Volume 24, Issue 2 (Summer 2023)
jrehab 2023, 24(2): 150-171 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Poursaeid Z, Mohsenpour M, Ghasisin L. The Experiences of the Families of People With Aphasia About the Barriers and Facilitators of Receiving Speech Therapy Services in Iran. jrehab 2023; 24 (2) :150-171
URL: http://rehabilitationj.uswr.ac.ir/article-1-3201-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3201-en.html
1- Department of Speech Therapy, Student Research Committee, School of Rehabilitation, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Speech Therapy, School of Rehabilitation, Isfahan University of Medical Sciences, Isfahan, Iran. ,ghasisin@rehab.mui.ac.ir, ghasisin@gmail.com
2- Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Speech Therapy, School of Rehabilitation, Isfahan University of Medical Sciences, Isfahan, Iran. ,
Full-Text [PDF 2464 kb]
(1538 Downloads)
| Abstract (HTML) (5039 Views)
Full-Text: (2383 Views)
Introduction
Aphasia is an acquired language disorder affecting all language representations and aspects of a patient’s life. Stroke is the most common cause of this disorder [1, 2, 3].
Aphasia has negative effects that will remain in a person’s life for a long time and affects the family of these people with consequences, such as economic problems and social isolation [4-8]. Treatment is effective in the recovery of people with aphasia. Qualified speech therapists can treat these people to a great extent [8].
The increasing age of the world population raises the incidence of stroke, and applying healthier ways of life saves more people from stroke. However, studies have shown that the treatment provided to people with aphasia differs from what the evidence suggests [8, 9, 10].
Shrubsol’s research showed that 75% of people with aphasia, who were suitable candidates for treatment, did not receive treatment during hospitalization. Wressle’s study showed that although, according to research, the participation of a person with aphasia in the goal-setting process of rehabilitation positively affects his compliance with treatment, people with stroke often do not participate in the goal-setting process [13, 14, 15].
Emerging evidence examines the barriers and facilitators of rehabilitating people with aphasia. The factors affecting treatment are different in various countries. Many speech therapists have mentioned time and place limitations as barriers to providing language therapy to these people. Studies have shown that some speech therapists have little self-confidence in advising patients, and resources appropriate to the country’s culture and language are unavailable. These cases are other barriers mentioned in studies [16, 17, 18].
In addition to barriers, studies have also mentioned facilitators of effective treatment. As a framework for assessing a person with aphasia, the International Classification of Functioning, Disability, and Health (ICF) facilitates effective therapy for people with aphasia [20].
In Iran, no information exists about the barriers and facilitators of providing speech therapy to people with aphasia. hence, it takes a long time to maximize the ability of communication in these people.
The incidence of stroke in Iran is estimated to be higher than in Western countries [18, 21]. Although stroke can happen at any age, more than 70% of strokes occur in people aged 65 years and older [22, 23]. Therefore, the incidence of stroke and aphasia is increasing in Iran.
To improve services for people with disabilities in society, it is necessary to know about the current status of services that are usually provided to plan for more effective treatments in the future [24].
Identifying the barriers and facilitators of providing effective speech therapy services to people with aphasia will help us to provide speech therapy services with maximum quality. The family members of these people are among the groups with valuable information about the disability status of people with aphasia [1]. However, no study has examined speech therapy services from the perspective of these individuals. This study was conducted to determine the factors affecting speech therapy services according to the lived experience of the families of people with aphasia in Iran.
Materials and Methods
This study was conducted with a qualitative content analysis method. To collect information, semi-structured individual interviews with open questions were used so the participants could freely express their experiences [25]. The participants were the families of people with aphasia. Purposive sampling was used in this study because it is the best method in qualitative research for a deep understanding of an experience [26]. Based on the moral consent form and the experience of participating in speech therapy sessions with the patient, the families who expressed their consent to participate in the study were selected. To reach data saturation, interviews were conducted with 12 families.
Study procedure
This study was approved by the Isfahan University of Medical Sciences and received the code of ethics. To start the sampling, we identified centers providing speech therapy to people with aphasia. Then the officials were informed of the study objectives; if satisfied, they were asked to talk to the families of people with aphasia and obtain their initial consent to participate. After this stage, the researchers contacted the families and carefully explained the study’s objectives. The ethical consent form was sent online to the families who agreed to participate in the study, and they were asked to return it after signing.
Due to the spread of COVID-19, the interviews were conducted online. Interviews were conducted by voice calls via WhatsApp or phone calls. Before the interview, the procedure was explained to the interviewees, and they were assured that the interview was completely private and the results would not affect the patient’s treatment process. The interview started with questions about the injury’s onset time and the problems it caused in the daily life of the patient and the family. Then it continued about the barriers and facilitators of receiving rehabilitation services. The duration of interviews with families was 25 minutes on average. After conducting the interview, the interviews were transcribed then sent to the families to confirm the accuracy of the information. Then, the Burnard approach was used to analyze the interview.
Data analysis
The obtained data were analyzed using the conventional content analysis method with Burnard’s approach [27]. After the interview, the critical points were noted, and the interviews were transcribed. Two people from the research team read the text of the interviews separately. They extracted meaning units, then summarized and categorized them according to their similarity. Afterwards, they named each category, and finally, a list of categories and subcategories were prepared. Next, the classes were compared and discussed. Then, the list agreed upon by both researchers was recorded. During this process, the original data were referred to several times, and the classes were checked regularly to ensure that the results represented the content of the data. OneNote 2007 software was used to organize classes.
Validity
To strengthen dependability, the research team was divided into two groups, and all the interviews were analyzed separately, and then the results of the two groups were compared and summarized. Finally, the necessary changes were made. Also, to strengthen the credibility of the data, after analyzing the interviews, the results were sent to two interviewees, and they confirmed the accuracy of the information.
Results
Study participants
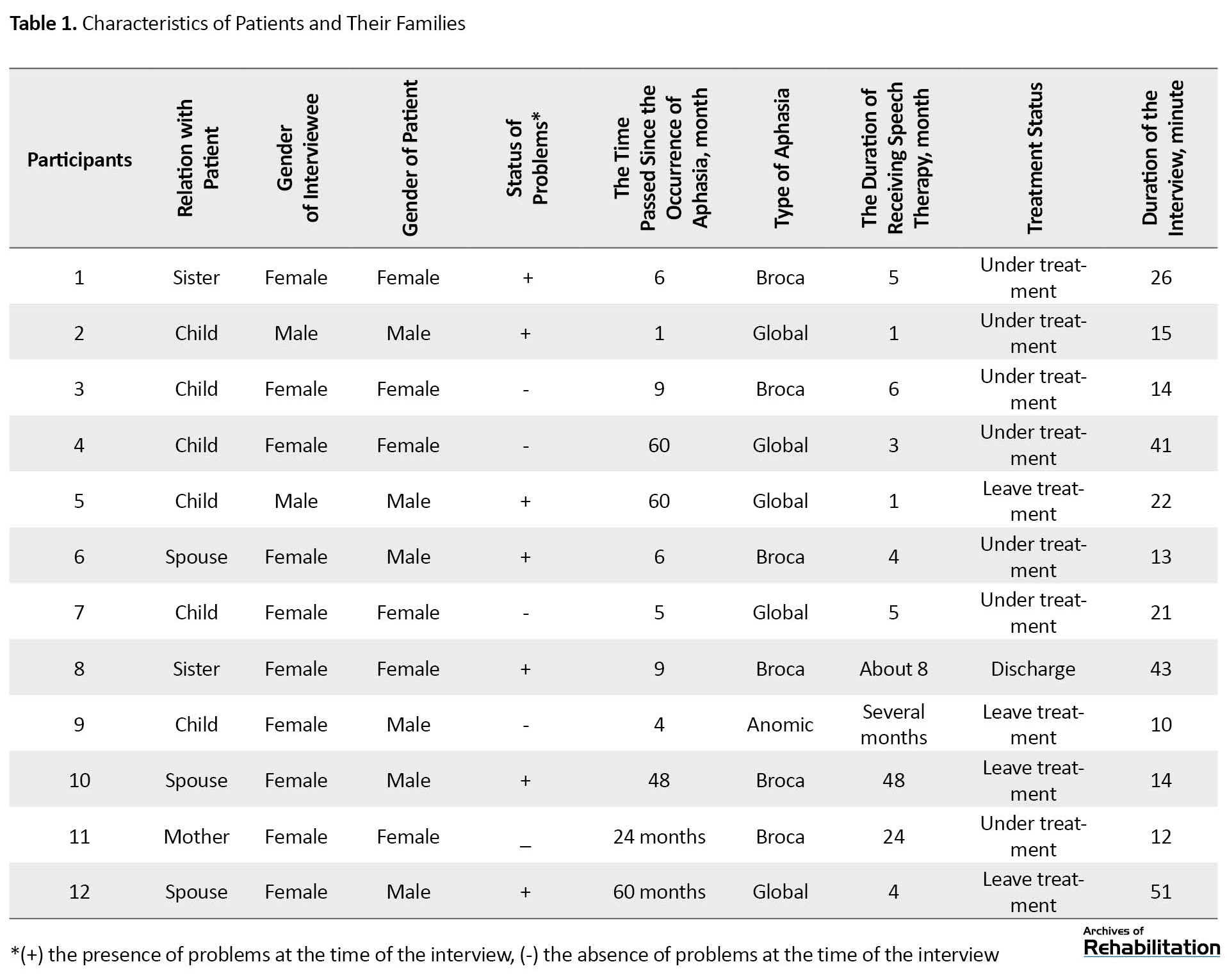
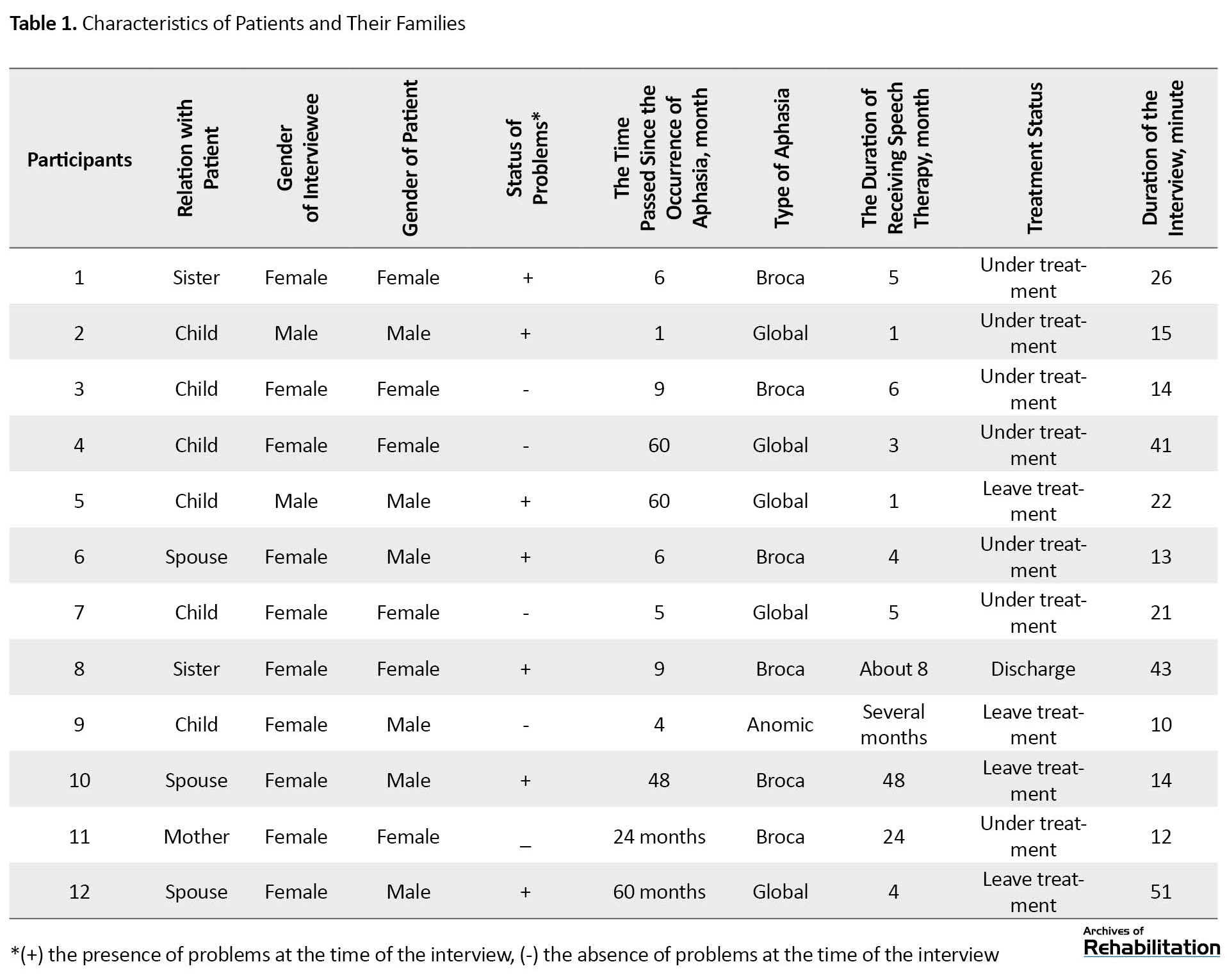
In this study, 12 people were interviewed. Table 1 presents the characteristics of these people.
The data analysis results from the interviews are presented in two sections: barriers and facilitators of speech therapy services. Participants’ quotes will also be written to present the topic with the participants’ words.
Barriers
Based on the analysis of the collected data, 5 classes and 12 subclasses were extracted. Table 2 shows the title of extracted classes and subclasses.

First class: effective factors on clients’ attendance in speech therapy sessions
Some families faced problems, including the high cost of treatment, the problems of commuting to the treatment place, and the limited access to the speech therapist. The spread of COVID-19 has also affected the patient’s attendance in treatment sessions by changing the way of receiving speech therapy services.
“His medicines, his special diet, physiotherapy, speech therapy... the cost was very expensive for me.” (Participant 12)
Second class: patient
In this class, the high severity of the injury is an barriers to treatment due to the negative impact on the morale of the people around and the patient’s non-cooperation to follow up the speech therapy sessions.
We came to several meetings, and then my father refused to come. (Participant 9)
Third class: treatment place
“The families were dissatisfied because it was impossible to set the meeting time according to their request, and the tools of the treatment center were not suitable for the treatment of aphasia.”
“Also, the very depressing atmosphere dominated that room; if that atmosphere were more spacious, maybe the person undergoing treatment would be more encouraged to come and sit there.” (Participant 5)
Fourth class: family
In this category, it is stated that the insufficient time of the families and their non-attendance in the treatment sessions makes them unable to accompany the patient to the treatment sessions.
“Yes, yes, we will do it. Of course, some days more and some days less. Our work is a bit too much.” (Participant 6)
Fifth class: speech therapist
In this class, the interviewees were dissatisfied with the speech therapist weakness in treating adult clients. They stated that they did not discuss their dissatisfaction with the treatment because they did not have a good relationship with the therapist.
“When we showed pictures of things and these things, he felt that these belonged to children. Then he didn’t cooperate anymore.” (Participant 12)
Facilitators
Facilitator of receiving speech therapy services are placed in 5 classes and 13 subclasses (Table 2).
First class: effective factors on clients’ attendance in speech therapy sessions
A reasonable cost of treatment facilitates receiving services. Also, doctors and internet search help the family to refer to speech therapy more easily.
“They were in the hospital for a week, and then their doctor told them to go to speech therapy immediately” (Participant 10)
Second class: patient
According to interviewees, the facilitators of the treatment were the young age of the patient, the low severity of the injury, and the patient’s cooperation to participate in the speech therapy sessions.
“Because she was young, she hoped to finally return to this life.” (Participant 8)
Third class: treatment place
The possibility of adjusting the frequency and duration of speech therapy sessions according to the family’s request and access to suitable facilities for treating aphasia have attracted the family’s satisfaction.
“My mother and I are looking for any means that will make my mother improve more.” (Participant 4)
Fourth class: family
The families stated that their awareness of the importance of practice and encouraging the patient to continue the sessions facilitated receiving these services.
“Yes, I told my mother, you couldn’t even say letters at first. You have progressed extremely. (Participant 3)
Fifth class: speech therapist
The speech therapist’s expression of the necessary recommendations and his high skill in treating the patient has facilitated receiving speech therapy services.
“It’s not just about working with the patient. You have to give him hope so that he can return to his original state.” (Participant 11)
Discussion
This study was conducted to investigate the experience of the families of people with aphasia on the factors affecting speech therapy services for these people.
Barriers to receiving speech therapy services
First class: effective factors on clients’ attendance in speech therapy sessions
According to ICF, the factors of this class are included in the environmental factors section. One of the barriersmentioned in the present study was that the families had not received the necessary recommendations in the hospital to refer to speech therapy. Similarly, in Hinckley’s study in 2013, people with aphasia and their caregivers stated that doctors have limited knowledge of aphasia and its treatment [30].
The last subclass examined the impact of the COVID-19 outbreak. Pak and Kong, in one of the studies, mentioned that due to the disease, it was necessary to change the method of providing treatment from face-to-face to online [31].
Second class: patient
The first subclass is placed in the section on body structure and function, and the second in the section on individual factors of the ICF. Of course, if the patient’s non-cooperation is caused by brain damage, it will again be placed in the structure and function of the body.
In this class, the high severity of the injury is considered to prevent treatment. In another study, several problems in expressive and understanding abilities prevented patients from participating in society [32].
Third class: treatment place
The factors of this class are included in the environmental factors of ICF. The impossibility of determining the duration and frequency of sessions according to the patient’s conditions was a obstacle to receiving speech therapy services. It has also been seen in studies that the intensity of the treatment and the duration of each session are less than what is suggested by the evidence [33].
Fourth class: family
The barriers of this class are included in the category of ICF environmental factors. The interviewees stated that the limitation of family free time and busyness hinder the treatment. In the study by Hu et al., families of people with aphasia said that new financial issues and increased responsibilities were among the changes they experienced [5].
Fifth class: speech therapist
The factors of this class are included in the category of environmental factors of ICF. One of the barriers mentioned in this subclass was that the speech therapist did not explain the purpose of the exercises to the family. In another study, family members reported that despite the need to receive information, they are not given enough information [5].
Facilitators of receiving speech therapy services
First class: effective factors on clients’ attendance in speech therapy sessions
The factors of this class are included in the section on environmental factors of the ICF. Families considered the reasonable cost of treatment to facilitate receiving speech therapy services. One of the reported facilitators was the different speech therapy costs proportional to the individual’s income [28].
Second class: patient
The first subclass is placed in the ICF category of individual factors. The second subclass is part of the structure and body function of the ICF. In the third subclass, if the patient’s high cooperation is due to his low injury, it can be placed in the body structure and function section of the ICF, and if the mood causes increased collaboration, it should be placed in the patient’s factors. The families considered the young age of the patient and his high intelligence to be helpful factors in the treatment. In a study conducted in Singapore, participants stated that older people are less likely to regain their communication ability [18].
Third class: treatment place
The characteristics of this subclass are included in the environmental factors of the ICF. In the reviewed studies, there are factors related to the treatment place which hinder the treatment. Perhaps the reason for this difference can be interpreted as the existing facilities for treating aphasia in other countries are unfavorable; therefore, their effect is mentioned as an obstacle.
Fourth class: family
The families’ role is part of the ICF environmental factors. According to the interviewees, the patient’s support from the family is a facilitator for the treatment. In Le hdorez’s study, people with aphasia also mentioned the daily support of family members as a facilitator [32].
The second subclass was the proper behavior of the family with the patient. Other studies have mentioned how the family communicates with the patient. However, the points mentioned in the present study differ from previous studies. In the present study, the families expressed some points about maintaining the patient’s morale. While previous studies showed that behaviors, such as paying close attention when listening to a person with aphasia and being patient when communicating with him, facilitate communication with the patient [17, 28, 32, 34], it can be concluded that the participants of the present study did not know how to communicate with the patient. The results of an investigation by Howe showed that the families of people with aphasia were interested in receiving training on the best way to communicate with the patient [5]. Therefore, comparing the results of the present study with previous studies emphasizes the importance of educating families about how to communicate with the patient.
Fifth class: speech therapist
These factors are included in the category of ICF environmental factors. The greater skill and knowledge of therapists in the field of aphasia is a positive factor in the treatment process. Previous studies showed that one of the reasons for clients’ satisfaction with the therapist is his skill [17].
In addition to the mentioned cases, proper communication between the therapist, client, and family helps progress the treatment. Hersh emphasized the importance of establishing a strong and friendly relationship before setting goals and evaluations [35]. Other studies have mentioned the respectful behavior of professionals, good communication between the rehabilitation team, the person with aphasia, and family members, and communication with the therapist [17, 36].
Conclusion
This study examined the barriers and facilitators of receiving speech therapy services from the perspective of families of people with aphasia. The factors related to the client’s presence in the speech therapy session, the patient, the treatment place, the family, and the speech therapist are the classes that can act as a barrier or facilitator.
Considering that the studies related to the quality of receiving speech therapy services for people with aphasia have not been conducted in Iran, by examining the results of this study, necessary planning can be done to reduce barriers and strengthen facilitators. In this way, the quality of life of people with aphasia and their families will increase.
Because no information is available about the quality of speech therapy services in the country, it is suggested that the quality of these services be reviewed and compared.
Limitations and Obstacles
Because of COVID-19, patients were referred to speech therapy clinics less frequently; therefore, it was difficult to access the families of these people. Another limitation was the possibility of people’s bias in providing information.
Ethical Considerations
Compliance with ethical guidelines
The participants were informed about the study objectives and methods and signed a written consent form. They were assured of the confidentiality of their information and were free to leave at any time. Ethical approval was obtained from Isfahan University of Medical Sciences (Code: IR.MUI.RESEARCH.REC. 2019.503).
Funding
This study was extracted from the Master thesis of Zahra Poursaeid. The study was funded by Isfahan University of Medical Sciences.
Authors' contributions
Conceptualization, data analysis, writing, editing & review: Leila Ghasisin, Mohaddeseh Mohsenpour, and Zahra Poursaeid; Data collection: Zahra Poursaeid; budget acquisition, supervision, and project administration: Leila Ghasisin.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Vice-Chancellor for Research and Technology of Isfahan University of Medical Sciences and the participations for their support and cooperation.
References
Aphasia is an acquired language disorder affecting all language representations and aspects of a patient’s life. Stroke is the most common cause of this disorder [1, 2, 3].
Aphasia has negative effects that will remain in a person’s life for a long time and affects the family of these people with consequences, such as economic problems and social isolation [4-8]. Treatment is effective in the recovery of people with aphasia. Qualified speech therapists can treat these people to a great extent [8].
The increasing age of the world population raises the incidence of stroke, and applying healthier ways of life saves more people from stroke. However, studies have shown that the treatment provided to people with aphasia differs from what the evidence suggests [8, 9, 10].
Shrubsol’s research showed that 75% of people with aphasia, who were suitable candidates for treatment, did not receive treatment during hospitalization. Wressle’s study showed that although, according to research, the participation of a person with aphasia in the goal-setting process of rehabilitation positively affects his compliance with treatment, people with stroke often do not participate in the goal-setting process [13, 14, 15].
Emerging evidence examines the barriers and facilitators of rehabilitating people with aphasia. The factors affecting treatment are different in various countries. Many speech therapists have mentioned time and place limitations as barriers to providing language therapy to these people. Studies have shown that some speech therapists have little self-confidence in advising patients, and resources appropriate to the country’s culture and language are unavailable. These cases are other barriers mentioned in studies [16, 17, 18].
In addition to barriers, studies have also mentioned facilitators of effective treatment. As a framework for assessing a person with aphasia, the International Classification of Functioning, Disability, and Health (ICF) facilitates effective therapy for people with aphasia [20].
In Iran, no information exists about the barriers and facilitators of providing speech therapy to people with aphasia. hence, it takes a long time to maximize the ability of communication in these people.
The incidence of stroke in Iran is estimated to be higher than in Western countries [18, 21]. Although stroke can happen at any age, more than 70% of strokes occur in people aged 65 years and older [22, 23]. Therefore, the incidence of stroke and aphasia is increasing in Iran.
To improve services for people with disabilities in society, it is necessary to know about the current status of services that are usually provided to plan for more effective treatments in the future [24].
Identifying the barriers and facilitators of providing effective speech therapy services to people with aphasia will help us to provide speech therapy services with maximum quality. The family members of these people are among the groups with valuable information about the disability status of people with aphasia [1]. However, no study has examined speech therapy services from the perspective of these individuals. This study was conducted to determine the factors affecting speech therapy services according to the lived experience of the families of people with aphasia in Iran.
Materials and Methods
This study was conducted with a qualitative content analysis method. To collect information, semi-structured individual interviews with open questions were used so the participants could freely express their experiences [25]. The participants were the families of people with aphasia. Purposive sampling was used in this study because it is the best method in qualitative research for a deep understanding of an experience [26]. Based on the moral consent form and the experience of participating in speech therapy sessions with the patient, the families who expressed their consent to participate in the study were selected. To reach data saturation, interviews were conducted with 12 families.
Study procedure
This study was approved by the Isfahan University of Medical Sciences and received the code of ethics. To start the sampling, we identified centers providing speech therapy to people with aphasia. Then the officials were informed of the study objectives; if satisfied, they were asked to talk to the families of people with aphasia and obtain their initial consent to participate. After this stage, the researchers contacted the families and carefully explained the study’s objectives. The ethical consent form was sent online to the families who agreed to participate in the study, and they were asked to return it after signing.
Due to the spread of COVID-19, the interviews were conducted online. Interviews were conducted by voice calls via WhatsApp or phone calls. Before the interview, the procedure was explained to the interviewees, and they were assured that the interview was completely private and the results would not affect the patient’s treatment process. The interview started with questions about the injury’s onset time and the problems it caused in the daily life of the patient and the family. Then it continued about the barriers and facilitators of receiving rehabilitation services. The duration of interviews with families was 25 minutes on average. After conducting the interview, the interviews were transcribed then sent to the families to confirm the accuracy of the information. Then, the Burnard approach was used to analyze the interview.
Data analysis
The obtained data were analyzed using the conventional content analysis method with Burnard’s approach [27]. After the interview, the critical points were noted, and the interviews were transcribed. Two people from the research team read the text of the interviews separately. They extracted meaning units, then summarized and categorized them according to their similarity. Afterwards, they named each category, and finally, a list of categories and subcategories were prepared. Next, the classes were compared and discussed. Then, the list agreed upon by both researchers was recorded. During this process, the original data were referred to several times, and the classes were checked regularly to ensure that the results represented the content of the data. OneNote 2007 software was used to organize classes.
Validity
To strengthen dependability, the research team was divided into two groups, and all the interviews were analyzed separately, and then the results of the two groups were compared and summarized. Finally, the necessary changes were made. Also, to strengthen the credibility of the data, after analyzing the interviews, the results were sent to two interviewees, and they confirmed the accuracy of the information.
Results
Study participants
In this study, 12 people were interviewed. Table 1 presents the characteristics of these people.
The data analysis results from the interviews are presented in two sections: barriers and facilitators of speech therapy services. Participants’ quotes will also be written to present the topic with the participants’ words.
Barriers
Based on the analysis of the collected data, 5 classes and 12 subclasses were extracted. Table 2 shows the title of extracted classes and subclasses.

First class: effective factors on clients’ attendance in speech therapy sessions
Some families faced problems, including the high cost of treatment, the problems of commuting to the treatment place, and the limited access to the speech therapist. The spread of COVID-19 has also affected the patient’s attendance in treatment sessions by changing the way of receiving speech therapy services.
“His medicines, his special diet, physiotherapy, speech therapy... the cost was very expensive for me.” (Participant 12)
Second class: patient
In this class, the high severity of the injury is an barriers to treatment due to the negative impact on the morale of the people around and the patient’s non-cooperation to follow up the speech therapy sessions.
We came to several meetings, and then my father refused to come. (Participant 9)
Third class: treatment place
“The families were dissatisfied because it was impossible to set the meeting time according to their request, and the tools of the treatment center were not suitable for the treatment of aphasia.”
“Also, the very depressing atmosphere dominated that room; if that atmosphere were more spacious, maybe the person undergoing treatment would be more encouraged to come and sit there.” (Participant 5)
Fourth class: family
In this category, it is stated that the insufficient time of the families and their non-attendance in the treatment sessions makes them unable to accompany the patient to the treatment sessions.
“Yes, yes, we will do it. Of course, some days more and some days less. Our work is a bit too much.” (Participant 6)
Fifth class: speech therapist
In this class, the interviewees were dissatisfied with the speech therapist weakness in treating adult clients. They stated that they did not discuss their dissatisfaction with the treatment because they did not have a good relationship with the therapist.
“When we showed pictures of things and these things, he felt that these belonged to children. Then he didn’t cooperate anymore.” (Participant 12)
Facilitators
Facilitator of receiving speech therapy services are placed in 5 classes and 13 subclasses (Table 2).
First class: effective factors on clients’ attendance in speech therapy sessions
A reasonable cost of treatment facilitates receiving services. Also, doctors and internet search help the family to refer to speech therapy more easily.
“They were in the hospital for a week, and then their doctor told them to go to speech therapy immediately” (Participant 10)
Second class: patient
According to interviewees, the facilitators of the treatment were the young age of the patient, the low severity of the injury, and the patient’s cooperation to participate in the speech therapy sessions.
“Because she was young, she hoped to finally return to this life.” (Participant 8)
Third class: treatment place
The possibility of adjusting the frequency and duration of speech therapy sessions according to the family’s request and access to suitable facilities for treating aphasia have attracted the family’s satisfaction.
“My mother and I are looking for any means that will make my mother improve more.” (Participant 4)
Fourth class: family
The families stated that their awareness of the importance of practice and encouraging the patient to continue the sessions facilitated receiving these services.
“Yes, I told my mother, you couldn’t even say letters at first. You have progressed extremely. (Participant 3)
Fifth class: speech therapist
The speech therapist’s expression of the necessary recommendations and his high skill in treating the patient has facilitated receiving speech therapy services.
“It’s not just about working with the patient. You have to give him hope so that he can return to his original state.” (Participant 11)
Discussion
This study was conducted to investigate the experience of the families of people with aphasia on the factors affecting speech therapy services for these people.
Barriers to receiving speech therapy services
First class: effective factors on clients’ attendance in speech therapy sessions
According to ICF, the factors of this class are included in the environmental factors section. One of the barriersmentioned in the present study was that the families had not received the necessary recommendations in the hospital to refer to speech therapy. Similarly, in Hinckley’s study in 2013, people with aphasia and their caregivers stated that doctors have limited knowledge of aphasia and its treatment [30].
The last subclass examined the impact of the COVID-19 outbreak. Pak and Kong, in one of the studies, mentioned that due to the disease, it was necessary to change the method of providing treatment from face-to-face to online [31].
Second class: patient
The first subclass is placed in the section on body structure and function, and the second in the section on individual factors of the ICF. Of course, if the patient’s non-cooperation is caused by brain damage, it will again be placed in the structure and function of the body.
In this class, the high severity of the injury is considered to prevent treatment. In another study, several problems in expressive and understanding abilities prevented patients from participating in society [32].
Third class: treatment place
The factors of this class are included in the environmental factors of ICF. The impossibility of determining the duration and frequency of sessions according to the patient’s conditions was a obstacle to receiving speech therapy services. It has also been seen in studies that the intensity of the treatment and the duration of each session are less than what is suggested by the evidence [33].
Fourth class: family
The barriers of this class are included in the category of ICF environmental factors. The interviewees stated that the limitation of family free time and busyness hinder the treatment. In the study by Hu et al., families of people with aphasia said that new financial issues and increased responsibilities were among the changes they experienced [5].
Fifth class: speech therapist
The factors of this class are included in the category of environmental factors of ICF. One of the barriers mentioned in this subclass was that the speech therapist did not explain the purpose of the exercises to the family. In another study, family members reported that despite the need to receive information, they are not given enough information [5].
Facilitators of receiving speech therapy services
First class: effective factors on clients’ attendance in speech therapy sessions
The factors of this class are included in the section on environmental factors of the ICF. Families considered the reasonable cost of treatment to facilitate receiving speech therapy services. One of the reported facilitators was the different speech therapy costs proportional to the individual’s income [28].
Second class: patient
The first subclass is placed in the ICF category of individual factors. The second subclass is part of the structure and body function of the ICF. In the third subclass, if the patient’s high cooperation is due to his low injury, it can be placed in the body structure and function section of the ICF, and if the mood causes increased collaboration, it should be placed in the patient’s factors. The families considered the young age of the patient and his high intelligence to be helpful factors in the treatment. In a study conducted in Singapore, participants stated that older people are less likely to regain their communication ability [18].
Third class: treatment place
The characteristics of this subclass are included in the environmental factors of the ICF. In the reviewed studies, there are factors related to the treatment place which hinder the treatment. Perhaps the reason for this difference can be interpreted as the existing facilities for treating aphasia in other countries are unfavorable; therefore, their effect is mentioned as an obstacle.
Fourth class: family
The families’ role is part of the ICF environmental factors. According to the interviewees, the patient’s support from the family is a facilitator for the treatment. In Le hdorez’s study, people with aphasia also mentioned the daily support of family members as a facilitator [32].
The second subclass was the proper behavior of the family with the patient. Other studies have mentioned how the family communicates with the patient. However, the points mentioned in the present study differ from previous studies. In the present study, the families expressed some points about maintaining the patient’s morale. While previous studies showed that behaviors, such as paying close attention when listening to a person with aphasia and being patient when communicating with him, facilitate communication with the patient [17, 28, 32, 34], it can be concluded that the participants of the present study did not know how to communicate with the patient. The results of an investigation by Howe showed that the families of people with aphasia were interested in receiving training on the best way to communicate with the patient [5]. Therefore, comparing the results of the present study with previous studies emphasizes the importance of educating families about how to communicate with the patient.
Fifth class: speech therapist
These factors are included in the category of ICF environmental factors. The greater skill and knowledge of therapists in the field of aphasia is a positive factor in the treatment process. Previous studies showed that one of the reasons for clients’ satisfaction with the therapist is his skill [17].
In addition to the mentioned cases, proper communication between the therapist, client, and family helps progress the treatment. Hersh emphasized the importance of establishing a strong and friendly relationship before setting goals and evaluations [35]. Other studies have mentioned the respectful behavior of professionals, good communication between the rehabilitation team, the person with aphasia, and family members, and communication with the therapist [17, 36].
Conclusion
This study examined the barriers and facilitators of receiving speech therapy services from the perspective of families of people with aphasia. The factors related to the client’s presence in the speech therapy session, the patient, the treatment place, the family, and the speech therapist are the classes that can act as a barrier or facilitator.
Considering that the studies related to the quality of receiving speech therapy services for people with aphasia have not been conducted in Iran, by examining the results of this study, necessary planning can be done to reduce barriers and strengthen facilitators. In this way, the quality of life of people with aphasia and their families will increase.
Because no information is available about the quality of speech therapy services in the country, it is suggested that the quality of these services be reviewed and compared.
Limitations and Obstacles
Because of COVID-19, patients were referred to speech therapy clinics less frequently; therefore, it was difficult to access the families of these people. Another limitation was the possibility of people’s bias in providing information.
Ethical Considerations
Compliance with ethical guidelines
The participants were informed about the study objectives and methods and signed a written consent form. They were assured of the confidentiality of their information and were free to leave at any time. Ethical approval was obtained from Isfahan University of Medical Sciences (Code: IR.MUI.RESEARCH.REC. 2019.503).
Funding
This study was extracted from the Master thesis of Zahra Poursaeid. The study was funded by Isfahan University of Medical Sciences.
Authors' contributions
Conceptualization, data analysis, writing, editing & review: Leila Ghasisin, Mohaddeseh Mohsenpour, and Zahra Poursaeid; Data collection: Zahra Poursaeid; budget acquisition, supervision, and project administration: Leila Ghasisin.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Vice-Chancellor for Research and Technology of Isfahan University of Medical Sciences and the participations for their support and cooperation.
References
- Le Dorze G, Signori FH. Needs, barriers and facilitators experienced by spouses of people with aphasia. Disability and Rehabilitation. 2010; 32(13):1073-87. [DOI:10.3109/09638280903374121] [PMID]
- Berg K, Isaksen J, Wallace SJ, Cruice M, Simmons-Mackie N, Worrall L. Establishing consensus on a definition of aphasia: An e-Delphi study of international aphasia researchers. Aphasiology. 2022; 36(4):385-400. [DOI:10.1080/02687038.2020.1852003]
- Simmons-Mackie N, Kagan A. Application of the ICF in aphasia. Seminars in Speech and Language. 2007; 28(4):244-53. [DOI:10.1055/s-2007-986521] [PMID]
- Brown K, Worrall L, Davidson B, Howe T. Snapshots of success: An insider perspective on living successfully with aphasia. Aphasiology. 2010; 24(10):1267-95. [DOI:10.1080/02687031003755429]
- Howe T, Davidson B, Worrall L, Hersh D, Ferguson A, Sherratt S, et al. ‘You needed to rehab… families as well’: Family members’ own goals for aphasia rehabilitation. International Journal of Language & Communication Disorders. 2012; 47(5):511-21. [DOI:10.1111/j.1460-6984.2012.00159.x] [PMID]
- Sherratt S, Worrall L, Pearson C, Howe T, Hersh D, Davidson B. “Well it has to be language-related”: Speech-language pathologists’ goals for people with aphasia and their families. International Journal of Speech-Language Pathology. 2011; 13(4):317-28. [DOI:10.3109/17549507.2011.584632] [PMID]
- Bethoux F, Calmels P, Gautheron V, Minaire P. Quality of life of the spouses of stroke patients: A preliminary study. International Journal of Rehabilitation Research. 1996; 19(4):291-300. [DOI:10.1097/00004356-199612000-00001] [PMID]
- Holland AL, Fromm DS, DeRuyter F, Stein M. Treatment efficacy: Aphasia. Journal of Speech, Language, and Hearing Research. 1996; 39(5):S27-S36. [DOI:10.1044/jshr.3905.s27] [PMID]
- Godecke E, Armstrong EA, Rai T, Middleton S, Ciccone N, Whitworth A, et al. A randomized controlled trial of very early rehabilitation in speech after stroke. International Journal of Stroke. 2016; 11(5):586-92. [DOI:10.1177/1747493016641116] [PMID]
- Code C, Petheram B. Delivering for aphasia. International Journal of Speech-Language Pathology. 2011; 13(1):3-10. [DOI:10.3109/17549507.2010.520090] [PMID]
- Hinckley JJ. Finding messages in bottles: Living successfully with stroke and aphasia. Topics in Stroke Rehabilitation. 2006; 13(1):25-36. [DOI:10.1310/FLJ3-04DQ-MG8W-89EU] [PMID]
- Greener J, Langhorne P. Systematic reviews in rehabilitation for stroke: Issues and approaches to addressing them. Clinical Rehabilitation. 2002;16(1):69-74. [DOI:10.1191/0269215502cr469oa] [PMID]
- Shrubsole K, Worrall L, Power E, O’Connor DA. Barriers and facilitators to meeting aphasia guideline recommendations: what factors influence speech pathologists’ practice? Disability and Rehabilitation. 2019; 41(13):1596-607. [DOI:10.1080/09638288.2018.1432706] [PMID]
- Worrall L, Sherratt S, Rogers P, Howe T, Hersh D, Ferguson A, et al. What people with aphasia want: Their goals according to the ICF. Aphasiology. 2011; 25(3):309-22. [DOI:10.1080/02687038.2010.508530]
- Rohde A, Townley-O’Neill K, Trendall K, Worrall L, Cornwell P. A comparison of client and therapist goals for people with aphasia: A qualitative exploratory study. Aphasiology. 2012; 26(10):1298-315. [DOI:10.1080/02687038.2012.706799]
- Young L, Shrubsole K, Worrall L, Power E. Factors that influence Australian speech-language pathologists’ self-reported uptake of aphasia rehabilitation recommendations from clinical practice guidelines. Aphasiology. 2018; 32(6):646-65. [DOI:10.1080/02687038.2018.1443201]
- Chow C. Barriers and facilitators that affect access to an outpatient speech-language therapy aphasia clinic [MSc Thesis]. Canterbury: University of Canterbury; 2015. [Link]
- Guo YE, Togher L, Power E. Speech pathology services for people with aphasia: what is the current practice in Singapore? Disability and Rehabilitation. 2014; 36(8):691-704. [DOI:10.3109/09638288.2013.804597] [PMID]
- Sekhon JK, Oates J, Kneebone I, Rose M. Counselling training for speech-language therapists working with people affected by post-stroke aphasia: A systematic review. International Journal of Language & Communication Disorders. 2019; 54(3):321-46. [DOI:10.1111/1460-6984.12455] [PMID]
- Verna A, Davidson B, Rose T. Speech-language pathology services for people with aphasia: A survey of current practice in Australia. International Journal of Speech-Language Pathology. 2009; 11(3):191-205. [DOI:10.1080/17549500902726059]
- Imani A, Dastgiri S, Azizi A. [Population aging and disease burden (Persian)]. Depiction of Health. 2016; 6(2):54-61. [Link]
- Ellis C, Urban S. Age and aphasia: A review of presence, type, recovery and clinical outcomes. Topics in Stroke Rehabilitation. 2016; 23(6):430-9. [DOI:10.1080/10749357.2016.1150412] [PMID]
- Kelly-Hayes M. Influence of age and health behaviors on stroke risk: Lessons from longitudinal studies. Journal of the American Geriatrics Society. 2010; 58 Suppl 2(Suppl 2):S325-8. [DOI:10.1111/j.1532-5415.2010.02915.x] [PMID] [PMCID]
- Code C, Heron C. Services for aphasia, other acquired adult neurogenic communication and swallowing disorders in the United Kingdom, 2000. Disability and Rehabilitation. 2003; 25(21):1231-7. [DOI:10.1080/09638280310001599961] [PMID]
- Rambod M. (2018). [Interviewing: The most common methods of data collection in qualitative studies (Persian)]. Sadra Medical Journal. 6(4), 303-16. [Link]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health. 2015; 42(5):533-44. [DOI:10.1007/s10488-013-0528-y] [PMID] [PMCID]
- Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Education Today. 1991; 11(6):461-6. [DOI:10.1016/0260-6917(91)90009-Y] [PMID]
- Howe TJ, Worrall LE, Hickson LM. Interviews with people with aphasia: Environmental factors that influence their community participation. Aphasiology. 2008; 22(10):1092-120. [DOI:10.1080/02687030701640941]
- Hersh D. How do people with aphasia view their discharge from therapy? Aphasiology. 2009; 23(3):331-50. [DOI:10.1080/02687030701764220]
- Hinckley JJ, Hasselkus A, Ganzfried E. What people living with aphasia think about the availability of aphasia resources. American Journal of Speech-Language Pathology. 2013; 22(2).[DOI:10.1044/1058-0360(2013/12-0090)]
- Kong AP. COVID-19 and Aphasia. Current Neurology and Neuroscience Reports. 2021; 21(11):61. [DOI:10.1007/s11910-021-01150-x] [PMID] [PMCID]
- Le Dorze G, Salois-Bellerose É, Alepins M, Croteau C, Hallé M-C. A description of the personal and environmental determinants of participation several years post-stroke according to the views of people who have aphasia. Aphasiology. 2014; 28(4):421-39. [DOI:10.1080/02687038.2013.869305]
- Kong AP. Family members’ report on speech-language pathology and community services for persons with aphasia in Hong Kong. Disability and Rehabilitation. 2011; 33(25-26):2633-45. [DOI:10.3109/09638288.2011.579220] [PMID]
- Borthwick S. Communication impairment in patients following stroke. Nursing Standard (through 2013). 2012; 26(19):35-41. [DOI:10.7748/ns2012.01.26.19.35.c8879] [PMID]
- Hersh D, Worrall L, Howe T, Sherratt S, Davidson B. SMARTER goal setting in aphasia rehabilitation. Aphasiology. 2012; 26(2):220-33. [DOI:10.1080/02687038.2011.640392]
- Hallé MC, Le Dorze G. Understanding significant others’ experience of aphasia and rehabilitation following stroke. Disability and Rehabilitation. 2014; 36(21):1774-82. [DOI:10.3109/09638288.2013.870608] [PMID]
Type of Study: Original |
Subject:
Speech & Language Pathology
Received: 12/10/2022 | Accepted: 22/01/2023 | Published: 1/07/2023
Received: 12/10/2022 | Accepted: 22/01/2023 | Published: 1/07/2023
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








