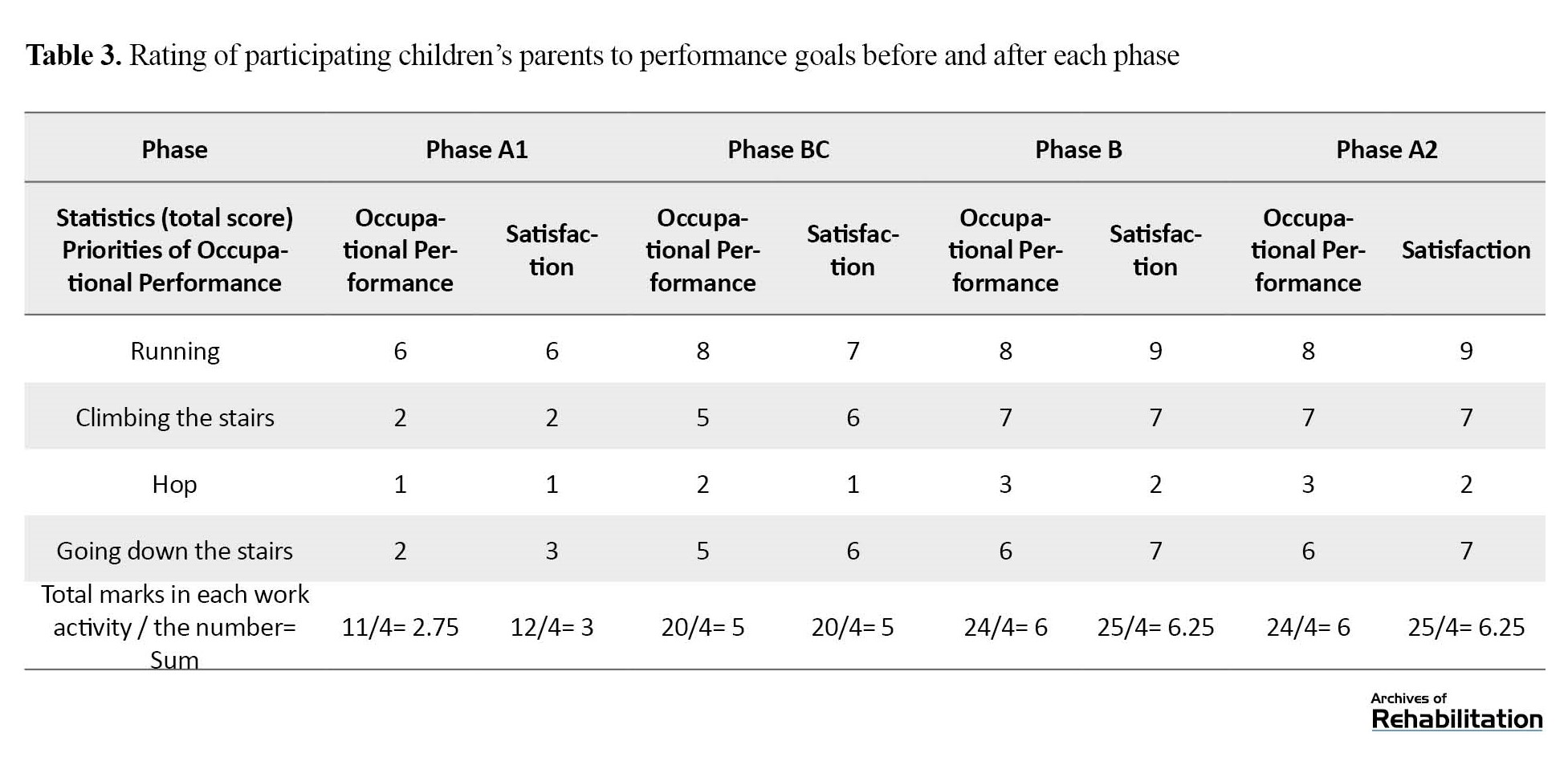
According to Figure 5, in the visual analysis of the movement speed, the maximum movement speed in the base phase is about 1.2 m/s, which did not change in the first B. Still, in the second BC, a slight increase in speed was visible, and the follow-up phase was associated with a decrease and an increase. Table 1 presents the PND index values and the speed variable’s effect size.
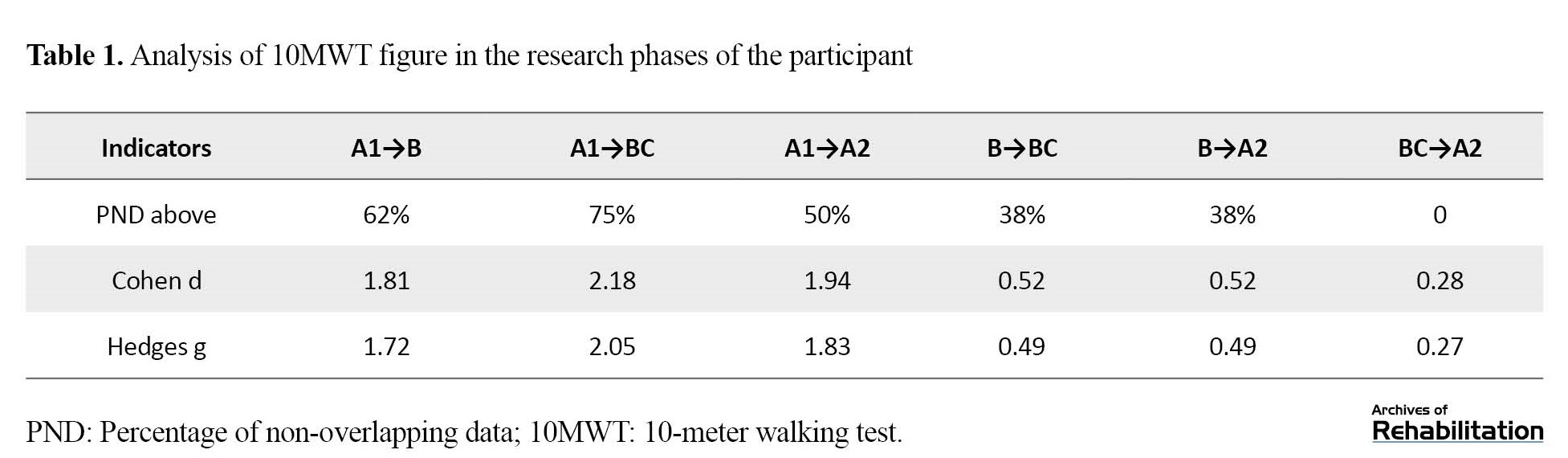
Comparing the phases of the study based on the PND index, from the base phase to intervention B, ambiguity exists in the effectiveness of the intervention (PND=62%), but from the base phase to BC, the intervention was effective (PND=75%). The effectiveness is not observed compared to the other phases (PND 50%) (Table 1).
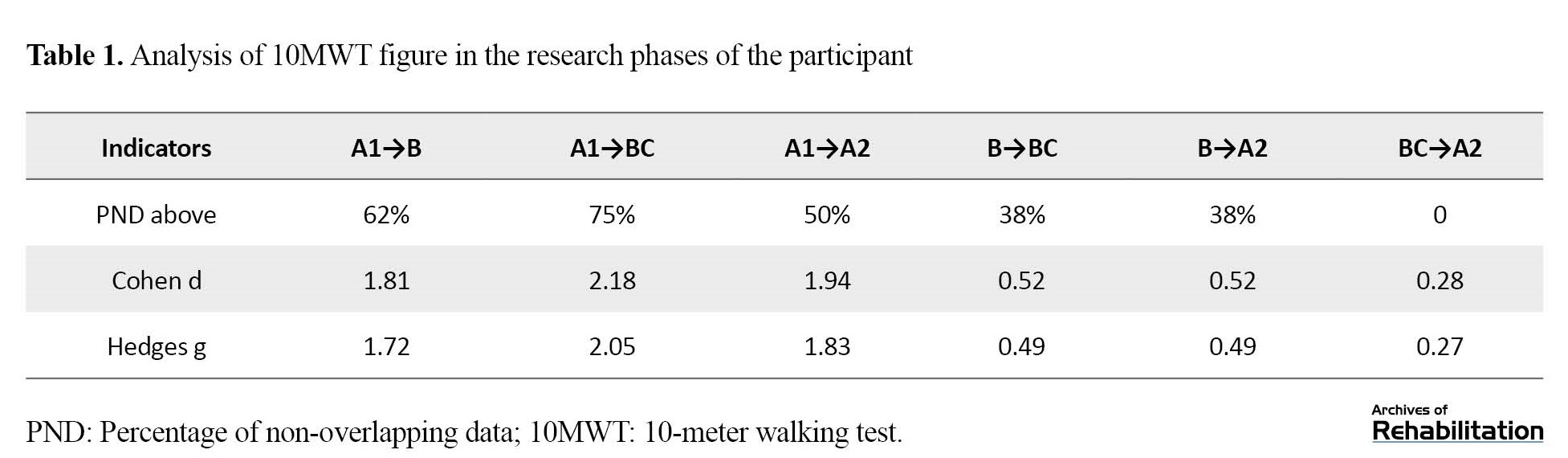
In the visual analysis of the balance figure, the decreasing trend of time was observed while walking, which remains constant in the follow-up phase (Figure 6). According to Table 2, the value of the PND index compared to the basic phases of the first and second intervention and follow-up in the functional balance variable shows the effectiveness of the intervention (PND=100% and PND=88%).
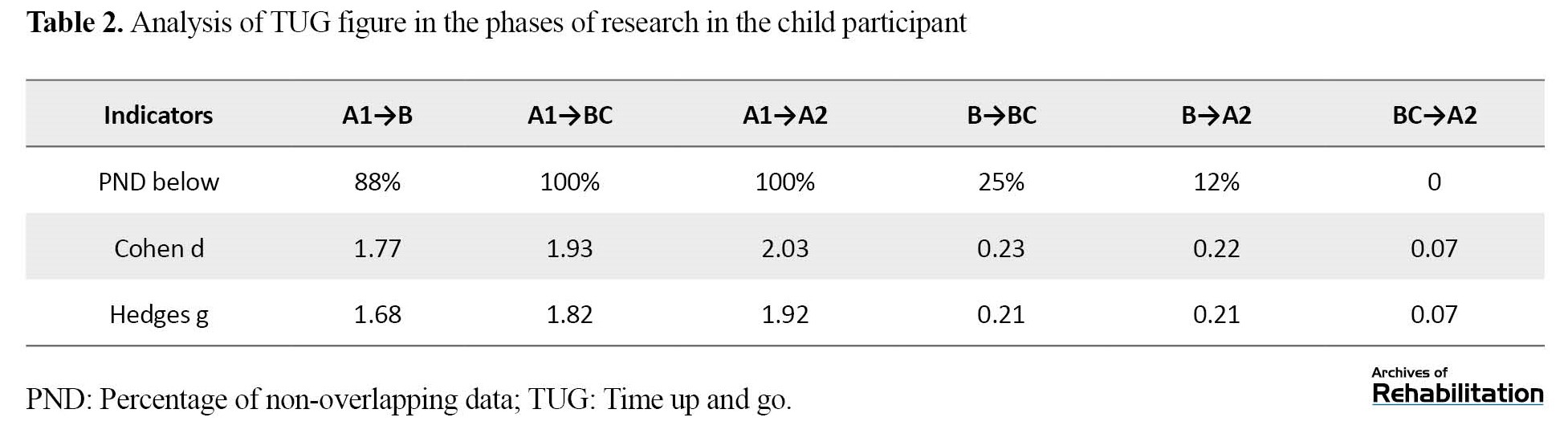
No intervention effectiveness is observed in the rest of the phases (PND>50%). In examining the effect size indices of the Cohen d and the Hedges g in the basic phase to the first and second intervention and the follow-up phase, the average effect size values were above 0.87 and below 2.67 (Table 2).
According to Figure 7, the visual analysis of the right and left hamstring spasticity showed a decreasing trend of spasticity in the first and second intervention phases and an increase in the follow-up phase.
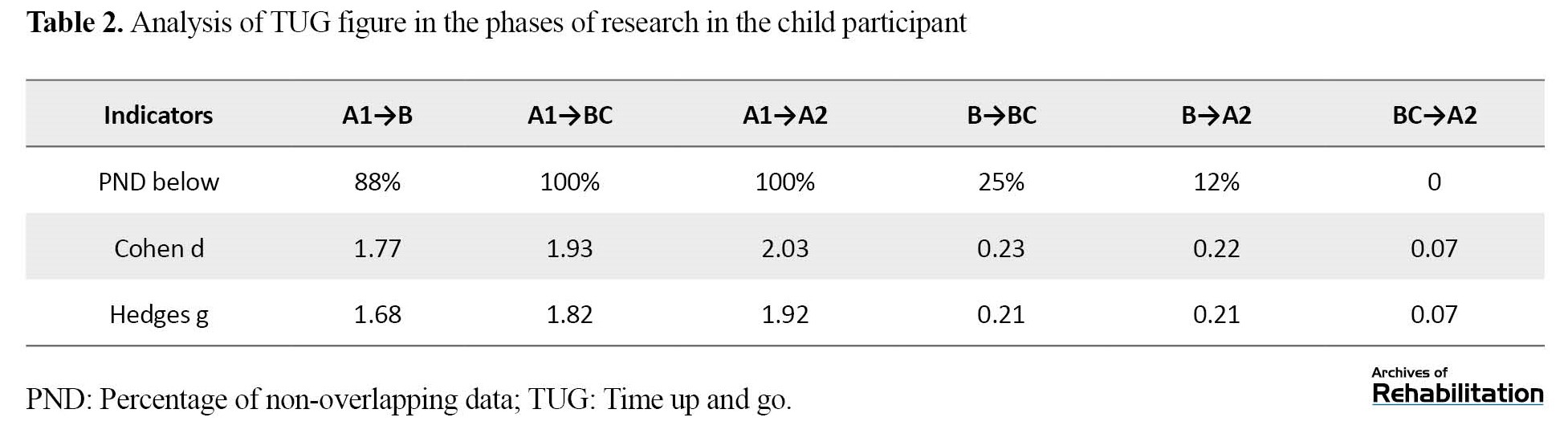
Table 3 presents parents’ satisfaction ratings with their child’s occupational performance in 4 activities parents desire.
In all 4 activities mentioned in the Table, the child’s occupational performance score and satisfaction have increased. This increase from the base phase to the second intervention and the follow-up phase has clinical significance because the difference between the average occupational performance and satisfaction with occupational performance in the base phase and the BC phase (second intervention) is more than 2.5 points [34].
Discussion
The mechanisms responsible for changes in motion control by Lycra orthoses and similar orthoses are neurophysiological and biomechanical. Proprioception, deep pressure, vibration, surface contact, and correcting the biomechanical alignment of the body increase proprioceptive feedback that improves posture and body awareness, muscle activity, and movement control [16]. One of the advantages of using this type of dynamic orthoses compared to hard orthoses is the neurophysiological mechanism of these orthoses. Despite being soft, these orthoses may be worn more often than hard orthoses due to their acceptance and comfort by children [27].
According to the PND Table results, functional speed improvement was observed in the second intervention phase. Still, ambiguity was observed in the effectiveness of the other phases. Also, no effect was observed in the comparison of the two phases of the intervention. Interestingly, neither dynamic orthosis showed a difference in the speed variable during walking, which is also clear in the visual analysis of the Figure. In the follow-up phase, according to the figures and tables, ambiguity exists in the durability of the work. One study [29] evaluated a dynamic elastomeric fabric orthosis on the functional speed of children with spastic diplegia CP through 10 MWT. The study results show an increase in speed in 5 of the 8 samples included in the study. The design of this study was a single case experimental design and A-B-A. The reason why the speed increased in some phases of the intervention and changes in the speed were observed in some phases may be due to two reasons: No control was observed over the activities performed by the participant during the intervention period, and no standard time existed to wear orthoses in children, and follow-up on wearing orthoses during the day was conducted by asking parents.
In examining the variable of balance while walking, compared to the basic phase with the first and second intervention phases (either dynamic orthosis or dynamic orthosis with spring and wristband), the effectiveness of the intervention existed, and reducing time meant improving balance in the studied sample. Comparing the baseline phase with the follow-up, the orthosis’s effectiveness exists and indicates the durability of the effect in the follow-up phase. Among the studies that evaluated the impact of suites, two evaluated balance after using orthoses similar to Lycra, although the balance evaluation tool in these studies is different. Flanagan et al. [19] assessed the effect of Lycra garments covering the whole body on children’s CP balance using the Bruininks-Oseretsky test of motor proficiency. Flanagan’s study is consistent with the present study regarding increasing balance after using dynamic orthoses. Also, Hosseini et al. [35] evaluated dynamic neoprene orthosis on postural control using a force plate and functional balance via Berg’s balance scale. Based on this balance scale, an increase in the functional balance of 5 children participating in the study was reported after 6 weeks of using the dynamic orthosis.
In children with spastic diplegia CP, the lower limb muscles are involved in spasticity. The possible mechanism of dynamic orthoses may cause adjustment of the tone of the spastic muscles via pressure or stretching on the spastic muscles and also by changing the biomechanical direction of the lower limb; therefore, in examining the spasticity of the hamstring muscle, after the amount of spasticity remains constant in the baseline phase, in the intervention phases in the right and left leg, a decrease was observed in hamstring spasticity, which in the follow-up phase, the spasticity value reached either the initial value in the baseline phase or one unit less than the baseline phase.
Accordingly, as long as the orthosis is worn, the muscle tone may decrease, and this problem can improve functional variables, such as the speed and balance discussed in the above sections.
The increased occupational performance scores and satisfaction with the child’s occupational performance in the intervention phases showed clinical significance. Previous studies also showed increased occupational performance [19, 36]. In another study, Flanagan et al. examined occupational performance using Theratog. After two months of using the orthosis, the satisfaction with occupational performance was significant [24]. In another study, significant results were reported in the COPM criterion in the immediate effect and 2 months and 4 months after the intervention [36].
A study examined the safety level and the amount of pressure exerted by a Lycra orthosis on the hypertonic arm muscles of children with CP. Safety was measured by the number and severity of adverse events, including skin problems and pressure, which may occur while wearing these garments. In this study, wearing time and possible adverse events were recorded daily by the child’s parents. The study results stated that the orthosis’s daily wearing time was good, and the rate of adverse events was very low [37]. In this study, the time the child wore the orthosis in each evaluation session was reported by the child’s parents, and the adverse effects caused by the orthosis were not reported either.
According to the results of this study, in the reduction of spasticity in the intervention phases, improvement in occupational performance and increase in satisfaction with occupational performance may be related to the decrease of muscle tonicity during activities. These results are also consistent with the results obtained in speed and balance.
Conclusion
The design of the orthosis in two sizes for 6 to 12 years reduced the process of customizing this orthosis. The designed dynamic orthosis modulates muscle tonicity and may improve speed, balance, and occupational performance. These improvements can also be observed in the child’s daily activities. Regarding the difference between orthosis with spring and wristband and orthosis without spring and wristband, no difference was found in the functional variables of this study and the period considered.
Limitations of the study include the unavailability of the Lycra material used in other studies in Iran and the use of similar material, as well as the inability to accurately control the time of wearing the orthosis at home and the small number of samples. It is suggested that this orthosis be performed in a larger sample size and with design changes in CP children with higher levels of GMFCS E&R and older ages.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1399.131). Before the start of the study, oral and written informed consent was obtained from the parents of children with CP to participate in the study. The child and the family could withdraw from participating in the research at any stage. The research process had no interference with common child treatments.
Funding
This article was extracted from the PhD dissertation of Sedige Sadat Mirbagheri, approved by Department of Orthotics and Prosthetics, University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Conceptualization: Mahmood Bahramizadeh, Gholamreza Aminian, and Sadigheh Sadat Mirbagheri; Methodology: Gholamreza Aminian, Mohsen Vahedi, Farzam Farhamand, and Sadigheh Sadat Mirbagheri; Research and review: Sadigheh Sadat Mirbaghri; Sources: Sadigheh Sadat Mirbaghri; Data analysis: Farzam Farhamand, Mohsen Vahedi, Hamid Dalvand, and Sadigheh Sadat Mirbagheri; Finance: Sadigheh Sadat Mirbaghri; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Teb and Sanat Company and the sincere cooperation of the company manager, Mohsen Mirmehdi, for implementing the orthosis manufacturing process.
References
Cerebral palfsy (CP) is the most common cause of motor disability in childhood [1]; its prevalence has been reported from 1.5 to 4 per 1000 live births worldwide [2] and 2.06 per 1000 births in Iran [3]. Three-fourths (77.4%) of children with CP are spastic type [2]. Spasticity with muscle weakness limits the ability to move in these children. Among the most common walking patterns in children with CP is the crouch walking pattern using the Roda criteria [7], the excessive knee flexion pattern (66%), and excessive hip flexion and adduction (57%) [8]. Walking with knee flexion leads to increased joint stress in the tibiofemoral and patellofemoral joints [9], patella fracture stress [10], pain, and muscle fatigue [11].
Using orthotic methods is necessary to limit the excessive flexion of the lower limb joints during walking. Limitation of joint flexion reduces secondary adaptations and improves walking performance and quality of life. Using neurophysiological principles, Lycra dynamic orthoses have recently been developed as a therapeutic modality for children with CP [16]. Lycra orthoses are not directly comparable to ankle foot orthoses (AFO). These orthoses are flexible, synthetic, neoprene, and Lycra garments. They are designed to be customized based on the measurements of the child’s body and can include any part of the body affected by spasticity. The action mechanism of these elastic orthoses is such that increasing the pressure on specific muscle groups may increase proprioceptiveness and facilitate joint movements [22]. Also, by raising awareness of the body position, these elastic orthoses are effective in biomechanics and body alignment [20]
Watson et al. suggested that dynamic movement orthoses may help support unstable body areas and increase sensory feedback in neurological conditions with prolonged stretching of shortened muscles and modulation of redundant and inefficient movements [23]. In examining the effect of various orthoses on walking with a crouch pattern, most studies have examined rigid orthoses, such as floor reaction AFO. Although they have shown improvements in knee kinematics, no evidence exists about the comfort and acceptance of these orthoses. A high percentage of not using these orthoses has been reported due to their design and application, lack of comfort, inability to wear orthoses with desired shoes, and participation in various formal and informal activities as they are rigid and bulky [26]. However, descriptive evidence maintains the acceptance and comfort of dynamic orthoses for children with CP [27].
So far, no study has investigated the effect of reinforced soft orthoses in the knee and wrist area in this category of children with CP. This study was conducted to design a dynamic movement orthosis with an additional structure in the knee and wrist to improve the biomechanical alignment of the lower limb joints.
Materials and Methods
This research was a fundamental and applied study of the design and construction of the single subject design. The interaction design (A-B-BC-A) type of study was conducted in two design and evaluation stages. This study was conducted in Hamedan City, Iran, in 2022 in the Tavana Occupational Therapy Clinic. The preparation of materials and fabrication of orthosis was conducted by Teb Va Sanat Orthopedic Equipment Company in Tehran City, Iran, supervised by orthotics and prosthetics researchers of the research team.
In the first stage, according to the mechanism, thigh, and fitness of the orthosis (which are among the effective factors of the orthosis), the initial plan was an orthosis containing the lower limb (pants) made of neoprene (Ancient Eagle.CR30.SBR70) by measuring specific areas on the limb (Figure 1) [28]. To improve the biomechanical alignment of the lower limb in CP children with crouch patterns and to increase stability in the sagittal plane in the knee region, reinforcement pieces were considered in the initial orthosis in the knee area. Also, to correct the biomechanical alignment of the lower limb in the closed chain of motion, an ankle piece, like ankle supports with spring reinforcement pieces and a stabilizing elastic piece tied around the ankle in the shape of “8” was used (Figure 2). The reason for choosing the spring as a reinforcement piece in the knee joint is the dynamic nature of the orthosis. In other words, the purpose of designing such an orthosis for children with CP was to use soft materials for ease of wearing compared to hard orthoses and allow joint movement. However, due to the time-consuming manufacturing process and the difficulty of wearing or removing the orthosis with the addition of spring pieces in the knee area, despite the installation of side zippers in the torso and legs, after checking on a sample with the desired criteria of the study, the second design was considered to optimize this design.
In the second design, to reduce the time of the manufacturing process, the ability to adjust the orthosis to individual sizes was provided by changing the type of elastic material and inserting straps in the thigh and leg area. The elastic material used in the second design was another type of neoprene with the adhesive property of a rough strap. Each part of the orthosis had goals. According to hip joint flexion in children with crouch patterns, the lumbar part was inserted by the related part of the body to correct the alignment of the body and hip joint by applying pressure and tension to this area. Straps in the thigh area to apply pressure on the spastic muscles, especially the adductor muscles, and the strap in the leg area under the patella were installed to apply extensor torque on the knee, similar to the one in floor reaction AFO. Four springs were placed around each knee joint, which could be separated in this study to compare the state without orthosis spring and the state of Buffner. Two springs and a supporting elastic in the wrist area were also installed around the wrist joint to create stability and maintain better alignment in the biomechanical closed chain. The pattern was designed to correspond to two sizes for 6- to 12-year-old children. This orthosis was designed using the advanced Marvelous software for clothing design (Figure 3).
Advantages of the new design
The advantages of the new design are as follows: The capability to measure in two sizes for children 6 to 12 years old, which are different in terms of the height of the lower limbs, and shortening the custom manufacturing process; the capability to adjust the environmental pressure through the thigh and leg straps and solve the problem of the tight or loose orthosis in the previous design; facilitation in putting on and taking off and making it easier to go to the bathroom compared to the previous design and design of jumpsuit clothes. After the second design was prepared, the second phase began.
The second stage included evaluation and validation of the final orthosis with single case experimental design and interaction design (A-B-BC-A) for the study sample. The study participants included a child with spastic diplegia CP [29] aged 6 to 12 years, level one or two of the gross motor function classification system expanded and revised (GMFCS E&R) and crouch walking pattern, who did not need external aids, such as a walker, to walk [29, 30]. The subject could walk at least 10 m without support [18]. The inclusion criteria were appropriate cooperation from the child and family [31], no history of orthopedic surgery in the last 9 months [18, 31, 32], and no history of epilepsy and respiratory diseases [20]. Meanwhile, the exclusion criteria were passing less than 9 months from the last botulinum toxin injection and the presence of proven deformity in the lower limb. The evaluations began after obtaining written and oral consent from the child’s family.
The basic phase (A1) was the control period. In each phase, the participant was subjected to the usual occupational therapy treatments three times a week, and the values of the functional tests: The 10-m walking test (10MWT), time up and go (TUG), and modified Ashworth scale (MAS). To evaluate right and left hamstring spasticity, the Canadian occupational performance measure (COPM) was conducted twice a week for one month (4 weeks). The results of the evaluations were recorded by a senior expert in occupational therapy who was present in the study process. After the basic phase, the intended design had two phases of intervention: The first intervention included dynamic movement orthosis (B), and the second was dynamic movement orthosis with knee springs and wristbands (BC), which were randomly selected. The method of wearing the orthosis in the intervention phases was such that to prevent the effect of wearing shoes and orthoses, it was worn for at least 5 h at home and at a time other than sleeping and without shoes or sandals. The post-intervention phase (A2) included the follow-up phase, which was also 4 weeks long, and similar to the baseline phase, the child underwent occupational therapy exercises. Also, the performance tests were conducted twice a week.
Results
Among dynamic orthoses (garments), this dynamic movement orthosis was the first and only orthosis that used dynamic reinforcement pieces in the knee and ankle joints. The springs used are made of steel wire with a thickness of 12 mm. Also, these springs are doubled springs with a width of one centimeter that have been rolled (Figure 4). The study participant was an 8-year-old boy with Gross motor function classification system Expanded & Revised (GMFCS E&R), height of 135 cm, and weight of 50 kg. The participant’s walking speed and balance with 10MWT and TUG scales and right and left hamstring spasticity changes with an MAS were evaluated. At the end of each phase, the COPM was used to check the occupational performance and satisfaction with the child’s occupational performance. Figures 5, 6, and 7 depict the speed, balance, and spasticity of the hamstring muscles of the right and left leg of the child.
The interpretation of the effectiveness of the provided interventions based on the data non-overlapping statistics is as follows: Percentage of non-overlapping data (PND) of 90%, very effective interventions; PND of 70%-90%, effective interventions; PND of 50%-70%, ambiguity in treatment effectiveness; PND of 50% or less, ineffective treatment. In the interpretation of the effectiveness of the interventions, the Cohen d and the Hedges g effect size indices were also examined. According to a study, values less than 0.87 indicate small effect sizes, between 0.87 and 2.67 medium, and above 2.67 large [33].
According to Figure 5, in the visual analysis of the movement speed, the maximum movement speed in the base phase is about 1.2 m/s, which did not change in the first B. Still, in the second BC, a slight increase in speed was visible, and the follow-up phase was associated with a decrease and an increase. Table 1 presents the PND index values and the speed variable’s effect size.
Comparing the phases of the study based on the PND index, from the base phase to intervention B, ambiguity exists in the effectiveness of the intervention (PND=62%), but from the base phase to BC, the intervention was effective (PND=75%). The effectiveness is not observed compared to the other phases (PND 50%) (Table 1).
In the visual analysis of the balance figure, the decreasing trend of time was observed while walking, which remains constant in the follow-up phase (Figure 6). According to Table 2, the value of the PND index compared to the basic phases of the first and second intervention and follow-up in the functional balance variable shows the effectiveness of the intervention (PND=100% and PND=88%).
No intervention effectiveness is observed in the rest of the phases (PND>50%). In examining the effect size indices of the Cohen d and the Hedges g in the basic phase to the first and second intervention and the follow-up phase, the average effect size values were above 0.87 and below 2.67 (Table 2).
According to Figure 7, the visual analysis of the right and left hamstring spasticity showed a decreasing trend of spasticity in the first and second intervention phases and an increase in the follow-up phase.
Table 3 presents parents’ satisfaction ratings with their child’s occupational performance in 4 activities parents desire.
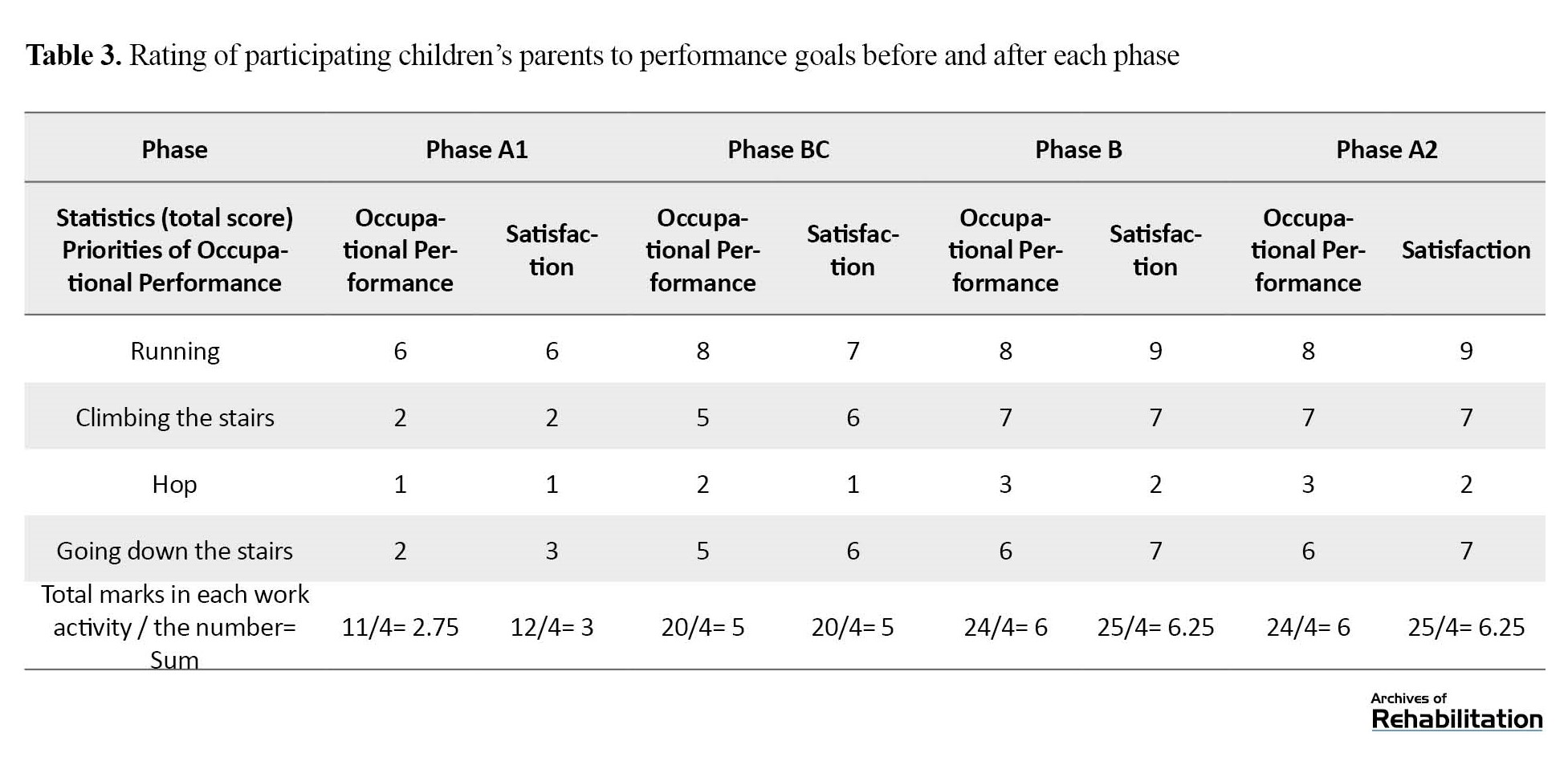
In all 4 activities mentioned in the Table, the child’s occupational performance score and satisfaction have increased. This increase from the base phase to the second intervention and the follow-up phase has clinical significance because the difference between the average occupational performance and satisfaction with occupational performance in the base phase and the BC phase (second intervention) is more than 2.5 points [34].
Discussion
The mechanisms responsible for changes in motion control by Lycra orthoses and similar orthoses are neurophysiological and biomechanical. Proprioception, deep pressure, vibration, surface contact, and correcting the biomechanical alignment of the body increase proprioceptive feedback that improves posture and body awareness, muscle activity, and movement control [16]. One of the advantages of using this type of dynamic orthoses compared to hard orthoses is the neurophysiological mechanism of these orthoses. Despite being soft, these orthoses may be worn more often than hard orthoses due to their acceptance and comfort by children [27].
According to the PND Table results, functional speed improvement was observed in the second intervention phase. Still, ambiguity was observed in the effectiveness of the other phases. Also, no effect was observed in the comparison of the two phases of the intervention. Interestingly, neither dynamic orthosis showed a difference in the speed variable during walking, which is also clear in the visual analysis of the Figure. In the follow-up phase, according to the figures and tables, ambiguity exists in the durability of the work. One study [29] evaluated a dynamic elastomeric fabric orthosis on the functional speed of children with spastic diplegia CP through 10 MWT. The study results show an increase in speed in 5 of the 8 samples included in the study. The design of this study was a single case experimental design and A-B-A. The reason why the speed increased in some phases of the intervention and changes in the speed were observed in some phases may be due to two reasons: No control was observed over the activities performed by the participant during the intervention period, and no standard time existed to wear orthoses in children, and follow-up on wearing orthoses during the day was conducted by asking parents.
In examining the variable of balance while walking, compared to the basic phase with the first and second intervention phases (either dynamic orthosis or dynamic orthosis with spring and wristband), the effectiveness of the intervention existed, and reducing time meant improving balance in the studied sample. Comparing the baseline phase with the follow-up, the orthosis’s effectiveness exists and indicates the durability of the effect in the follow-up phase. Among the studies that evaluated the impact of suites, two evaluated balance after using orthoses similar to Lycra, although the balance evaluation tool in these studies is different. Flanagan et al. [19] assessed the effect of Lycra garments covering the whole body on children’s CP balance using the Bruininks-Oseretsky test of motor proficiency. Flanagan’s study is consistent with the present study regarding increasing balance after using dynamic orthoses. Also, Hosseini et al. [35] evaluated dynamic neoprene orthosis on postural control using a force plate and functional balance via Berg’s balance scale. Based on this balance scale, an increase in the functional balance of 5 children participating in the study was reported after 6 weeks of using the dynamic orthosis.
In children with spastic diplegia CP, the lower limb muscles are involved in spasticity. The possible mechanism of dynamic orthoses may cause adjustment of the tone of the spastic muscles via pressure or stretching on the spastic muscles and also by changing the biomechanical direction of the lower limb; therefore, in examining the spasticity of the hamstring muscle, after the amount of spasticity remains constant in the baseline phase, in the intervention phases in the right and left leg, a decrease was observed in hamstring spasticity, which in the follow-up phase, the spasticity value reached either the initial value in the baseline phase or one unit less than the baseline phase.
Accordingly, as long as the orthosis is worn, the muscle tone may decrease, and this problem can improve functional variables, such as the speed and balance discussed in the above sections.
The increased occupational performance scores and satisfaction with the child’s occupational performance in the intervention phases showed clinical significance. Previous studies also showed increased occupational performance [19, 36]. In another study, Flanagan et al. examined occupational performance using Theratog. After two months of using the orthosis, the satisfaction with occupational performance was significant [24]. In another study, significant results were reported in the COPM criterion in the immediate effect and 2 months and 4 months after the intervention [36].
A study examined the safety level and the amount of pressure exerted by a Lycra orthosis on the hypertonic arm muscles of children with CP. Safety was measured by the number and severity of adverse events, including skin problems and pressure, which may occur while wearing these garments. In this study, wearing time and possible adverse events were recorded daily by the child’s parents. The study results stated that the orthosis’s daily wearing time was good, and the rate of adverse events was very low [37]. In this study, the time the child wore the orthosis in each evaluation session was reported by the child’s parents, and the adverse effects caused by the orthosis were not reported either.
According to the results of this study, in the reduction of spasticity in the intervention phases, improvement in occupational performance and increase in satisfaction with occupational performance may be related to the decrease of muscle tonicity during activities. These results are also consistent with the results obtained in speed and balance.
Conclusion
The design of the orthosis in two sizes for 6 to 12 years reduced the process of customizing this orthosis. The designed dynamic orthosis modulates muscle tonicity and may improve speed, balance, and occupational performance. These improvements can also be observed in the child’s daily activities. Regarding the difference between orthosis with spring and wristband and orthosis without spring and wristband, no difference was found in the functional variables of this study and the period considered.
Limitations of the study include the unavailability of the Lycra material used in other studies in Iran and the use of similar material, as well as the inability to accurately control the time of wearing the orthosis at home and the small number of samples. It is suggested that this orthosis be performed in a larger sample size and with design changes in CP children with higher levels of GMFCS E&R and older ages.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1399.131). Before the start of the study, oral and written informed consent was obtained from the parents of children with CP to participate in the study. The child and the family could withdraw from participating in the research at any stage. The research process had no interference with common child treatments.
Funding
This article was extracted from the PhD dissertation of Sedige Sadat Mirbagheri, approved by Department of Orthotics and Prosthetics, University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Conceptualization: Mahmood Bahramizadeh, Gholamreza Aminian, and Sadigheh Sadat Mirbagheri; Methodology: Gholamreza Aminian, Mohsen Vahedi, Farzam Farhamand, and Sadigheh Sadat Mirbagheri; Research and review: Sadigheh Sadat Mirbaghri; Sources: Sadigheh Sadat Mirbaghri; Data analysis: Farzam Farhamand, Mohsen Vahedi, Hamid Dalvand, and Sadigheh Sadat Mirbagheri; Finance: Sadigheh Sadat Mirbaghri; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Teb and Sanat Company and the sincere cooperation of the company manager, Mohsen Mirmehdi, for implementing the orthosis manufacturing process.
References
- Shevell M. Cerebral palsy to cerebral palsy spectrum disorder: Time for a name change? Neurology. 2019; 92(5):233-5.[DOI:10.1212/WNL.0000000000006747] [PMID]
- Graham HK, Rosenbaum P, Paneth N, Dan B, Lin JP, Damiano DL, et al. Cerebral palsy. Nature Reviews. Disease Primers. 2016; 2:15082. [DOI:10.1038/nrdp.2015.82] [PMID] [PMCID]
- Joghataei M, Kazem M. Assessment the level of community needs in welfare services on the whole country. Tehran: University of Social Welfare and Rehabilitation Sciences; 1990. [Link]
- Ferdjallah M, Harris GF, Smith P, Wertsch JJ. Analysis of postural control synergies during quiet standing in healthy children and children with cerebral palsy. Clinical Biomechanics. 2002; 17(3):203-10. [DOI:10.1016/S0268-0033(01)00121-8] [PMID]
- Moreau NG, Bodkin AW, Bjornson K, Hobbs A, Soileau M, Lahasky K. Effectiveness of rehabilitation interventions to improve gait speed in children with cerebral palsy: Systematic review and meta-analysis. Physical Therapy. 2016; 96(12):1938-54. [DOI:10.2522/ptj.20150401] [PMID] [PMCID]
- Bjornson KF, Zhou C, Stevenson RD, Christakis D. Relation of stride activity and participation in mobility-based life habits among children with cerebral palsy. Archives of Physical Medicine and Rehabilitation. 2014; 95(2):360-8. [DOI:10.1016/j.apmr.2013.10.022] [PMID] [PMCID]
- Rodda JM, Graham HK, Carson L, Galea MP, Wolfe R. Sagittal gait patterns in spastic diplegia. The Journal of Bone and Joint Surgery. British Volume. 2004; 86(2):251-8. [DOI:10.1302/0301-620X.86B2.13878] [PMID]
- Chambers HG. Treatment of functional limitations at the knee in ambulatory children with cerebral palsy. European Journal of Neurology. 2001; 8(Suppl 5):59-74. [DOI:10.1046/j.1468-1331.2001.00039.x] [PMID]
- Steele KM, Demers MS, Schwartz MH, Delp SL. Compressive tibiofemoral force during crouch gait. Gait & Posture. 2012; 35(4):556-60. [DOI:10.1016/j.gaitpost.2011.11.023] [PMID] [PMCID]
- Perry J, Antonelli D, Ford W. Analysis of knee-joint forces during flexed-knee stance. Journal of Bone and Joint Surgery. American Volume. 1975; 57(7):961-7. [DOI:10.2106/00004623-197557070-00014] [PMID]
- Rethlefsen SA, Nguyen DT, Wren TA, Milewski MD, Kay RM. Knee pain and patellofemoral symptoms in patients with cerebral palsy. Journal of Pediatric Orthopedics. 2015; 35(5):519-22. [DOI:10.1097/BPO.0000000000000304] [PMID]
- Bell KJ, Ounpuu S, DeLuca PA, Romness MJ. Natural progression of gait in children with cerebral palsy. Journal of Pediatric Orthopedics. 2002; 22(5):677-82. [DOI:10.1097/01241398-200209000-00020] [PMID]
- Galey SA, Lerner ZF, Bulea TC, Zimbler S, Damiano DL. Effectiveness of surgical and non-surgical management of crouch gait in cerebral palsy: A systematic review. Gait & Posture. 2017; 54:93-105. [DOI:10.1016/j.gaitpost.2017.02.024] [PMID] [PMCID]
- Rogozinski BM, Davids JR, Davis RB 3rd, Jameson GG, Blackhurst DW. The efficacy of the floor-reaction ankle-foot orthosis in children with cerebral palsy. The Journal of Bone and Joint Surgery. American Volume. 2009; 91(10):2440-7. [DOI:10.2106/JBJS.H.00965] [PMID]
- Abd El-Kafy EM. The clinical impact of orthotic correction of lower limb rotational deformities in children with cerebral palsy: A randomized controlled trial. Clinical Rehabilitation. 2014; 28(10):1004-14. [DOI:10.1177/0269215514533710] [PMID]
- Hylton N, Allen C. The development and use of SPIO lycra compression bracing in children with neuromotor deficits. Pediatric Rehabilitation. 1997; 1(2):109-16. [DOI:10.3109/17518429709025853] [PMID]
- Harris SR. A study of a dynamic proximal stability splint in the management of children with cerebral palsy. Developmental Medicine and Child Neurology. 1996; 38(2):181-3. [PMID]
- Rennie DJ, Attfield SF, Morton RE, Polak FJ, Nicholson J. An evaluation of lycra garments in the lower limb using 3-D gait analysis and functional assessment (PEDI). Gait & Posture. 2000; 12(1):1-6. [DOI:10.1016/S0966-6362(00)00066-7] [PMID]
- Flanagan A, Krzak J, Peer M, Johnson P, Urban M. Evaluation of short-term intensive orthotic garment use in children who have cerebral palsy. Pediatric Physical Therapy. 2009; 21(2):201-4.[DOI:10.1097/PEP.0b013e3181a347ab] [PMID]
- Blair E, Ballantyne J, Horsman S, Chauvel P. A study of a dynamic proximal stability splint in the management of children with cerebral palsy. Developmental Medicine and Child Neurology. 1995; 37(6):544-54. [DOI:10.1111/j.1469-8749.1995.tb12041.x] [PMID]
- Gerard A, Toussaint-Thorin M, Mohammad Y, Letellier G, Fritot S, Masson S, et al. Propensix: Pressure garment therapy using compressive dynamic Lycra® sleeve to improve bi-manual performance in unilateral cerebral palsy: A multicenter randomized controlled trial protocol. Trials. 2022; 23(1):117. [DOI:10.1186/s13063-022-06041-1] [PMID] [PMCID]
- Serrao M, Casali C, Ranavolo A, Mari S, Conte C, Chini G, et al. Use of dynamic movement orthoses to improve gait stability and trunk control in ataxic patients. European Journal of Physical and Rehabilitation Medicine. 2017; 53(5):735-43. [Link]
- Watson MJ, Crosby P, Matthews M. An evaluation of the effects of a dynamic lycra orthosis on arm function in a late stage patient with acquired brain injury. Brain Injury. 2007; 21(7):753-61. [DOI:10.1080/02699050701481613] [PMID]
- Attard J, Rithalia S. Physiological effects of lycra® pressure garments on children with cerebral palsy. In: Anand SC, M Kennedy JF, Miraftab M, Rajendran S, editors. edical and Healthcare Textiles: A volume in Woodhead Publishing Series in Textiles. Amsterdam: Elsevier; 2010. [DOI:10.1533/9780857090348.300]
- Indurkar I, Chaudhary NI, Chaudhary S, Sheikh MK, Gawande U. A case study on the use of theratogs® with conventional physiotherapy on a child with cerebral palsy, GMFCS level V. Journal of Survey in Fisheries Sciences. 2023; 10(4S):3082-7. [DOI:10.53555/sfs.v10i4S.1885]
- Civil DA. Design and development of a soft pediatric support garment for ankle-foot orthoses wearers [master thesis]. Newark: University of Delaware; 2019. [Link]
- Stone KA. Dynamic elastomeric fabric orthoses (defo) and physiotherapy after botulinum toxin (BT) in adults with focal spasticity: A feasibility study using mixed methods [doctoral dissertation]. Exeter: University of Exeter; 2014. [Link]
- Bahramizadeh M, Rassafiani M, Aminian G, Rashedi V, Farmani F, Mirbagheri SS. Effect of dynamic elastomeric fabric orthoses on postural control in children with cerebral palsy. Pediatric Physical Therapy. 2015; 27(4):349-54. [DOI:10.1097/PEP.0000000000000171] [PMID]
- Matthews MJ, Watson M, Richardson B. Effects of dynamic elastomeric fabric orthoses on children with cerebral palsy. Prosthetics and Orthotics International. 2009; 33(4):339-47. [DOI:10.3109/03093640903150287] [PMID]
- Knox V. The use of lycra garments in children with cerebral palsy: A report of a descriptive clinical trial. British Journal of Occupational Therapy. 2003; 66(2):71-7. [DOI:10.1177/030802260306600205]
- Kerem M, Livanelioglu A, Topcu M. Effects of Johnstone pressure splints combined with neurodevelopmental therapy on spasticity and cutaneous sensory inputs in spastic cerebral palsy. Developmental Medicine and Child Neurology. 2001; 43(5):307-13. [DOI:10.1017/S0012162201000585] [PMID]
- Gunel MK, Mutlu A, Tarsuslu T, Livanelioglu A. Relationship among the manual ability classification system (MACS), the gross motor function classification system (GMFCS), and the functional status (WeeFIM) in children with spastic cerebral palsy. European Journal of Pediatrics. 2009; 168(4):477-85. [DOI:10.1007/s00431-008-0775-1] [PMID]
- Bloom M, Fischer J, Orme JG. Evaluating practice: Guidelines for the accountable professional. Boston: Pearson/Allyn and Bacon; 2006. [Link]
- Law MC, Canadian Association of Occupational Therapists. Canadian occupational performance measure. Ottawa: Canadian Association of Occupational Therapists; 1998. [Link]
- Hosseini M, Mirbagheri SS, Bahramizadeh M, Rassaffiani M, Torkeman R. [The effect of neoprene dynamic orthosis on postural control in children with cerebral palsy (pilot study) (Persian)]. Journal of Modern Rehabilitation. 2015; 9(2):69-76. [Link]
- Christy JB, Chapman CG, Murphy P. The effect of intense physical therapy for children with cerebral palsy. Journal of Pediatric Rehabilitation Medicine. 2012; 5(3):159-70. [DOI:10.3233/PRM-2012-0208] [PMID]
- Béghin L, Mohammad Y, Fritot S, Letellier G, Masson S, Zagamé Y, et al. Safety and adherence of pressure garment therapy in children with upper limb unilateral cerebral palsy. Results from a randomized clinical trial ancillary analysis. Frontiers in Pediatrics. 2023; 11:1043350. [DOI:10.3389/fped.2023.1043350] [PMID] [PMCID]
Type of Study: Original |
Subject:
Orthotics & Prosthetics
Received: 24/06/2023 | Accepted: 23/10/2023 | Published: 1/04/2024
Received: 24/06/2023 | Accepted: 23/10/2023 | Published: 1/04/2024
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |