Volume 26, Issue 3 (Autumn 2025)
jrehab 2025, 26(3): 344-359 |
Back to browse issues page
Ethics code: IR.USWR.REC.1402.140
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abolhasani E, Aminian G, Baghaei Roodsari R, Jiryaei Sharahi Z. The Effect of Spandex Anti-friction Pad on Satisfaction, Pain, Balance, and Walking in Unilateral Transtibial Amputees: A Pilot Study. jrehab 2025; 26 (3) :344-359
URL: http://rehabilitationj.uswr.ac.ir/article-1-3547-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3547-en.html
1- Karaj Red Crescent Society Rehabilitation Center, Alborz Province Red Crescent Society, Karaj, Iran.
2- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,gholamrezaaminian@yahoo.com
3- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Orthotics and Prosthetics, Iran-Helal Institute of Applied Science and Technology, Tehran, Iran.
2- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Orthotics and Prosthetics, Iran-Helal Institute of Applied Science and Technology, Tehran, Iran.
Full-Text [PDF 2485 kb]
(194 Downloads)
| Abstract (HTML) (1896 Views)
Full-Text: (180 Views)
Introduction
The transtibial amputation is the most common type of lower limb amputation, whose rate is increasing due to vascular diseases such as diabetes and trauma [1]. The ratio of transtibial amputation to transfemoral amputation is 2:1 [2]. The risk of creating ulcers and amputations in individuals with diabetes is significantly higher than in non-diabetic individuals. It is estimated that, every 20 seconds, an amputation is performed on a diabetic person somewhere in the world [3]. Amputation creates permanent disability, and the amputee requires a prosthesis for stability, mobility, and performing daily living activities [4].
Socket suspension is an important factor that can affect the mobility and walking of an amputee. The suspension system is an important component of the transtibial prosthesis, responsible for holding the prosthesis on the residual limb during the swing phase of gait. Considering the importance of the prosthetic suspension systems in the rehabilitation process, selecting an appropriate suspension system based on the functional needs and expectations of amputees is a significant step [5, 6]. There are some complications caused by a weak suspension system, including pain, skin ulcers, and abnormal walking due to piston movement (the vertical movement between the socket and the residual limb during the stance and swing phases of gait). This may lead to reduced satisfaction and comfort for the amputee [11-14]. These complications can lead to a decrease in the walking ability of amputees. This factor has always been an important factor for the rehabilitation team in assessing an individual’s potential for walking with a prosthetic leg [15, 16]. To address these issues, the interface between the prosthetic socket and the residual limb, which is made from various materials such as silicone, has been introduced as a gel liner. The gel liner is an expensive commercial product and is difficult for people in developing countries to buy [5].
Silicone has various properties and can be used to make silicone liners for prostheses. It exhibits the highest friction with the skin compared to other materials [17]. This increased level of friction is important for improving the suspension of silicone gel liners, which makes greater adherence of the liner to the skin over the entire residual limb. However, in individuals using gel liner with pin suspension systems, it has been reported that friction increases in the anterior knee region, especially at the patellar tendon, during walking and when a high degree of knee flexion is required, such as prolonged sitting [18]. This friction may lead to some changes in skin, as tissues try to protect themselves from further damage [19, 20]. This problem can also cause increased wear and tear of the gel liner in the patellar tendon area, which can overshadow the benefits of the gel liner [5, 11, 17]. Excessive and prolonged friction, along with relatively high localized pressure between the skin of the residual limb and the gel liner in the patellar tendon can eventually cause hole in this area that are subjected to excessive friction [6]. It seems that the discomfort experienced by individuals from this friction is due to the mismatch between the skin movements of the residual limb and the gel liner [17]. This problem in the patellar tendon area is more common among transtibial amputees using hybrid sockets, because the concept of hybrid socket in below-the-knee prosthetics basically arises from integrating the patellar tendon bearing (PTB) and total surface bearing (TSB) designs. Actually, there is greater weight bearing and friction with the gel liner in PTB design compared to TSB design due to the greater load-bearing and involvement of the patellar tendon [5].
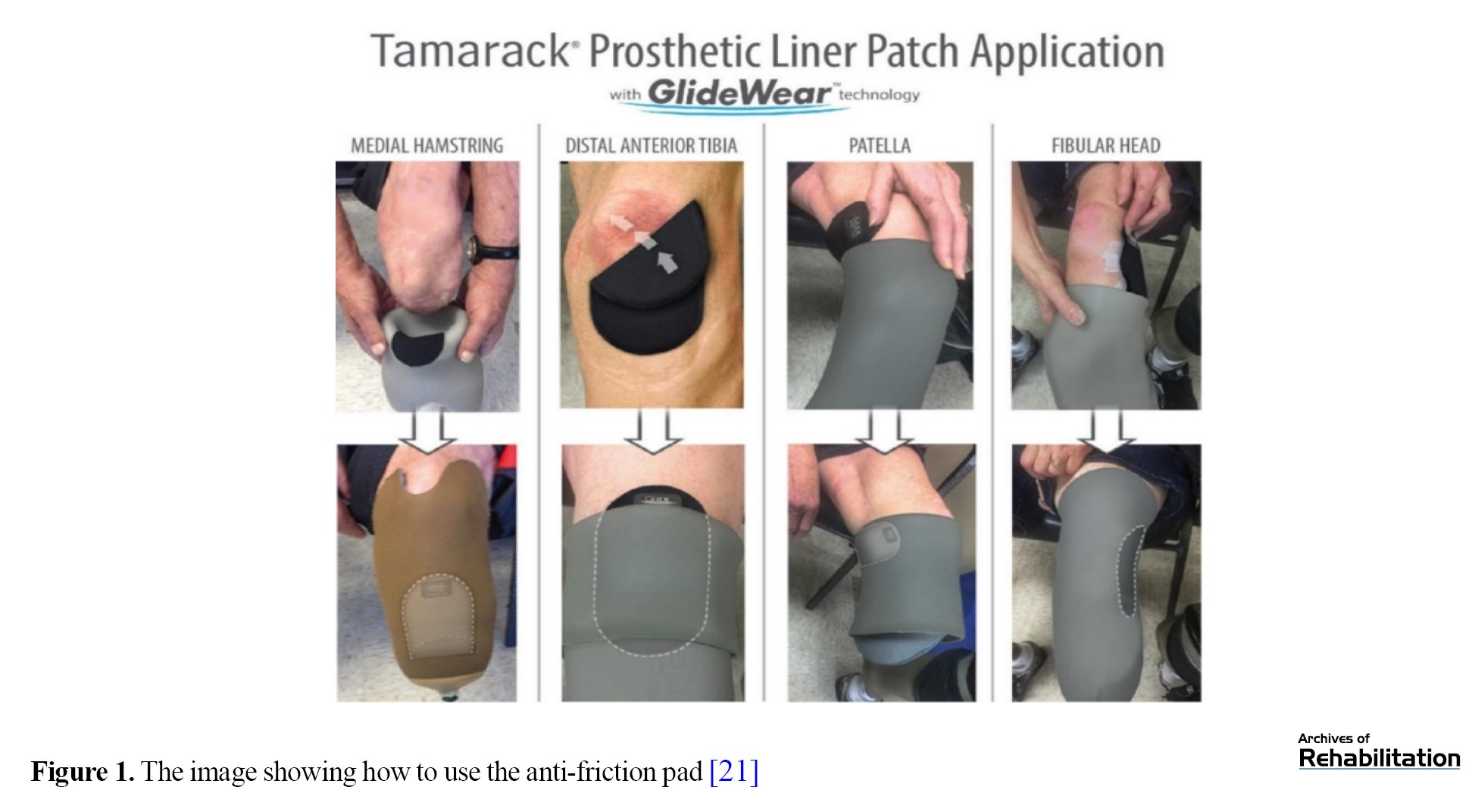
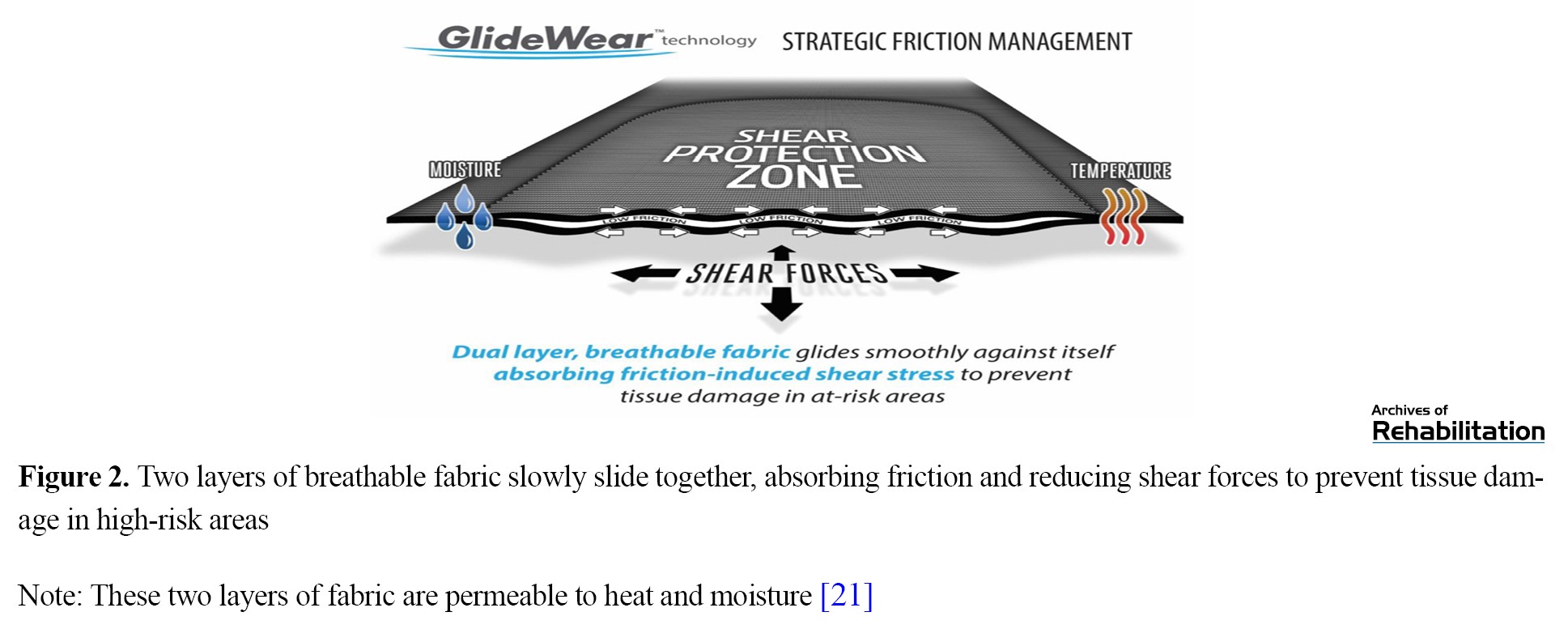
It seems that a spandex anti-friction pad may be a solution to reduce friction between the skin and the gel liner in the patellar tendon and may reduce the pain at this common weight-bearing site. It may help to enhance the ability to walk and satisfaction with the prosthesis in users [21]. To our knowledge, there is no study on the use of spandex anti-friction pads for reducing pain and friction in the patellar tendon of amputees. Therefore, this study aimed to investigate the effect of two-layer spandex anti-friction pads on the pain, standing capability, and walking ability of unilateral transtibial amputees (UTTAs) who had experienced pain, dissatisfaction, and friction in their patellar tendon during daily activities. The structure, materials, and design of this pad are similar to those used in the pad made by the GlideWear™ Company. It should be noted that the area for the pad use is localized, and the overall adherence of the liner to the stump for suspension is not affected.
Materials and Methods
Participants
The present study is a quasi-experimental study with a pre-test-post-test design conducted from July to December 2023 in Karaj, Iran. The study population consisted of individuals with unilateral transtibial amputations at K2 and K3 functional levels presented to the Orthotics and Prosthetics Center of the Red Crescent in Karaj and Tehran, Iran. Of these, 16 people were selected. The inclusion criteria were unilateral transtibial amputation due to trauma, age 18-60 years, having amputation for at least six months, sensory integrity in the stump, experience of using PTB and TSB hybrid sockets, experience of using gel liners and shuttle locks, and having complaints of pain in the patellar tendon due to friction with the gel liner. The contact sensitivity to the gel liner, skin damage for reasons other than friction, and the presence of open wounds or amputations in the upper limb were the exclusion criteria. In this study, G*Power software was used to determine the sample size, considering α=0.05, β=0.2, P0=0.8, and P1=0.9. Participants used prostheses with a proper fit and intact gel liner suitable for the residual limb. Similar prosthetic components were used for all individuals, and the proper alignment for each individual was set according to the bench alignment settings and finally adjusted by an experienced orthotics/prosthetics specialist.
Measures
The visual analog scale (VAS) was used to measure the pain. It was a 10-cm line printed on a piece of paper with markers with endpoints representing “no pain” and “worst pain” or “unbearable pain”. The person places a mark on the line to indicate their pain intensity.
The orthotics and prosthetics user’s survey (OPUS) questionnaire was utilized to assess the patient satisfaction with the prosthesis. It has 21 items rated on a six-point Likert scale: 5 (strongly agree), 4 (agree), 3 (neither agree nor disagree), 2 (disagree), 1 (strongly disagree), and 0 (do not know/not applicable). We used the first 11 items to assess the satisfaction; therefore, the total score ranged from 11 to 55. Participants were first asked to walk for three minutes with their prostheses along a predetermined parallel path in the training hall at their chosen speed. Then, the OPUS was completed by them.
Also, their walking time on a treadmill at 4 kilometers per hour was recorded (in seconds) by using a stopwatch. In this regard, after a 10-minute rest interval, they were instructed to start walking on the treadmill at the mentioned speed. The duration that each participant was able to walk on the treadmill was recorded with the stopwatch.
After resting for 10 minutes, they performed the one-leg standing balance test (OLSTP). In this test, they were asked to stand on their prosthetic leg (keeping the healthy leg bent at the knee beside the prosthetic leg), and the standing duration was recorded by a stopwatch. To prevent test learning by the participants, each test was conducted only once. The tests were performed next to a wall to prevent falls and several foam mats were placed around the participants.
In the next stage, anti-friction pads were prepared according to the size of the patella tendon for each participant and placed on the skin of the residual limb, and the gel liner was pulled over the skin. The application of the anti-friction pad was in accordance with the instructions available on the official website of Tamarack® Habilitation Technologies Inc. (Figure 1). The anti-friction pad of this study consists of two layers of spandex fabric similar to the original sample, with a coefficient of friction between the two layers close to zero. Based on the manufacturer’s instructions, the fabric consisted of 15% spandex or Lycra and 85% Nylon. As a result, the shear and friction forces in the area may be affected by using the smooth sliding property of these two layers over each other (Figure 2). For adaptation, each participant used the anti-friction pad along with their prosthesis for one week Then, we asked them to return again for the final evaluation and all assessments were repeated and data was recorded.
Data analysis
For data analysis, SPSS software, version 26 was used. The Kolmogorov-Smirnov test was employed to assess the normal distribution of statistical data. For analyzing data with a normal distribution (satisfaction and walking time), the paired t-test was used, while for data with abnormal distribution (pain and duration of standing on the prosthetic leg), the Wilcoxon test was used to evaluate the differences between pre-test and post-test phases. The significance level was set at 0.05.
Results
In this study, 11 men and 5 women participated with a mean age of 54.94 years, a weight of 83.19 kg, and a height of 170.25 cm. Table 1 presents the participants’ information.
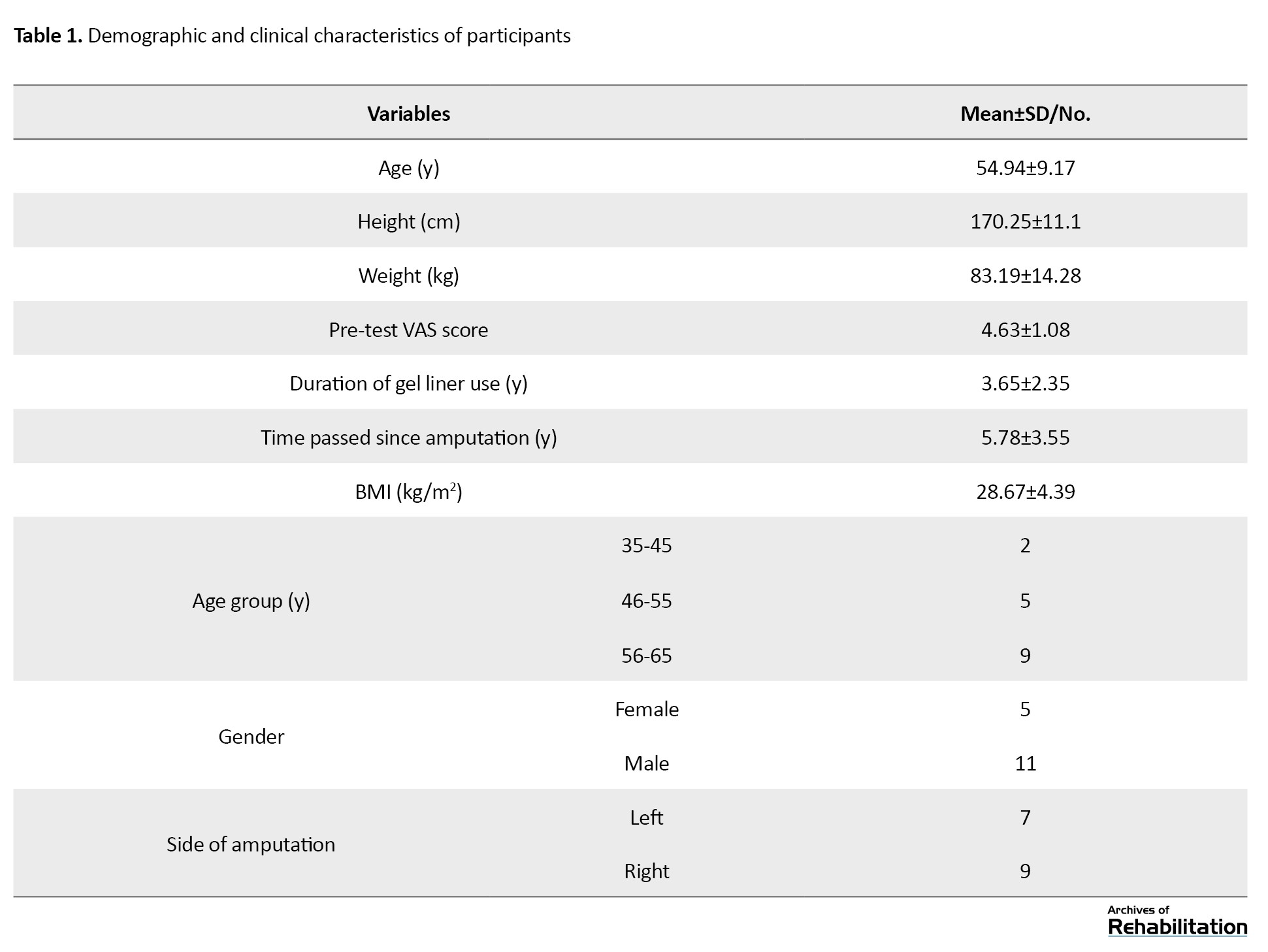
Table 2 presents the results of the comparison using a paired t-test for two variables: satisfaction (OPUS score) and treadmill walking time before and after using the anti-friction pad.
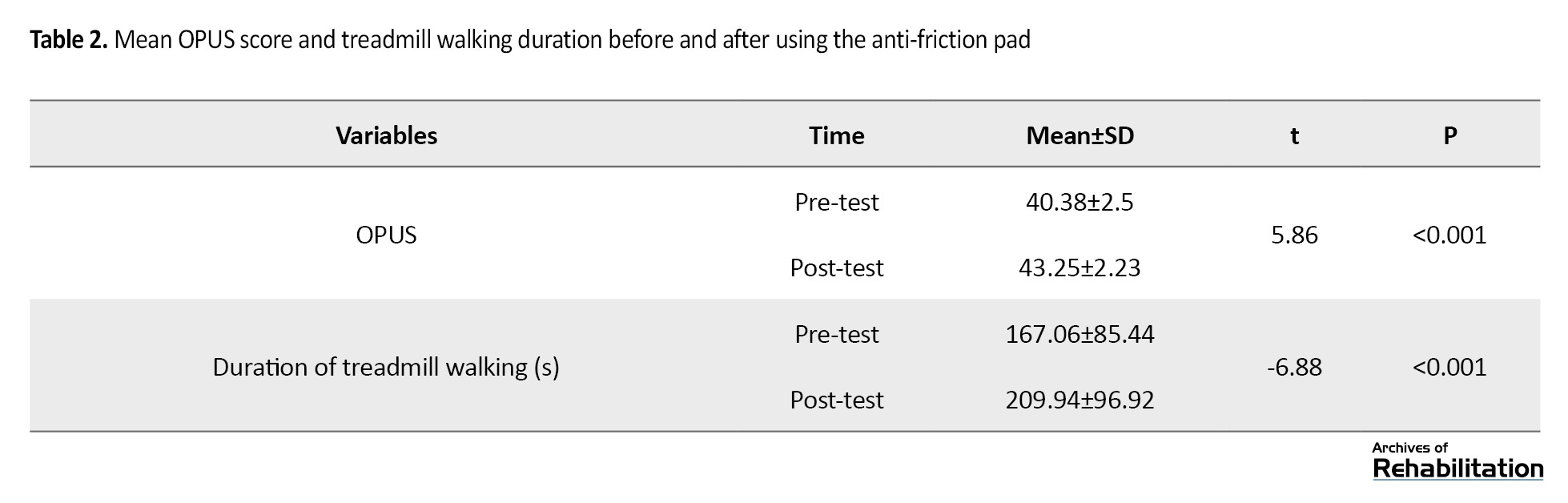
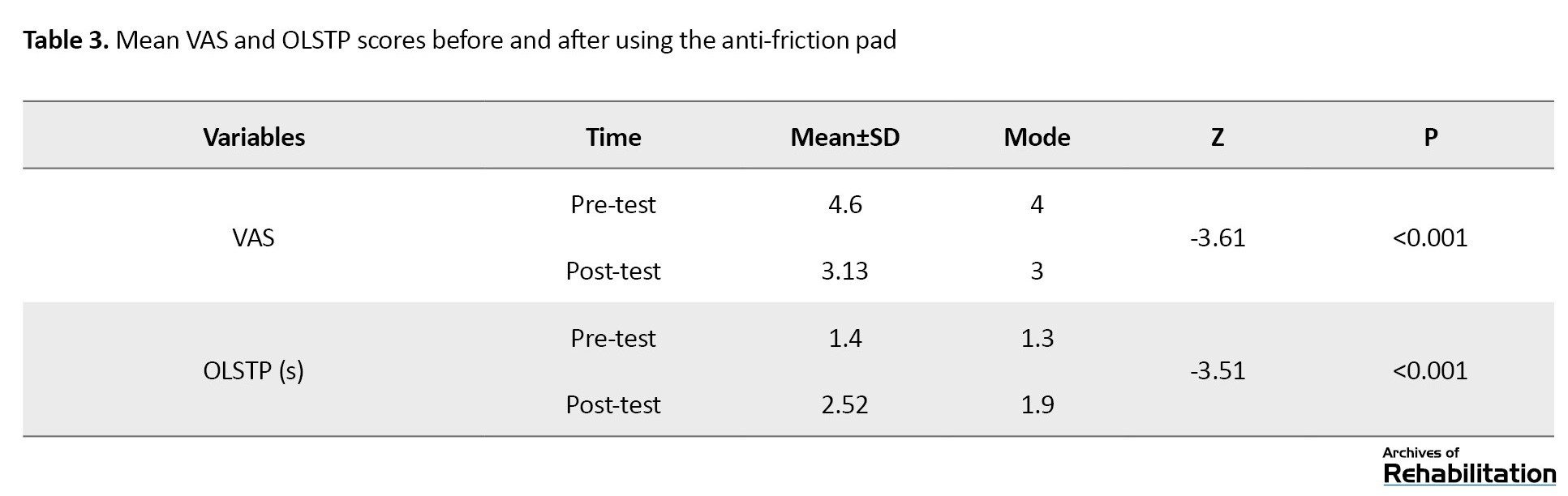
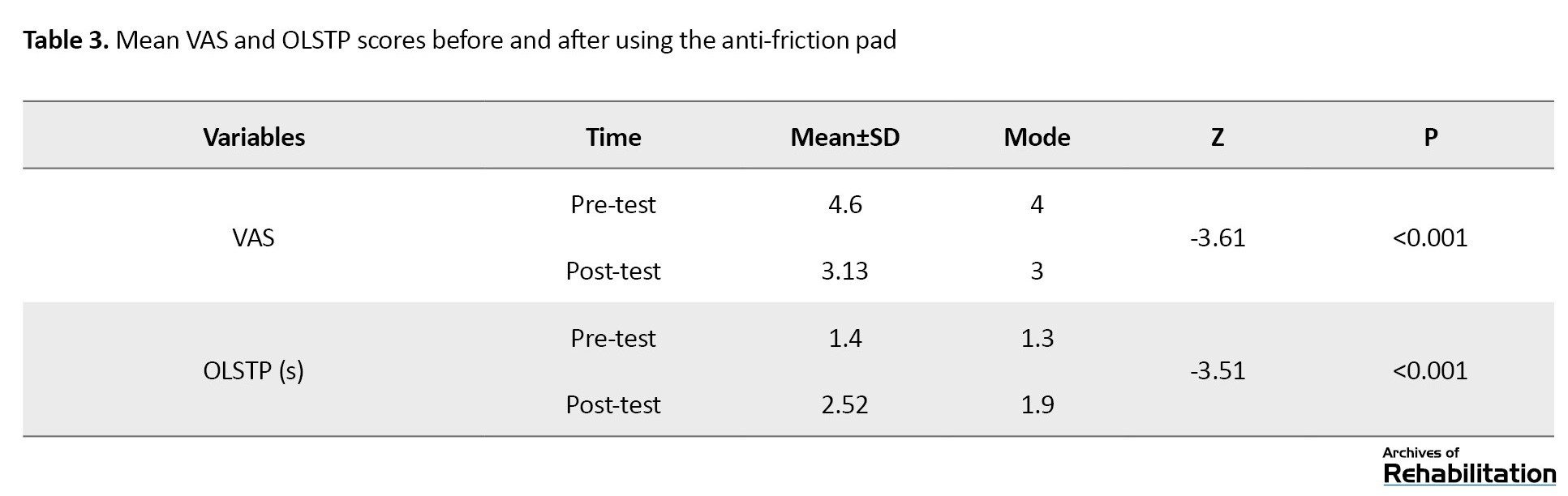
The satisfaction of participants and the duration of walking on the treadmill significantly increased after using the pad (P<0.001). The results of the Wilcoxon test (Table 3) revealed that pain significantly decreased and the standing duration on the prosthetic leg increased significantly after using the anti-friction pad (P<0.001).
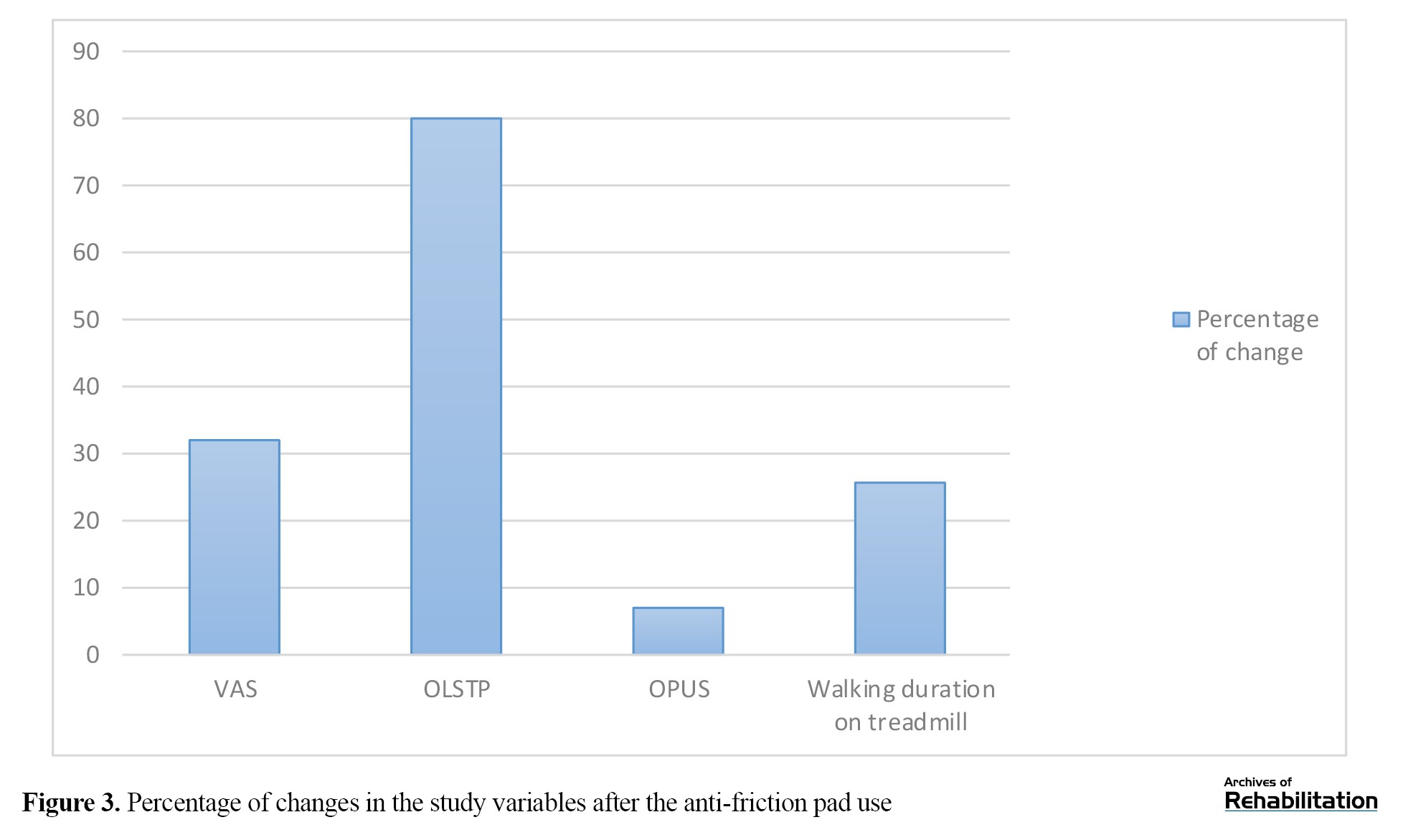
The percentage of changes for each variable based on its initial score is illustrated in Figure 3. As can be seen, the variable of standing duration on the prosthetic leg showed the highest change after using the anti-friction pad in this study, while the satisfaction variable showed only slight changes.
Discussion
This study examined the effectiveness of a two-layer anti-friction pad in reducing the friction in the patellar tendon of residual limb in UTTAs. The results showed that, after one week of using this pad, a significant decrease in pain (VAS score) and an increase in satisfaction with the prosthesis (OPUS score) were observed in the areas that were exposed to greater friction and pressure. Also, the duration of walking at a speed of 4 kilometers per hour on a treadmill and the duration of standing on the prosthetic leg (OLSTP score) significantly increased.
The anti-friction pad use had a significant impact on pain reduction in our study. The results of a similar study on the impact of a four-week walking training program showed that static weight-bearing was significantly related to walking speed, and pain had a significant role in walking speed during transtibial amputee rehabilitation. The study suggested that static weight-bearing can be a predictor of walking speed, which may be changed through pain reduction [26]. This implies that pain reduction can be an important factor related to functional activities and the ability to walk in people with transtibial amputation. Pain can manifest in various ways, such as residual limb pain, phantom pain, and back pain, which can affect the individual’s daily activities [27].
The current study showed that the use of an anti-friction pad significantly increased UTTAs’ satisfaction with the prosthesis after one week. Although the rate of increase was not high, it can be stated that the reduction of friction and pain in the patellar tendon area after using the anti-friction pad had a positive impact on the satisfaction of UTTAs in this study. These factors were then very important for the amputee. It should be noted that the UTTAs used this device for only one week; therefore, its effect on satisfaction was not high. Skin friction is an important issue that 41% of UTTAs may experience. In hybrid sockets and other patellar tendon weight-bearing sockets, the concentration of pressure at a single point and the friction and wear of the stump against the socket in the patellar tendon area are important issues [29]. Therefore, reduced friction might be effective in increasing the satisfaction of prosthetic users in our study.
In another similar study, the effects of reduced contact pressure and tactile sensitivity on long-term treadmill walking were examined. The results showed that the plantar flexor muscles in the contralateral limb experienced fatigue, which may affect the ability of individuals to walk with the prosthetic leg. The inability to complete weight-bearing on the prosthetic side may lead to a shift of weight towards the sound side, resulting in increased discomfort in this side over time [30]. Accordingly, it can be said that by increasing the comfort and reducing the friction in the sockets of participants in our study, the pad caused less pressure on the sound side in addition to the prosthetic side.
In our study, the duration of standing on the prosthetic leg showed the highest percentage of change after the use of the anti-friction pad, compared to other study variables (an 80% increase compared to the pre-test duration). It can be said that the pad increased the weight-bearing capacity of the prosthetic leg, indicating a significant reduction in pressure and friction between the socket and residual limb at weight-bearing areas, as well as increased socket comfort, which in turn increased the duration of standing on the prosthetic leg. Therefore, the pad may help provide smoother walking for prosthetic users; however, laboratory studies with motion analysis cameras are needed to confirm this finding.
There was a lack of similar studies using anti-friction pads for comparison due to the novelty of this study. Other limitations included the small sample size and lack of access to the users of specific prosthetic sockets, including hybrid sockets with gel liner. Additionally, the participants had a mean age of about 50, which can affect the results regarding the standing and walking duration. Another limitation of this study was the lack of complete control over confounding factors such as the users’ skills in using different types of prostheses, which may affect the socket comfort. The participants in this study already had prostheses and it was not possible to fabricate a completely new prosthesis for them. The features of these previously made prostheses may affect the findings. To mitigate this effect, each individual was assessed before and after receiving the spandex anti-friction pad. It is recommended that this study be repeated in other regions of the transtibial residual limb, such as the popliteal area and distal limb, and even in the ischial area of people with transfemoral amputations. Additionally, further studies should be conducted on a higher number of amputees over a longer period to assess the effect of the anti-friction pad on other related variables such as functional performance and activities of daily living.
Conclusion
The use of a spandex anti-friction pad, aiming to reduce pressure and friction between the socket and stump, may reduce pain in the patella tendon area of UTTAs and increase their satisfaction with the prosthetic leg. It can also help them walk greater distances and stand on their prosthetic leg longer. However, to confirm these findings, further studies are needed.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1402.140). Written informed consent was obtained from all participants after explaining the study objectives to them. All ethical issues, such as confidentiality of patient information, participants’ right to leave the study at any time, not charging them for the anti-friction pad, and ensuring compensation for any potential damages, were considered.
Funding
This study was extracted from the master’s thesis of the Erfan Abolhosseni, approved by the Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Conceptualization, and investigation: Erfan Abolhasani and Roshanak Baghaei; Methodology: Gholamreza Aminian; Validation and data analysis: Zahra Jiryaei; Resources and writing: Erfan Abolhasani; Review, editing, and supervision: Gholamreza Aminian.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study and also the Red Crescent Society of Karaj and all the prosthetists for their assistance in this study.
References
The transtibial amputation is the most common type of lower limb amputation, whose rate is increasing due to vascular diseases such as diabetes and trauma [1]. The ratio of transtibial amputation to transfemoral amputation is 2:1 [2]. The risk of creating ulcers and amputations in individuals with diabetes is significantly higher than in non-diabetic individuals. It is estimated that, every 20 seconds, an amputation is performed on a diabetic person somewhere in the world [3]. Amputation creates permanent disability, and the amputee requires a prosthesis for stability, mobility, and performing daily living activities [4].
Socket suspension is an important factor that can affect the mobility and walking of an amputee. The suspension system is an important component of the transtibial prosthesis, responsible for holding the prosthesis on the residual limb during the swing phase of gait. Considering the importance of the prosthetic suspension systems in the rehabilitation process, selecting an appropriate suspension system based on the functional needs and expectations of amputees is a significant step [5, 6]. There are some complications caused by a weak suspension system, including pain, skin ulcers, and abnormal walking due to piston movement (the vertical movement between the socket and the residual limb during the stance and swing phases of gait). This may lead to reduced satisfaction and comfort for the amputee [11-14]. These complications can lead to a decrease in the walking ability of amputees. This factor has always been an important factor for the rehabilitation team in assessing an individual’s potential for walking with a prosthetic leg [15, 16]. To address these issues, the interface between the prosthetic socket and the residual limb, which is made from various materials such as silicone, has been introduced as a gel liner. The gel liner is an expensive commercial product and is difficult for people in developing countries to buy [5].
Silicone has various properties and can be used to make silicone liners for prostheses. It exhibits the highest friction with the skin compared to other materials [17]. This increased level of friction is important for improving the suspension of silicone gel liners, which makes greater adherence of the liner to the skin over the entire residual limb. However, in individuals using gel liner with pin suspension systems, it has been reported that friction increases in the anterior knee region, especially at the patellar tendon, during walking and when a high degree of knee flexion is required, such as prolonged sitting [18]. This friction may lead to some changes in skin, as tissues try to protect themselves from further damage [19, 20]. This problem can also cause increased wear and tear of the gel liner in the patellar tendon area, which can overshadow the benefits of the gel liner [5, 11, 17]. Excessive and prolonged friction, along with relatively high localized pressure between the skin of the residual limb and the gel liner in the patellar tendon can eventually cause hole in this area that are subjected to excessive friction [6]. It seems that the discomfort experienced by individuals from this friction is due to the mismatch between the skin movements of the residual limb and the gel liner [17]. This problem in the patellar tendon area is more common among transtibial amputees using hybrid sockets, because the concept of hybrid socket in below-the-knee prosthetics basically arises from integrating the patellar tendon bearing (PTB) and total surface bearing (TSB) designs. Actually, there is greater weight bearing and friction with the gel liner in PTB design compared to TSB design due to the greater load-bearing and involvement of the patellar tendon [5].
It seems that a spandex anti-friction pad may be a solution to reduce friction between the skin and the gel liner in the patellar tendon and may reduce the pain at this common weight-bearing site. It may help to enhance the ability to walk and satisfaction with the prosthesis in users [21]. To our knowledge, there is no study on the use of spandex anti-friction pads for reducing pain and friction in the patellar tendon of amputees. Therefore, this study aimed to investigate the effect of two-layer spandex anti-friction pads on the pain, standing capability, and walking ability of unilateral transtibial amputees (UTTAs) who had experienced pain, dissatisfaction, and friction in their patellar tendon during daily activities. The structure, materials, and design of this pad are similar to those used in the pad made by the GlideWear™ Company. It should be noted that the area for the pad use is localized, and the overall adherence of the liner to the stump for suspension is not affected.
Materials and Methods
Participants
The present study is a quasi-experimental study with a pre-test-post-test design conducted from July to December 2023 in Karaj, Iran. The study population consisted of individuals with unilateral transtibial amputations at K2 and K3 functional levels presented to the Orthotics and Prosthetics Center of the Red Crescent in Karaj and Tehran, Iran. Of these, 16 people were selected. The inclusion criteria were unilateral transtibial amputation due to trauma, age 18-60 years, having amputation for at least six months, sensory integrity in the stump, experience of using PTB and TSB hybrid sockets, experience of using gel liners and shuttle locks, and having complaints of pain in the patellar tendon due to friction with the gel liner. The contact sensitivity to the gel liner, skin damage for reasons other than friction, and the presence of open wounds or amputations in the upper limb were the exclusion criteria. In this study, G*Power software was used to determine the sample size, considering α=0.05, β=0.2, P0=0.8, and P1=0.9. Participants used prostheses with a proper fit and intact gel liner suitable for the residual limb. Similar prosthetic components were used for all individuals, and the proper alignment for each individual was set according to the bench alignment settings and finally adjusted by an experienced orthotics/prosthetics specialist.
Measures
The visual analog scale (VAS) was used to measure the pain. It was a 10-cm line printed on a piece of paper with markers with endpoints representing “no pain” and “worst pain” or “unbearable pain”. The person places a mark on the line to indicate their pain intensity.
The orthotics and prosthetics user’s survey (OPUS) questionnaire was utilized to assess the patient satisfaction with the prosthesis. It has 21 items rated on a six-point Likert scale: 5 (strongly agree), 4 (agree), 3 (neither agree nor disagree), 2 (disagree), 1 (strongly disagree), and 0 (do not know/not applicable). We used the first 11 items to assess the satisfaction; therefore, the total score ranged from 11 to 55. Participants were first asked to walk for three minutes with their prostheses along a predetermined parallel path in the training hall at their chosen speed. Then, the OPUS was completed by them.
Also, their walking time on a treadmill at 4 kilometers per hour was recorded (in seconds) by using a stopwatch. In this regard, after a 10-minute rest interval, they were instructed to start walking on the treadmill at the mentioned speed. The duration that each participant was able to walk on the treadmill was recorded with the stopwatch.
After resting for 10 minutes, they performed the one-leg standing balance test (OLSTP). In this test, they were asked to stand on their prosthetic leg (keeping the healthy leg bent at the knee beside the prosthetic leg), and the standing duration was recorded by a stopwatch. To prevent test learning by the participants, each test was conducted only once. The tests were performed next to a wall to prevent falls and several foam mats were placed around the participants.
In the next stage, anti-friction pads were prepared according to the size of the patella tendon for each participant and placed on the skin of the residual limb, and the gel liner was pulled over the skin. The application of the anti-friction pad was in accordance with the instructions available on the official website of Tamarack® Habilitation Technologies Inc. (Figure 1). The anti-friction pad of this study consists of two layers of spandex fabric similar to the original sample, with a coefficient of friction between the two layers close to zero. Based on the manufacturer’s instructions, the fabric consisted of 15% spandex or Lycra and 85% Nylon. As a result, the shear and friction forces in the area may be affected by using the smooth sliding property of these two layers over each other (Figure 2). For adaptation, each participant used the anti-friction pad along with their prosthesis for one week Then, we asked them to return again for the final evaluation and all assessments were repeated and data was recorded.
Data analysis
For data analysis, SPSS software, version 26 was used. The Kolmogorov-Smirnov test was employed to assess the normal distribution of statistical data. For analyzing data with a normal distribution (satisfaction and walking time), the paired t-test was used, while for data with abnormal distribution (pain and duration of standing on the prosthetic leg), the Wilcoxon test was used to evaluate the differences between pre-test and post-test phases. The significance level was set at 0.05.
Results
In this study, 11 men and 5 women participated with a mean age of 54.94 years, a weight of 83.19 kg, and a height of 170.25 cm. Table 1 presents the participants’ information.
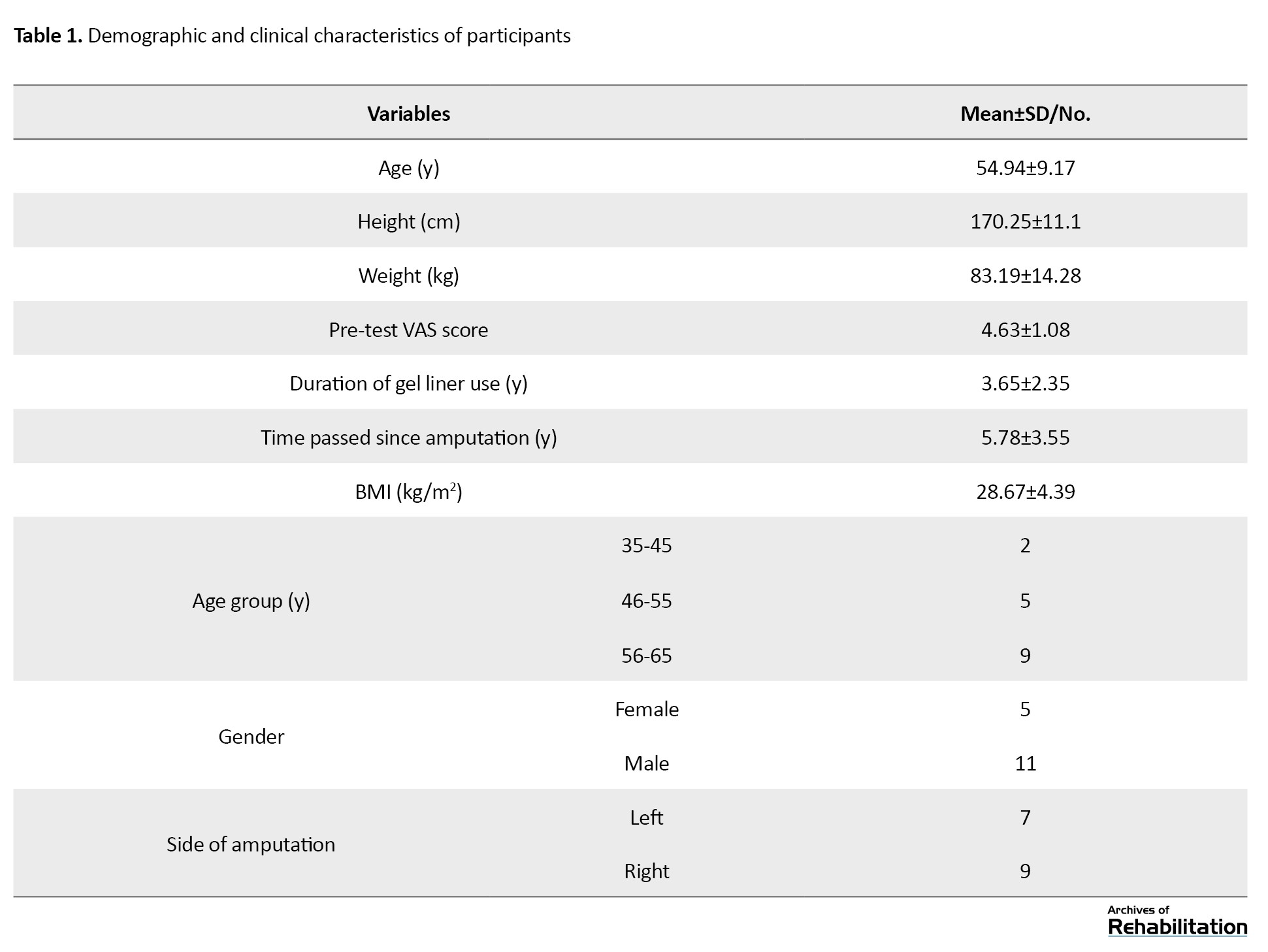
Table 2 presents the results of the comparison using a paired t-test for two variables: satisfaction (OPUS score) and treadmill walking time before and after using the anti-friction pad.
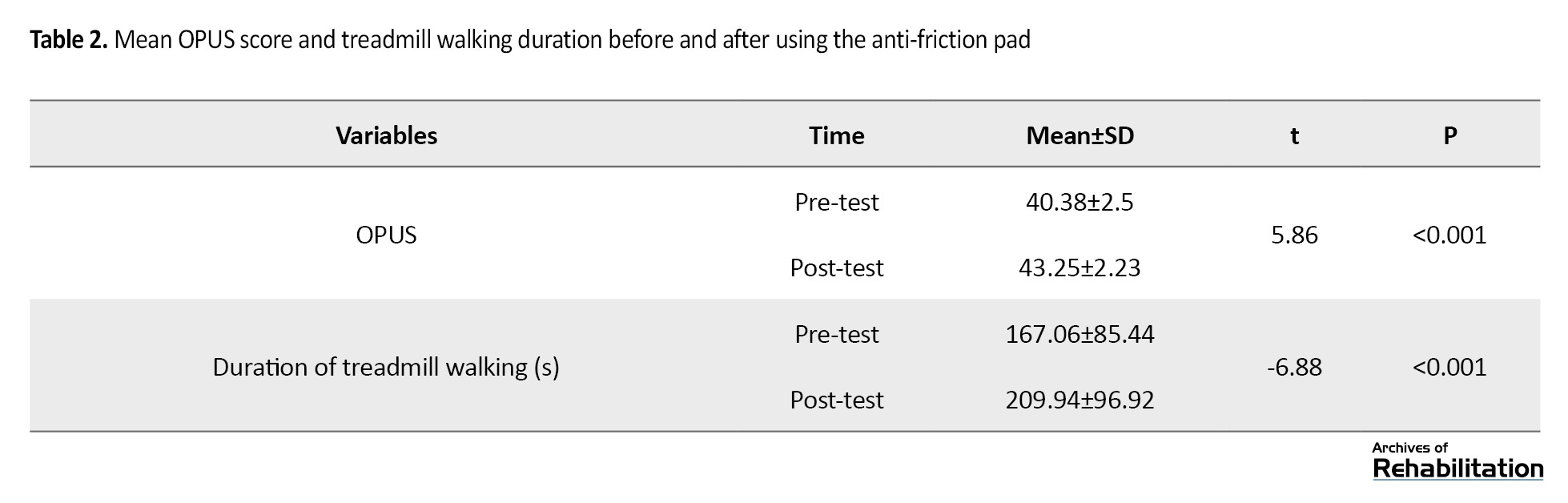
The satisfaction of participants and the duration of walking on the treadmill significantly increased after using the pad (P<0.001). The results of the Wilcoxon test (Table 3) revealed that pain significantly decreased and the standing duration on the prosthetic leg increased significantly after using the anti-friction pad (P<0.001).
The percentage of changes for each variable based on its initial score is illustrated in Figure 3. As can be seen, the variable of standing duration on the prosthetic leg showed the highest change after using the anti-friction pad in this study, while the satisfaction variable showed only slight changes.
Discussion
This study examined the effectiveness of a two-layer anti-friction pad in reducing the friction in the patellar tendon of residual limb in UTTAs. The results showed that, after one week of using this pad, a significant decrease in pain (VAS score) and an increase in satisfaction with the prosthesis (OPUS score) were observed in the areas that were exposed to greater friction and pressure. Also, the duration of walking at a speed of 4 kilometers per hour on a treadmill and the duration of standing on the prosthetic leg (OLSTP score) significantly increased.
The anti-friction pad use had a significant impact on pain reduction in our study. The results of a similar study on the impact of a four-week walking training program showed that static weight-bearing was significantly related to walking speed, and pain had a significant role in walking speed during transtibial amputee rehabilitation. The study suggested that static weight-bearing can be a predictor of walking speed, which may be changed through pain reduction [26]. This implies that pain reduction can be an important factor related to functional activities and the ability to walk in people with transtibial amputation. Pain can manifest in various ways, such as residual limb pain, phantom pain, and back pain, which can affect the individual’s daily activities [27].
The current study showed that the use of an anti-friction pad significantly increased UTTAs’ satisfaction with the prosthesis after one week. Although the rate of increase was not high, it can be stated that the reduction of friction and pain in the patellar tendon area after using the anti-friction pad had a positive impact on the satisfaction of UTTAs in this study. These factors were then very important for the amputee. It should be noted that the UTTAs used this device for only one week; therefore, its effect on satisfaction was not high. Skin friction is an important issue that 41% of UTTAs may experience. In hybrid sockets and other patellar tendon weight-bearing sockets, the concentration of pressure at a single point and the friction and wear of the stump against the socket in the patellar tendon area are important issues [29]. Therefore, reduced friction might be effective in increasing the satisfaction of prosthetic users in our study.
In another similar study, the effects of reduced contact pressure and tactile sensitivity on long-term treadmill walking were examined. The results showed that the plantar flexor muscles in the contralateral limb experienced fatigue, which may affect the ability of individuals to walk with the prosthetic leg. The inability to complete weight-bearing on the prosthetic side may lead to a shift of weight towards the sound side, resulting in increased discomfort in this side over time [30]. Accordingly, it can be said that by increasing the comfort and reducing the friction in the sockets of participants in our study, the pad caused less pressure on the sound side in addition to the prosthetic side.
In our study, the duration of standing on the prosthetic leg showed the highest percentage of change after the use of the anti-friction pad, compared to other study variables (an 80% increase compared to the pre-test duration). It can be said that the pad increased the weight-bearing capacity of the prosthetic leg, indicating a significant reduction in pressure and friction between the socket and residual limb at weight-bearing areas, as well as increased socket comfort, which in turn increased the duration of standing on the prosthetic leg. Therefore, the pad may help provide smoother walking for prosthetic users; however, laboratory studies with motion analysis cameras are needed to confirm this finding.
There was a lack of similar studies using anti-friction pads for comparison due to the novelty of this study. Other limitations included the small sample size and lack of access to the users of specific prosthetic sockets, including hybrid sockets with gel liner. Additionally, the participants had a mean age of about 50, which can affect the results regarding the standing and walking duration. Another limitation of this study was the lack of complete control over confounding factors such as the users’ skills in using different types of prostheses, which may affect the socket comfort. The participants in this study already had prostheses and it was not possible to fabricate a completely new prosthesis for them. The features of these previously made prostheses may affect the findings. To mitigate this effect, each individual was assessed before and after receiving the spandex anti-friction pad. It is recommended that this study be repeated in other regions of the transtibial residual limb, such as the popliteal area and distal limb, and even in the ischial area of people with transfemoral amputations. Additionally, further studies should be conducted on a higher number of amputees over a longer period to assess the effect of the anti-friction pad on other related variables such as functional performance and activities of daily living.
Conclusion
The use of a spandex anti-friction pad, aiming to reduce pressure and friction between the socket and stump, may reduce pain in the patella tendon area of UTTAs and increase their satisfaction with the prosthetic leg. It can also help them walk greater distances and stand on their prosthetic leg longer. However, to confirm these findings, further studies are needed.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR.USWR.REC.1402.140). Written informed consent was obtained from all participants after explaining the study objectives to them. All ethical issues, such as confidentiality of patient information, participants’ right to leave the study at any time, not charging them for the anti-friction pad, and ensuring compensation for any potential damages, were considered.
Funding
This study was extracted from the master’s thesis of the Erfan Abolhosseni, approved by the Department of Orthotics and Prosthetics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Conceptualization, and investigation: Erfan Abolhasani and Roshanak Baghaei; Methodology: Gholamreza Aminian; Validation and data analysis: Zahra Jiryaei; Resources and writing: Erfan Abolhasani; Review, editing, and supervision: Gholamreza Aminian.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their cooperation in this study and also the Red Crescent Society of Karaj and all the prosthetists for their assistance in this study.
References
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation. 2008; 89(3):422-9. [DOI:10.1016/j.apmr.2007.11.005] [PMID]
- Marino M, Pattni S, Greenberg M, Miller A, Hocker E, Ritter S, et al. Access to prosthetic devices in developing countries: Pathways and challenges. Paper presented at: 2015 IEEE Global Humanitarian Technology Conference (GHTC); 2015 October 8; Seattle, USA. [DOI:10.1109/GHTC.2015.7343953]
- Modares Sabzevari MH, Anbarian M, Safari MR, Tabatabai SF, Razi M J. [Biomechanical analysis of the effect of solid ankle cushion heel and dynamic feet during running of individuals with unilateral transtibial amputations (Persian)]. Archives of Rehabilitation. 2022; 23(1):126-39. [DOI:10.32598/RJ.23.1.3317.1]
- Bacarin TA, Sacco IC, Hennig EM. Plantar pressure distribution patterns during gait in diabetic neuropathy patients with a history of foot ulcers. Clinics. 2009; 64(2):113-20. [DOI:10.1590/S1807-59322009000200008] [PMID]
- Baars EC, Geertzen JH. Literature review of the possible advantages of silicon liner socket use in trans-tibial prostheses. Prosthetics and Orthotics International. 2005; 29(1):27-37. [DOI:10.1080/17461550500069612] [PMID]
- Gholizadeh H, Abu Osman NA, Eshraghi A, Ali S, Razak NA. Transtibial prosthesis suspension systems: Systematic review of literature. Clinical Biomechanics. 2014; 29(1):87-97. [DOI:10.1016/j.clinbiomech.2013.10.013] [PMID]
- Gholizadeh H, Abu Osman NA, Eshraghi A, Ali S, Yahyavi ES. Satisfaction and problems experienced with transfemoral suspension systems: A comparison between common suction socket and seal-in liner. Archives of Physical Medicine and Rehabilitation. 2013; 94(8):1584-9. [DOI:10.1016/j.apmr.2012.12.007] [PMID]
- Kapp S. Suspension systems for prostheses. Clinical Orthopaedics and Related Research. 1999; (361):55-62. [DOI:10.1097/00003086-199904000-00008] [PMID]
- Schaffalitzky E, Gallagher P, Maclachlan M, Wegener ST. Developing consensus on important factors associated with lower limb prosthetic prescription and use. Disability and Rehabilitation. 2012; 34(24):2085-94. [DOI:10.3109/09638288.2012.671885] [PMID]
- Van de Weg FB, Van der Windt DA. A questionnaire survey of the effect of different interface types on patient satisfaction and perceived problems among trans-tibial amputees. Prosthetics and Orthotics International. 2005; 29(3):231-9. [DOI:10.1080/03093640500199679] [PMID]
- Gholizadeh H, Osman NA, Kamyab M, Eshraghi A, Abas WA, Azam MN. Transtibial prosthetic socket pistoning: static evaluation of seal-in(®) x5 and dermo(®) liner using motion analysis system. Clinical Biomechanics. 2012; 27(1):34-9. [DOI:10.1016/j.clinbiomech.2011.07.004] [PMID]
- Goswami J, Lynn R, Street G, Harlander M. Walking in a vacuum-assisted socket shifts the stump fluid balance. Prosthetics and Orthotics International. 2003; 27(2):107-13. [DOI:10.1080/03093640308726666] [PMID]
- McCurdie I, Hanspal R, Nieveen R. ICEROSS--A consensus view: a questionnaire survey of the use of ICEROSS in the United Kingdom. Prosthetics and Orthotics International. 1997; 21(2):124-8. [DOI:10.3109/03093649709164540] [PMID]
- Kristinsson O. The ICEROSS concept: A discussion of a philosophy. Prosthetics and Orthotics International. 1993; 17(1):49-55. [DOI:10.3109/03093649309164354] [PMID]
- Newton RL, Morgan D, Schreiber MH. Radiological evaluation of prosthetic fit in below-the-knee amputees. Skeletal Radiology. 1988; 17(4):276-80. [DOI:10.1007/BF00401811] [PMID]
- Batten HR, McPhail SM, Mandrusiak AM, Varghese PN, Kuys SS. Gait speed as an indicator of prosthetic walking potential following lower limb amputation. Prosthetics and Orthotics International. 2019; 43(2):196-203. [DOI:10.1177/0309364618792723] [PMID]
- Zarezadeh F, Arazpour M, Bahramizadeh M, Mardani MA. [Comparing the effect of new silicone foot prosthesis and conventional foot prosthesis on plantar pressure in diabetic patients with transmetatarsal amputation (Persian)]. Archives of Rehabilitation. 2019; 20(2):124-35. [DOI:10.32598/rj.20.2.124]
- Hachisuka K, Nakamura T, Ohmine S, Shitama H, Shinkoda K. Hygiene problems of residual limb and silicone liners in transtibial amputees wearing the total surface bearing socket. Archives of Physical Medicine and Rehabilitation. 2001; 82(9):1286-90. [DOI:10.1053/apmr.2001.25154] [PMID]
- Baars ECT, Dijkstra PU, Geertzen JH. Skin problems of the stump and hand function in lower limb amputees: A historic cohort study. Prosthetics and Orthotics International. 2008; 32(2):179-85. [DOI:10.1080/03093640802016456] [PMID]
- Bui KM, Raugi GJ, Nguyen VQ, Reiber GE. Skin problems in individuals with lower-limb loss: Literature review and proposed classification system. Journal of Rehabilitation Research and Development. 2009; 46(9):1085-90. [DOI:10.1682/JRRD.2009.04.0052] [PMID]
- Lee Childers W, Wurdeman SR. Transtibial Amputation: Prosthetic Management. In: Krajbich JI, Pinzur MS, Potter BK, Stevens PM, editors. Atlas of Amputations and Limb Deficiencies. Philadelphia: Wolters Kluwer Health; 2018. [Link]
- Tamarack Habilitation Technologies, Inc. How GlideWear™ Works. Minnesota: Tamarack Habilitation Technologies, Inc; 2025. [Link]
- Highsmith JM. Skin Problems in the Amputee. In: Krajbich JI, Pinzur MS, Potter BK, Stevens PM, editors. Atlas of Amputations and Limb Deficiencies. Philadelphia: Wolters Kluwer Health; 2018. [Link]
- Li S, Melton DH, Li S. Tactile, thermal, and electrical thresholds in patients with and without phantom limb pain after traumatic lower limb amputation. Journal of Pain Research. 2015; 8:169-74. [DOI:10.2147/JPR.S77412] [PMID]
- Kark L, Simmons A. Patient satisfaction following lower-limb amputation: The role of gait deviation. Prosthetics and Orthotics International. 2011; 35(2):225-33. [DOI:10.1177/0309364611406169] [PMID]
- Jones ME, Bashford GM, Bliokas VV. Weight-bearing, pain and walking velocity during primary transtibial amputee rehabilitation. Clinical Rehabilitation. 2001; 15(2):172-6. [DOI:10.1191/026921501676151107] [PMID]
- Morgan SJ, Friedly JL, Amtmann D, Salem R, Hafner BJ. Cross-sectional assessment of factors related to pain intensity and pain interference in lower limb prosthesis users. Archives of Physical Medicine and Rehabilitation. 2017; 98(1):105-113. [DOI:10.1016/j.apmr.2016.09.118] [PMID]
- Baghbanbashi A, Farahmand B, Azadinia F, Jalali M. Evaluation of user's satisfaction with orthotic and prosthetic devices and services in orthotics and prosthetics center of Iran University of Medical Sciences. Canadian Prosthetics & Orthotics Journal. 2022; 5(1):37981. [DOI:10.33137/cpoj.v5i1.37981] [PMID]
- Chatterjee S, Majumder S, RoyChowdhury A, Pal S. Problems with use of trans-tibial prosthesis. Journal of Medical Imaging and Health Informatics. 2016; 6(2):269-84. [DOI:10.1166/jmihi.2016.1686]
- Yeung LF, Leung AK, Zhang M, Lee WC. Effects of long-distance walking on socket-limb interface pressure, tactile sensitivity and subjective perceptions of trans-tibial amputees. Disability and Rehabilitation. 2013; 35(11):888-93. [DOI:10.3109/09638288.2012.712197] [PMID]
Type of Study: Original |
Subject:
Orthotics & Prosthetics
Received: 23/09/2024 | Accepted: 11/05/2025 | Published: 1/10/2025
Received: 23/09/2024 | Accepted: 11/05/2025 | Published: 1/10/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |