Volume 26, Issue 4 (Winter 2026)
jrehab 2026, 26(4): 654-667 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zarezadeh F, Khajooei Z, Babaei F, Saedi M, Mardani M A. Prosthetic Reconstruction of Maxillofacial Orbital Defect With Combined Retention: Case Study. jrehab 2026; 26 (4) :654-667
URL: http://rehabilitationj.uswr.ac.ir/article-1-3640-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3640-en.html
1- Department of Orthotics and Prosthetics, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Orthotics and Prosthetics, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Orthotics and Prosthetics, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Red Crescent Society of Yazd Province, Yazd, Iran. ,natelnoory@yahoo.com
2- Department of Orthotics and Prosthetics, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Orthotics and Prosthetics, Faculty of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Red Crescent Society of Yazd Province, Yazd, Iran. ,
Full-Text [PDF 2734 kb]
(64 Downloads)
| Abstract (HTML) (1877 Views)
Discussion
Prosthetic rehabilitation offers the fastest method of restoring facial aesthetics to a normal or near-normal appearance, requiring the least time and cost for the patient. In addition, this method does not involve the surgical risk, except in cases where an initial surgical procedure on the affected area is necessary to achieve a better prosthesis fit on the face [6].
Recent studies emphasize the importance of orbital reconstruction using silicone prostheses. These methods not only provide patients with a more natural appearance but also play a key role in restoring self-confidence and improving their quality of life. For example, the use of silicone prostheses and craniofacial implants has shown significant positive effects in enhancing social functioning and reducing patients’ psychological anxiety [7].
Orbital prostheses are recognized as an effective solution for restoring appearance and improving the quality of life in patients with orbital defects. This method plays a significant role in helping patients return to their social lives by providing a natural appearance, increasing self-confidence, and mitigating negative psychological effects. With a focus on precise design and high-quality materials, lightweight, aesthetic, and comfortable prostheses can be offered that achieve desirable results without the need for complex interventions. Attention to the individual needs of each patient during the fabrication process is the key to the success of this method [8]. We must consider that each patient consults a prosthetist with unique and individual problems; however, during the fabrication of the prosthesis, it is essential to consider many of the aforementioned factors. The selection of a suspension system for such patients should be made in a way that addresses their problem while remaining easy to use.
Studies on patients who have undergone orbital surgery show that reconstruction with prostheses can significantly reduce depression and anxiety, while improving their quality of life [9].
Description of the constructed prosthesis
As mentioned, an impression is taken from the patient’s orbital region, and following the described steps, the prosthesis is fabricated. However, to achieve an ideal facial prosthesis, three essential principles must be observed: the use of a simple and comfortable suspension system, a natural appearance of the prosthesis, and ensuring its durability [2].
Use of a simple and comfortable suspension system
The first key factor for achieving an ideal facial prosthesis is the use of an appropriate retention method to ensure that the prosthesis is positioned correctly and is easy to use. Attention to this point is highly important during prosthesis fabrication and should be the first factor considered before starting any work on a maxillofacial prosthesis.
When selecting a suspension method, the prosthesis should be easy to use, simple to wear and remove, cause no skin sensitivity, and preserve the remaining tissues. Achieving proper retention also requires careful consideration of the prosthesis’s weight, size, and the position of the outer contour lines of the affected area. The overall weight of the prosthesis is determined by the material used in its fabrication. However, the modeling and wax-up stages should be performed in a way that minimizes material usage, resulting in a lighter prosthesis with better suspension. The size of the prosthesis also depends on the type of suspension method chosen for it.
Natural appearance of the prosthesis
The second factor we considered for achieving an ideal prosthesis was its natural appearance. However, to achieve the best aesthetic outcome, two fundamental principles must be observed: form and color.
Form
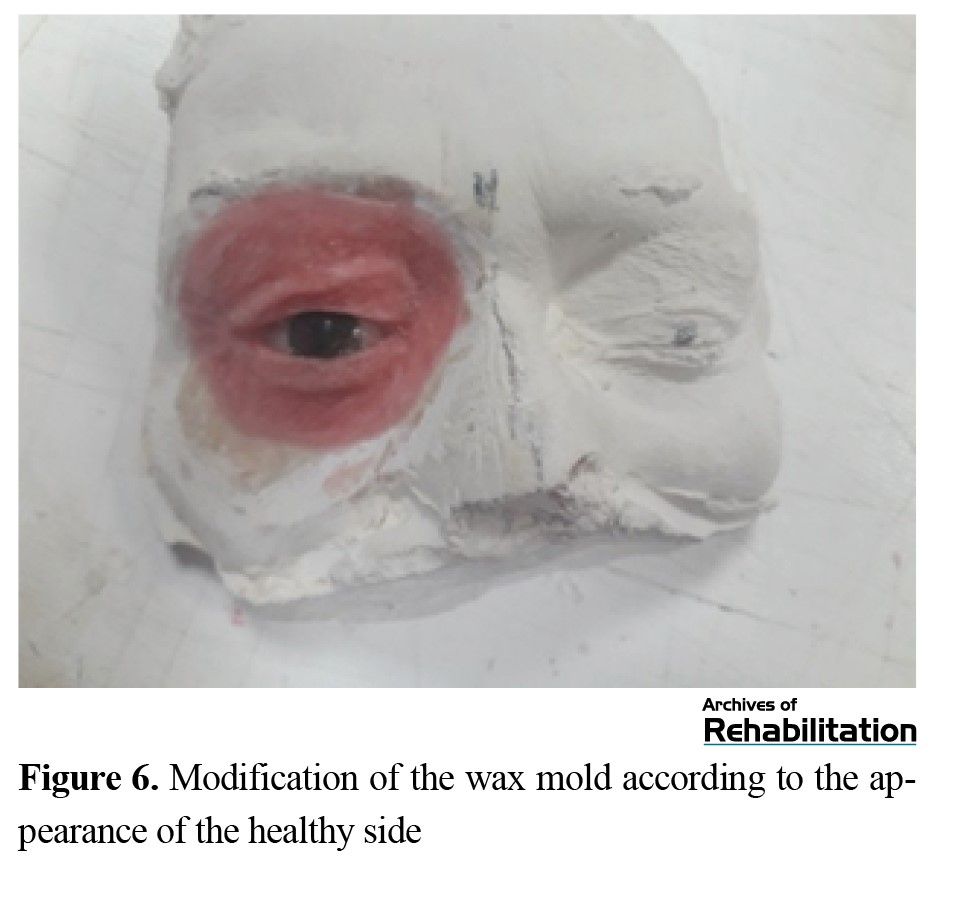
The most important principle in the appearance of a prosthesis is that its physical and anatomical shape is accurate. During the wax modeling stage, this principle must be given significant attention, ensuring that all anatomical structures are clearly represented.
Color
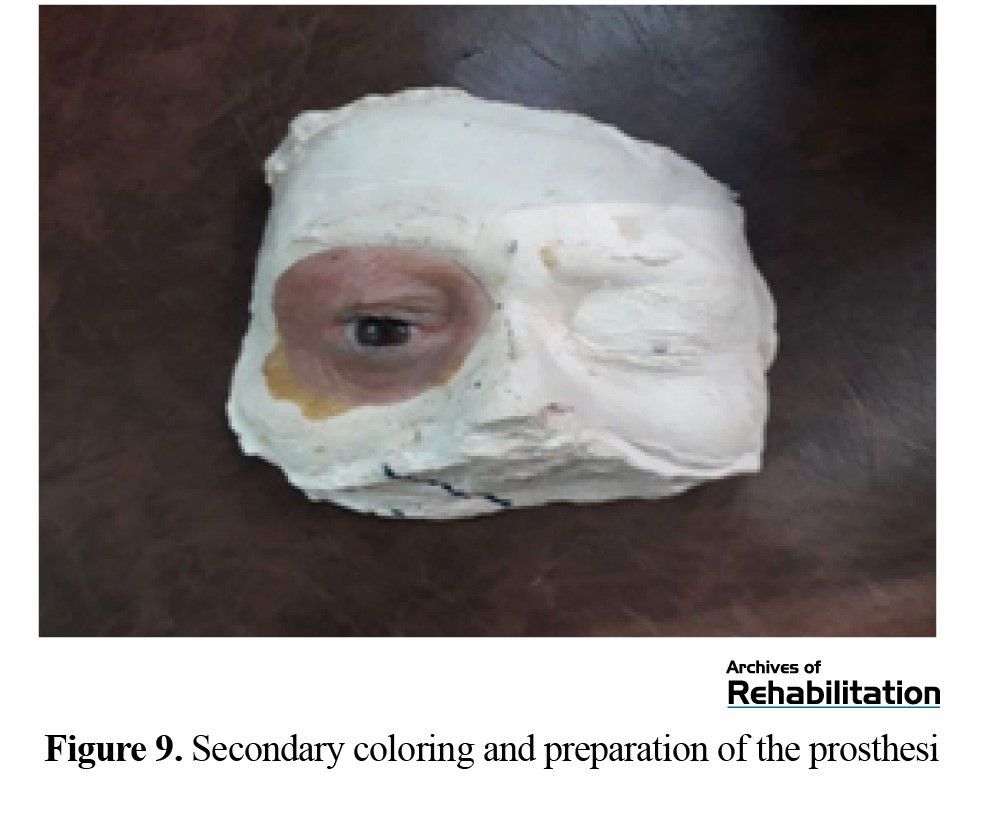
Color, like form, is one of the most important factors in making a prosthesis appear natural. The color used on the prosthesis should be similar to the patient’s skin. Therefore, one of the key criteria for judging the quality of a prosthesis is its color. To achieve a prosthesis that appears lifelike and natural, we must put the factors mentioned above at the forefront of our work, and the correct color selection is a crucial part of this process. The colors we used for this purpose included cosmetic colors from Dermacolor and oil paints commonly used by artists. For the oil paints, we used three primary colors: red, blue, and green.
Conclusion
The advantages of this prosthesis fabrication method include rapid production and reduced prosthetic treatment time, ease of use with simple insertion and removal, no skin sensitivity, increased prosthesis longevity, lower cost, and ultimately, reduced psychological distress and restoration of appearance.
Nevertheless, it is worth noting that the methods presented in this study and the related articles are considered alongside other approaches. Ultimately, as previously mentioned, numerous factors, resources, and conditions influence the prosthetist’s choice of fabrication method [5].
Ethical Considerations
Compliance with ethical guidelines
In this study, the participant was informed of the study objectives and were free to withdraw at any time. This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1402.178).
Funding
This study was funded by the University of Social Welfare and Rehabilitation Sciences .
Authors' contributions
Conceptualization, methodology, referencing, writing, and preparation of the original draft were carried out by all authors under the supervision of Fatemeh Zare Zadeh and Mohammad Ali Mardani.
Conflict of interest
This article has no conflict of interest.
Acknowledgments
The authors sincerely thank the Vice-Chancellor for Research and Technology of the University of Social Welfare and Rehabilitation Sciences as well as the participant for their support and cooperation.
References
Full-Text: (44 Views)
Introduction
Orbital defects, whether due to congenital diseases, trauma, or surgical complications, can significantly affect patients’ quality of life. In addition to their functional impact on vision and facial structure, these defects also have considerable psychological and social consequences, often leading to reduced self-confidence and social isolation [1].
One of the effective solutions for compensating these defects is the use of orbital prostheses, whose primary goal is to restore the natural appearance of the face and improve the psychological well-being of patients. Studies have shown that silicone prostheses can help improve patients’ self-confidence and sense of satisfaction, as well as facilitate the return to social activities [2, 3].
In addition to aesthetic aspects, reconstruction of orbital defects using prostheses can improve quality of life both functionally and cosmetically. One of these methods involves the design and manufacture of prostheses using technologies such as 3D modeling, which provide high precision in reconstructing anatomical details [4].However, the high cost of these designs and the unavailability of such technologies in many countries multiply the need to provide simple and accessible methods for manufacturing maxillofacial prostheses. In prosthetic studies, especially those involving maxillofacial prostheses, methods are typically presented in a case-based and technical manner, describing and introducing a specific fabrication technique. In a study on a patient with a partial ear defect, the prosthesis was fabricated using the self-suspension method. An important point in this article was the preservation of the remaining organ that was removed in the surgical procedure, and another was the introduction of a new method of suspending ear prostheses [5].
Given the importance of this issue, the present study focuses on the design and fabrication of an orbital prosthesis that not only restores the natural appearance of patients but can also play a significant role in improving their psychological well-being and functional performance. This study aims to provide a simple and comprehensive solution for orbital reconstruction using accessible methods and materials, while also evaluating its positive effects on patients’ self-confidence and quality of life. Considering the novelty of topics related to maxillofacial prostheses, the introduction of required materials, fabrication tools, impression techniques, mold-making, casting materials, and various suspension methods can serve as a valuable contribution in presenting one of the fabrication techniques to the clinical and therapeutic community.
Materials and Methods
In this study, a 60-year-old woman with an orbital defect and no history of receiving a prosthesis was referred. To begin the process of fabricating the orbital prosthesis, the first step was patient evaluation. At this stage, examinations included assessment of the sensitivity, stiffness, and softness of the healthy or unhealthy tissue, and the presence of bleeding, wounds, or injuries in the orbital area (Figure 1).
Orbital defects, whether due to congenital diseases, trauma, or surgical complications, can significantly affect patients’ quality of life. In addition to their functional impact on vision and facial structure, these defects also have considerable psychological and social consequences, often leading to reduced self-confidence and social isolation [1].
One of the effective solutions for compensating these defects is the use of orbital prostheses, whose primary goal is to restore the natural appearance of the face and improve the psychological well-being of patients. Studies have shown that silicone prostheses can help improve patients’ self-confidence and sense of satisfaction, as well as facilitate the return to social activities [2, 3].
In addition to aesthetic aspects, reconstruction of orbital defects using prostheses can improve quality of life both functionally and cosmetically. One of these methods involves the design and manufacture of prostheses using technologies such as 3D modeling, which provide high precision in reconstructing anatomical details [4].However, the high cost of these designs and the unavailability of such technologies in many countries multiply the need to provide simple and accessible methods for manufacturing maxillofacial prostheses. In prosthetic studies, especially those involving maxillofacial prostheses, methods are typically presented in a case-based and technical manner, describing and introducing a specific fabrication technique. In a study on a patient with a partial ear defect, the prosthesis was fabricated using the self-suspension method. An important point in this article was the preservation of the remaining organ that was removed in the surgical procedure, and another was the introduction of a new method of suspending ear prostheses [5].
Given the importance of this issue, the present study focuses on the design and fabrication of an orbital prosthesis that not only restores the natural appearance of patients but can also play a significant role in improving their psychological well-being and functional performance. This study aims to provide a simple and comprehensive solution for orbital reconstruction using accessible methods and materials, while also evaluating its positive effects on patients’ self-confidence and quality of life. Considering the novelty of topics related to maxillofacial prostheses, the introduction of required materials, fabrication tools, impression techniques, mold-making, casting materials, and various suspension methods can serve as a valuable contribution in presenting one of the fabrication techniques to the clinical and therapeutic community.
Materials and Methods
In this study, a 60-year-old woman with an orbital defect and no history of receiving a prosthesis was referred. To begin the process of fabricating the orbital prosthesis, the first step was patient evaluation. At this stage, examinations included assessment of the sensitivity, stiffness, and softness of the healthy or unhealthy tissue, and the presence of bleeding, wounds, or injuries in the orbital area (Figure 1).
One of the important aspects of this stage was evaluating the patient’s psychological readiness to receive a prosthesis. Different retention methods were explained to the patient. Given the patient’s reluctance to undergo reoperation and implant placement, his reluctance to use adhesives, and the fact that she wore glasses, a combined mechanical and anatomical retention method was selected [5].
The second stage was the fabrication of the primary or base color. Matching the skin, considering the tissue, surrounding lines, and color, is a very difficult task. Skin color varies under different pathological and physiological conditions, and it also depends on factors such as blood vessels and the presence of pigments like melanin and carotene.
After completing the evaluation stages, an impression of the patient was taken (Figure 2).
The second stage was the fabrication of the primary or base color. Matching the skin, considering the tissue, surrounding lines, and color, is a very difficult task. Skin color varies under different pathological and physiological conditions, and it also depends on factors such as blood vessels and the presence of pigments like melanin and carotene.
After completing the evaluation stages, an impression of the patient was taken (Figure 2).
Molding was performed of both the healthy and defective orbital areas, as well as the surrounding regions, including the eyelids and the remaining soft tissue, to ensure precise adaptation of the prosthesis. At this stage, a precise mold of the orbital area was prepared using suitable impression materials such as alginate (Iranian Chromogel alginate). For facial impression, the patient’s face must be completely horizontal, and a tray is used to hold the alginate in place. Eyelashes and eyebrows are isolated with Vaseline. The alginate is mixed with cold water and placed into the tray. To support the volume of the alginate, pieces of plaster bandage are applied on top. The alginate is ready for removal after 5 minutes.
The third stage involves molding the affected side. The most important rule when taking an impression of the damaged area is to prevent compression or displacement of the tissues. Any distortion during the molding process will result in an inaccurate mold, and ultimately, a prosthesis that does not fit the patient properly. Factors that cause these distortions include: Rotation of the neck during molding, Heaviness of the molding material, Shrinkage of the impression material.
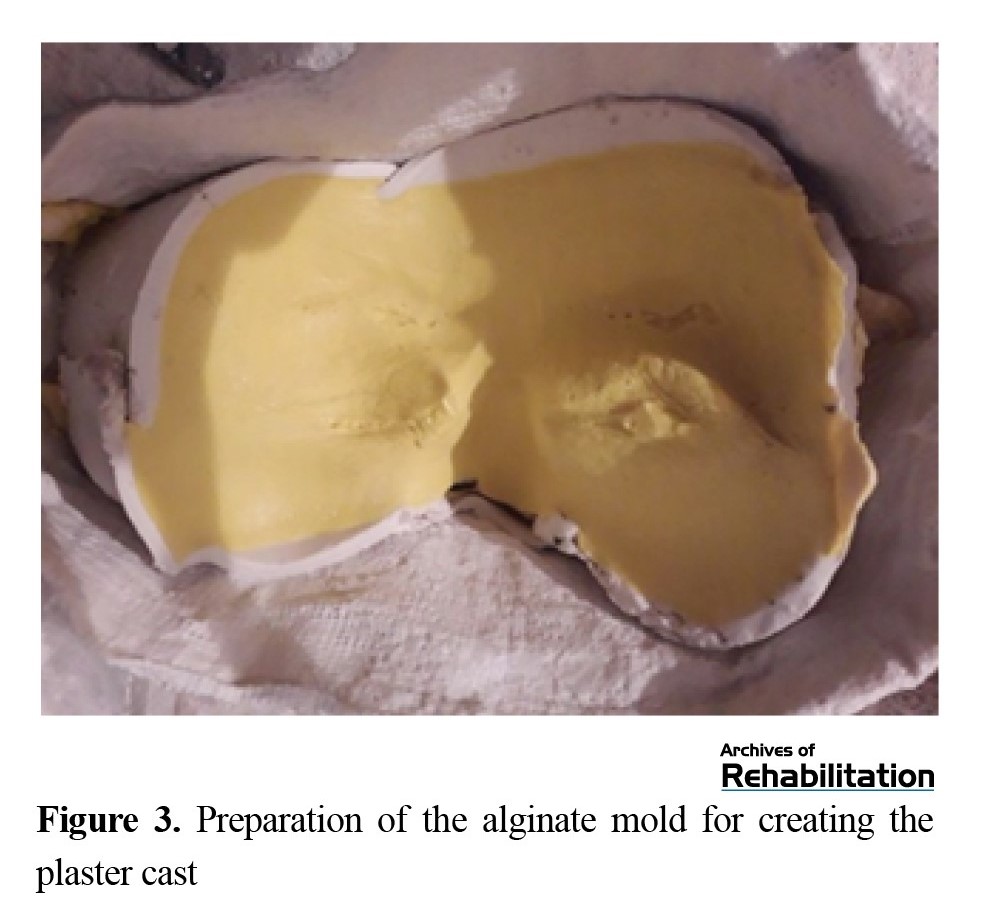
By considering the above points, errors during the molding process can be minimized. Alginate comes in powder form and must be mixed with cold water (Figure 3).
The third stage involves molding the affected side. The most important rule when taking an impression of the damaged area is to prevent compression or displacement of the tissues. Any distortion during the molding process will result in an inaccurate mold, and ultimately, a prosthesis that does not fit the patient properly. Factors that cause these distortions include: Rotation of the neck during molding, Heaviness of the molding material, Shrinkage of the impression material.
By considering the above points, errors during the molding process can be minimized. Alginate comes in powder form and must be mixed with cold water (Figure 3).
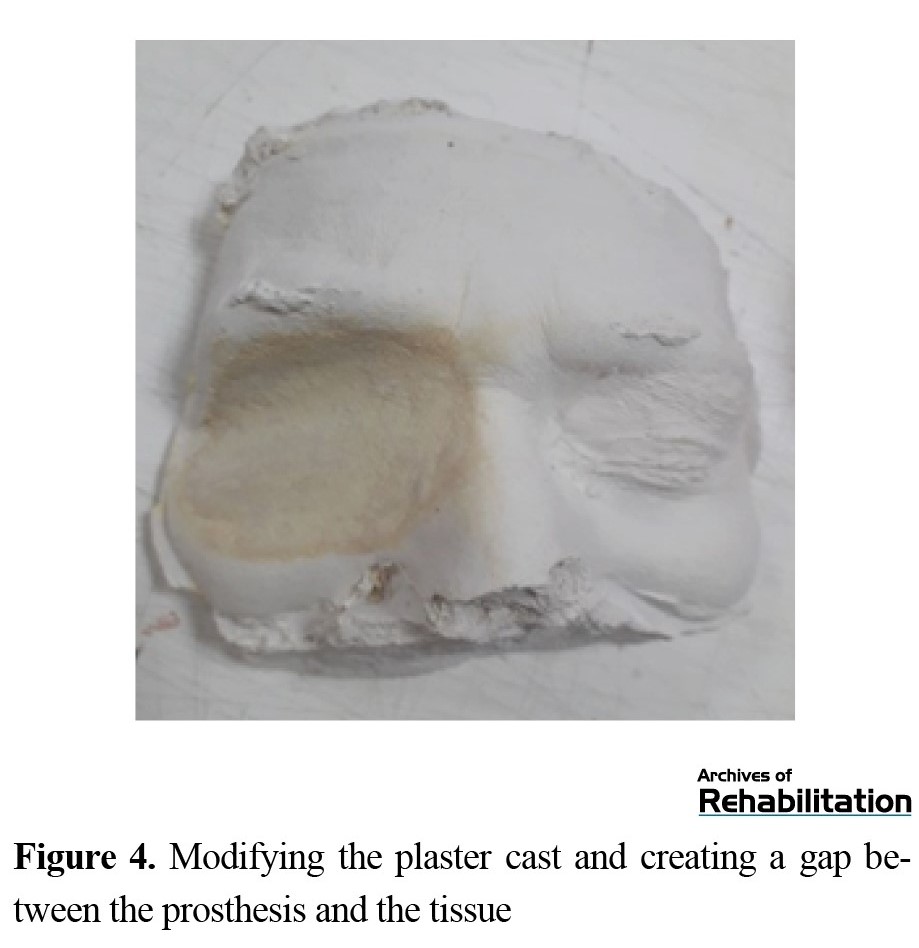
After the alginate becomes stiff, it is carefully removed from the defect. A Gypsum plaster was used to fill the space in the orbital area (Figure 4).
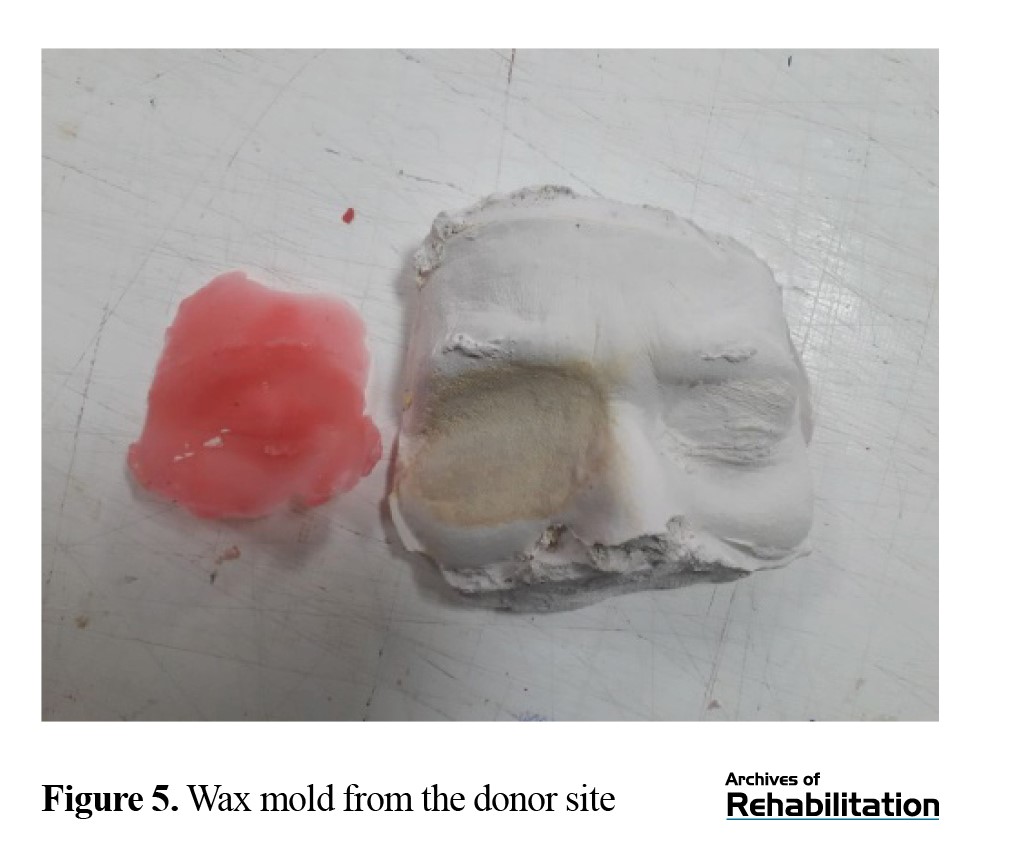
After preparing the initial mold, necessary modifications were made to the plaster mold in the orbital area to ensure its accuracy and precise adaptation to the targeted region. Then, in the lower section, layers of wax were gradually added to shape the final form of the eyelids and other soft tissue structures of the eye region (Figure 5).
In the next stage, the prosthetic eye was positioned, and layers of wax were added to reconstruct the eyelids and achieve the precise shape of the orbital area. This step was performed to ensure an accurate fit between the prosthesis and the patient’s anatomy (Figure 6).
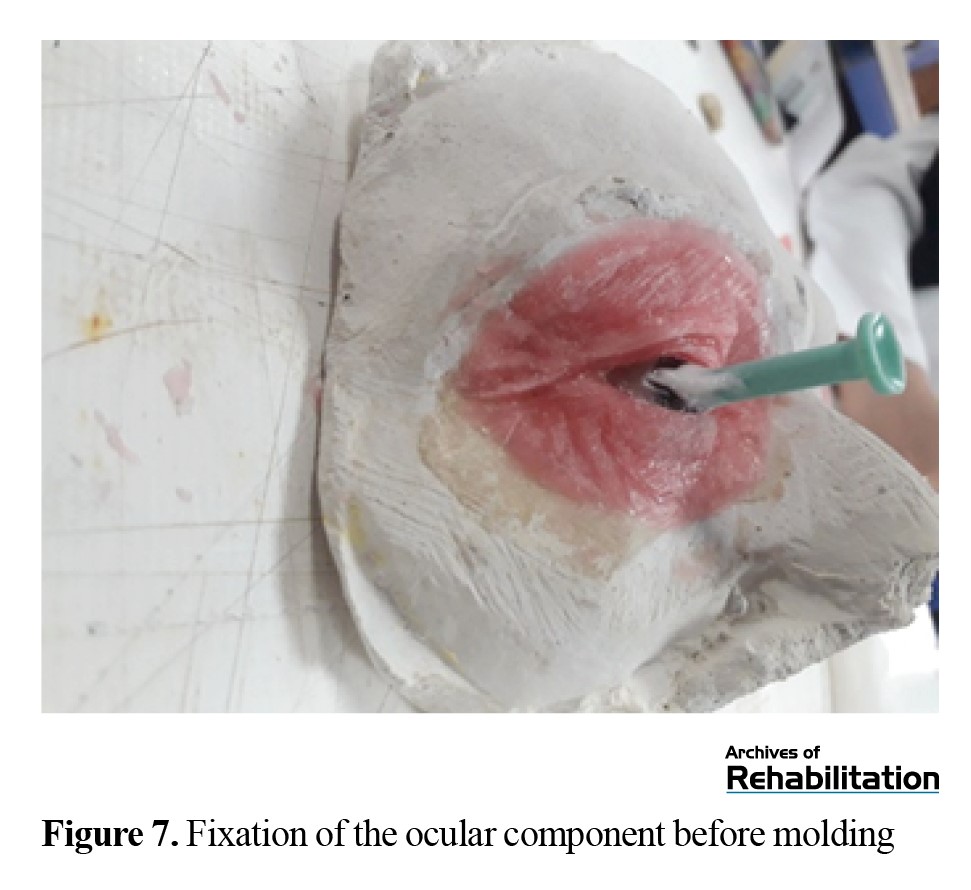
The final form of the prosthesis was then carefully completed, paying attention to details such as the eyelids and soft tissue features (Figure 7).
Next, the final molding of the prosthesis and the prosthetic eye (Acropars heat-cured acrylic) was performed, and the eye was fixed in place to prepare for the subsequent stages (Figure 7).
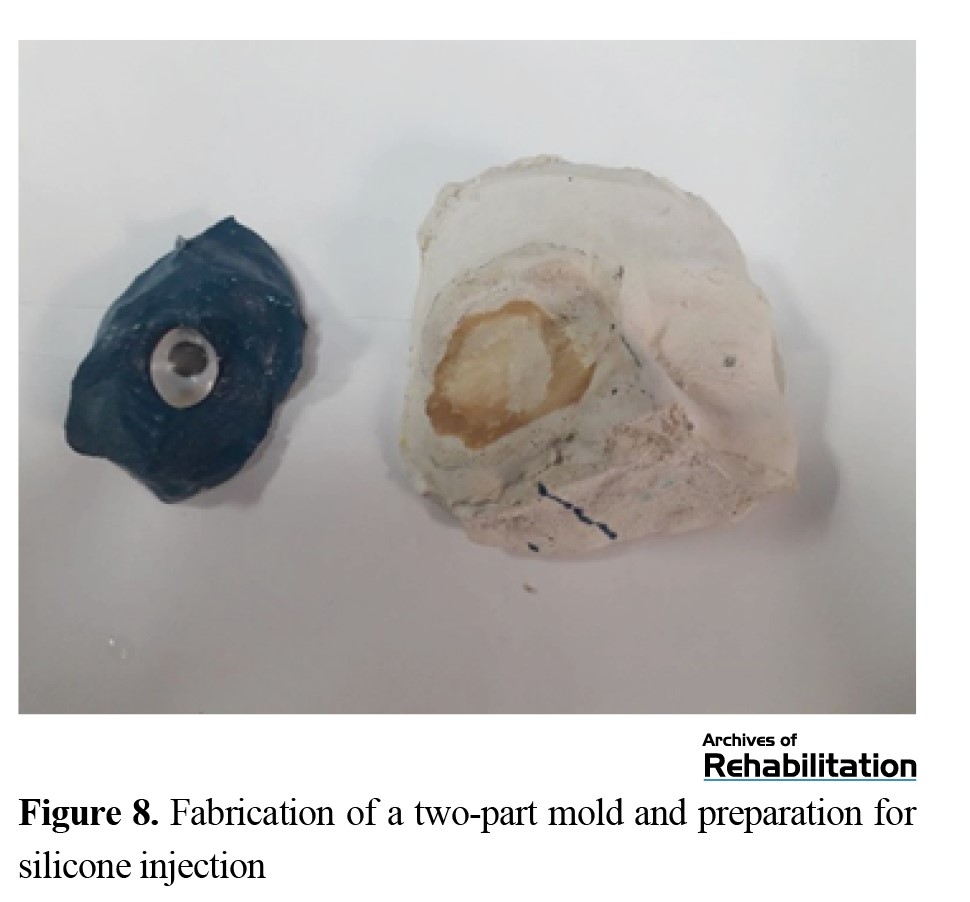
For precise placement of the ocular, the distance from the pupil of the healthy side to the nasal bridge line was measured using a digital PD meter, and the ocular piece was placed on the prosthetic side between the wax layers. The next stage, after completing the wax modeling, is the final molding. Depending on the scope of the work and the complexities of the amputated area, two-, three-, or four-part molds are prepared to prevent tearing of the silicone during removal. For this reason, a two-part mold is first created. The additional parts of the mold are then made using plaster (Figure 8).
For precise placement of the ocular, the distance from the pupil of the healthy side to the nasal bridge line was measured using a digital PD meter, and the ocular piece was placed on the prosthetic side between the wax layers. The next stage, after completing the wax modeling, is the final molding. Depending on the scope of the work and the complexities of the amputated area, two-, three-, or four-part molds are prepared to prevent tearing of the silicone during removal. For this reason, a two-part mold is first created. The additional parts of the mold are then made using plaster (Figure 8).
The excess wax was then removed from the mold using boiling water, preparing the mold for silicone pouring.
For the fabrication of the final prosthesis, RTV silicone (RTV2 silicones with a hardness of 10 or 20) was mixed with an appropriate color. This mixture was blended with cosmetic and oil-based colors to achieve the best match with the patient’s skin tone. During this stage, color matching was checked under natural light to ensure a natural appearance of the final prosthesis. For secondary coloring, oil-based paints were used; in the presence of the patient, the selected color was mixed with silicone adhesive and applied to the prosthesis using a sponge or fine brush. Finally, the prosthesis was allowed to rest for 24 hours to dry and for better color integration (Figure 9).
For the fabrication of the final prosthesis, RTV silicone (RTV2 silicones with a hardness of 10 or 20) was mixed with an appropriate color. This mixture was blended with cosmetic and oil-based colors to achieve the best match with the patient’s skin tone. During this stage, color matching was checked under natural light to ensure a natural appearance of the final prosthesis. For secondary coloring, oil-based paints were used; in the presence of the patient, the selected color was mixed with silicone adhesive and applied to the prosthesis using a sponge or fine brush. Finally, the prosthesis was allowed to rest for 24 hours to dry and for better color integration (Figure 9).
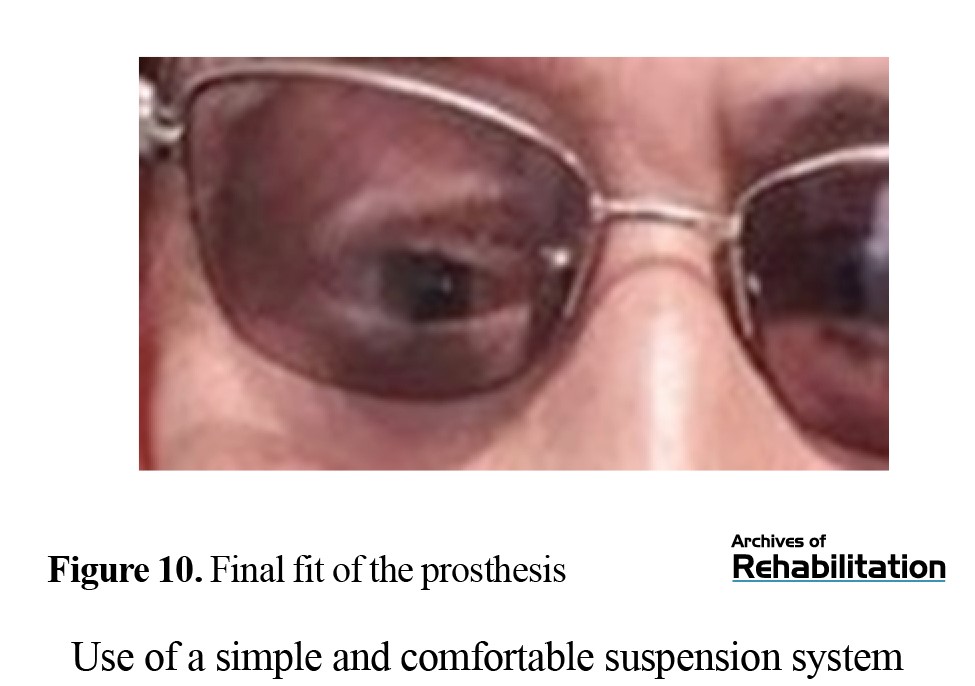
In the final stage, the prosthesis was evaluated on the patient’s face for shape, color, size, placement, angulation, and proper suspension. After making the necessary corrections and adjustments, the silicone prosthesis was delivered to the patient for use (Figure 10).
Discussion
Prosthetic rehabilitation offers the fastest method of restoring facial aesthetics to a normal or near-normal appearance, requiring the least time and cost for the patient. In addition, this method does not involve the surgical risk, except in cases where an initial surgical procedure on the affected area is necessary to achieve a better prosthesis fit on the face [6].
Recent studies emphasize the importance of orbital reconstruction using silicone prostheses. These methods not only provide patients with a more natural appearance but also play a key role in restoring self-confidence and improving their quality of life. For example, the use of silicone prostheses and craniofacial implants has shown significant positive effects in enhancing social functioning and reducing patients’ psychological anxiety [7].
Orbital prostheses are recognized as an effective solution for restoring appearance and improving the quality of life in patients with orbital defects. This method plays a significant role in helping patients return to their social lives by providing a natural appearance, increasing self-confidence, and mitigating negative psychological effects. With a focus on precise design and high-quality materials, lightweight, aesthetic, and comfortable prostheses can be offered that achieve desirable results without the need for complex interventions. Attention to the individual needs of each patient during the fabrication process is the key to the success of this method [8]. We must consider that each patient consults a prosthetist with unique and individual problems; however, during the fabrication of the prosthesis, it is essential to consider many of the aforementioned factors. The selection of a suspension system for such patients should be made in a way that addresses their problem while remaining easy to use.
Studies on patients who have undergone orbital surgery show that reconstruction with prostheses can significantly reduce depression and anxiety, while improving their quality of life [9].
Description of the constructed prosthesis
As mentioned, an impression is taken from the patient’s orbital region, and following the described steps, the prosthesis is fabricated. However, to achieve an ideal facial prosthesis, three essential principles must be observed: the use of a simple and comfortable suspension system, a natural appearance of the prosthesis, and ensuring its durability [2].
Use of a simple and comfortable suspension system
The first key factor for achieving an ideal facial prosthesis is the use of an appropriate retention method to ensure that the prosthesis is positioned correctly and is easy to use. Attention to this point is highly important during prosthesis fabrication and should be the first factor considered before starting any work on a maxillofacial prosthesis.
When selecting a suspension method, the prosthesis should be easy to use, simple to wear and remove, cause no skin sensitivity, and preserve the remaining tissues. Achieving proper retention also requires careful consideration of the prosthesis’s weight, size, and the position of the outer contour lines of the affected area. The overall weight of the prosthesis is determined by the material used in its fabrication. However, the modeling and wax-up stages should be performed in a way that minimizes material usage, resulting in a lighter prosthesis with better suspension. The size of the prosthesis also depends on the type of suspension method chosen for it.
Natural appearance of the prosthesis
The second factor we considered for achieving an ideal prosthesis was its natural appearance. However, to achieve the best aesthetic outcome, two fundamental principles must be observed: form and color.
Form
The most important principle in the appearance of a prosthesis is that its physical and anatomical shape is accurate. During the wax modeling stage, this principle must be given significant attention, ensuring that all anatomical structures are clearly represented.
Color
Color, like form, is one of the most important factors in making a prosthesis appear natural. The color used on the prosthesis should be similar to the patient’s skin. Therefore, one of the key criteria for judging the quality of a prosthesis is its color. To achieve a prosthesis that appears lifelike and natural, we must put the factors mentioned above at the forefront of our work, and the correct color selection is a crucial part of this process. The colors we used for this purpose included cosmetic colors from Dermacolor and oil paints commonly used by artists. For the oil paints, we used three primary colors: red, blue, and green.
Conclusion
The advantages of this prosthesis fabrication method include rapid production and reduced prosthetic treatment time, ease of use with simple insertion and removal, no skin sensitivity, increased prosthesis longevity, lower cost, and ultimately, reduced psychological distress and restoration of appearance.
Nevertheless, it is worth noting that the methods presented in this study and the related articles are considered alongside other approaches. Ultimately, as previously mentioned, numerous factors, resources, and conditions influence the prosthetist’s choice of fabrication method [5].
Ethical Considerations
Compliance with ethical guidelines
In this study, the participant was informed of the study objectives and were free to withdraw at any time. This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1402.178).
Funding
This study was funded by the University of Social Welfare and Rehabilitation Sciences .
Authors' contributions
Conceptualization, methodology, referencing, writing, and preparation of the original draft were carried out by all authors under the supervision of Fatemeh Zare Zadeh and Mohammad Ali Mardani.
Conflict of interest
This article has no conflict of interest.
Acknowledgments
The authors sincerely thank the Vice-Chancellor for Research and Technology of the University of Social Welfare and Rehabilitation Sciences as well as the participant for their support and cooperation.
References
- Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, et al. National population-based estimates for major birth defects, 2010-2014. Birth Defects Research. 2019; 111(18):1420-35. [DOI:10.1002/bdr2.1589] [PMID]
- Dings JP, Merkx MA, de Clonie Maclennan-Naphausen MT, van de Pol P, Maal TJ, Meijer GJ. Maxillofacial prosthetic rehabilitation: A survey on the quality of life. The Journal of Prosthetic Dentistry. 2018; 120(5):780-6. [DOI:10.1016/j.prosdent.2018.03.032] [PMID]
- Mehdi ME, Atiqi OE, Yafi I, Benlaassel OA, Zinedine S, Geouatri M, et al. [Reconstruction of orbital exenteration defects: About 20 cases (French)]. The Pan African Medical Journal. 2022; 43:105. [DOI:10.11604/pamj.2022.43.105.26034] [PMID]
- Blessing NW, Rong AJ, Brian CT, Erickson BP, Lee BW, Johnson TE. Orbital bony reconstruction with presized and precontoured porous polyethylene-titanium implants. Ophthalmic Plastic & Reconstructive Surgery. 2021; 37(3):284-9. [DOI:10.1097/IOP.0000000000001829] [PMID]
- Mardani MA, Zarezadeh F, Hashemi H. [Implant-based prosthetic reconstruction in patients with congenital ear defects (Persian)]. Archives of Rehabilitation. 2022; 23(3):450-63. [DOI:10.32598/RJ.23.3.2883.3]
- Subramaniam S, Breik O, Cadd B, Peart G, Wiesenfeld D, Heggie A, et al. Long-term outcomes of craniofacial implants for the restoration of facial defects. International Journal of Oral and Maxillofacial Surgery. 2018; 47(6):773-82. [DOI:10.1016/j.ijom.2018.01.013] [PMID]
- Mardani MA, Arazpour M, Bani MA, Hutchins SW, Zarezadeh F, Sojodi M, et al. Prosthetic rehabilitation of a patient with partial ear amputation using a self suspension technique. Prosthetics and Orthotics International. 2011; 35(4):473-7. [DOI:10.1177/0309364611422269] [PMID]
- Alberga J, Eggels I, Visser A, van Minnen B, Korfage A, Vissink A, et al. Outcome of implants placed to retain craniofacial prostheses-A retrospective cohort study with a follow-up of up to 30 years. Clinical Implant Dentistry and Related Research. 2022; 24(5):643-54. [DOI:10.1111/cid.13106] [PMID]
- Balakrishnan N, Agrawal S, Bhargava R, Jain V, Pushker N, Meel R, et al. Psychosocial factors among patients undergoing orbital exenteration. Clinical and Experimental Optometry. 2023; 106(6):626-32. [DOI:10.1080/08164622.2022.2106781] [PMID]
Type of Study: Case report |
Subject:
Orthotics & Prosthetics
Received: 25/05/2025 | Accepted: 31/08/2025 | Published: 1/01/2026
Received: 25/05/2025 | Accepted: 31/08/2025 | Published: 1/01/2026
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |