Volume 25, Issue 4 (Winter 2025)
jrehab 2025, 25(4): 890-905 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gallego-Peñalver F J, Cía-Blasco P, Gómez-Trullén E M. Unilateral Psoas Muscle Atrophy as a Possible Risk Factor for Low Back Pain After Total Hip Arthroplasty: A Case Report. jrehab 2025; 25 (4) :890-905
URL: http://rehabilitationj.uswr.ac.ir/article-1-3463-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3463-en.html
1- Department of Physical Medicine and Nursing, Faculty of Zaragoza, iHealthy Research Group, IIS Aragón, Zaragoza, Spain. & Rehabilitation Department, Hospital Obispo Polanco, Teruel, Spain. , franciscojosegp@gmail.com
2- Rehabilitation Department, Hospital Obispo Polanco, Teruel, Spain., C. San Juan Bosco, 15, 50009, Zaragoza. Spain.
3- Pain Unit, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain.
2- Rehabilitation Department, Hospital Obispo Polanco, Teruel, Spain., C. San Juan Bosco, 15, 50009, Zaragoza. Spain.
3- Pain Unit, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain.
Keywords: Total hip replacement, Postoperative complications, Psoas muscle, Muscular atrophy, Low back pain
Full-Text [PDF 2231 kb]
(664 Downloads)
| Abstract (HTML) (5485 Views)
Full-Text: (1031 Views)
Introduction
Lumbar pain is highly prevalent and is the leading cause of work disability in young people. It is estimated that two-thirds of adults experience low back pain (LBP) at some point in their lives, and 10% will develop chronic LBP [۱]. One of the most common causes of LBP is intervertebral disk degeneration. The etiology of intervertebral disk degeneration is multifactorial and is related, in most cases, to occupational activities and lifestyle, particularly factors such as obesity and smoking [۲]. The aging process contributes physiologically to intervertebral disk degeneration; it is estimated that by the age of 70, the water content of the nucleus pulposus decreases to 70% [۳]. Other causes that accelerate the degenerative process include infectious diseases, inflammatory processes, trauma, or biomechanical changes [۲، ۴]. In addition to the factors mentioned above, alterations in muscle function and biomechanical factors play crucial roles in developing and exacerbating LBP [۵]. Deficits in muscle strength and coordination may contribute to abnormal loading patterns on the spine, further exacerbating degenerative processes and increasing the risk of low back pain [۶].
Understanding the complex interplay between biomechanical factors and muscle function in LBP holds significant implications for addressing related conditions, such as the potential complications of total hip arthroplasty (THA). Recent studies indicate a correlation between THA and unilateral atrophy of the psoas muscle (PM) on the implant side, raising the possibility that this atrophy may be a late complication of surgery [۷]. The location of PM makes it a crucial stabilizer of the spine, influencing both static posture and lumbar spine dynamics [۸، ۹]. PM atrophy significantly impacts lumbar spine biomechanics and may contribute to the development of degenerative disk diseases.
In this context, we present the clinical case of a 53-year-old man who had previously undergone right THA. Eight years post-surgery, the patient experienced a chronic condition of lumbosciatalgia radiating to the left leg and weakness in the right hip flexion. Clinical and radiological analysis revealed the presence of an extruded L5–S1 disk herniation and unilateral atrophy of the PM on the same side of the arthroplasty. While the patient experienced some improvement with a conservative pharmacological and rehabilitative approach, complete recovery was not achieved, possibly due to the extended period of evolution of his condition. This prolonged evolution could have caused irreversible damage to the affected anatomical structures, limiting the patient’s ability to recover fully. This article will delve into the clinical case, explore the connection between PM atrophy and lumbar disk degeneration, and emphasize the importance of early detection and comprehensive management in patients with PM atrophy following THA.
Aside from illustrating a unique scenario, this clinical case has served as the starting point for an ongoing research endeavor, underscoring its value in the realm of medicine and routine clinical practice, especially in rehabilitation. This research was approved by the CEICA (Research Ethics Committee of the Autonomous Community of Aragon) under reference number C.P.-C.I.-PI21/346 and has been registered in the ClinicalTrials.gov database under the identifier NCT05647629.
Clinical Case
We present a 53-year-old male who presented to the Emergency Service of Hospital Clínico Lozano Blesa with an acute episode of left sciatica. He had been experiencing this pain for the past 12 hours before arriving at the Emergency Department, and it was rated 9/10 on the numerical rating scale. The patient denied any history of LBP or leg radiation prior to presentation. It w:::as char:::acterized by its mechanical nature and radiation to the left lower extremity, extending to the ankle and the first toe. The patient did not exhibit febrile symptoms or report recent traumas at admission. Radicular stretching and positive Lasegue and Bragard tests worsened the pain. Additional physical examination revealed pain in the quadratus lumborum and spinal erector muscles, with neuropathic radiation from the back of the leg to the foot. Motor weakness 2/5 in Kendall’s muscle grading system was observed in the extension of the left first toe (extensor digitorum longus) and in plantar flexion of the left ankle (triceps surae), as well as moderate weakness 2/5 in the flexion of the right hip, with the rest of the lumbosacral myotomes being normal. Sensory examination revealed hypoesthesia and hypoalgesia in the left S1 dermatome but no alterations in the other dermatomes. No sensory disturbances related to the cauda equina were observed, and no signs of sphincter dysfunction were detected.
Anamnesis and Radiological Evaluation
Upon reviewing the patient’s medical history, we found that he underwent right THA in April 2012 due to progressive unilateral coxarthrosis over the past two years. Four weeks after surgery, the patient completed six sessions of physiotherapy. In these sessions, the patient was instructed and evaluated on performing muscle strengthening exercises for the hip (gluteals, iliopsoas, adductors, quadriceps, and hamstrings), in addition to gait re-education. The patient reported mild weakness in right hip flexion and pain in the right inguinal region but no lumbar pain. These symptoms were considered common postoperative sequelae. THA, performed through a lateral approach with an SL-Plus+Epfit prosthesis, was indicated in response to hip osteoarthritis grade 3 according to the Kellgren–Lawrence classification (Figure 1).

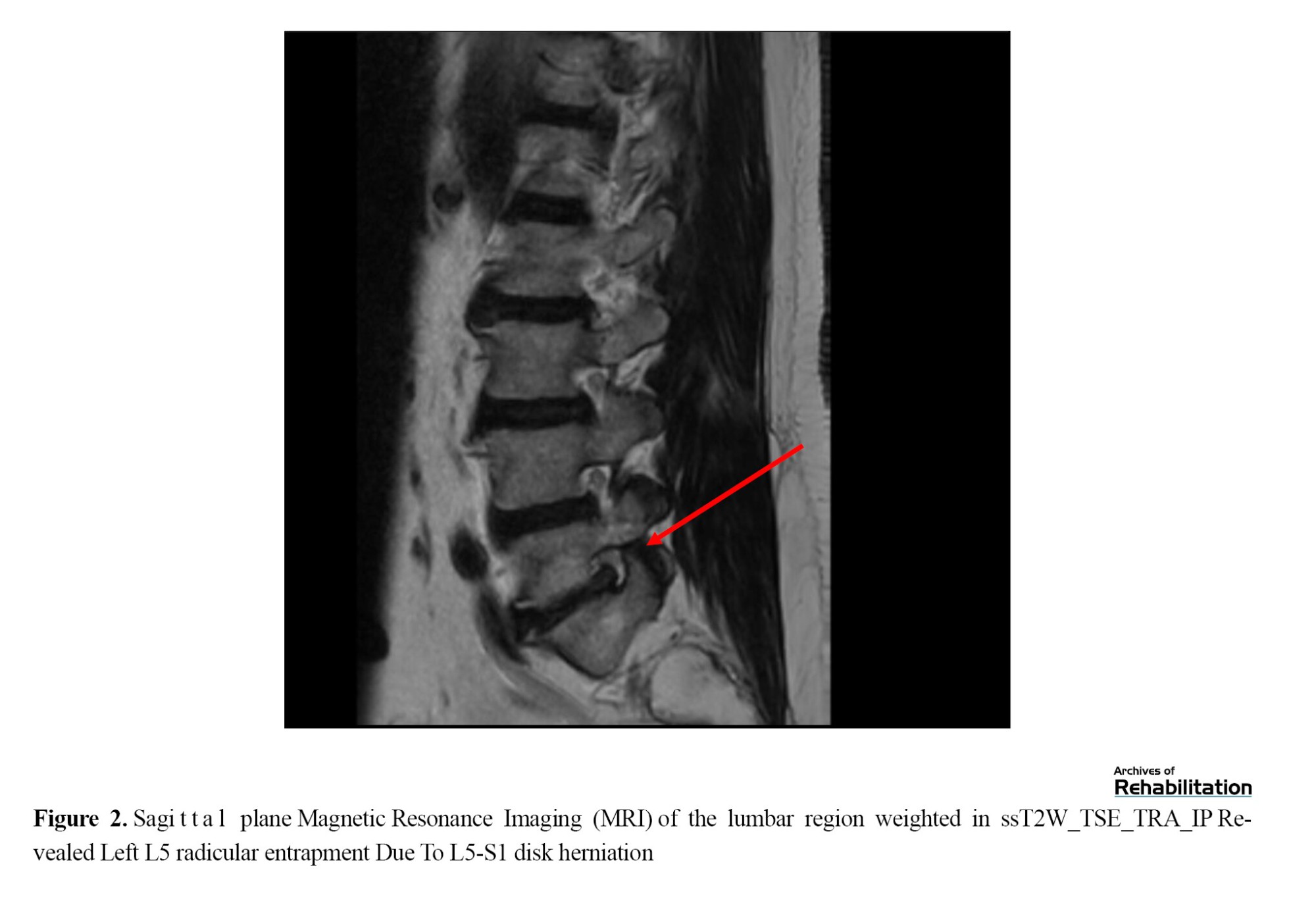
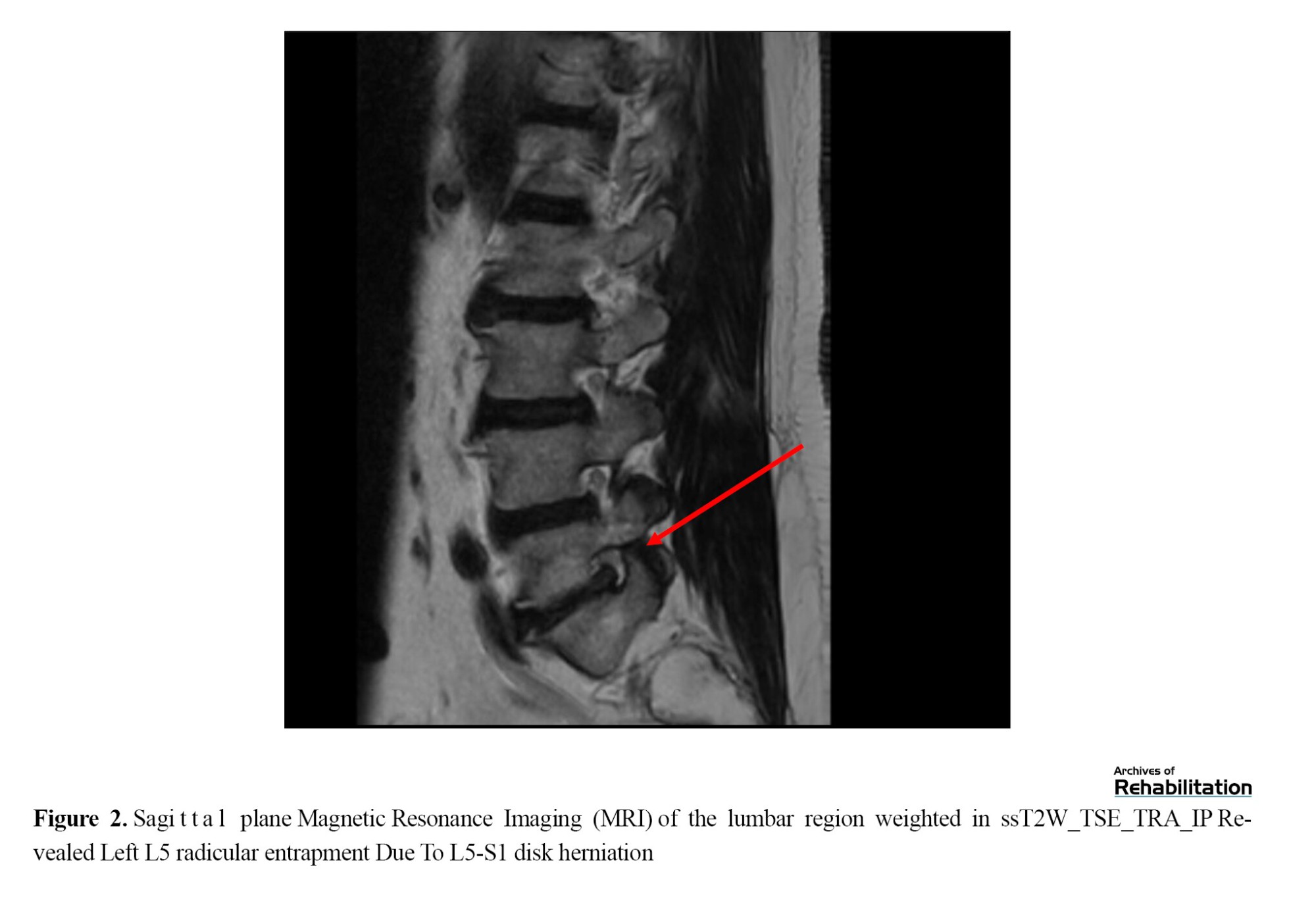
The current evaluation recorded a body mass index of 29.58 kg/m2. Lumbar X-rays did not reveal substantial findings, but lumbar magnetic resonance imaging (MRI) revealed the presence of a left paramedian disk herniation at the L5–S1 level, accompanied by a voluminous sequestered disk fragment in an extraforaminal location (Figure 2).
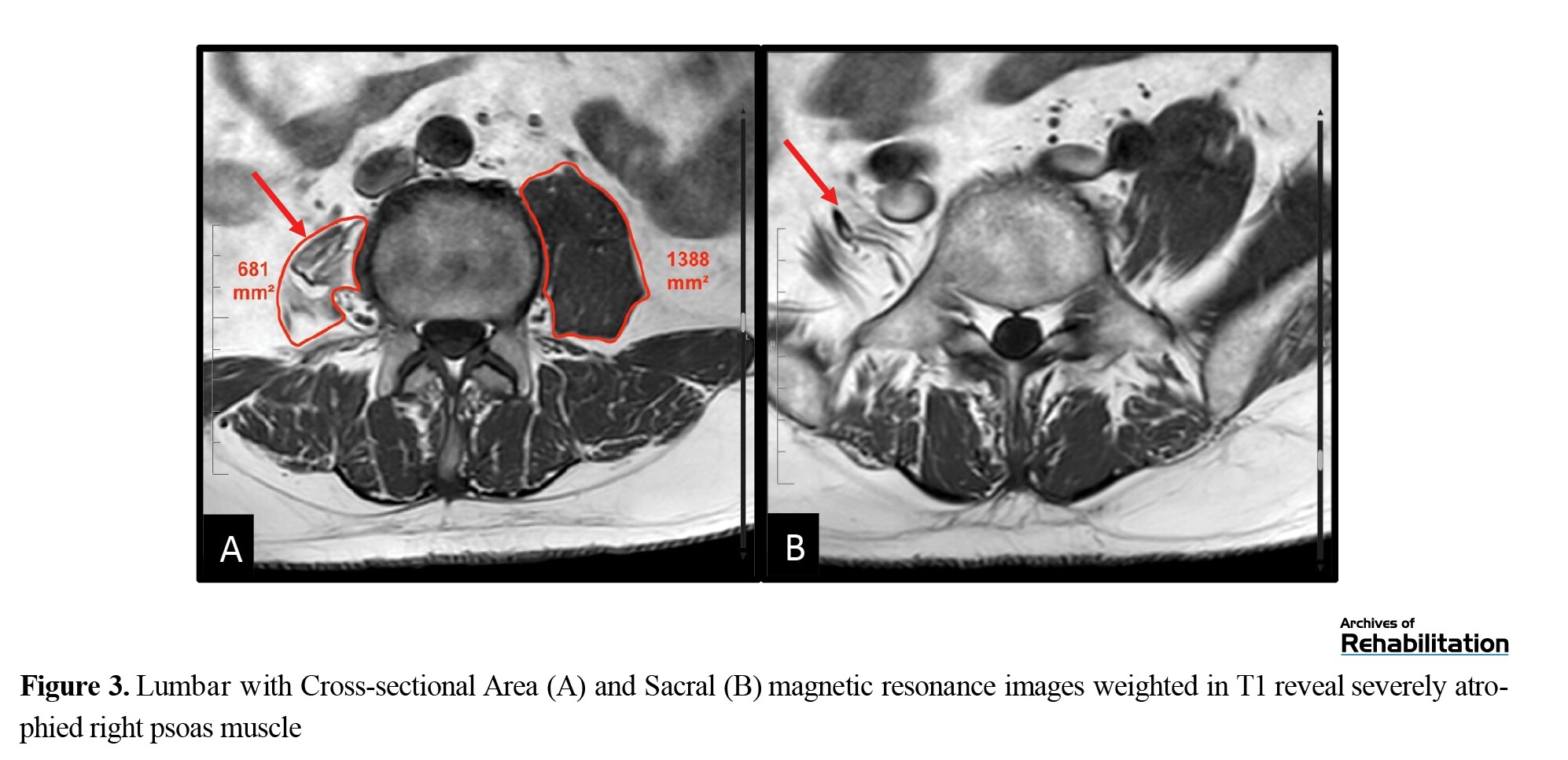
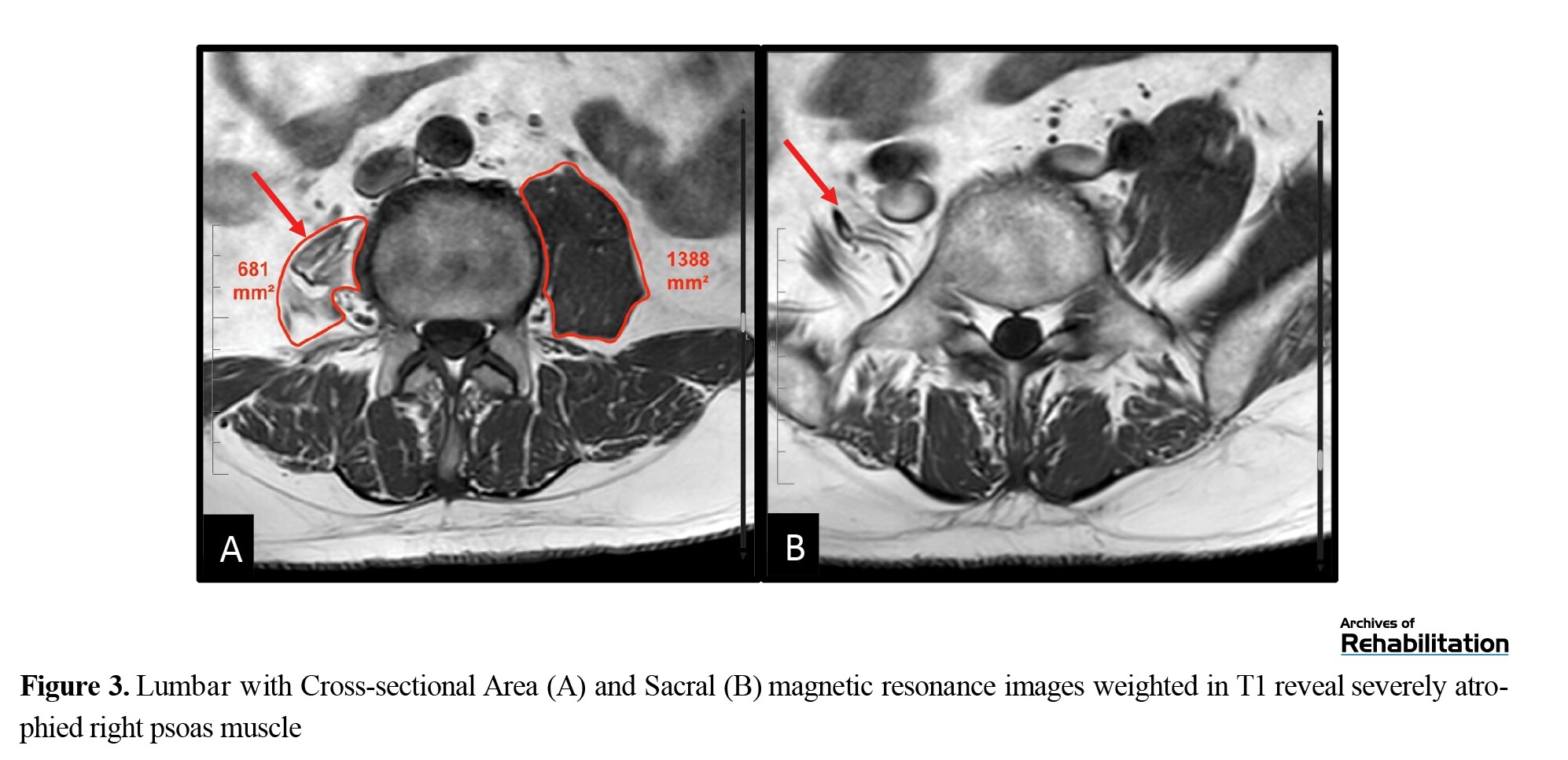
Marked atrophy of the right PM was highlighted and accentuated by adipose tissue infiltration in the same region. The cross-sectional area (CSA) of the PM was quantified bilaterally by a radiologist at the L3–L4 intervertebral disk, obtaining a section of 681 mm² on the right side, with a Goutallier score of 3 indicates severe muscular atrophy. The left side showed a CSA of 1388 mm², with a Goutallier score of 0 (Figure 3A). The right and left psoas/disk CSA indices were calculated as 0.49 and 0.99, respectively. MRI revealed sections of the PM where the muscular belly was absent (Figure 3B). These findings demonstrated the pathology, excluding alternative neuromuscular and central nervous system diseases.
Evolution
Because of the intensity of pain and clinical manifestations, the patient was admitted to the Neurosurgery Department and treated with opioid-derived analgesia. In addition, caudal epidural injection with local anesthetic and corticosteroid was performed, resulting in a favorable response. The patient was discharged after two days of admission, and a rehabilitation program was initiated through 15 sessions of physiotherapy with exercises focused on strengthening the flexor muscles of the right hip, with special attention to PM, lumbopelvic stabilization exercises, stretches for the erector muscles of the back, transcutaneous electrical nerve stimulation electroanalgesia, and sciatic nerve neurodynamics. Gait retraining was also integral to the therapeutic plan, correcting antialgic anomalous patterns and improving movement dynamics. An electromyogram performed on an outpatient basis revealed a chronic pattern of radicular suffering with denervation of the left S1 root.
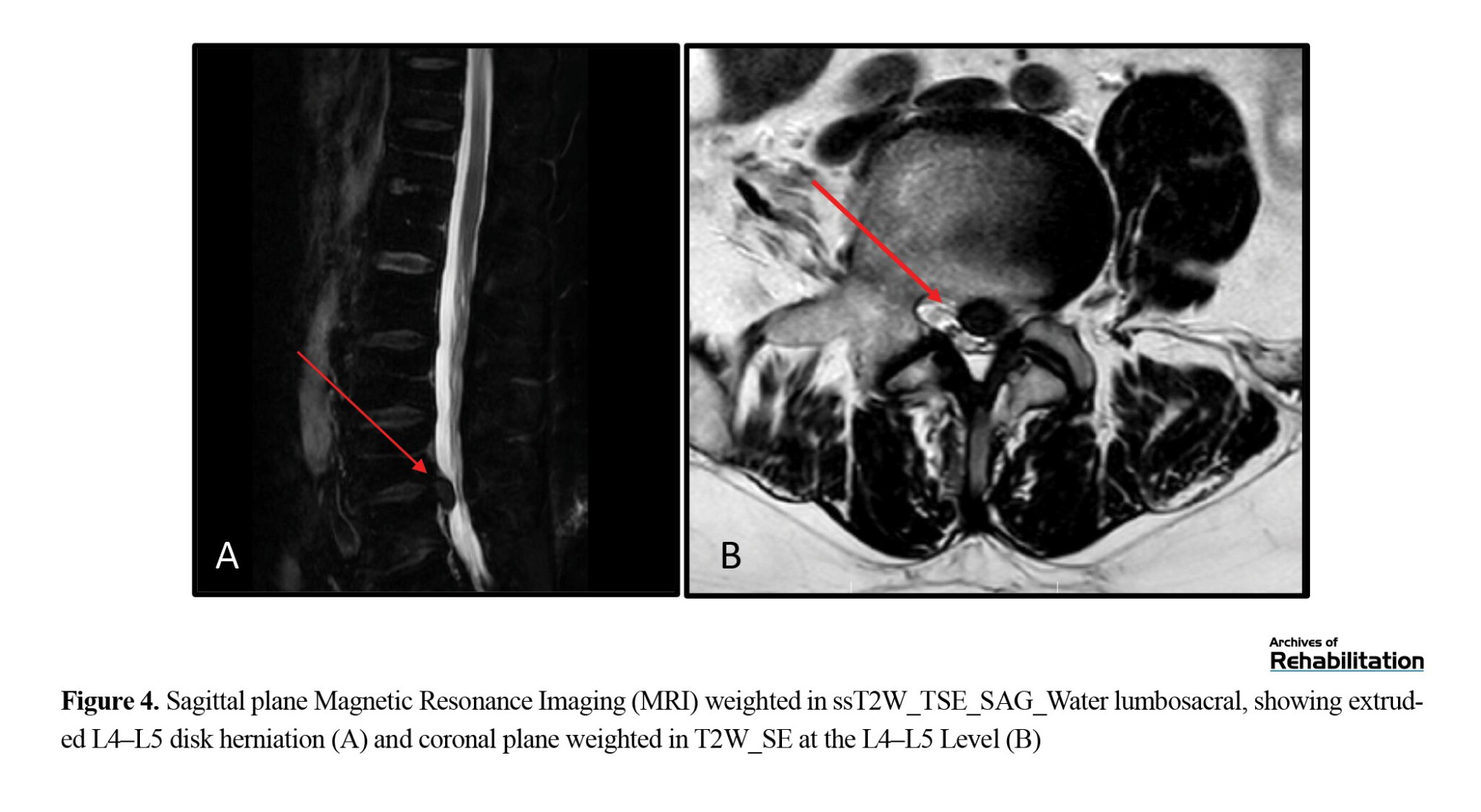
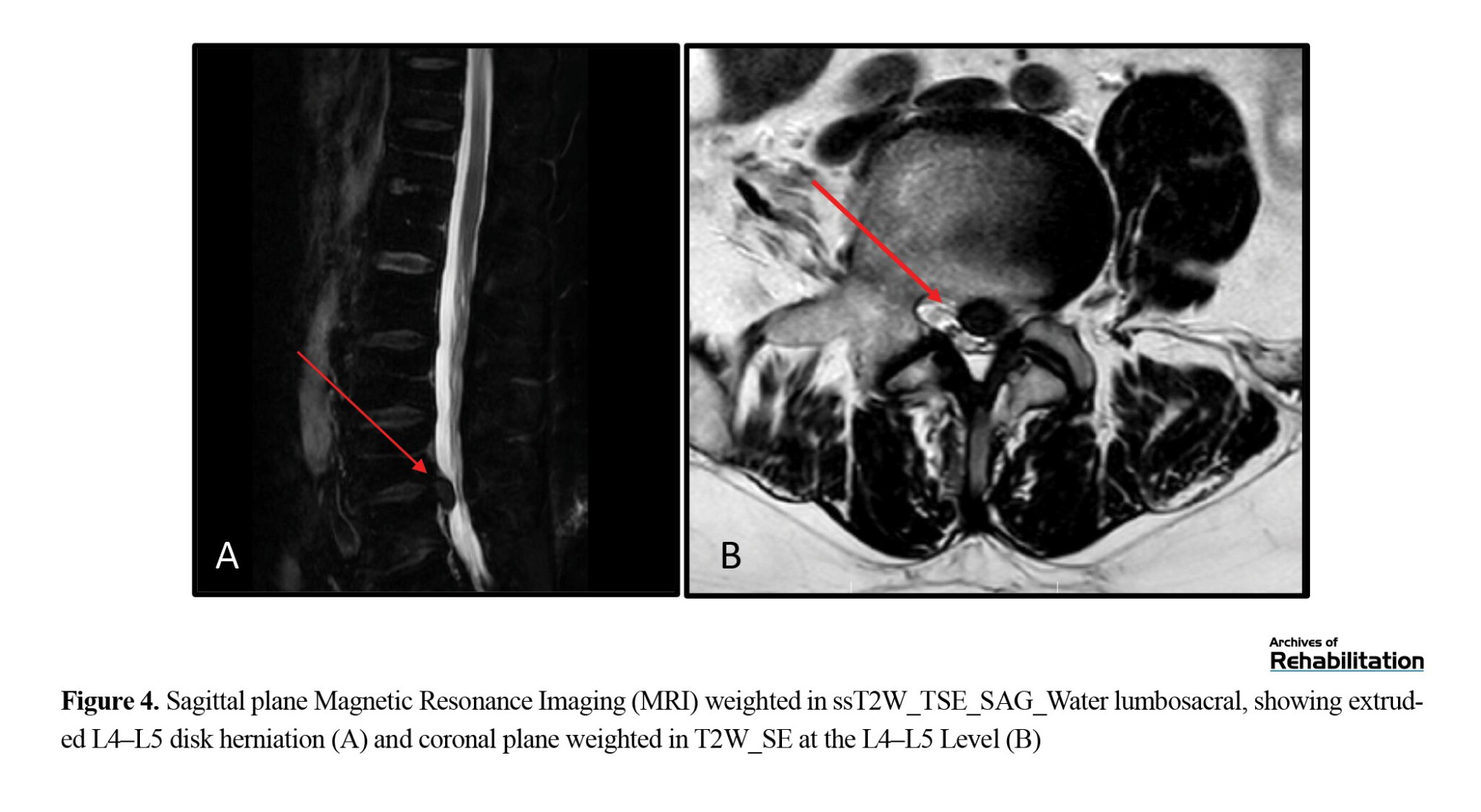
Despite sustained efforts in conservative therapy and rehabilitation, the persistence of pain and radicular involvement led to a new stage in case management. Considering the prolonged duration of symptoms, which lasted around 24 months, and the lack of a satisfactory response to conservative measures, surgical intervention was necessary in February 2021. Finally, surgery was performed through microdiskectomy and left L5–S1 foraminotomy, which successfully relieved the pain for approximately 12 months. One year later, the patient presented again with left L5 radiculopathy without sensory or motor deficits. The latest lumbar MRI identified a left-sided medio-paramedial and posterolateral disk herniation at the L4–L5 level. This herniation is higher than the previously treated disk herniation with discreet caudal migration in extensive contact with the left L5 root (Figure 4). Given the findings of left L5 radicular pain without distal neurological deficits on the most recent physical examination, the patient has been placed under the care of the Paint Unit for further evaluation and management.
Discussion
Hip osteoarthritis is a highly prevalent condition affecting adults [۱۰]. Although its geographical distribution varies, it is estimated that 25% of those affected experience symptoms, with a 10% chance of undergoing THA [۱۱]. Despite the overall success of the intervention, it can also lead to complications such as stem subsidence, infections, venous thromboembolic disease, nerve/vascular injuries, heterotopic ossification, leg length discrepancies, periprosthetic fractures, or muscle atrophy in the intervened limb, resulting in changes in lumbopelvic biomechanics [۱۲، ۱۳]. Rasch et al., in their 2007 study, described how 22 patients with hip osteoarthritis undergoing surgery exhibited changes in the muscles of the lower limbs, which were evident through magnetic resonance imaging and correlated with functional impairment and pain [۱۴]. Consistent with this finding, Mak et al. published a series of 341 THA cases in which PM atrophy ipsilateral to the surgery was observed [۷], in line with the 40 cases reported in 2011 by Ploumis and colleagues [۱۵]. The latter showed a higher degree of unilateral atrophy and fat infiltration on the implant than on the non-intervened side.
In the context of hip prosthetic surgery, psoas tenotomy during hip reduction, iatrogenic femoral nerve injury [۱۶], intramuscular hematomas, lower limb lengthening, and muscle irritation or tendinopathy secondary to friction with the acetabulum [۱۷] are events in which we can observe a direct relationship with progressive atrophy of the PM.
The origin of the PM in the vertebral bodies and intervertebral disks of the T12, L1, L2, L3, and L4 vertebrae has a natural stabilizing effect on the spine, ensuring the transmission of craniocaudal forces in the upper lumbar spine. Therefore, at the L4–L5 and L5–S1 lumbar levels, the stabilizing effect exerted by the PM is nonexistent. The lack of natural protection in the lower lumbar segments, combined with their increased mobility and load, may play a predisposing role in developing degenerative intervertebral disk pathology in the L4-L5 and L5-S1 vertebral regions. This finding, along with other reasons such as the gradual increase in load on the lower vertebrae, supports the evidence that 97% of disk herniations in healthy individuals manifest in the last two intervertebral levels, with 54% at the L5–S1 level and 43% at the L4–L5 level [۱۸]. Unilateral atrophy of the PM can induce chronic pelvic torsion. This compromises the integrity of the sacroiliac joints and the intervertebral joints of the lumbar spine and lumbosacral hinge, increasing lumbar lordosis and leading to degenerative changes in the lower vertebral segments [۱۹].
Rehabilitation in patients undergoing THA focuses on achieving the greatest range of joint mobility without pain and acquiring functional gait [۲۰]. However, in this context, there should be a systematic insistence on strengthening hip flexion and adduction, avoiding potential alterations in lumbopelvic biomechanics. In the case described in this article, standard rehabilitation treatment was performed immediately after THA, focusing on regaining hip joint mobility and achieving adequate functional recovery. Years later, when lumbosciatic, the unilateral atrophy of the PM and the degree of fat infiltration were detected, specific work was performed on the psoas, pelvic, and abdominal muscles to reduce pain derived from lumbar degenerative disease.
Analysis of the psoas muscle’s CSA indices concerning the L4–L5 intervertebral disk revealed values of 0.49 for the right and 0.99 for the left sides. These findings indicate a marked disparity between both sides, favoring the unaffected side in the clinical context [۷، ۲۱]. These indices, used by Kijima et al., were employed to associate atrophy with pain in patients with coxarthrosis, demonstrating a clear relationship between the degree of atrophy and the presence of pain [۲۲].
Our study identified severe unilateral atrophy on the right side as a possible contributing factor to disk degeneration and subsequent development of lumbosciatica. This process likely manifests over a medium- to long-term period, as the patient sought medical attention for LBP 8 years after hip surgery.
PM atrophy can substantially impact the stability of the lumbar spine, especially in the L4–L5–S1 vertebral segments, emphasizing the importance of assessing lumbar biomechanics over time in patients undergoing THA. This ongoing assessment is crucial for understanding and addressing the potential effects of muscle atrophy on these patients’ long-term health and stability of the lumbar region.
In this context, it is relevant to consider the information available in previous studies that have assessed the resolution of back pain after hip replacement surgery. Despite some reports of healing rates ranging from 53% to 82% [23-25], it is essential to note that these studies had a relatively short follow-up period, usually less than 1 or 2 years. This condition raises questions about the true progression of LBP in patients after THA, emphasizing the need for long-term research with a large, simple size, and high-quality method to understand the impact of this intervention on the health of the lumbar spine fully.
The development of a new upper-level disk herniation further emphasizes the clinical presentation. This event could be likened to the “adjacent segment disease” in cases of vertebral fusions [۲۶، ۲۷], and in our scenario, it is induced by the restricted mobility at L5-S1 resulting from the previously performed discectomy. In this case, following L5 discectomy surgery, a left posterolateral L4 disk herniation appeared, one segment above. This event further strengthens the potential correlation between lumbar biomechanical alteration and possible atrophy of the psoas muscle following THA.
Conclusion
The case presented makes us consider that total hip arthroplasty surgery may result in long-term unilateral atrophy of the ipsilateral psoas muscle. This fact could change the lumbar biomechanics, potentially accelerating the process of disc degeneration and subsequent low back pain.
Ultimately, this study highlights the need for close collaboration among orthopedic surgeons, physiotherapists, rehabilitation physicians, and neurosurgeons for a multidisciplinary and holistic approach to managing patients undergoing THA. The prevention and early identification of PM atrophy and its appropriate management could significantly improve these patients’ clinical course and quality of life, providing new perspectives for orthopedic medicine and rehabilitation.
However, the scope of this study is limited and raises new questions. Further research is needed to elucidate the relationship between PM atrophy, hip surgery, and lumbar disk degeneration. Future studies could shed light on unexplored areas and help develop more precise and personalized treatment strategies for affected patients.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the CEICA (Research Ethics Committee of the Autonomous Community of Aragon) under reference number C.P.-C.I.-PI21/346.
Funding
The authors declared no conflict of interest regarding the clinical case. Also, the research was self-funded.
Authors' contributions
The authors contributed equally to preparing this paper.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank the iHealthy Research Group for their support and collaboration in this project.
Lumbar pain is highly prevalent and is the leading cause of work disability in young people. It is estimated that two-thirds of adults experience low back pain (LBP) at some point in their lives, and 10% will develop chronic LBP [۱]. One of the most common causes of LBP is intervertebral disk degeneration. The etiology of intervertebral disk degeneration is multifactorial and is related, in most cases, to occupational activities and lifestyle, particularly factors such as obesity and smoking [۲]. The aging process contributes physiologically to intervertebral disk degeneration; it is estimated that by the age of 70, the water content of the nucleus pulposus decreases to 70% [۳]. Other causes that accelerate the degenerative process include infectious diseases, inflammatory processes, trauma, or biomechanical changes [۲، ۴]. In addition to the factors mentioned above, alterations in muscle function and biomechanical factors play crucial roles in developing and exacerbating LBP [۵]. Deficits in muscle strength and coordination may contribute to abnormal loading patterns on the spine, further exacerbating degenerative processes and increasing the risk of low back pain [۶].
Understanding the complex interplay between biomechanical factors and muscle function in LBP holds significant implications for addressing related conditions, such as the potential complications of total hip arthroplasty (THA). Recent studies indicate a correlation between THA and unilateral atrophy of the psoas muscle (PM) on the implant side, raising the possibility that this atrophy may be a late complication of surgery [۷]. The location of PM makes it a crucial stabilizer of the spine, influencing both static posture and lumbar spine dynamics [۸، ۹]. PM atrophy significantly impacts lumbar spine biomechanics and may contribute to the development of degenerative disk diseases.
In this context, we present the clinical case of a 53-year-old man who had previously undergone right THA. Eight years post-surgery, the patient experienced a chronic condition of lumbosciatalgia radiating to the left leg and weakness in the right hip flexion. Clinical and radiological analysis revealed the presence of an extruded L5–S1 disk herniation and unilateral atrophy of the PM on the same side of the arthroplasty. While the patient experienced some improvement with a conservative pharmacological and rehabilitative approach, complete recovery was not achieved, possibly due to the extended period of evolution of his condition. This prolonged evolution could have caused irreversible damage to the affected anatomical structures, limiting the patient’s ability to recover fully. This article will delve into the clinical case, explore the connection between PM atrophy and lumbar disk degeneration, and emphasize the importance of early detection and comprehensive management in patients with PM atrophy following THA.
Aside from illustrating a unique scenario, this clinical case has served as the starting point for an ongoing research endeavor, underscoring its value in the realm of medicine and routine clinical practice, especially in rehabilitation. This research was approved by the CEICA (Research Ethics Committee of the Autonomous Community of Aragon) under reference number C.P.-C.I.-PI21/346 and has been registered in the ClinicalTrials.gov database under the identifier NCT05647629.
Clinical Case
We present a 53-year-old male who presented to the Emergency Service of Hospital Clínico Lozano Blesa with an acute episode of left sciatica. He had been experiencing this pain for the past 12 hours before arriving at the Emergency Department, and it was rated 9/10 on the numerical rating scale. The patient denied any history of LBP or leg radiation prior to presentation. It w:::as char:::acterized by its mechanical nature and radiation to the left lower extremity, extending to the ankle and the first toe. The patient did not exhibit febrile symptoms or report recent traumas at admission. Radicular stretching and positive Lasegue and Bragard tests worsened the pain. Additional physical examination revealed pain in the quadratus lumborum and spinal erector muscles, with neuropathic radiation from the back of the leg to the foot. Motor weakness 2/5 in Kendall’s muscle grading system was observed in the extension of the left first toe (extensor digitorum longus) and in plantar flexion of the left ankle (triceps surae), as well as moderate weakness 2/5 in the flexion of the right hip, with the rest of the lumbosacral myotomes being normal. Sensory examination revealed hypoesthesia and hypoalgesia in the left S1 dermatome but no alterations in the other dermatomes. No sensory disturbances related to the cauda equina were observed, and no signs of sphincter dysfunction were detected.
Anamnesis and Radiological Evaluation
Upon reviewing the patient’s medical history, we found that he underwent right THA in April 2012 due to progressive unilateral coxarthrosis over the past two years. Four weeks after surgery, the patient completed six sessions of physiotherapy. In these sessions, the patient was instructed and evaluated on performing muscle strengthening exercises for the hip (gluteals, iliopsoas, adductors, quadriceps, and hamstrings), in addition to gait re-education. The patient reported mild weakness in right hip flexion and pain in the right inguinal region but no lumbar pain. These symptoms were considered common postoperative sequelae. THA, performed through a lateral approach with an SL-Plus+Epfit prosthesis, was indicated in response to hip osteoarthritis grade 3 according to the Kellgren–Lawrence classification (Figure 1).

The current evaluation recorded a body mass index of 29.58 kg/m2. Lumbar X-rays did not reveal substantial findings, but lumbar magnetic resonance imaging (MRI) revealed the presence of a left paramedian disk herniation at the L5–S1 level, accompanied by a voluminous sequestered disk fragment in an extraforaminal location (Figure 2).
Marked atrophy of the right PM was highlighted and accentuated by adipose tissue infiltration in the same region. The cross-sectional area (CSA) of the PM was quantified bilaterally by a radiologist at the L3–L4 intervertebral disk, obtaining a section of 681 mm² on the right side, with a Goutallier score of 3 indicates severe muscular atrophy. The left side showed a CSA of 1388 mm², with a Goutallier score of 0 (Figure 3A). The right and left psoas/disk CSA indices were calculated as 0.49 and 0.99, respectively. MRI revealed sections of the PM where the muscular belly was absent (Figure 3B). These findings demonstrated the pathology, excluding alternative neuromuscular and central nervous system diseases.
Evolution
Because of the intensity of pain and clinical manifestations, the patient was admitted to the Neurosurgery Department and treated with opioid-derived analgesia. In addition, caudal epidural injection with local anesthetic and corticosteroid was performed, resulting in a favorable response. The patient was discharged after two days of admission, and a rehabilitation program was initiated through 15 sessions of physiotherapy with exercises focused on strengthening the flexor muscles of the right hip, with special attention to PM, lumbopelvic stabilization exercises, stretches for the erector muscles of the back, transcutaneous electrical nerve stimulation electroanalgesia, and sciatic nerve neurodynamics. Gait retraining was also integral to the therapeutic plan, correcting antialgic anomalous patterns and improving movement dynamics. An electromyogram performed on an outpatient basis revealed a chronic pattern of radicular suffering with denervation of the left S1 root.
Despite sustained efforts in conservative therapy and rehabilitation, the persistence of pain and radicular involvement led to a new stage in case management. Considering the prolonged duration of symptoms, which lasted around 24 months, and the lack of a satisfactory response to conservative measures, surgical intervention was necessary in February 2021. Finally, surgery was performed through microdiskectomy and left L5–S1 foraminotomy, which successfully relieved the pain for approximately 12 months. One year later, the patient presented again with left L5 radiculopathy without sensory or motor deficits. The latest lumbar MRI identified a left-sided medio-paramedial and posterolateral disk herniation at the L4–L5 level. This herniation is higher than the previously treated disk herniation with discreet caudal migration in extensive contact with the left L5 root (Figure 4). Given the findings of left L5 radicular pain without distal neurological deficits on the most recent physical examination, the patient has been placed under the care of the Paint Unit for further evaluation and management.
Discussion
Hip osteoarthritis is a highly prevalent condition affecting adults [۱۰]. Although its geographical distribution varies, it is estimated that 25% of those affected experience symptoms, with a 10% chance of undergoing THA [۱۱]. Despite the overall success of the intervention, it can also lead to complications such as stem subsidence, infections, venous thromboembolic disease, nerve/vascular injuries, heterotopic ossification, leg length discrepancies, periprosthetic fractures, or muscle atrophy in the intervened limb, resulting in changes in lumbopelvic biomechanics [۱۲، ۱۳]. Rasch et al., in their 2007 study, described how 22 patients with hip osteoarthritis undergoing surgery exhibited changes in the muscles of the lower limbs, which were evident through magnetic resonance imaging and correlated with functional impairment and pain [۱۴]. Consistent with this finding, Mak et al. published a series of 341 THA cases in which PM atrophy ipsilateral to the surgery was observed [۷], in line with the 40 cases reported in 2011 by Ploumis and colleagues [۱۵]. The latter showed a higher degree of unilateral atrophy and fat infiltration on the implant than on the non-intervened side.
In the context of hip prosthetic surgery, psoas tenotomy during hip reduction, iatrogenic femoral nerve injury [۱۶], intramuscular hematomas, lower limb lengthening, and muscle irritation or tendinopathy secondary to friction with the acetabulum [۱۷] are events in which we can observe a direct relationship with progressive atrophy of the PM.
The origin of the PM in the vertebral bodies and intervertebral disks of the T12, L1, L2, L3, and L4 vertebrae has a natural stabilizing effect on the spine, ensuring the transmission of craniocaudal forces in the upper lumbar spine. Therefore, at the L4–L5 and L5–S1 lumbar levels, the stabilizing effect exerted by the PM is nonexistent. The lack of natural protection in the lower lumbar segments, combined with their increased mobility and load, may play a predisposing role in developing degenerative intervertebral disk pathology in the L4-L5 and L5-S1 vertebral regions. This finding, along with other reasons such as the gradual increase in load on the lower vertebrae, supports the evidence that 97% of disk herniations in healthy individuals manifest in the last two intervertebral levels, with 54% at the L5–S1 level and 43% at the L4–L5 level [۱۸]. Unilateral atrophy of the PM can induce chronic pelvic torsion. This compromises the integrity of the sacroiliac joints and the intervertebral joints of the lumbar spine and lumbosacral hinge, increasing lumbar lordosis and leading to degenerative changes in the lower vertebral segments [۱۹].
Rehabilitation in patients undergoing THA focuses on achieving the greatest range of joint mobility without pain and acquiring functional gait [۲۰]. However, in this context, there should be a systematic insistence on strengthening hip flexion and adduction, avoiding potential alterations in lumbopelvic biomechanics. In the case described in this article, standard rehabilitation treatment was performed immediately after THA, focusing on regaining hip joint mobility and achieving adequate functional recovery. Years later, when lumbosciatic, the unilateral atrophy of the PM and the degree of fat infiltration were detected, specific work was performed on the psoas, pelvic, and abdominal muscles to reduce pain derived from lumbar degenerative disease.
Analysis of the psoas muscle’s CSA indices concerning the L4–L5 intervertebral disk revealed values of 0.49 for the right and 0.99 for the left sides. These findings indicate a marked disparity between both sides, favoring the unaffected side in the clinical context [۷، ۲۱]. These indices, used by Kijima et al., were employed to associate atrophy with pain in patients with coxarthrosis, demonstrating a clear relationship between the degree of atrophy and the presence of pain [۲۲].
Our study identified severe unilateral atrophy on the right side as a possible contributing factor to disk degeneration and subsequent development of lumbosciatica. This process likely manifests over a medium- to long-term period, as the patient sought medical attention for LBP 8 years after hip surgery.
PM atrophy can substantially impact the stability of the lumbar spine, especially in the L4–L5–S1 vertebral segments, emphasizing the importance of assessing lumbar biomechanics over time in patients undergoing THA. This ongoing assessment is crucial for understanding and addressing the potential effects of muscle atrophy on these patients’ long-term health and stability of the lumbar region.
In this context, it is relevant to consider the information available in previous studies that have assessed the resolution of back pain after hip replacement surgery. Despite some reports of healing rates ranging from 53% to 82% [23-25], it is essential to note that these studies had a relatively short follow-up period, usually less than 1 or 2 years. This condition raises questions about the true progression of LBP in patients after THA, emphasizing the need for long-term research with a large, simple size, and high-quality method to understand the impact of this intervention on the health of the lumbar spine fully.
The development of a new upper-level disk herniation further emphasizes the clinical presentation. This event could be likened to the “adjacent segment disease” in cases of vertebral fusions [۲۶، ۲۷], and in our scenario, it is induced by the restricted mobility at L5-S1 resulting from the previously performed discectomy. In this case, following L5 discectomy surgery, a left posterolateral L4 disk herniation appeared, one segment above. This event further strengthens the potential correlation between lumbar biomechanical alteration and possible atrophy of the psoas muscle following THA.
Conclusion
The case presented makes us consider that total hip arthroplasty surgery may result in long-term unilateral atrophy of the ipsilateral psoas muscle. This fact could change the lumbar biomechanics, potentially accelerating the process of disc degeneration and subsequent low back pain.
Ultimately, this study highlights the need for close collaboration among orthopedic surgeons, physiotherapists, rehabilitation physicians, and neurosurgeons for a multidisciplinary and holistic approach to managing patients undergoing THA. The prevention and early identification of PM atrophy and its appropriate management could significantly improve these patients’ clinical course and quality of life, providing new perspectives for orthopedic medicine and rehabilitation.
However, the scope of this study is limited and raises new questions. Further research is needed to elucidate the relationship between PM atrophy, hip surgery, and lumbar disk degeneration. Future studies could shed light on unexplored areas and help develop more precise and personalized treatment strategies for affected patients.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the CEICA (Research Ethics Committee of the Autonomous Community of Aragon) under reference number C.P.-C.I.-PI21/346.
Funding
The authors declared no conflict of interest regarding the clinical case. Also, the research was self-funded.
Authors' contributions
The authors contributed equally to preparing this paper.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank the iHealthy Research Group for their support and collaboration in this project.
References
- Domenech J, Baños R, Peñalver L, Garcia-Palacios A, Herrero R, Ezzedine A, et al. Design considerations of a randomized clinical trial on a cognitive behavioural intervention using communication and information technologies for managing chronic low back pain. BMC Musculoskeletal Disorders. 2013; 14:142. [DOI:10.1186/1471-2474-14-142] [PMID]
- Oichi T, Taniguchi Y, Oshima Y, Tanaka S, Saito T. Pathomechanism of intervertebral disc degeneration. JOR Spine. 2020; 3(1):e1076. [DOI:10.1002/jsp2.1076] [PMID]
- Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976). 1995; 20(11):1307-14. [DOI:10.1097/00007632-199506000-00022] [PMID]
- Kos N, Gradisnik L, Velnar T. A brief review of the degenerative intervertebral disc disease. Medical Archives. 2019; 73(6):421-4. [DOI:10.5455/medarh.2019.73.421-424] [PMID]
- Noonan AM, Brown SHM. Paraspinal muscle pathophysiology associated with low back pain and spine degenerative disorders. JOR Spine. 2021; 4(3):e1171. [DOI:10.1002/jsp2.1171] [PMID]
- Alston W, Carlson KE, Feldman DJ, Grimm Z, Gerontinos E. A quantitative study of muscle factors in the chronic low back syndrome. Journal of the American Geriatrics Society. 1966; 14(10):1041-7. [DOI:10.1111/j.1532-5415.1966.tb02885.x] [PMID]
- Mak D, Chisholm C, Davies AM, Botchu R, James SL. Psoas muscle atrophy following unilateral hip arthroplasty. Skeletal Radiology. 2020; 49(10):1539-45. [DOI:10.1007/s00256-020-03447-3] [PMID]
- Syed HR, Yaeger K, Sandhu FA. Resolution of the more anteriorly positioned psoas muscle following correction of spinal sagittal alignment from spondylolisthesis: Case report. Journal of Neurosurgery Spine. 2017; 26(4):441-7. [DOI:10.3171/2016.9.SPINE16324] [PMID]
- Elliott JM, Zylstra ED, Centeno CJ. The presence and utilization of psoas musculature despite congenital absence of the right hip. Manual Therapy. 2004; 9(2):109-13. [DOI:10.1016/S1356-689X(03)00128-0] [PMID]
- Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: A review. Journal of the American Medical Association. 2021; 325(6):568-78. [DOI:10.1001/jama.2020.22171] [PMID]
- Murphy NJ, Eyles JP, Hunter DJ. Hip osteoarthritis: Etiopathogenesis and implications for management. Advances in Therapy. 2016; 33(11):1921-46. [DOI:10.1007/s12325-016-0409-3] [PMID]
- Nutt JL, Papanikolaou K, Kellett CF. (ii) Complications of total hip arthroplasty. Orthopaedics and Trauma. 2013; 27(5):272-6. [DOI:10.1016/j.mporth.2013.08.012]
- Nolan DR, Fitzgerald RH Jr, Beckenbaugh RD, Coventry MB. Complications of total hip arthroplasty treated by reoperation. The Journal of Bone and Joint Surgery. 1975; 57(7):977-81. [DOI:10.2106/00004623-197557070-00017]
- Rasch A, Byström AH, Dalen N, Berg HE. Reduced muscle radiological density, cross-sectional area, and strength of major hip and knee muscles in 22 patients with hip osteoarthritis. Acta Orthopaedica. 2007; 78(4):505-10. [DOI:10.1080/17453670710014158] [PMID]
- Ploumis A, Michailidis N, Christodoulou P, Kalaitzoglou I, Gouvas G, Beris A. Ipsilateral atrophy of paraspinal and psoas muscle in unilateral back pain patients with monosegmental degenerative disc disease. The British Journal of Radiology. 2011; 84(1004):709-13. [DOI:10.1259/bjr/58136533] [PMID]
- Slater N, Singh R, Senasinghe N, Gore R, Goroszeniuk T, James D. Pressure monitoring of the femoral nerve during total hip replacement: An explanation for iatropathic palsy. Journal of the Royal College of Surgeons of Edinburgh. 2000; 45(4):231-3. [PMID]
- Morohashi I, Homma Y, Kanda A, Yamamoto Y, Obata H, Mogami A, et al. Iliopsoas impingement after revision total hip arthroplasty treated with iliopsoas muscle transection. Annals of Medicine and Surgery. 2016; 7:30-3. [DOI:10.1016/j.amsu.2016.03.004] [PMID]
- Martínez A. [Valoración de la efectividad de Escuela de Espalda en pacientes afectos de lumbalgia subaguda o crónica (Spanish)] [PhD dissertation] . Zaragoza: Universidad de Zaragoza; 2018. [Link]
- Regev GJ, Kim CW, Tomiya A, Lee YP, Ghofrani H, Garfin SR, et al. Psoas muscle architectural design, in vivo sarcomere length range, and passive tensile properties support its role as a lumbar spine stabilizer. Spine (Phila Pa 1976). 2011; 36(26):E1666-74. [DOI:10.1097/BRS.0b013e31821847b3] [PMID]
- Garden FH. Rehabilitation Following total hip arthroplasty. Journal of Back and Musculoskeletal Rehabilitation. 1994; 4(3):185-92. [DOI:10.3233/BMR-1994-4308] [PMID]
- Pezolato A, de Vasconcelos EE, Defino HL, Nogueira-Barbosa MH. Fat infiltration in the lumbar multifidus and erector spinae muscles in subjects with sway-back posture. European Spine Journal. 2012; 21(11):2158-64. [DOI:10.1007/s00586-012-2286-z] [PMID]
- Kijima H, Yamada S, Konishi N, Kubota H, Tazawa H, Tani T, et al. The differences in imaging findings between painless and painful osteoarthritis of the hip. Clinical Medicine Insights Arthritis Musculoskeletal Disorders. 2020; 13:117954412094674. [DOI:10.1177/1179544120946747] [PMID]
- Parvizi J, Pour AE, Hillibrand A, Goldberg G, Sharkey PF, Rothman RH. Back pain and total hip arthroplasty: A prospective natural history study. Clinical Orthopaedics and Related Research. 2010; 468(5):1325-30. [DOI:10.1007/s11999-010-1236-5] [PMID]
- Vigdorchik JM, Shafi KA, Kolin DA, Buckland AJ, Carroll KM, Jerabek SA. Does low back pain improve following total hip arthroplasty? The Journal of Arthroplasty. 2022; 37(8):S937-40. [DOI:10.1016/j.arth.2022.03.038] [PMID]
- Staibano P, Winemaker M, Petruccelli D, de Beer J. Total joint arthroplasty and preoperative low back pain. The Journal of Arthroplasty. 2014; 29(5):867-71. [DOI:10.1016/j.arth.2013.10.001] [PMID]
- McDonald CL, Alsoof D, Glueck J, Osorio C, Stone B, McCluskey L, et al. Adjacent segment disease after spinal fusion. JBJS Reviews. 2023; 11(6):e23.00028. [DOI:10.2106/JBJS.RVW.23.00028]
- Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine (Phila Pa 1976). 2004; 29(17):1938-44. [DOI:10.1097/01.brs.0000137069.88904.03] [PMID]
Type of Study: Case report |
Subject:
Rehabilitation Management
Received: 10/03/2024 | Accepted: 3/07/2024 | Published: 1/01/2025
Received: 10/03/2024 | Accepted: 3/07/2024 | Published: 1/01/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |