Volume 24, Issue 2 (Summer 2023)
jrehab 2023, 24(2): 212-233 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rohani Ravari M H, Ebadi A, Darouie A. Facilitators and Barriers to Stuttering Telepractice in Preschool Children: A Qualitative Study. jrehab 2023; 24 (2) :212-233
URL: http://rehabilitationj.uswr.ac.ir/article-1-3197-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3197-en.html
1- Department of Speech Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran., Department of Speech Therapy, University of Social Welfare and Rehabilitation Sciences, Koodakyar Alley, Daneshjoo Blvd., Velenjak, Tehran, Iran
2- Behavioral Sciences Research Center, Life Style Institute, Nursing Faculty, Baqiyatallah University of Medical Sciences, Tehran, Iran., Behavioral Sciences Research Center, Life style institute, Nursing Faculty, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Department of Speech Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,adarouie@hotmail.com
2- Behavioral Sciences Research Center, Life Style Institute, Nursing Faculty, Baqiyatallah University of Medical Sciences, Tehran, Iran., Behavioral Sciences Research Center, Life style institute, Nursing Faculty, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Department of Speech Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Full-Text [PDF 2055 kb]
(1484 Downloads)
| Abstract (HTML) (4358 Views)
Full-Text: (2770 Views)
Introduction
Today, information and communication technology has significantly advanced, leading professionals to use it remotely to perform many tasks, including health and rehabilitation [1]. Remote rehabilitation refers to providing rehabilitation services to people remotely at home or in other environments using information and communication technology. This type of rehabilitation service not only allows receiving services for people who live far from medical centers or are unable to travel to medical centers due to disability but also saves time spent to travel home by clients so that each rehabilitation specialist can provide services to more clients during the day [2].
In recent years, the American Speech-Language-Hearing Association (ASHA) has introduced a method of therapy called telepractice. According to the definition of this association, telepractice refers to the application of information and communication technology to provide specialized remote speech, language, and hearing pathology services by linking clients to the therapist or therapist to the therapist for evaluation, intervention, and or counseling [3]. This medical service method has gained worldwide acceptance considering its scientific background [4].
The importance of delivering high-quality therapy to all parts of the world has led to the advancement of telepractice in recent decades. There are global studies on the effect of telepractice on speech and language disorders, and the results indicate the effectiveness of this treatment method [5-17]. One of these studies is O’Brian et al., conducted in Australia. They investigated the effects of webcam delivery in the first phase of the Lidcombe Program on three children who stuttered. During this study, the therapist performed the treatment sessions via Internet video calls, and there were no face-to-face visits between the therapist and the children or their parents. The results showed reduced stuttering severity. Also, the therapist and parents were satisfied with this treatment method [18].
According to previous studies, the advantages of telepractice include facilitating access to treatment and reducing referral costs [19]. The literature review reveals problems in the telepractice implementation, including professional issues and the fact that therapists view face-to-face treatment as a gold standard, legislative issues such as the fact that it is not legally possible in some countries to provide telepractice to clients living in other states, insurance and reimbursement of costs and technological problems [7, 11, 20].
Knowing the factors that facilitate or hinder telepractice delivery can help improve the quality of this service. Reinforcement of the facilitators and removing barriers can deliver telepractice services to the clients with higher quality and with the same effect as face-to-face treatments in spatial situations like disasters and pandemics.
Jahromi et al. (2021) investigated the advantages and challenges of stuttering telepractice. The results of this study referred to access to specialist therapists, reduction of treatment trips, and saving time and money as advantages of telepractice and low quality of existing technology and uncertainty about the effectiveness of this treatment by clients as existing challenges for the stuttering telepractice [21]. Jahromi et al. investigated the stuttering telepractice among people over 14 years and interviewed only those with stuttering and the parents of some of these people to collect data. The present study aimed to investigate the facilitators and barriers to stuttering telepractice in preschool children. Also, the parents of the children and the therapists were interviewed to collect data.
Materials and Methods
Standards for reporting qualitative research were used to report the study methodology [22].
Qualitative approach
The present study explored facilitators of and barriers to stuttering telepractice in preschool children. To conduct the present study, the qualitative method was used, and the naturalistic philosophy was considered. It should be noted that this study is part of a PhD dissertation in the field of stuttering telepractice in preschool children.
Researcher characteristics and reflexivity
The first author of the present study conducted all interviews. He was a PhD student in speech therapy interested in telepractice, and his master’s dissertation was on stuttering telepractice of preschool children. It should be noted that the interviewer did not already know the participants, and he made the first contact with the participants in the interview session.
Context, setting, and sampling strategy
This qualitative study was conducted in Iran from January to October 2021. Purposive sampling was conducted on therapists who have experienced telepractice, therapists who have not performed telepractice, parents who have undergone successful stuttering telepractice, and parents who have experienced failure to stutter telepractice. The purposive sampling method was used because this sampling method produces more diverse information by selecting more knowledgeable people in this field. Since using more diverse information references increases the credibility of the study to increase diversity, participants of the present study were from different provinces of Iran, including Tehran, North Khorasan, Yazd, Fars, South Khorasan, Mazandaran, and Isfahan. Also, one of the participants lived in Austria, both parents were Persian speakers, and the children had stuttering. Attempts have also been made to sample highly-experienced, low-experienced therapists and families with different levels of education and from different economic and social categories. Due to the geographical dispersion of the participants, the interviews were conducted by voice calls using WhatsApp software.
Analyses began immediately after the first interview. The interview continued until reaching data saturation. When sufficient data were collected to form each category, the researcher could use this data to determine the dimensions of the concepts and form the categories and subcategories related to the concepts, data saturation was reached, and data collection was completed.
Data collection and data collection instruments and technologies
Unstructured interviews were used to collect data. Unstructured interviews allow the participants to talk freely, and the interviewee himself or herself determines aspects of the topic and the extent and depth of talks and also allows the researcher to guide the next interviews with the same person or people and learn more about the concepts gained in previous interviews [23].
When they were selected, an unstructured interview was conducted with the first person. The interview began with an open-ended question titled “Please explain your experience with stuttering telepractice in preschool children” for therapists and “Please explain your experience with receiving stuttering telepractice” for parents. Questions were asked at baseline and during the interview to clarify the issues raised in the interview. The interview took between 32 to 66 minutes (average: 50.6 minutes). Interviews were recorded after obtaining the participant’s permission using a voice recorder.
At the end of the interview, while thanking the participants, they were asked to raise any important issue that came to their mind that was not mentioned in the interview. Besides, they were told they could send any important thing about the interview topic to the interviewer via text or voice message. They were also told that they would be referred to assess the precision of analyses and could cooperate if they wished.
Study participants
At baseline, interviews began with therapists who had experienced stuttering telepractice in preschool children. Subsequently, interviews were conducted with parents with experience in telepractice when the researcher needed to collect data from other informants. Then, the parents who had failed telepractice were interviewed to confirm the obtained concepts and find different dimensions of the concepts. Finally, the therapists who did not perform the telepractice were interviewed. Interviews with parents who had failed telepractice and therapists who did not receive telepractice helped identify barriers and confirm facilitators suggested by other participants.
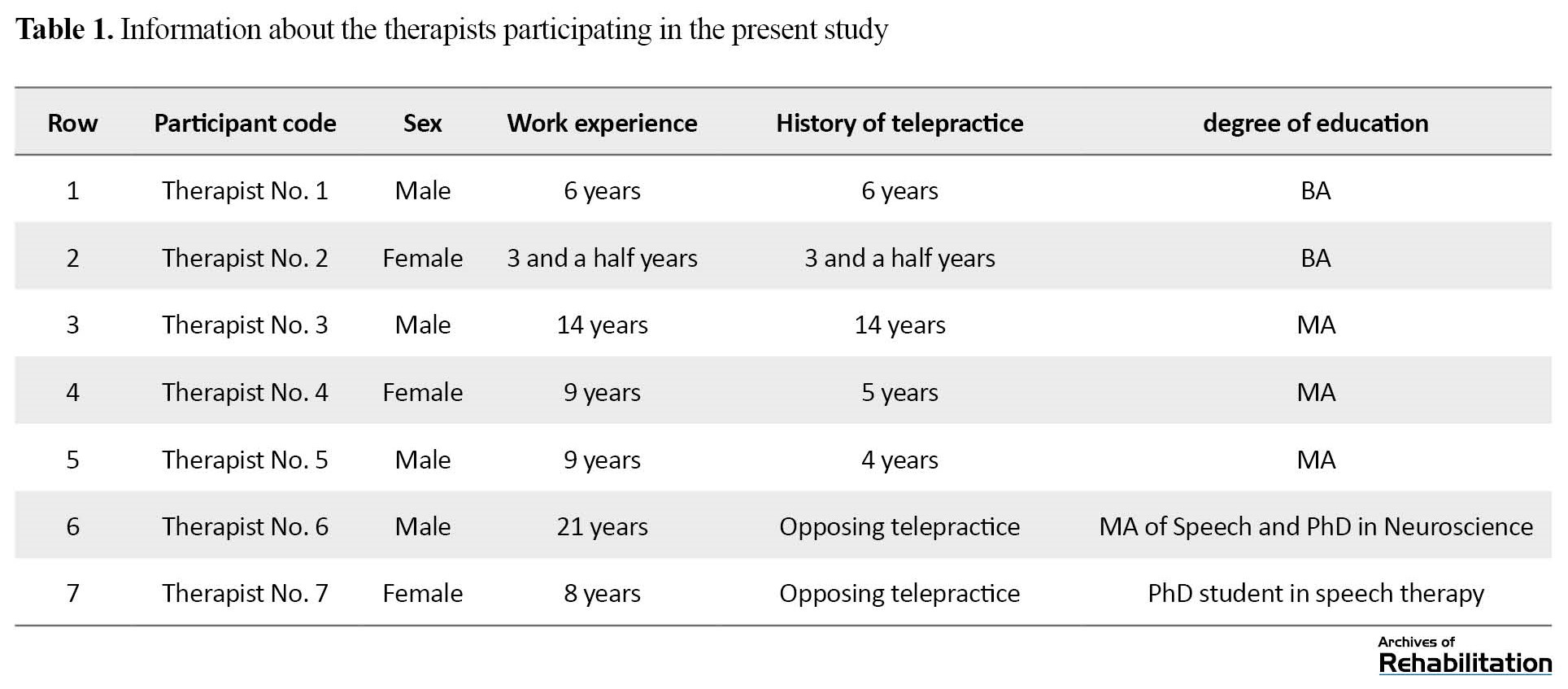
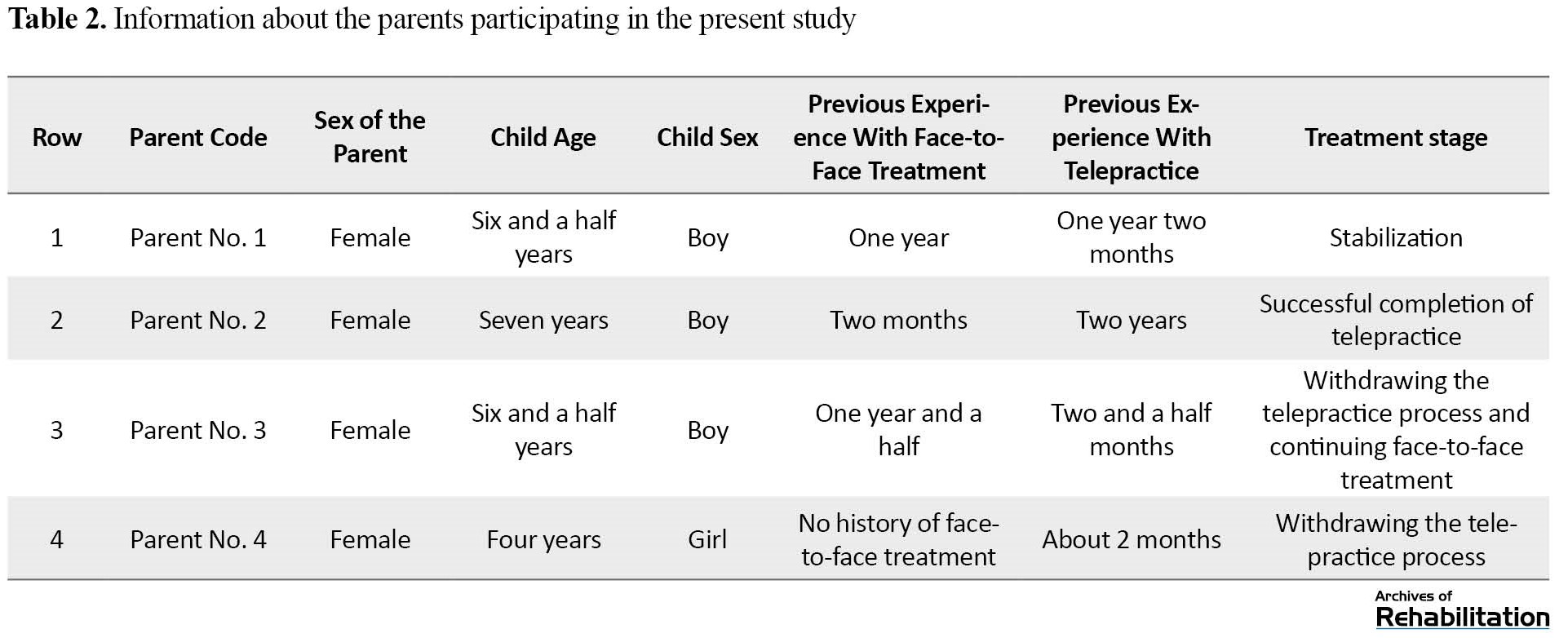
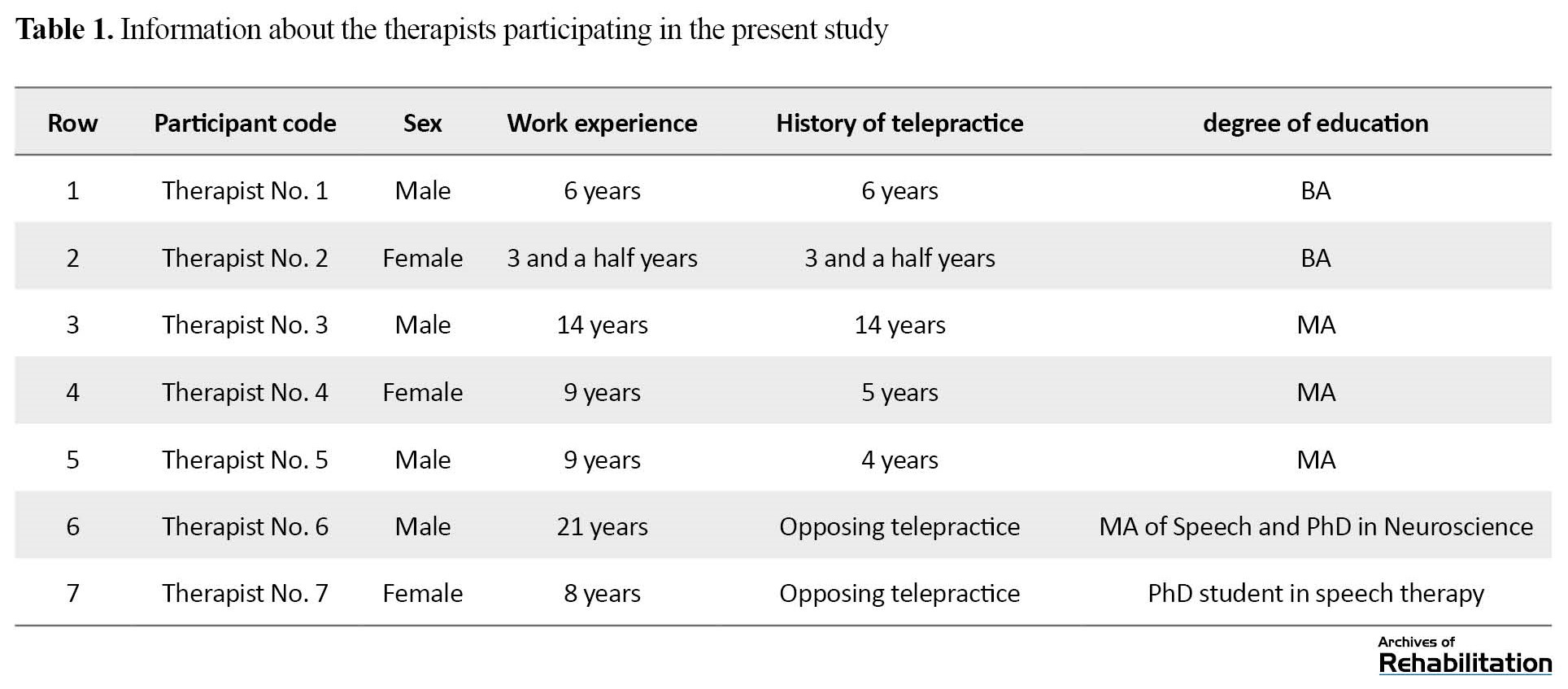
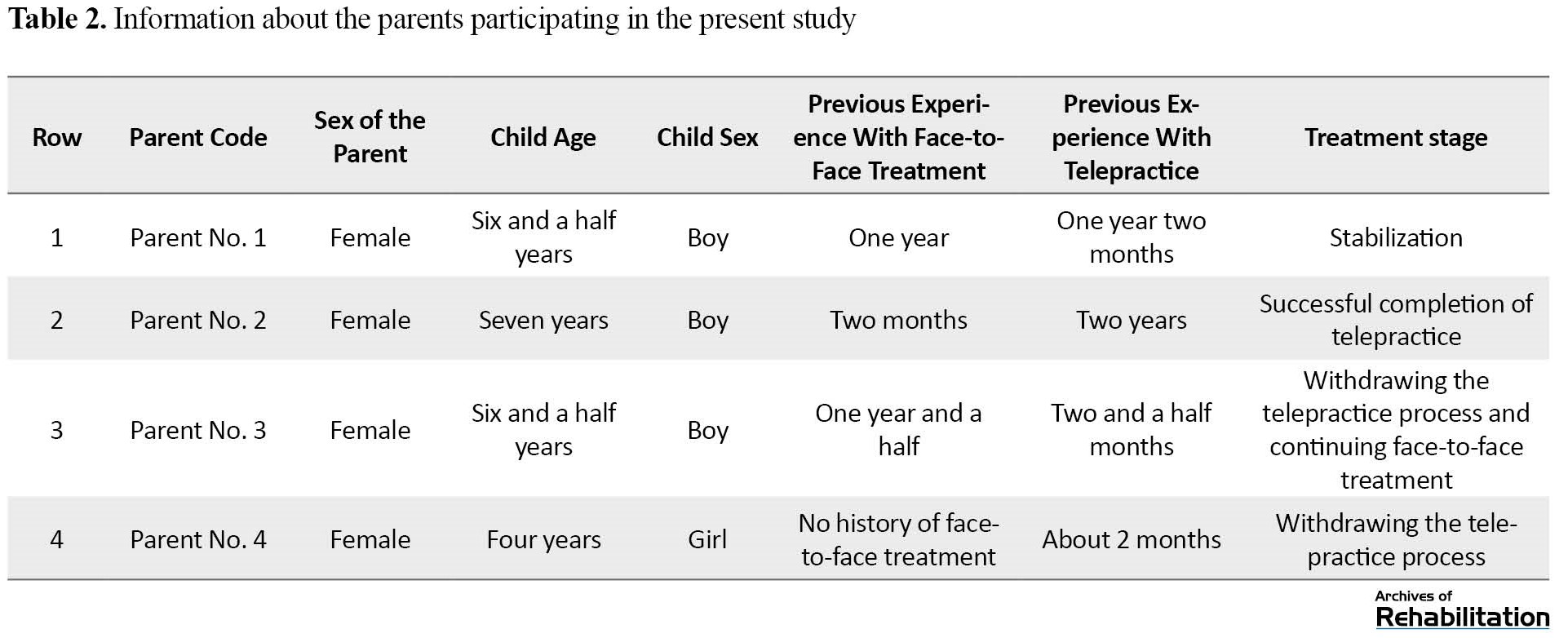
Participants of the present study included 11 people, including 5 therapists with experience in telepractice, 2 parents who had successful telepractice, 2 parents who discontinued telepractice, and 2 therapists who did not perform telepractice. As mentioned earlier, attempts were made to gather more comprehensive data in this study to use people with different characteristics, such as the therapist’s experience level, different sex, etc. Tables 1 and 2 present information about the therapists and parents participating in the study.
Data processing and analysis
All interview audio files recorded during the sessions were labeled and saved using a numeric code, then converted to text by the first author. The written files were labeled using a numeric code similar to the audio file. To protect the participant’s privacy, the participants’ names were abbreviated, and only the first letter of the name was written (for example, “A” instead of “Ali”).
The collected data were analyzed using the qualitative content analysis method reported by Graneheim and Lundman [24]. In this method, the interview text must first be read several times so that the analyst can make sense of the general content of the interviews. The data are then analyzed to achieve basic meanings and codes. Afterward, these codes are categorized based on their similarities, and subcategories and categories are formed accordingly. Finally, the main categories are extracted [24].
To perform the analysis, the first author read the interviews several times. Then the data were studied in detail and coded. The codes were then grouped based on similarity, subcategorized, and categorized. In all stages, the process and findings of each stage were reviewed periodically by two other authors. If there was a disagreement in any of the stages, a discussion was made between the authors to reach an agreement.
Data analysis was carried out using MAXQDA ver. 2020. All audio files were entered into this software, and the interviews were transcribed using the Transcribe section of the software. Then the coding was carried out, and the subcategories and categories were identified.
Trustworthiness
To increase the data trustworthiness, the four criteria of credibility, transferability, confirmability, and dependability (Lincoln & Guba) have been used [25, 26]. The researcher has been engaged in the study process for about one year, and this long-term engagement increases the credibility and accuracy of the findings. Two experienced research team members continuously reviewed the data and the study process. Another method used to improve the data credibility included member checks. The concepts obtained from analyzing each interview were sent to the participant, and the codes extracted from the interview were approved or corrected by them. The triangulation technique was used to collect data from different information sources, including therapists with experience in telepractice, therapists opposed to telepractice, parents with successful telepractice experience, and parents with unsuccessful telepractice experience.
To increase transferability, attempts were made to provide an accurate description of the participants so that the readers of the study report could know about the participants’ characteristics and make a correct judgment about the study process. To increase the confirmability, notes were taken, and reports were made during the analysis so that readers of the reports could follow them to achieve similar results. To ensure dependability, an attempt has been made to accurately record and report all study stages and processes so readers can use these reports to perform the audit process.
To observe the participants’ privacy, anonymity was considered, and the participants were marked using numeric codes. The first author transcribed interviews. Personal information was only available to the research team and has not been published anywhere. Also, before the interview, participants were given complete explanations about the purpose and process of the research, and if they had consent, they would enter the study. In addition, the participants’ audio files will be deleted 6 months after the article publication, which has been notified to the participants.
Results
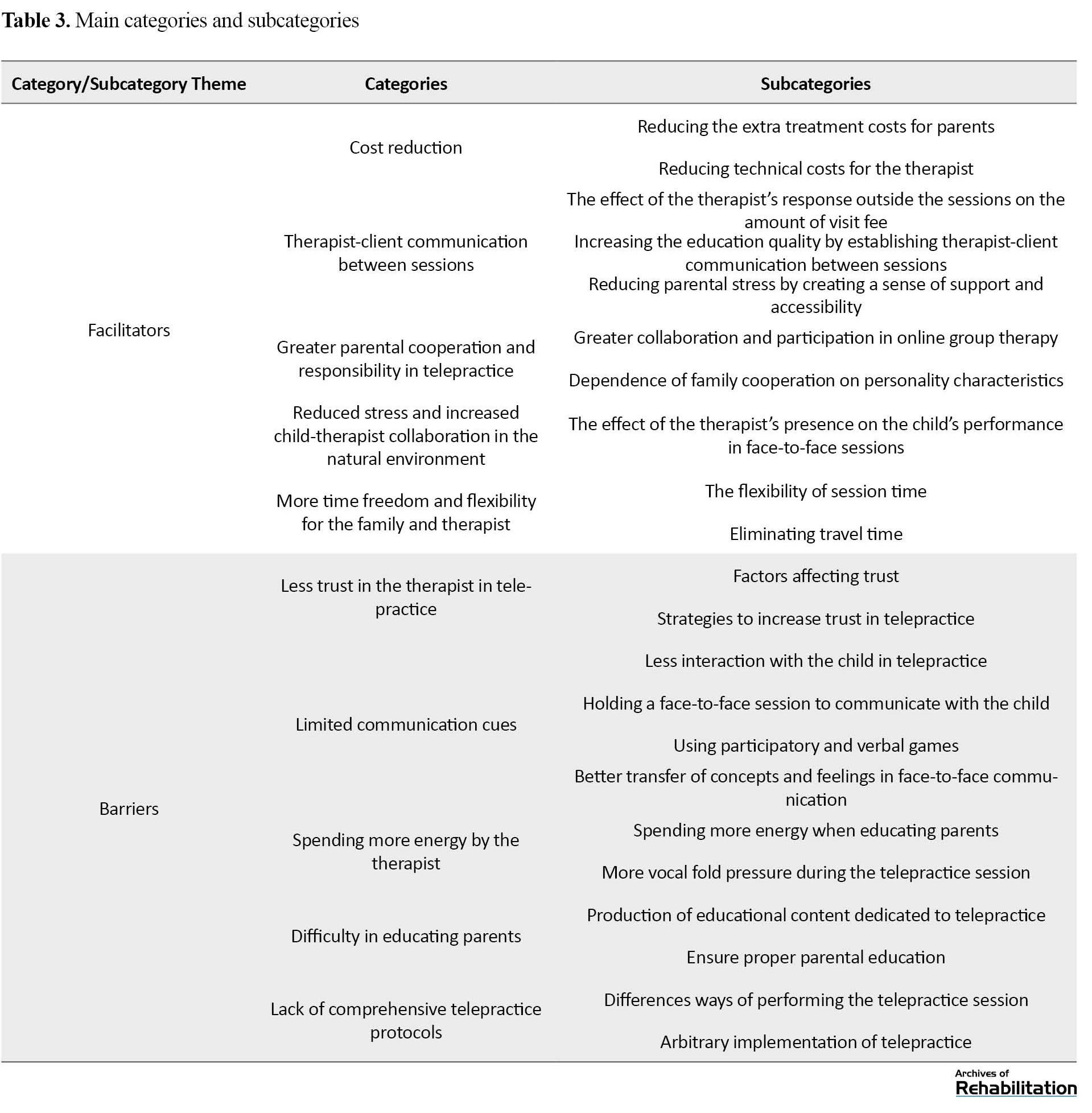
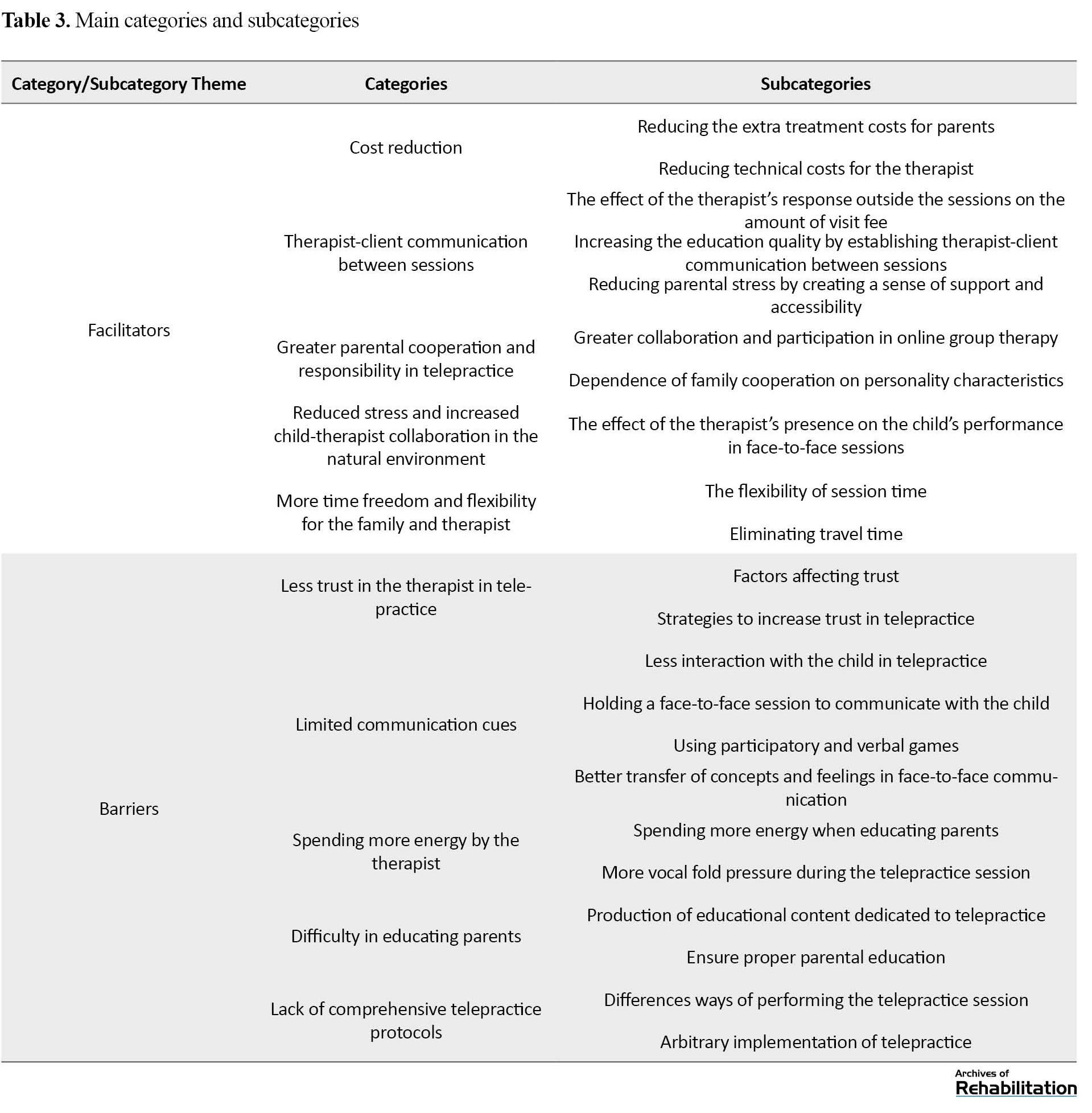
Data analysis led to the emergence of 5 main categories of barriers and 5 main categories of facilitators. Facilitator categories included cost reduction, therapist-client communication between sessions, greater parental cooperation and responsibility in telepractice, reduced stress and increased child-therapist collaboration in the natural environment, and more time freedom and flexibility for the family and therapist. The barriers categories included less trust in the therapist in telepractice, limited communication cues, spending more energy by the therapist, difficulty in educating parents, and lack of comprehensive telepractice protocols. These main categories consist of subcategories, which are shown in Table 3.
Facilitators
Costeduction
The cost is reduced for the therapist and the parent during the telepractice session, making this treatment more economical. In this type of treatment, the cost of commuting to the clinic is eliminated for both the therapist and the parents. In addition, therapists undertake lower clinic payments, the cost of the secretary, and the clinic’s running costs.
“The therapist does not have to go to a certain place. This is an advantage that he does not have to spend some time going to the clinic, and he can do it at home. However, therapists are doing it at the clinic. The job is done better there, and taking it into account, I think it could be cost-effective.” (Therapist No. 5, four years of telepractice)
Therapist-client communication between sessions
Many therapists allow the parent to communicate with the therapist between sessions. This communication increases the quality of education for parents because whenever parents face a challenge during the week, they can raise the issue with the therapist and solve the problem or ensure the correctness of their job.
“Every moment I felt that if I had a problem, I could raise it with them, it gave me a lot of comforts, rather than you thinking that there is no one, now from this week to next week, to answer your question and then you would say that I have to wait until then or what to do in the meantime. This puts a bit of stress on a person, but as soon as I could ask a question from them regarding any problem at any moment, it was good that he helped me immediately.” (Parent No. 2, successful telepractice)
Timely resolution of problems that occur for parents can also reduce parental stress and anxiety, resulting in better treatment outcomes. This relationship positively affects the parents’ payment of the visit fee, and the parents are more willing to pay the visit fee because they can also contact the therapist during the week and solve their problems as soon as possible.
Greater parental cooperation and responsibility in telepractice
Parents usually consider themselves responsible for the telepractice due to the nature of this treatment and the fact that the therapist does not interact directly with the child in many cases; therefore, they show more cooperation with the therapist. However, it should be noted that the amount of collaboration also depends on the family characteristics.
“Some families feel more responsible during the telepractice session; now they help their child themselves. It has a negative effect on some families. However, on the other hand, when some families refer in person, they are assured that the therapist has made a good impression and now consider their role less significant.” (Therapist No. 4, five years of experience in telepractice)
Group therapy is also one of the factors that increase parental cooperation. Many therapists use group synchronous and sometimes asynchronous telepractice. In addition to attracting more parental involvement, these group therapies improve the child’s communication skills, and the child experiences a different environment to control their stuttering.
Reduced stress and increased child-therapist collaboration in natural environment
Stress and anxiety negatively affect the severity of stuttering. Therefore, the lower the child’s stress, the lower the child’s stuttering intensity will be. The therapist’s presence has little effect on the severity of the child’s stuttering during the telepractice, which allows the therapist to better assess the actual severity of the child’s stuttering.
“She feels more secure next to her family. She sits in her own house and is talking to someone online, which is very different from when she is treated in a different place in the presence of some strangers and absence of her family.” (Parent No. 3, leaving the telepractice session)
Lower stress level makes the child more cooperative and make it easier to achieve therapeutic goals. Besides, treatment increases generalizability in the child’s living environment and can accelerate the treatment process.
More time freedom and time flexibility for the family and therapist
The timing of the telepractice is more flexible and can be held at any time agreed upon by the therapist and the client. This advantage increases the possibility of participation of other family members, including the child’s father or siblings, because it is much easier to coordinate to attend the online session, which is less time-consuming. In addition, the time the therapist and clients have to spend to get to the clinic is eliminated, and people can spend this time doing other daily tasks.
“When we have an online session, it takes half an hour or 40 minutes, but now you think you have to be in Tehran now; I had gone half an hour earlier, I mean the time I went (3:00 to 4:00 PM). But if I had an appointment at 6:00 PM, I had to move an hour earlier. When I wanted to return, I had to be in traffic for another hour. It takes a much shorter time online.” (Parent No. 1, treatment stabilization phase)
In addition, if the session is canceled, time management will be easier for both the parent and the therapist, and these people can easily replace the canceled session with another activity.
Barriers
Less trust in the therapist in telepractice
Because there is no real communication between the client and the therapist during the telepractice, the client-therapist mutual trust may encounter problems and be formed later.
“Another issue, in my personal opinion, is trust. For example, I think that if the mother comes to the clinic and talks to me, she communicates with me, she knows me, or now the father does not make any difference, or the child herself/himself sees something, the therapist, sees that I am working in a clinic, so, I am a speech therapist, and I am working with a child. There is a trust that leads to better cooperation, but I feel that the trust formed in the face-to-face sessions may not be found in online sessions.” (Therapist No. 1, 6 years of telepractice)
Several factors affect trust formation, including the high level of knowledge and ability to communicate properly with the parent and child and the therapist’s reputation as a stuttering therapist. However, poor trust in telepractice is less commonly reported in clients who have been referred to a therapist.
Limited communication cues
Several communication cues, such as body language, are limited online. If one of the parties has a problem with the Internet connection, even facial expressions may be affected. Following these changes, giving feedback on the parent’s activities during the session may be difficult. For these reasons, the therapist usually interacts with the child less frequently and with the parent more frequently. Therefore, the therapist attempts to treat the child by educating the parent, or in other words, using more parent-centered therapies.
“Face-to-face therapy may be a bit better because anyway, when I talk to a parent face to face, I may convey my words to him/her better than just hearing my voice on the phone, and I may better convey my feelings to him/her.” (Therapist No. 1, 6 years of experience in telepractice)
Difficulty in educating parents
In face-to-face therapies, the parent sees the therapist’s activities; therefore, they have a practical model of therapeutic activities. However, this practical model is usually unavailable in telepractice, and the therapist must prepare educational content for parent education in advance and provide the parent with modeling based on the treatment stage. Besides, the therapist must ensure the correctness of the parents’ learning so that the treatment proceeds properly to achieve the therapeutic goals.
“In face-to-face therapies, the therapist works, and the parent sees the process. The therapist does not want to spend much of this energy anymore because the parent is seeing his/her work directly.” (Therapist No. 3, 14 years of experience in telepractice)
Spending more energy by the therapist
One of the reasons that therapist spends more energy during telepractice is the difficulty of educating parents. To properly educate the parents, the therapist must devote more energy to performing the training accurately and precisely. Also, considering the nature of online communication, sometimes the therapist has to endure more voice pressure to attract the child’s attention, which causes the therapist to spend more energy.
“You also have to check the sounds and videos sent by the parents between sessions. That’s it, too much voice pressure; I undergo too much voice pressure during online sessions, which is one of my real problems. That’s why I have to rest between sessions or divide clients. For example, I should assign young and adult clients alternately because when you visit two or three children, you will undergo a lot of voice pressure.” (Therapist No. 4, 5 years of experience in telepractice)
Lack of comprehensive telepractice protocols
The existence of treatment protocols makes the treatment more accurate and organized, and as a result, better treatment outcomes are obtained. At present, therapists perform telepractice using their experiences in face-to-face therapy. Therefore, the implementation of telepractice has greater differences than face-to-face therapies, and protocol development can increase coherence in telepractice.
“We do the same treatments that we have in person, and these treatments have been designed and built and trained for face-to-face treatment, and we are using the same treatments online; if we have a special treatment protocol for online treatments, it can be very helpful.” (Therapist No. 2, three and a half years of telepractice)
Discussion
The present study has searched for the factors which are helping to improve the telepractice quality as facilitators, furthermore, for obstacles to this treatment method. These findings can use as a base for future research on telepractice quality improvement. Among these, we can mention the reduction of treatment costs and travel time, which have been mentioned in the study by Jahromi et al. [21]. However, the results of this study showed more dimensions of these two advantages. In addition to reducing travel costs for individuals, it also reduces technical expenses for the therapist, and face-to-face treatment can have other additional charges for parents, including buying a gift given to the child by the therapist and reducing costs, such as going to the amusement park and restaurant on the way to the clinic. In addition to saving time for the therapist and clients, telepractice makes sessions more flexible, and the therapist can hold therapy sessions when the child has more energy and cooperation.
Studies show that parents play a very important role in treating child stuttering, and better treatment outcomes will be obtained when parents exhibit more cooperation [27, 28]. This study showed that due to the nature of this treatment, parents feel more responsible and will thus have higher cooperation, which is an important advantage for telepractice. However, it should be noted that some parents may generally have less cooperation than other parents due to their personality traits.
Considering the important role of parents in the stuttering treatment, inter-session client-therapist communication increases the quality of parental education, so parents do the related exercises more accurately at home during the week. In addition, when their problems are resolved, parents’ stress and anxiety are greatly reduced, and studies have shown that this stress reduction helps a lot in advancing the stuttering treatment [29]. In addition to the effect of parental stress and anxiety, studies show a significant relationship between stutter anxiety and stuttering [30, 31]. Telepractice is provided in a natural environment, namely home, and the child feels relaxed at home beside his or her parents, and his or her anxiety is reduced. Also, the stuttering severity in the treatment session can be a good indicator of stuttering severity during daily routine. In addition, studies generally have shown that online communication has less effect on anxiety than face-to-face communication [32].
Studies of school children stuttering show that online and face-to-face classes have the same effect on the severity of stuttering and anxiety and that telepractice has less impact on the child’s anxiety [33]. These different results may be due to the child’s awareness of treatment sessions. Considering their greater awareness of online communication, older children are more affected by this communication, and as a result, these sessions have the same effect on the child’s anxiety as face-to-face sessions.
In addition to the telepractice advantages reported in the present study, by recognizing and eliminating telepractice barriers, more effective services can be provided to people in need by recognizing and eliminating the obstacles. These barriers include less parental trust in the therapist in telepractice. The problem of trusting the therapist is not seen among the clients referred to the therapist by a referrer trusted by the parents because the parents trust the therapist based on their trust in the referrer and then start their online treatment with him. Another factor that greatly impacts trust is the therapist’s experience and reputation. It is much easier for parents to trust therapists with sufficient years of work experience or are known as stuttering therapists. Besides, the ability to respond and the high level of knowledge of the therapist also greatly impact this trust.
Another factor that affects trust is the relationship between parents, which allows parents to share their experiences with their children’s stuttering treatment. There will be an increase in awareness and trust in the therapist when a parent who has recently had a childhood stutter and has also recently been referred for treatment and then hears the experience of other parents who have improvements in treatment increases.
Previous studies on online communications show that communication cues are reduced, and online communications may not affect real communications [32]. In telepractice, due to these limitations and the difficulty of online communication with children, many therapists place the parent as the main focus of education and treatment and advance the child’s therapy through parental education.
Some therapists use voice games such as singing or participatory games such as handy dandy and drawing to communicate with the child.
A more effective relationship is usually formed between the teacher and the learner in face-to-face training, and the learner can better get answers to the questions that arise. The teacher can also better identify the strengths and weaknesses of the learner and provide appropriate feedback [34]. This is also true in telepractice, and the therapist must ensure the correctness of the parents’ learning and produce various educational content. This difficulty in training causes the therapist to spend more energy, making telepractice more difficult than face-to-face therapy for the therapist.
The existence of a treatment model and framework can provide a unified structure for treatment and studies [35]. Despite the existence of some models of telepractice, such as the model developed by Karimi et al. [36]in Iran, speech and language pathologists perform telepractice using their face-to-face treatment experiences. They believe they have not been introduced to a comprehensive telepractice model for child stuttering, which can be used to provide better and more effective telepractice. The existing frameworks should be introduced more widely to stuttering therapists, and comprehensive telepractice frameworks should be designed.
Conclusions
Telepractice facilitates receipt of treatment services, considering its characteristics such as reducing costs, increasing access to therapists, and giving parents and therapists more time freedom. Besides, the parents’ stress and anxiety are reduced when they communicate with the therapist during the weekly sessions. Also, receiving treatment in a natural environment reduces the child’s stress.
In telepractice, limited communication cues affect the interaction between the child and the therapist, leading to greater therapist-parent interaction and further training for the parents. The therapist has to spend more energy due to this additional training to parents and subsequent difficulties.
It is suggested that future studies should investigate how to reinforce the facilitators and also find some ways to remove the barriers to telepractice. Also, future studies can develop treatment protocols for this treatment method based on these facilitators and barriers to improve the telepractice quality.
Study Limitations
In the present study, attempts were made to use everyone who knows about telepractice. Despite the efforts, all parents who participated in the present study are mothers of children. The researcher has not found a father responsible for the child’s stuttering treatment.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1399.238).
Funding
This article was extracted from the PhD thesis of Mohammad Hosein Rohani Ravari approved by the Department of Speech Therapy, University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Methodology: Abbas Ebadi; data analysis: Abbas Ebadi and Mohammad Hosein Rohani Ravari; Draft preparation, investigation, and resources: Mohammad Hosein Rohani Ravar; Supervision, validation, editing & review: Akbar Darouie and Abbas Ebadi; Conceptualization: All Authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the children and parents participated in this study as well as the therapists for their cooperation.
References
Today, information and communication technology has significantly advanced, leading professionals to use it remotely to perform many tasks, including health and rehabilitation [1]. Remote rehabilitation refers to providing rehabilitation services to people remotely at home or in other environments using information and communication technology. This type of rehabilitation service not only allows receiving services for people who live far from medical centers or are unable to travel to medical centers due to disability but also saves time spent to travel home by clients so that each rehabilitation specialist can provide services to more clients during the day [2].
In recent years, the American Speech-Language-Hearing Association (ASHA) has introduced a method of therapy called telepractice. According to the definition of this association, telepractice refers to the application of information and communication technology to provide specialized remote speech, language, and hearing pathology services by linking clients to the therapist or therapist to the therapist for evaluation, intervention, and or counseling [3]. This medical service method has gained worldwide acceptance considering its scientific background [4].
The importance of delivering high-quality therapy to all parts of the world has led to the advancement of telepractice in recent decades. There are global studies on the effect of telepractice on speech and language disorders, and the results indicate the effectiveness of this treatment method [5-17]. One of these studies is O’Brian et al., conducted in Australia. They investigated the effects of webcam delivery in the first phase of the Lidcombe Program on three children who stuttered. During this study, the therapist performed the treatment sessions via Internet video calls, and there were no face-to-face visits between the therapist and the children or their parents. The results showed reduced stuttering severity. Also, the therapist and parents were satisfied with this treatment method [18].
According to previous studies, the advantages of telepractice include facilitating access to treatment and reducing referral costs [19]. The literature review reveals problems in the telepractice implementation, including professional issues and the fact that therapists view face-to-face treatment as a gold standard, legislative issues such as the fact that it is not legally possible in some countries to provide telepractice to clients living in other states, insurance and reimbursement of costs and technological problems [7, 11, 20].
Knowing the factors that facilitate or hinder telepractice delivery can help improve the quality of this service. Reinforcement of the facilitators and removing barriers can deliver telepractice services to the clients with higher quality and with the same effect as face-to-face treatments in spatial situations like disasters and pandemics.
Jahromi et al. (2021) investigated the advantages and challenges of stuttering telepractice. The results of this study referred to access to specialist therapists, reduction of treatment trips, and saving time and money as advantages of telepractice and low quality of existing technology and uncertainty about the effectiveness of this treatment by clients as existing challenges for the stuttering telepractice [21]. Jahromi et al. investigated the stuttering telepractice among people over 14 years and interviewed only those with stuttering and the parents of some of these people to collect data. The present study aimed to investigate the facilitators and barriers to stuttering telepractice in preschool children. Also, the parents of the children and the therapists were interviewed to collect data.
Materials and Methods
Standards for reporting qualitative research were used to report the study methodology [22].
Qualitative approach
The present study explored facilitators of and barriers to stuttering telepractice in preschool children. To conduct the present study, the qualitative method was used, and the naturalistic philosophy was considered. It should be noted that this study is part of a PhD dissertation in the field of stuttering telepractice in preschool children.
Researcher characteristics and reflexivity
The first author of the present study conducted all interviews. He was a PhD student in speech therapy interested in telepractice, and his master’s dissertation was on stuttering telepractice of preschool children. It should be noted that the interviewer did not already know the participants, and he made the first contact with the participants in the interview session.
Context, setting, and sampling strategy
This qualitative study was conducted in Iran from January to October 2021. Purposive sampling was conducted on therapists who have experienced telepractice, therapists who have not performed telepractice, parents who have undergone successful stuttering telepractice, and parents who have experienced failure to stutter telepractice. The purposive sampling method was used because this sampling method produces more diverse information by selecting more knowledgeable people in this field. Since using more diverse information references increases the credibility of the study to increase diversity, participants of the present study were from different provinces of Iran, including Tehran, North Khorasan, Yazd, Fars, South Khorasan, Mazandaran, and Isfahan. Also, one of the participants lived in Austria, both parents were Persian speakers, and the children had stuttering. Attempts have also been made to sample highly-experienced, low-experienced therapists and families with different levels of education and from different economic and social categories. Due to the geographical dispersion of the participants, the interviews were conducted by voice calls using WhatsApp software.
Analyses began immediately after the first interview. The interview continued until reaching data saturation. When sufficient data were collected to form each category, the researcher could use this data to determine the dimensions of the concepts and form the categories and subcategories related to the concepts, data saturation was reached, and data collection was completed.
Data collection and data collection instruments and technologies
Unstructured interviews were used to collect data. Unstructured interviews allow the participants to talk freely, and the interviewee himself or herself determines aspects of the topic and the extent and depth of talks and also allows the researcher to guide the next interviews with the same person or people and learn more about the concepts gained in previous interviews [23].
When they were selected, an unstructured interview was conducted with the first person. The interview began with an open-ended question titled “Please explain your experience with stuttering telepractice in preschool children” for therapists and “Please explain your experience with receiving stuttering telepractice” for parents. Questions were asked at baseline and during the interview to clarify the issues raised in the interview. The interview took between 32 to 66 minutes (average: 50.6 minutes). Interviews were recorded after obtaining the participant’s permission using a voice recorder.
At the end of the interview, while thanking the participants, they were asked to raise any important issue that came to their mind that was not mentioned in the interview. Besides, they were told they could send any important thing about the interview topic to the interviewer via text or voice message. They were also told that they would be referred to assess the precision of analyses and could cooperate if they wished.
Study participants
At baseline, interviews began with therapists who had experienced stuttering telepractice in preschool children. Subsequently, interviews were conducted with parents with experience in telepractice when the researcher needed to collect data from other informants. Then, the parents who had failed telepractice were interviewed to confirm the obtained concepts and find different dimensions of the concepts. Finally, the therapists who did not perform the telepractice were interviewed. Interviews with parents who had failed telepractice and therapists who did not receive telepractice helped identify barriers and confirm facilitators suggested by other participants.
Participants of the present study included 11 people, including 5 therapists with experience in telepractice, 2 parents who had successful telepractice, 2 parents who discontinued telepractice, and 2 therapists who did not perform telepractice. As mentioned earlier, attempts were made to gather more comprehensive data in this study to use people with different characteristics, such as the therapist’s experience level, different sex, etc. Tables 1 and 2 present information about the therapists and parents participating in the study.
Data processing and analysis
All interview audio files recorded during the sessions were labeled and saved using a numeric code, then converted to text by the first author. The written files were labeled using a numeric code similar to the audio file. To protect the participant’s privacy, the participants’ names were abbreviated, and only the first letter of the name was written (for example, “A” instead of “Ali”).
The collected data were analyzed using the qualitative content analysis method reported by Graneheim and Lundman [24]. In this method, the interview text must first be read several times so that the analyst can make sense of the general content of the interviews. The data are then analyzed to achieve basic meanings and codes. Afterward, these codes are categorized based on their similarities, and subcategories and categories are formed accordingly. Finally, the main categories are extracted [24].
To perform the analysis, the first author read the interviews several times. Then the data were studied in detail and coded. The codes were then grouped based on similarity, subcategorized, and categorized. In all stages, the process and findings of each stage were reviewed periodically by two other authors. If there was a disagreement in any of the stages, a discussion was made between the authors to reach an agreement.
Data analysis was carried out using MAXQDA ver. 2020. All audio files were entered into this software, and the interviews were transcribed using the Transcribe section of the software. Then the coding was carried out, and the subcategories and categories were identified.
Trustworthiness
To increase the data trustworthiness, the four criteria of credibility, transferability, confirmability, and dependability (Lincoln & Guba) have been used [25, 26]. The researcher has been engaged in the study process for about one year, and this long-term engagement increases the credibility and accuracy of the findings. Two experienced research team members continuously reviewed the data and the study process. Another method used to improve the data credibility included member checks. The concepts obtained from analyzing each interview were sent to the participant, and the codes extracted from the interview were approved or corrected by them. The triangulation technique was used to collect data from different information sources, including therapists with experience in telepractice, therapists opposed to telepractice, parents with successful telepractice experience, and parents with unsuccessful telepractice experience.
To increase transferability, attempts were made to provide an accurate description of the participants so that the readers of the study report could know about the participants’ characteristics and make a correct judgment about the study process. To increase the confirmability, notes were taken, and reports were made during the analysis so that readers of the reports could follow them to achieve similar results. To ensure dependability, an attempt has been made to accurately record and report all study stages and processes so readers can use these reports to perform the audit process.
To observe the participants’ privacy, anonymity was considered, and the participants were marked using numeric codes. The first author transcribed interviews. Personal information was only available to the research team and has not been published anywhere. Also, before the interview, participants were given complete explanations about the purpose and process of the research, and if they had consent, they would enter the study. In addition, the participants’ audio files will be deleted 6 months after the article publication, which has been notified to the participants.
Results
Data analysis led to the emergence of 5 main categories of barriers and 5 main categories of facilitators. Facilitator categories included cost reduction, therapist-client communication between sessions, greater parental cooperation and responsibility in telepractice, reduced stress and increased child-therapist collaboration in the natural environment, and more time freedom and flexibility for the family and therapist. The barriers categories included less trust in the therapist in telepractice, limited communication cues, spending more energy by the therapist, difficulty in educating parents, and lack of comprehensive telepractice protocols. These main categories consist of subcategories, which are shown in Table 3.
Facilitators
Costeduction
The cost is reduced for the therapist and the parent during the telepractice session, making this treatment more economical. In this type of treatment, the cost of commuting to the clinic is eliminated for both the therapist and the parents. In addition, therapists undertake lower clinic payments, the cost of the secretary, and the clinic’s running costs.
“The therapist does not have to go to a certain place. This is an advantage that he does not have to spend some time going to the clinic, and he can do it at home. However, therapists are doing it at the clinic. The job is done better there, and taking it into account, I think it could be cost-effective.” (Therapist No. 5, four years of telepractice)
Therapist-client communication between sessions
Many therapists allow the parent to communicate with the therapist between sessions. This communication increases the quality of education for parents because whenever parents face a challenge during the week, they can raise the issue with the therapist and solve the problem or ensure the correctness of their job.
“Every moment I felt that if I had a problem, I could raise it with them, it gave me a lot of comforts, rather than you thinking that there is no one, now from this week to next week, to answer your question and then you would say that I have to wait until then or what to do in the meantime. This puts a bit of stress on a person, but as soon as I could ask a question from them regarding any problem at any moment, it was good that he helped me immediately.” (Parent No. 2, successful telepractice)
Timely resolution of problems that occur for parents can also reduce parental stress and anxiety, resulting in better treatment outcomes. This relationship positively affects the parents’ payment of the visit fee, and the parents are more willing to pay the visit fee because they can also contact the therapist during the week and solve their problems as soon as possible.
Greater parental cooperation and responsibility in telepractice
Parents usually consider themselves responsible for the telepractice due to the nature of this treatment and the fact that the therapist does not interact directly with the child in many cases; therefore, they show more cooperation with the therapist. However, it should be noted that the amount of collaboration also depends on the family characteristics.
“Some families feel more responsible during the telepractice session; now they help their child themselves. It has a negative effect on some families. However, on the other hand, when some families refer in person, they are assured that the therapist has made a good impression and now consider their role less significant.” (Therapist No. 4, five years of experience in telepractice)
Group therapy is also one of the factors that increase parental cooperation. Many therapists use group synchronous and sometimes asynchronous telepractice. In addition to attracting more parental involvement, these group therapies improve the child’s communication skills, and the child experiences a different environment to control their stuttering.
Reduced stress and increased child-therapist collaboration in natural environment
Stress and anxiety negatively affect the severity of stuttering. Therefore, the lower the child’s stress, the lower the child’s stuttering intensity will be. The therapist’s presence has little effect on the severity of the child’s stuttering during the telepractice, which allows the therapist to better assess the actual severity of the child’s stuttering.
“She feels more secure next to her family. She sits in her own house and is talking to someone online, which is very different from when she is treated in a different place in the presence of some strangers and absence of her family.” (Parent No. 3, leaving the telepractice session)
Lower stress level makes the child more cooperative and make it easier to achieve therapeutic goals. Besides, treatment increases generalizability in the child’s living environment and can accelerate the treatment process.
More time freedom and time flexibility for the family and therapist
The timing of the telepractice is more flexible and can be held at any time agreed upon by the therapist and the client. This advantage increases the possibility of participation of other family members, including the child’s father or siblings, because it is much easier to coordinate to attend the online session, which is less time-consuming. In addition, the time the therapist and clients have to spend to get to the clinic is eliminated, and people can spend this time doing other daily tasks.
“When we have an online session, it takes half an hour or 40 minutes, but now you think you have to be in Tehran now; I had gone half an hour earlier, I mean the time I went (3:00 to 4:00 PM). But if I had an appointment at 6:00 PM, I had to move an hour earlier. When I wanted to return, I had to be in traffic for another hour. It takes a much shorter time online.” (Parent No. 1, treatment stabilization phase)
In addition, if the session is canceled, time management will be easier for both the parent and the therapist, and these people can easily replace the canceled session with another activity.
Barriers
Less trust in the therapist in telepractice
Because there is no real communication between the client and the therapist during the telepractice, the client-therapist mutual trust may encounter problems and be formed later.
“Another issue, in my personal opinion, is trust. For example, I think that if the mother comes to the clinic and talks to me, she communicates with me, she knows me, or now the father does not make any difference, or the child herself/himself sees something, the therapist, sees that I am working in a clinic, so, I am a speech therapist, and I am working with a child. There is a trust that leads to better cooperation, but I feel that the trust formed in the face-to-face sessions may not be found in online sessions.” (Therapist No. 1, 6 years of telepractice)
Several factors affect trust formation, including the high level of knowledge and ability to communicate properly with the parent and child and the therapist’s reputation as a stuttering therapist. However, poor trust in telepractice is less commonly reported in clients who have been referred to a therapist.
Limited communication cues
Several communication cues, such as body language, are limited online. If one of the parties has a problem with the Internet connection, even facial expressions may be affected. Following these changes, giving feedback on the parent’s activities during the session may be difficult. For these reasons, the therapist usually interacts with the child less frequently and with the parent more frequently. Therefore, the therapist attempts to treat the child by educating the parent, or in other words, using more parent-centered therapies.
“Face-to-face therapy may be a bit better because anyway, when I talk to a parent face to face, I may convey my words to him/her better than just hearing my voice on the phone, and I may better convey my feelings to him/her.” (Therapist No. 1, 6 years of experience in telepractice)
Difficulty in educating parents
In face-to-face therapies, the parent sees the therapist’s activities; therefore, they have a practical model of therapeutic activities. However, this practical model is usually unavailable in telepractice, and the therapist must prepare educational content for parent education in advance and provide the parent with modeling based on the treatment stage. Besides, the therapist must ensure the correctness of the parents’ learning so that the treatment proceeds properly to achieve the therapeutic goals.
“In face-to-face therapies, the therapist works, and the parent sees the process. The therapist does not want to spend much of this energy anymore because the parent is seeing his/her work directly.” (Therapist No. 3, 14 years of experience in telepractice)
Spending more energy by the therapist
One of the reasons that therapist spends more energy during telepractice is the difficulty of educating parents. To properly educate the parents, the therapist must devote more energy to performing the training accurately and precisely. Also, considering the nature of online communication, sometimes the therapist has to endure more voice pressure to attract the child’s attention, which causes the therapist to spend more energy.
“You also have to check the sounds and videos sent by the parents between sessions. That’s it, too much voice pressure; I undergo too much voice pressure during online sessions, which is one of my real problems. That’s why I have to rest between sessions or divide clients. For example, I should assign young and adult clients alternately because when you visit two or three children, you will undergo a lot of voice pressure.” (Therapist No. 4, 5 years of experience in telepractice)
Lack of comprehensive telepractice protocols
The existence of treatment protocols makes the treatment more accurate and organized, and as a result, better treatment outcomes are obtained. At present, therapists perform telepractice using their experiences in face-to-face therapy. Therefore, the implementation of telepractice has greater differences than face-to-face therapies, and protocol development can increase coherence in telepractice.
“We do the same treatments that we have in person, and these treatments have been designed and built and trained for face-to-face treatment, and we are using the same treatments online; if we have a special treatment protocol for online treatments, it can be very helpful.” (Therapist No. 2, three and a half years of telepractice)
Discussion
The present study has searched for the factors which are helping to improve the telepractice quality as facilitators, furthermore, for obstacles to this treatment method. These findings can use as a base for future research on telepractice quality improvement. Among these, we can mention the reduction of treatment costs and travel time, which have been mentioned in the study by Jahromi et al. [21]. However, the results of this study showed more dimensions of these two advantages. In addition to reducing travel costs for individuals, it also reduces technical expenses for the therapist, and face-to-face treatment can have other additional charges for parents, including buying a gift given to the child by the therapist and reducing costs, such as going to the amusement park and restaurant on the way to the clinic. In addition to saving time for the therapist and clients, telepractice makes sessions more flexible, and the therapist can hold therapy sessions when the child has more energy and cooperation.
Studies show that parents play a very important role in treating child stuttering, and better treatment outcomes will be obtained when parents exhibit more cooperation [27, 28]. This study showed that due to the nature of this treatment, parents feel more responsible and will thus have higher cooperation, which is an important advantage for telepractice. However, it should be noted that some parents may generally have less cooperation than other parents due to their personality traits.
Considering the important role of parents in the stuttering treatment, inter-session client-therapist communication increases the quality of parental education, so parents do the related exercises more accurately at home during the week. In addition, when their problems are resolved, parents’ stress and anxiety are greatly reduced, and studies have shown that this stress reduction helps a lot in advancing the stuttering treatment [29]. In addition to the effect of parental stress and anxiety, studies show a significant relationship between stutter anxiety and stuttering [30, 31]. Telepractice is provided in a natural environment, namely home, and the child feels relaxed at home beside his or her parents, and his or her anxiety is reduced. Also, the stuttering severity in the treatment session can be a good indicator of stuttering severity during daily routine. In addition, studies generally have shown that online communication has less effect on anxiety than face-to-face communication [32].
Studies of school children stuttering show that online and face-to-face classes have the same effect on the severity of stuttering and anxiety and that telepractice has less impact on the child’s anxiety [33]. These different results may be due to the child’s awareness of treatment sessions. Considering their greater awareness of online communication, older children are more affected by this communication, and as a result, these sessions have the same effect on the child’s anxiety as face-to-face sessions.
In addition to the telepractice advantages reported in the present study, by recognizing and eliminating telepractice barriers, more effective services can be provided to people in need by recognizing and eliminating the obstacles. These barriers include less parental trust in the therapist in telepractice. The problem of trusting the therapist is not seen among the clients referred to the therapist by a referrer trusted by the parents because the parents trust the therapist based on their trust in the referrer and then start their online treatment with him. Another factor that greatly impacts trust is the therapist’s experience and reputation. It is much easier for parents to trust therapists with sufficient years of work experience or are known as stuttering therapists. Besides, the ability to respond and the high level of knowledge of the therapist also greatly impact this trust.
Another factor that affects trust is the relationship between parents, which allows parents to share their experiences with their children’s stuttering treatment. There will be an increase in awareness and trust in the therapist when a parent who has recently had a childhood stutter and has also recently been referred for treatment and then hears the experience of other parents who have improvements in treatment increases.
Previous studies on online communications show that communication cues are reduced, and online communications may not affect real communications [32]. In telepractice, due to these limitations and the difficulty of online communication with children, many therapists place the parent as the main focus of education and treatment and advance the child’s therapy through parental education.
Some therapists use voice games such as singing or participatory games such as handy dandy and drawing to communicate with the child.
A more effective relationship is usually formed between the teacher and the learner in face-to-face training, and the learner can better get answers to the questions that arise. The teacher can also better identify the strengths and weaknesses of the learner and provide appropriate feedback [34]. This is also true in telepractice, and the therapist must ensure the correctness of the parents’ learning and produce various educational content. This difficulty in training causes the therapist to spend more energy, making telepractice more difficult than face-to-face therapy for the therapist.
The existence of a treatment model and framework can provide a unified structure for treatment and studies [35]. Despite the existence of some models of telepractice, such as the model developed by Karimi et al. [36]in Iran, speech and language pathologists perform telepractice using their face-to-face treatment experiences. They believe they have not been introduced to a comprehensive telepractice model for child stuttering, which can be used to provide better and more effective telepractice. The existing frameworks should be introduced more widely to stuttering therapists, and comprehensive telepractice frameworks should be designed.
Conclusions
Telepractice facilitates receipt of treatment services, considering its characteristics such as reducing costs, increasing access to therapists, and giving parents and therapists more time freedom. Besides, the parents’ stress and anxiety are reduced when they communicate with the therapist during the weekly sessions. Also, receiving treatment in a natural environment reduces the child’s stress.
In telepractice, limited communication cues affect the interaction between the child and the therapist, leading to greater therapist-parent interaction and further training for the parents. The therapist has to spend more energy due to this additional training to parents and subsequent difficulties.
It is suggested that future studies should investigate how to reinforce the facilitators and also find some ways to remove the barriers to telepractice. Also, future studies can develop treatment protocols for this treatment method based on these facilitators and barriers to improve the telepractice quality.
Study Limitations
In the present study, attempts were made to use everyone who knows about telepractice. Despite the efforts, all parents who participated in the present study are mothers of children. The researcher has not found a father responsible for the child’s stuttering treatment.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1399.238).
Funding
This article was extracted from the PhD thesis of Mohammad Hosein Rohani Ravari approved by the Department of Speech Therapy, University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
Methodology: Abbas Ebadi; data analysis: Abbas Ebadi and Mohammad Hosein Rohani Ravari; Draft preparation, investigation, and resources: Mohammad Hosein Rohani Ravar; Supervision, validation, editing & review: Akbar Darouie and Abbas Ebadi; Conceptualization: All Authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the children and parents participated in this study as well as the therapists for their cooperation.
References
- Maheu M, Whitten P, Allen A. E-Health, telehealth, and telemedicine. Journal For Healthcare Quality. 2002; 24(4):52. [DOI:10.1111/j.1945-1474.2002.tb00449.x]
- Brennan DM, Mawson S, Brownsell S. Telerehabilitation: Enabling the remote delivery of healthcare, rehabilitation, and self management. In: Gaggioli A, Keshner EA, Weiss PL, Riva G, editors. Advanced technologies in rehabilitation. Amsterdam: IOS Press; 2009. [Link]
- ASHA. American Speech-Language-Hearing Association: Making effective communication, a human right, accessible and achievable for all. Maryland: American Speech-Language-Hearing Association. [Link]
- Houston KT. Telepractice in speech-language pathology. California: Plural Publishing, Incorporated; 2013. [Link]
- Brennan-Jones CG, Eikelboom RH, Swanepoel W. Diagnosis of hearing loss using automated audiometry in an asynchronous telehealth model: A pilot accuracy study. Journal of Telemedicine and Telecare. 2017; 23(2):256-62. [DOI:10.1177/1357633X16641552] [PMID]
- O'Brian S, Smith K, Onslow M. Webcam delivery of the lidcombe program for preschool children who stutter: A randomised controlled trial. Journal of Speech, Language, and Hearing Research. 2014; 57(3):825-30. [PMID]
- Bridgman K, Onslow M, O'Brian S, Jones M, Block S. Lidcombe Program webcam treatment for early stuttering: A randomized controlled trial. Journal of Speech, Language. 2016; 59(5):932-9. [DOI:10.1044/2016_JSLHR-S-15-0011] [PMID]
- Chen PH, Liu TW. A pilot study of telepractice for teaching listening and spoken language to Mandarin-speaking children with congenital hearing loss. Deafness & Education International. 2017; 19(3-4):134-43. [DOI:10.1080/14643154.2017.1402567]
- Collins A, Burns CL, Ward EC, Comans T, Blake C, Kenny L, et al. Home-based telehealth service for swallowing and nutrition management following head and neck cancer treatment. Journal of Telemedicine and Telecare. 2017; 23(10):866-72. [DOI:10.1177/1357633X17733020] [PMID]
- Coufal K, Parham D, Jakubowitz M, Howell C, Reyes J. Comparing traditional service delivery and telepractice for speech sound production using a functional outcome measure. American Journal of Speech-Language Pathology, 2018; 27(1):82-90. [DOI:10.1044/2017_AJSLP-16-0070] [PMID]
- Howell S, Tripoliti E, Pring T. Delivering the Lee Silverman Voice Treatment (LSVT) by web camera: A feasibility study. International Journal of Language & Communication Disorders. 2009; 44(3):287-300. [DOI:10.1080/13682820802033968] [PMID]
- Jones M, Onslow M, Harrison E, Packman A. Treating Stuttering in Young ChildrenPredicting Treatment Time in the Lidcombe Program. Journal of Speech, Language, and Hearing Research. 2000; 43(6):1440-50. [DOI:10.1044/jslhr.4306.1440] [PMID]
- Kurland J, Liu A, Stokes P. Effects of a tablet-based home practice program with telepractice on treatment outcomes in chronic aphasia. Journal of Speech, Language, and Hearing Research. 2018; 61(5):1140-56. [DOI:10.1044/2018_JSLHR-L-17-0277] [PMID] [PMCID]
- Mashima PA, Birkmire-Peters DP, Syms MJ, Holtel MR, Burgess LP, Peters LJ. Telehealth: Voice therapy using telecommunications technology. American Journal of Speech-Language Pathology. 2003; 12(4):432-9. [DOI:10.1044/1058-0360(2003/089)] [PMID]
- Sharma S, Ward EC, Burns C, Theodoros D, Russell T. Assessing swallowing disorders online: A pilot telerehabilitation study. Telemedicine Journal and e-Health. 2011; 17(9):688-95. [DOI:10.1089/tmj.2011.0034] [PMID]
- Sutherland R, Trembath D, Hodge A, Drevensek S, Lee S, Silove N, et al. Telehealth language assessments using consumer grade equipment in rural and urban settings: Feasible, reliable and well tolerated. Journal of Telemedicine and Telecare. 2017; 23(1):106-15. [DOI:10.1177/1357633X15623921] [PMID]
- Wall LR, Ward EC, Cartmill B, Hill AJ, Porceddu SV. Examining user perceptions of SwallowIT: A pilot study of a new telepractice application for delivering intensive swallowing therapy to head and neck cancer patients. Journal of Telemedicine and Telecare 2017; 23(1):53-9. [DOI:10.1177/1357633X15617887] [PMID]
- O’Brian S, Smith K, Onslow M. Webcam delivery of the Lidcombe Program for early stuttering: A phase I clinical trial. Journal of Speech, Language, and Hearing Research. 2014; 57(3):825-30. [DOI:10.1044/2014_JSLHR-S-13-0094] [PMID]
- McGill M, Noureal N, Siegel J. Telepractice Treatment of Stuttering: A systematic review. Telemedicine Journal and e-Health. 2019; 25(5):359-68. [DOI:10.1089/tmj.2017.0319] [PMID]
- Theodoros D. Telepractice in speech-language pathology: The evidence, the challenges, and the future. Perspectives on Telepractice. 2011; 1(1):10-21. [DOI:10.1044/tele1.1.10]
- Eslami Jahromi M, Farokhzadian J, Ahmadian L. Two-sided perspective on tele-speech therapy: Experiences of stuttering patients, and their parents. Assistive Technology. 2022; 34(6):717-24. [DOI:10.1080/10400435.2021.1937378] [PMID]
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine. 2014; 89(9):1245-51. [DOI:10.1097/ACM.0000000000000388] [PMID]
- Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory. California: Sage Publications; 2015. [Link]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004; 24(2):105-12. [DOI:10.1016/j.nedt.2003.10.001] [PMID]
- Guba EG. Criteria for assessing the trustworthiness of naturalistic inquiries. ECTJ. 1981; 29(2):75-91. [DOI:10.1007/BF02766777]
- Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Education for Information. 2004; 22(2):63-75. [DOI:10.3233/EFI-2004-22201]
- Logan KJ, Caruso AJ. Parents as partners in the treatment of childhood stuttering. Seminars in Speech and Language. 1997; 18(4):309-26; quiz 327. [DOI:10.1055/s-2008-1064078] [PMID]
- Rustin L, Cook F. Parental involvement in the treatment of stuttering. Language, Speech, and Hearing Services in Schools. 1995; 26(2):127-37. [DOI:10.1044/0161-1461.2602.127]
- Berquez A, Kelman E. Methods in stuttering therapy for desensitizing parents of children who stutter. American Journal of Speech-Language Pathology. 2018; 27(3S):1124-38. [DOI:10.1044/2018_AJSLP-ODC11-17-0183] [PMID]
- Kazenski D, Guitar B, McCauley R, Falls W, Dutko LS. Stuttering severity and responses to social-communicative challenge in preschool-age children who stutter. Speech, Language and Hearing. 2014; 17(3):142-52. [DOI:10.1179/2050572813Y.0000000032]
- Manning W, Gayle Beck J. The role of psychological processes in estimates of stuttering severity. Journal of Fluency Disorders. 2013; 38(4):356-67. [DOI:10.1016/j.jfludis.2013.08.002] [PMID]
- Hammick JK, Lee MJ. Do shy people feel less communication apprehension online? The effects of virtual reality on the relationship between personality characteristics and communication outcomes. Computers in Human Behavior. 2014; 33:302-10. [DOI:10.1016/j.chb.2013.01.046]
- Moïse-Richard A, Ménard L, Bouchard S, Leclercq AL. Real and virtual classrooms can trigger the same levels of stuttering severity ratings and anxiety in school-age children and adolescents who stutter. Journal of Fluency Disorders. 2021; 68:105830. [DOI:10.1016/j.jfludis.2021.105830] [PMID]
- Shaheen S, Maryam A. A study on the usefulness, difficulties and recommendations for online teaching. Pramana Research Journal. 2020; 10(8):64-71. [Link]
- Fawcett J, DeSanto-Madeya S. Contemporary nursing knowledge: Analysis and evaluation of nursing models and theories. Pennsylvania: FA Davis; 2012. [Link]
- Karimi P, Karimi H, Moazeni A, Shafiei B, Shafiei M. Developing a parent’s early telehealth program for stuttering children younger than 4 years and assessing its validity. Journal of Modern Rehabilitation. 2019; 13(1):11-22. [DOI:10.32598/JMR.13.1.11]
Type of Study: Original |
Subject:
Speech & Language Pathology
Received: 6/10/2022 | Accepted: 9/01/2023 | Published: 1/07/2023
Received: 6/10/2022 | Accepted: 9/01/2023 | Published: 1/07/2023
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








