Volume 25, Issue 4 (Winter 2025)
jrehab 2025, 25(4): 746-765 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghorbanpour Z, Hosseini S A, Osqueizadeh R, Jamali S, Pishyareh E, Fallah S. Development and Validation of a Single-Item Scale to Screen Fear of Falling in Patients Experiencing Chronic Stroke. jrehab 2025; 25 (4) :746-765
URL: http://rehabilitationj.uswr.ac.ir/article-1-3404-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3404-en.html
Zahra Ghorbanpour1 

 , Seyed Ali Hosseini2
, Seyed Ali Hosseini2 

 , Reza Osqueizadeh3
, Reza Osqueizadeh3 

 , Shamsi Jamali4
, Shamsi Jamali4 

 , Ebrahim Pishyareh *5
, Ebrahim Pishyareh *5 

 , Soheila Fallah6
, Soheila Fallah6 




 , Seyed Ali Hosseini2
, Seyed Ali Hosseini2 

 , Reza Osqueizadeh3
, Reza Osqueizadeh3 

 , Shamsi Jamali4
, Shamsi Jamali4 

 , Ebrahim Pishyareh *5
, Ebrahim Pishyareh *5 

 , Soheila Fallah6
, Soheila Fallah6 


1- Department of Occupational Therapy, Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Occupational Therapy, Neuromusculoskeletal Rehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Ergonomics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Occupational Therapy, Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,eb.pishyareh@uswr.ac.ir
6- Department of Neurosciences, Faculty of Advanced Technologies in Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Occupational Therapy, Neuromusculoskeletal Rehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Ergonomics, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Occupational Therapy, Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
6- Department of Neurosciences, Faculty of Advanced Technologies in Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 2642 kb]
(753 Downloads)
| Abstract (HTML) (5444 Views)
Full-Text: (792 Views)
Introduction
Fear of falling (FOF) is a psychological condition associated with excessive concern about losing balance [1]. This fear could lead to uncertainty, decreased physical activity, communication and balance, low self-esteem, confined social interactions, and impaired quality of life [2-4]. People who have had a stroke are more likely than other people to be subjected to FOF [5, 6]. This condition can be due to the physical and cognitive changes after a stroke [7]. In addition, stroke patients often experience falling due to their balance problems [2]. Studies have revealed a relationship between FOF and earlier falls and balance problems in stroke patients [8, 9]. Therefore, the fear of falling as one of the common factors affecting the balance and quality of life of stroke patients needs to be screened and managed early.
Also, FOF is a long-standing complication in stroke patients, so nearly 60% of the patients who have experienced a stroke report some level of FOF after being discharged [10]. Furthermore, about 50% of the patients mentioned above still report the fear of falling 6 months after the incident, though they are expected to develop adaptations to the new condition [11, 12]. Therefore, they impose an extra cost for the associated healthcare arrangements [10]. With early and fast screening of the FOF, its complications can be prevented, and the effect of treatment protocols can be checked step by step.
Some well-accepted, valid, and reliable instruments have been developed in this field, such as ABC (activities-specific balance confidence), falls efficacy scale (FES), and falls efficacy scale-international (FES-I) [13-15]. The ABC items are focused on balance confidence in mobility (not fear while performing mobility) [14, 16]. while FES and FES-I are more appropriate for evaluating the fear concept [16]. However, it should be noted that symptoms of fear of falling in social and heavy bodily activities cannot be assessed via FES [17]. Therefore, FES-I could be considered a proper alternative tool to evaluate concerns of falling in various levels of social activities [18], being widely employed as a valid and reliable indicator to assess indoor and outdoor activities [13, 19, 20]. Psychometric evaluation of this tool for stroke patients has also been completed in the Persian language, with high levels of validity and reliability [13].
Nevertheless, considering the cognitive and temporal deficits experienced after stroke (up to 22% at 5 months to 14 years after stroke) [21], the frequency and severity of fatigue in these patients [22], complicated questionnaires (eg, FES-I ) may lead to confusion and lack of motivation to participate in surveys [23]. So, applying a fast and accurate evaluation tool for fear of falling is essential.
Addressing this issue, several single-item scales have recently been developed for rapid rating and comfortable screening of FOF, but not in stroke patients. As a good example, the FOF screening scale has been psychometrically evaluated in older adults residing in nursing homes [24] and another in young-old community-dwelling [25]. However, both scales have been developed in healthy older people. Nonetheless, it should be considered that aging and stroke are two entirely different phenomena. Different nature of balance problems in stroke patients due to asymmetry in the limbs caused by unilateral neglect, and deficits in sensation, cognition, emotion and motor planning, would be evidence enough. So, it would be helpful to develop, evaluate, and validate single-item scales for rapid screening of FOF in stroke patients.
To our knowledge, there is no accurate single-item tool to assess FOF in stroke patients; therefore, the current study was carried out to design and validate a single-item scale to accurately and fast screen of FOF in stroke patients.
On the other hand, taking into account the prevalence and the effect of psychological factors, especially anxiety [26] and depression [27], on the FOF in stroke patients, and according to conclusions in neuroscience and motor control, psychological factors like depression and anxiety act as direct confounding factors in disturbing postural control strategy into internal attentional focus in motor control. Also, according to the suggestions of Meimandi and Schmid studies, for a more accurate evaluation of the FOF, in this study, these factors (anxiety and depression) were also evaluated, and their effects were controlled.
Participants and Methods
Study Design and Participants
The study followed a cross-sectional design in which 180 first-stroke patients (mean age: 55.90±12.86 years) participated. They were recruited from rehabilitation hospitals and clinics, including Rafideh Hospital, Loqman Hospital, Tajrish SHohada Hospital, Nizam Mafi Clinic, Hasti Clinic, and Iran Rehabilitation Faculty Clinic through convenience sampling, which was carried out within 3 months between December 2021 and March 2022. The main inclusion criteria were as follows: 6- to 48-month duration from the stroke, ability to stand independently (for a minimum of 90 s), ability to walk for a minimum of 10 m without assistive devices, and obtaining scores ≥44 in star cancellation test for measuring unilateral neglect [28], and ≥23 in mini-mental status examination test [29]. If the patient did not want to continue the evaluations, she/he would be excluded from the study.
An experienced occupational therapist implemented the FES-I (the questionnaire for creating low fear of falling and high fear of falling groups), hospital anxiety and depression scale (HADS) (grouping to control anxiety and depression), and FOF-rating scale (RS) (newly developed questionnaire) tests and completed the demographic questionnaire.
Sampling was done so that all the potential candidates who met the inclusion criteria and visited the hospitals and rehabilitation clinics were included in the 3-month study.
To include the variables of anxiety and depression from the beginning, two groups with a high FOF and without a high FOF were considered. Then, the participants were allocated to these groups based on their level of anxiety and depression. Participants with and without anxiety and depression were also assigned to two groups with and without a high fear of falling level. Before proceeding to statistical analyses, we ensured that the two groups with high FOF and without high FOF levels did not have any significant statistical difference in terms of anxiety and depression.
Experiments were carried out in “Javad Movaffaghiyan Research Center laboratory,” and took 20-30 minutes on average (rest was given without restriction whenever needed). Finally, raw data were processed and analyzed using IBM SPSS statistics (Version 10), and the comparisons between two groups with and without high FOF for FESI and FOF-RS were carried out accordingly.
The study received approval from the university (IR.USWR.REC.1397.179), and all participants completed and signed the informed consent forms. All ethical considerations of working with human samples were observed.
Study Assessments
Falls Efficacy Scale – International (FES-I)
The 16-item FES-I is developed upon the original form comprising 10 items from the FES questionnaire and 6 additional social activities items to assess troubles with falling in outdoor and indoor activities. Each item is scored with a 4-point Likert scale (1=not concerned at all, 4=very concerned), thus a total score of 64 representing extreme concern for falling. The psychometric properties of the Persian version have been examined in stroke patients (α=0.78) [13]. Based on the previous literature, a score of 23 was set as the cut-off point for the distribution of participants to low (<23) and high FOF (≥23) groups [18, 24, 30].
Hospital Anxiety and Depression Scale (HADS)
The HADS questionnaire comprises two sections, within which HADS-A has seven questions for anxiety, and HADS-D has 7 questions for depression. The questionnaire is a reliable tool for evaluating and screening anxiety (r=0.74) and depression (r=0.70) in stroke patients [31]. Also, the Persian version of the HADS is a reliable and valid measure for anxiety and depression [32].
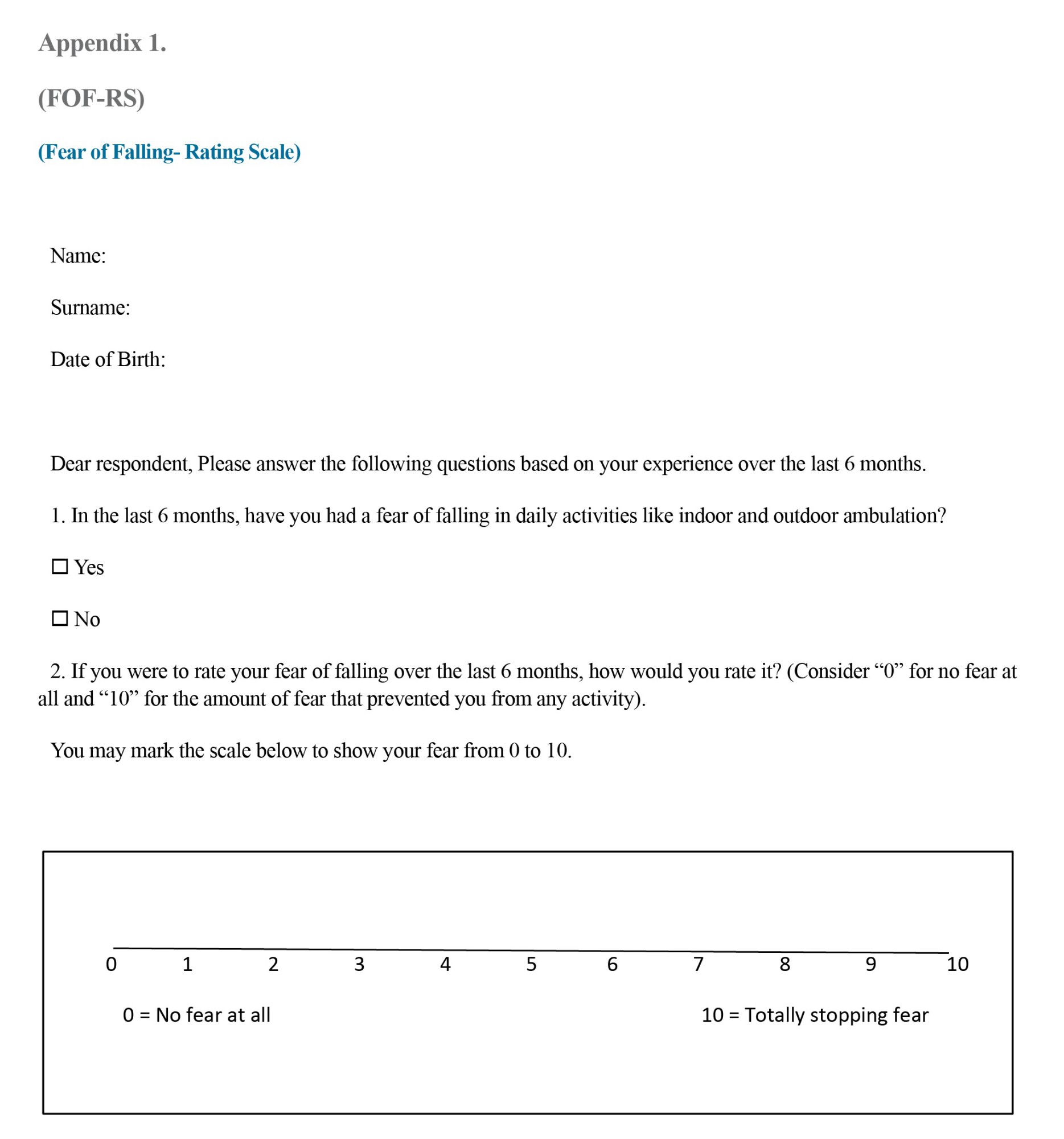
Fear of Falling-Rating Scale (FOF-RS): (Appendix 1) FoF-RS has been designed to quickly screen an individual’s fear of falling through a valid single-item scale and facilitate respondent contribution. FOF over the last 6 months was quantified via a Preparation question. An opening question would remind the respondent of their FOF in the last 6 months, followed by the next question regarding fear of falling in that period on a 0-10 scale (0 representing no fear of falling at all, and 10 representing a fear that keeps the individual from performing any tasks. Also, for greater clarity, there is a visual analog scale under the question so that the patient can better rate her/his fear of falling.
Statistical Analysis
The normality of data was tested via the Shapiro-Wilk test. Taking into account the distorting effect of anxiety and depression, at first, the mean difference of these factors was compared in two groups of low FOF and high FOF with an independent sample t test. Next, MedCalc was utilized to analyze the ROC curve. Finally, FOF-RS validity in stroke patients was determined based on negative predictive value (NPV), positive predictive value (PPV), area under curve (AUC), and specificity and sensitivity.
Results
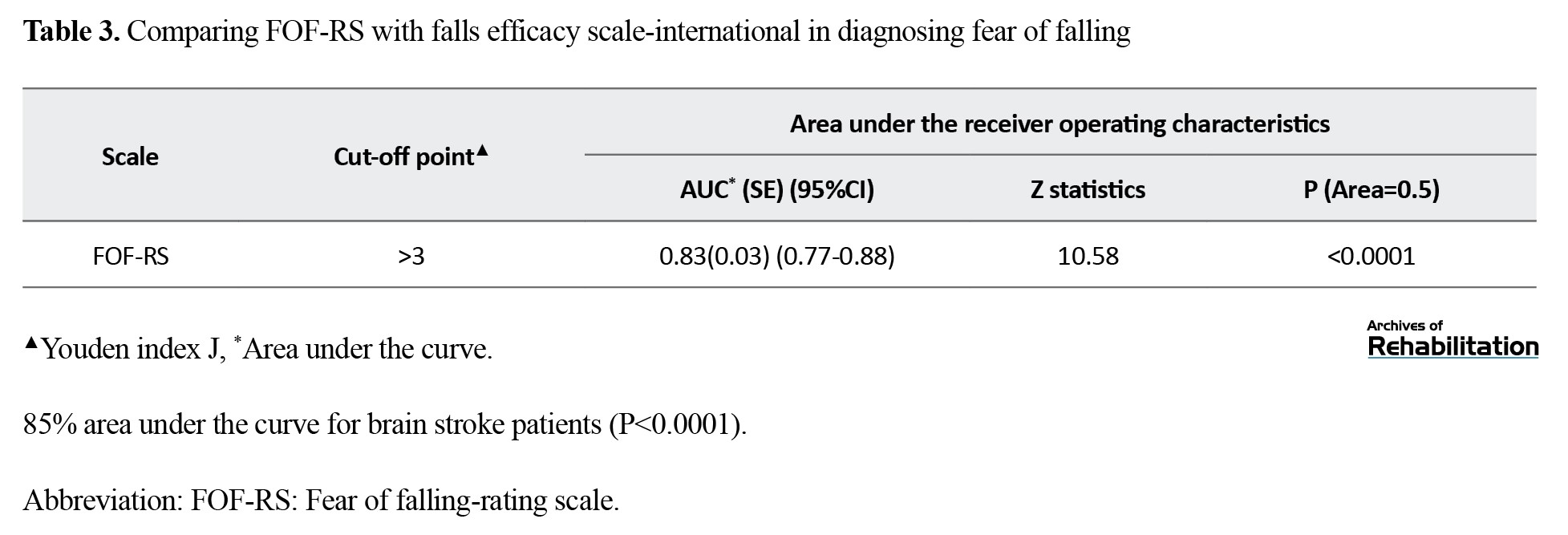
Demographic information is summarized in Table 1.
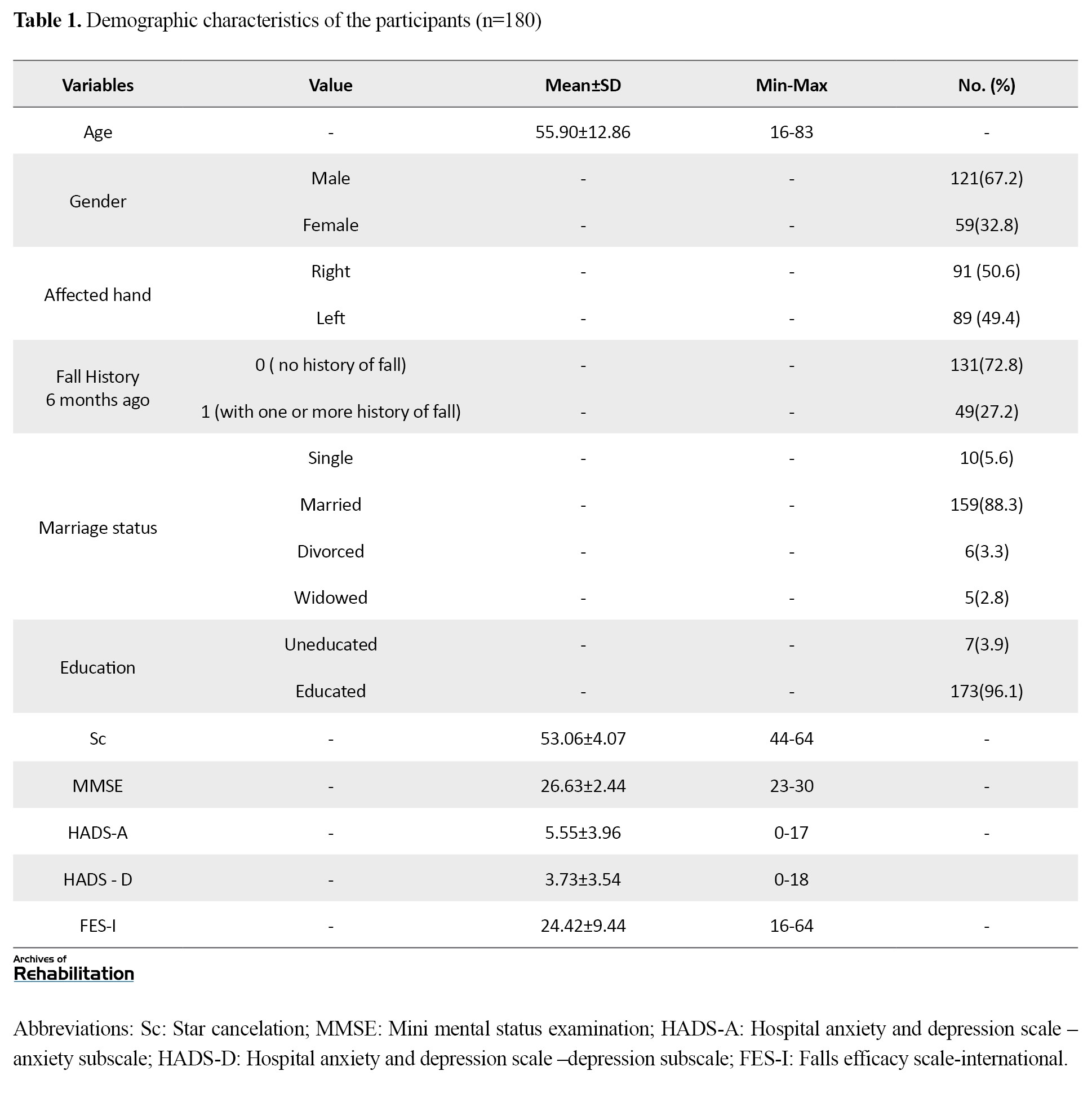
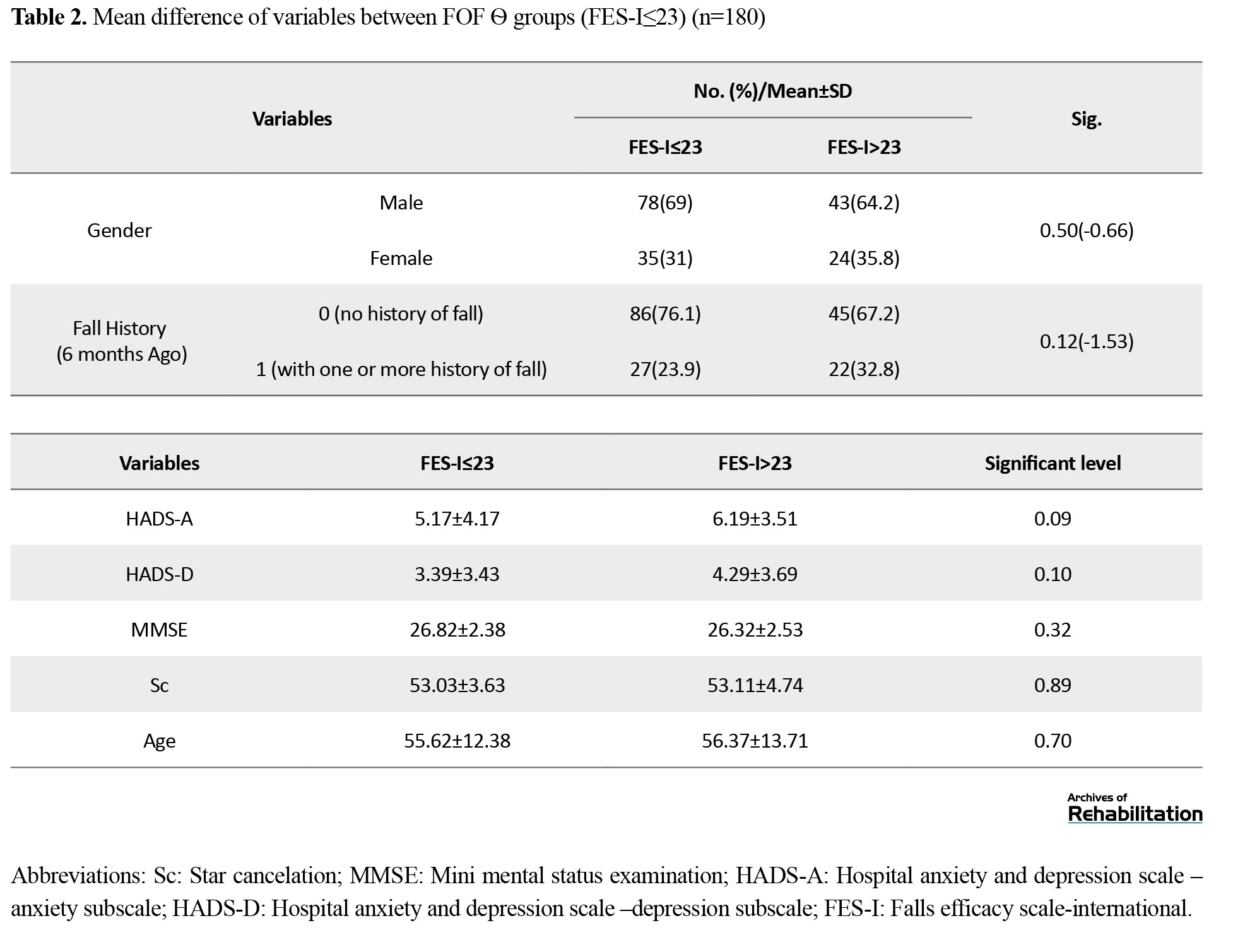
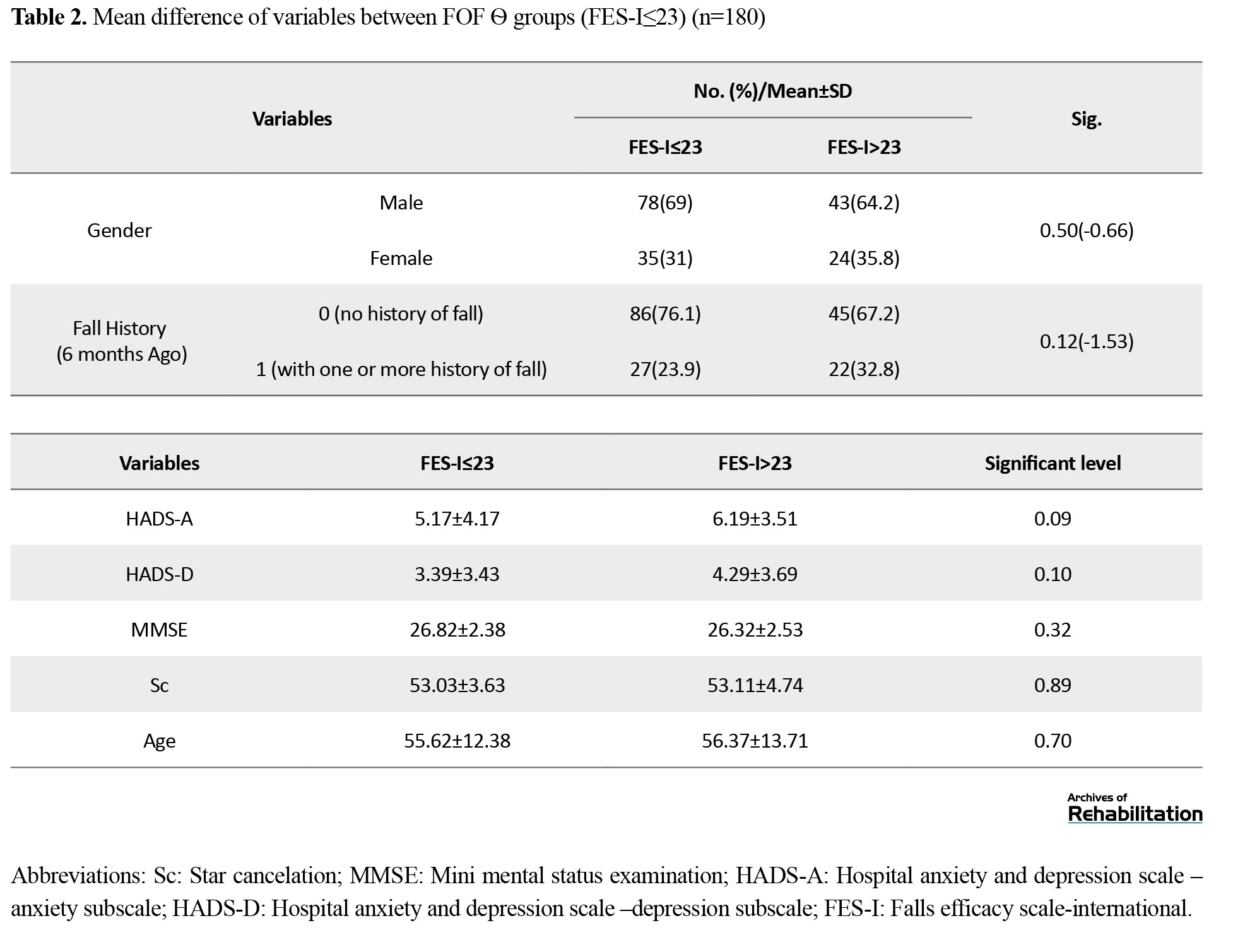
According to the FES-I questionnaire cut-off point [23], participant data were classified into two groups, including stroke patients with low FOF (scores≤23) and those with high FOF (scores>23). No statistically significant difference was observed in age, gender, cognition, anxiety, depression, and fall history between these two groups (Table 2).
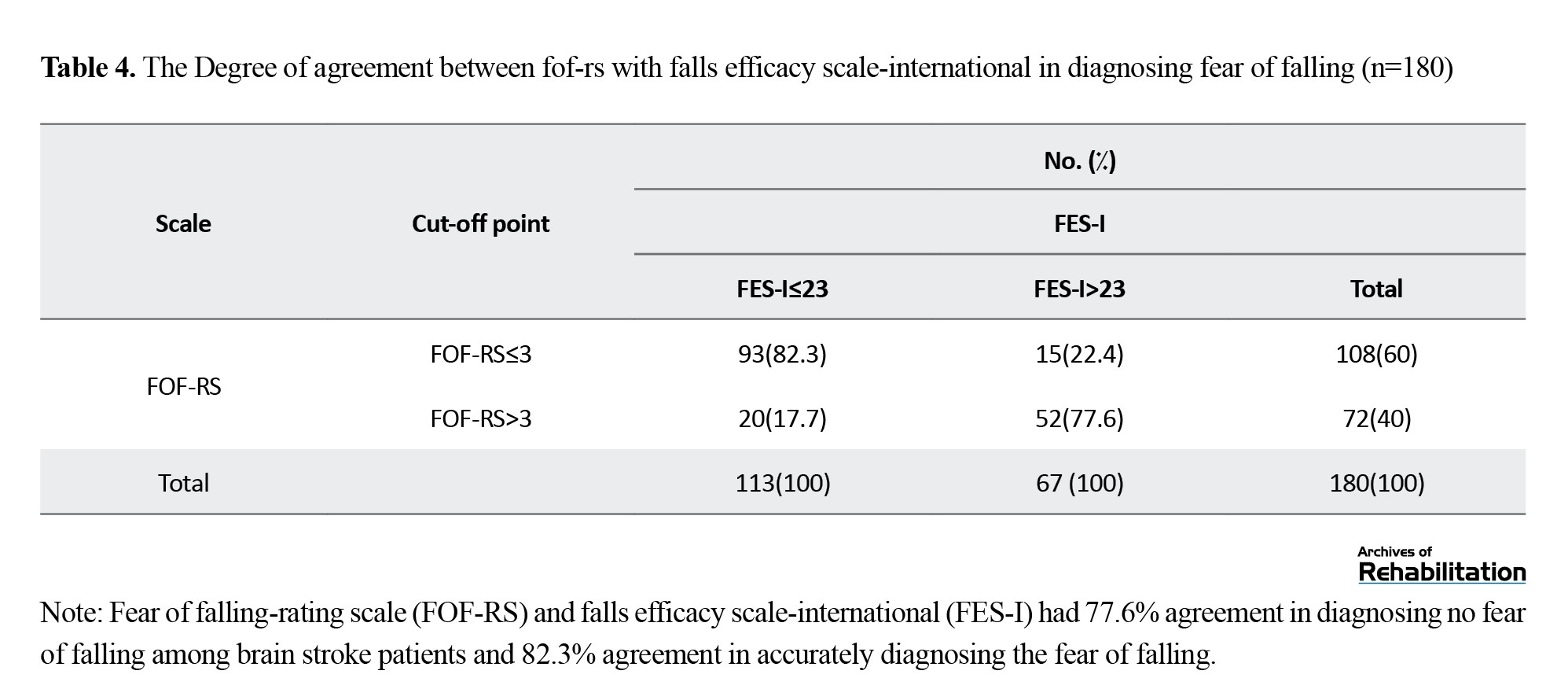
Finding Cut-off Point for FOF-RS Via ROC Curve Analysis
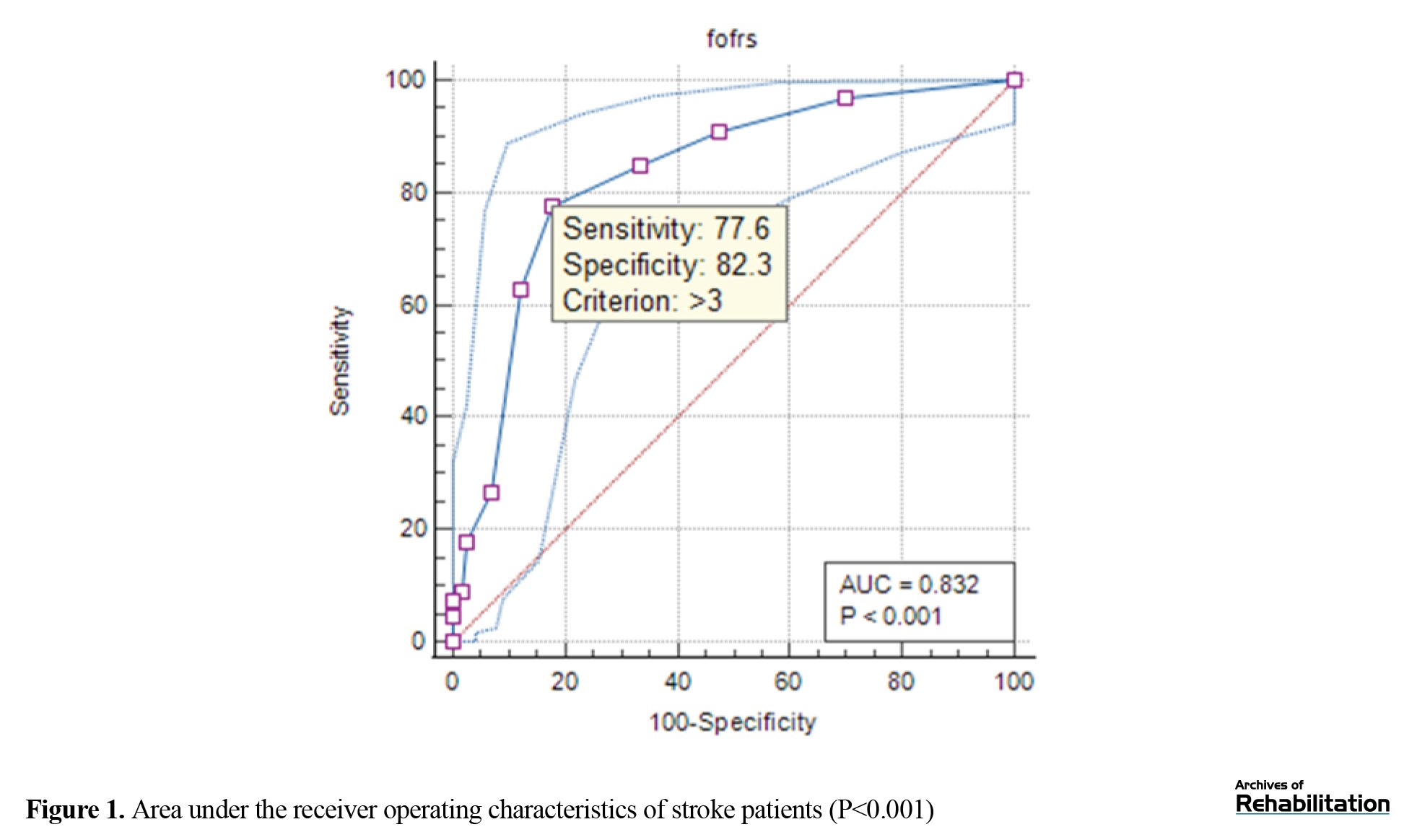
Based on FES-I, receiver operating characteristics (ROC) curve analysis revealed a 0.83% area under the curve for stroke patients (Table 3, Figure 1).
This result proves the capability of this scale for screening FOF in stroke patients. Also, the cut-off point 3 was determined for stroke patients.
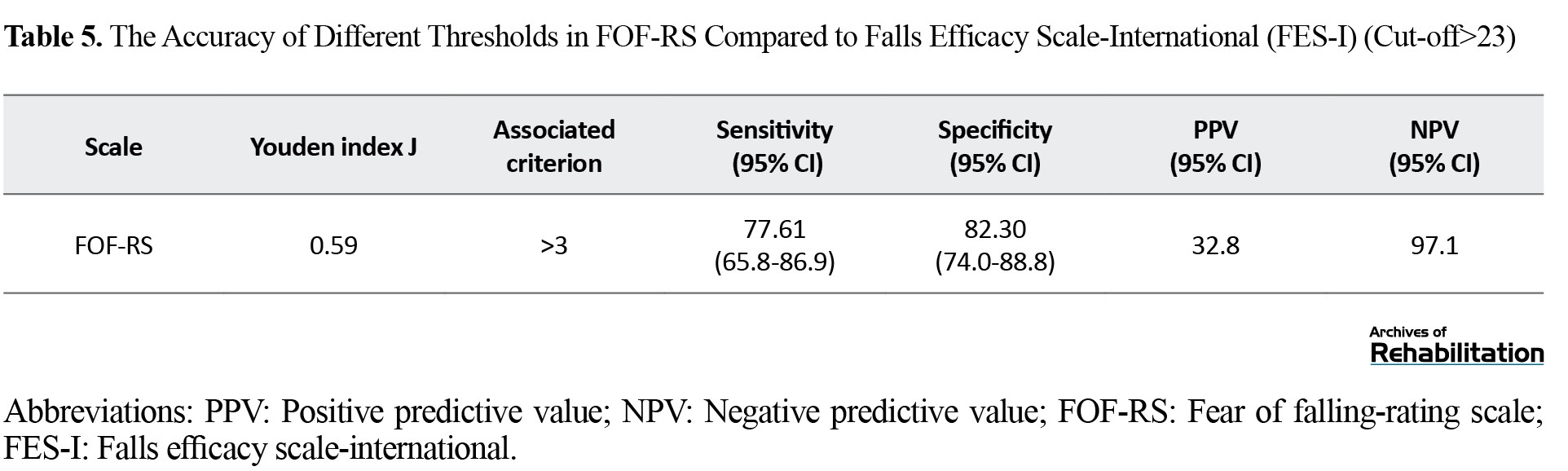
Agreement Between FOF-RS and FES-I in Assessing FOF
Regarding the FOF-RS and FES-I agreement, results revealed that in those with a low FOF, the agreement was 82.3%; in those with high FOF, this agreement was 77.6% (Table 4).
This agreement among stroke patients had acceptable compatibility levels.
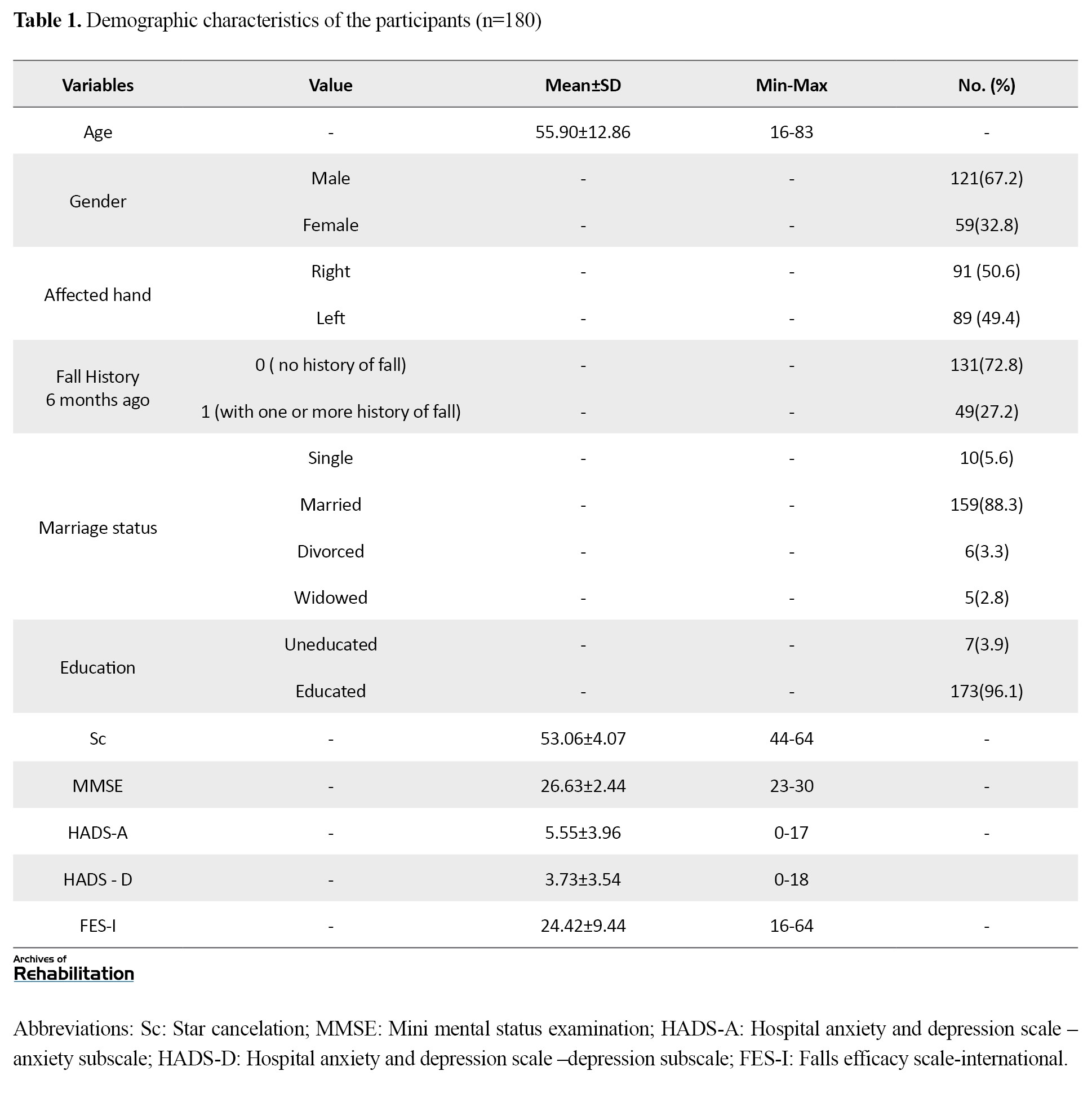
Sensitivity, specificity, PPV, NPV, and AUC for Screening FOF
The sensitivity for screening for fear of falling was 77.61%. Also, specificity in this regard was 82.3% (Table 5).
Youden index J was calculated using MedCalc (>3).
Discussion
According to the plotted ROC curve, FOF-RS showed good diagnostic accuracy for screening fear of falling in stroke patients. The cut-off point “3” for screening fear of falling in stroke patients (with controlling anxiety and depression) indicated excellent sensitivity and specificity.
This single-item scale has a unique capability of assessing and screening fear of falling in stroke patients. Belloni and Meimandi have developed single-item scales for fear of falling in older people. The current study’s results align with Belloni and Meimandi’s findings [25, 33] in older adults. However, the AUC and concordance of this scale with FES-I are higher than the single-item scale in Meimandi’s study.
It seems that the appearance and number of items in the scale of the present study are the reason for this difference. In addition to the main question, the current scale has a preparatory question at the beginning and a visual analog clarifying the question at the end (Appendix 1). Expanding the number of items on scales has been proven to enhance diagnostic precision [34, 35].
Equally important is the concept of anxiety and depression, which is common in stroke patients and disturb the assessments. Schmid [37] highlighted the importance of managing anxiety and depression by occupational therapists and associates in handling the essentials of post-stroke care [36]. Also, the impact of confounding variables on the consistency of the tests has been underlined in several studies [37, 38].
Additionally, according to conclusions in neuroscience and motor control, psychological factors like depression and anxiety act as a direct confounding factor in disturbing postural control strategy into internal attentional focus in motor control [39, 40], so as an indirect mediator in falling and FOF [9, 41].
Considering all the mentioned cases, it seems that controlling these confounding factors (anxiety, depression) in the present study can increase the scale’s diagnostic accuracy. Also, the relationship between FES-I and psychological factors such as anxiety and depression has been reported in other studies [42, 43]. Therefore, it seems that controlling these factors in the present study and matching them in two groups with a low FOF and a high FOF have increased the diagnostic accuracy of the scale.
Conclusion
Fear of falling is a critical obstacle to an individual’s social participation and communication [44-46]. It is a highly prevalent phenomenon among stroke patients. Therefore, its early and fast screening in activities of daily living is an essential factor in post-stroke treatment [47]. Regarding the findings of these studies, FOF-RS can be considered a newly developed rating scale to screen fear of falling and assessing the effectiveness of step-by-step protocols in clinical settings for stroke patients cost-efficiently in time and other required resources.
Study Limitations
There were some limitations in completing the current study: only stroke patients with acceptable levels of walking ability (10 m) and cognition (MMSE≥23) took part in the study. So, the results are less generalizable to stroke patients with lower physical abilities and cognition.
Study Suggestions
It is suggested that the same research study be done in stroke patients with lower functional levels and other neurologic disorders.
Clinical Implications:
Developing an easy-to-administer, fast, and valid scale for screening fear of falling in stroke patients (with a cut-off point) for the first time,
Facilitating the design and step-by-step assessment of interventional protocols for fear of falling,
Early identification of at-risk stroke patients and early and proper management of subsequent restrictions in activities of daily life,
The first step is to consider anxiety and depression as confounding factors in assessing the diagnostic accuracy of fear of fall scales.
Disclosure Statement
The authors report no competing interests to declare.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this study. Ethical approval was obtained from the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1397.179).
Funding
This study was funded by the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Grant number:2138).
Authors' contributions
Conceptualization, Methodology, Validation: Ghorban Taghizadeh, Zahra Ghorbanpour, Ebrahim Pishyareh and Seyed Ali Hosseini; Analysis, investigation, Resources, initial draft preparation: All authors; Editing & review, visualization: Zahra Ghorbanpour, Ebrahim Pishyareh and Reza Osqueizadeh; Supervision, project management, and funding acquisition: Seyed Ali Hosseini, Ebrahim Pishyareh and Zahra Ghorbanpour.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all individuals participated in this study and the Deputy for Research of the University of Social Welfare and Rehabilitation Sciences for the financial support.
References
Fear of falling (FOF) is a psychological condition associated with excessive concern about losing balance [1]. This fear could lead to uncertainty, decreased physical activity, communication and balance, low self-esteem, confined social interactions, and impaired quality of life [2-4]. People who have had a stroke are more likely than other people to be subjected to FOF [5, 6]. This condition can be due to the physical and cognitive changes after a stroke [7]. In addition, stroke patients often experience falling due to their balance problems [2]. Studies have revealed a relationship between FOF and earlier falls and balance problems in stroke patients [8, 9]. Therefore, the fear of falling as one of the common factors affecting the balance and quality of life of stroke patients needs to be screened and managed early.
Also, FOF is a long-standing complication in stroke patients, so nearly 60% of the patients who have experienced a stroke report some level of FOF after being discharged [10]. Furthermore, about 50% of the patients mentioned above still report the fear of falling 6 months after the incident, though they are expected to develop adaptations to the new condition [11, 12]. Therefore, they impose an extra cost for the associated healthcare arrangements [10]. With early and fast screening of the FOF, its complications can be prevented, and the effect of treatment protocols can be checked step by step.
Some well-accepted, valid, and reliable instruments have been developed in this field, such as ABC (activities-specific balance confidence), falls efficacy scale (FES), and falls efficacy scale-international (FES-I) [13-15]. The ABC items are focused on balance confidence in mobility (not fear while performing mobility) [14, 16]. while FES and FES-I are more appropriate for evaluating the fear concept [16]. However, it should be noted that symptoms of fear of falling in social and heavy bodily activities cannot be assessed via FES [17]. Therefore, FES-I could be considered a proper alternative tool to evaluate concerns of falling in various levels of social activities [18], being widely employed as a valid and reliable indicator to assess indoor and outdoor activities [13, 19, 20]. Psychometric evaluation of this tool for stroke patients has also been completed in the Persian language, with high levels of validity and reliability [13].
Nevertheless, considering the cognitive and temporal deficits experienced after stroke (up to 22% at 5 months to 14 years after stroke) [21], the frequency and severity of fatigue in these patients [22], complicated questionnaires (eg, FES-I ) may lead to confusion and lack of motivation to participate in surveys [23]. So, applying a fast and accurate evaluation tool for fear of falling is essential.
Addressing this issue, several single-item scales have recently been developed for rapid rating and comfortable screening of FOF, but not in stroke patients. As a good example, the FOF screening scale has been psychometrically evaluated in older adults residing in nursing homes [24] and another in young-old community-dwelling [25]. However, both scales have been developed in healthy older people. Nonetheless, it should be considered that aging and stroke are two entirely different phenomena. Different nature of balance problems in stroke patients due to asymmetry in the limbs caused by unilateral neglect, and deficits in sensation, cognition, emotion and motor planning, would be evidence enough. So, it would be helpful to develop, evaluate, and validate single-item scales for rapid screening of FOF in stroke patients.
To our knowledge, there is no accurate single-item tool to assess FOF in stroke patients; therefore, the current study was carried out to design and validate a single-item scale to accurately and fast screen of FOF in stroke patients.
On the other hand, taking into account the prevalence and the effect of psychological factors, especially anxiety [26] and depression [27], on the FOF in stroke patients, and according to conclusions in neuroscience and motor control, psychological factors like depression and anxiety act as direct confounding factors in disturbing postural control strategy into internal attentional focus in motor control. Also, according to the suggestions of Meimandi and Schmid studies, for a more accurate evaluation of the FOF, in this study, these factors (anxiety and depression) were also evaluated, and their effects were controlled.
Participants and Methods
Study Design and Participants
The study followed a cross-sectional design in which 180 first-stroke patients (mean age: 55.90±12.86 years) participated. They were recruited from rehabilitation hospitals and clinics, including Rafideh Hospital, Loqman Hospital, Tajrish SHohada Hospital, Nizam Mafi Clinic, Hasti Clinic, and Iran Rehabilitation Faculty Clinic through convenience sampling, which was carried out within 3 months between December 2021 and March 2022. The main inclusion criteria were as follows: 6- to 48-month duration from the stroke, ability to stand independently (for a minimum of 90 s), ability to walk for a minimum of 10 m without assistive devices, and obtaining scores ≥44 in star cancellation test for measuring unilateral neglect [28], and ≥23 in mini-mental status examination test [29]. If the patient did not want to continue the evaluations, she/he would be excluded from the study.
An experienced occupational therapist implemented the FES-I (the questionnaire for creating low fear of falling and high fear of falling groups), hospital anxiety and depression scale (HADS) (grouping to control anxiety and depression), and FOF-rating scale (RS) (newly developed questionnaire) tests and completed the demographic questionnaire.
Sampling was done so that all the potential candidates who met the inclusion criteria and visited the hospitals and rehabilitation clinics were included in the 3-month study.
To include the variables of anxiety and depression from the beginning, two groups with a high FOF and without a high FOF were considered. Then, the participants were allocated to these groups based on their level of anxiety and depression. Participants with and without anxiety and depression were also assigned to two groups with and without a high fear of falling level. Before proceeding to statistical analyses, we ensured that the two groups with high FOF and without high FOF levels did not have any significant statistical difference in terms of anxiety and depression.
Experiments were carried out in “Javad Movaffaghiyan Research Center laboratory,” and took 20-30 minutes on average (rest was given without restriction whenever needed). Finally, raw data were processed and analyzed using IBM SPSS statistics (Version 10), and the comparisons between two groups with and without high FOF for FESI and FOF-RS were carried out accordingly.
The study received approval from the university (IR.USWR.REC.1397.179), and all participants completed and signed the informed consent forms. All ethical considerations of working with human samples were observed.
Study Assessments
Falls Efficacy Scale – International (FES-I)
The 16-item FES-I is developed upon the original form comprising 10 items from the FES questionnaire and 6 additional social activities items to assess troubles with falling in outdoor and indoor activities. Each item is scored with a 4-point Likert scale (1=not concerned at all, 4=very concerned), thus a total score of 64 representing extreme concern for falling. The psychometric properties of the Persian version have been examined in stroke patients (α=0.78) [13]. Based on the previous literature, a score of 23 was set as the cut-off point for the distribution of participants to low (<23) and high FOF (≥23) groups [18, 24, 30].
Hospital Anxiety and Depression Scale (HADS)
The HADS questionnaire comprises two sections, within which HADS-A has seven questions for anxiety, and HADS-D has 7 questions for depression. The questionnaire is a reliable tool for evaluating and screening anxiety (r=0.74) and depression (r=0.70) in stroke patients [31]. Also, the Persian version of the HADS is a reliable and valid measure for anxiety and depression [32].
Fear of Falling-Rating Scale (FOF-RS): (Appendix 1) FoF-RS has been designed to quickly screen an individual’s fear of falling through a valid single-item scale and facilitate respondent contribution. FOF over the last 6 months was quantified via a Preparation question. An opening question would remind the respondent of their FOF in the last 6 months, followed by the next question regarding fear of falling in that period on a 0-10 scale (0 representing no fear of falling at all, and 10 representing a fear that keeps the individual from performing any tasks. Also, for greater clarity, there is a visual analog scale under the question so that the patient can better rate her/his fear of falling.
Statistical Analysis
The normality of data was tested via the Shapiro-Wilk test. Taking into account the distorting effect of anxiety and depression, at first, the mean difference of these factors was compared in two groups of low FOF and high FOF with an independent sample t test. Next, MedCalc was utilized to analyze the ROC curve. Finally, FOF-RS validity in stroke patients was determined based on negative predictive value (NPV), positive predictive value (PPV), area under curve (AUC), and specificity and sensitivity.
Results
Demographic information is summarized in Table 1.
According to the FES-I questionnaire cut-off point [23], participant data were classified into two groups, including stroke patients with low FOF (scores≤23) and those with high FOF (scores>23). No statistically significant difference was observed in age, gender, cognition, anxiety, depression, and fall history between these two groups (Table 2).
Finding Cut-off Point for FOF-RS Via ROC Curve Analysis
Based on FES-I, receiver operating characteristics (ROC) curve analysis revealed a 0.83% area under the curve for stroke patients (Table 3, Figure 1).
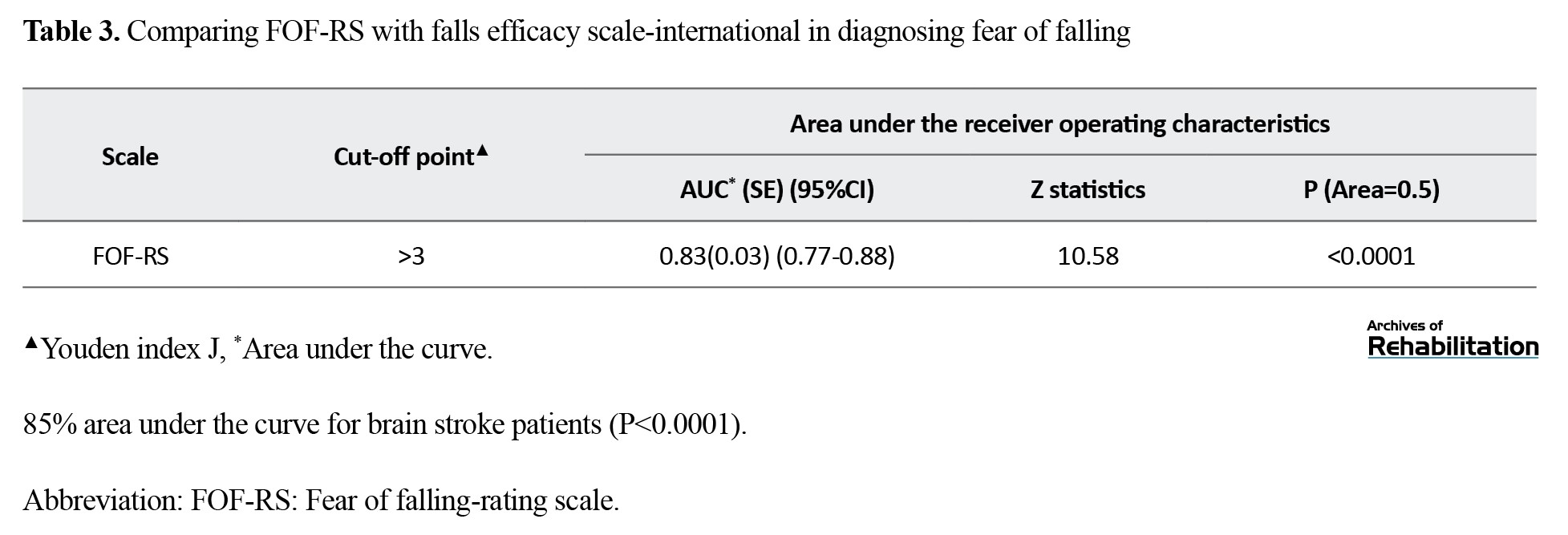
This result proves the capability of this scale for screening FOF in stroke patients. Also, the cut-off point 3 was determined for stroke patients.
Agreement Between FOF-RS and FES-I in Assessing FOF
Regarding the FOF-RS and FES-I agreement, results revealed that in those with a low FOF, the agreement was 82.3%; in those with high FOF, this agreement was 77.6% (Table 4).
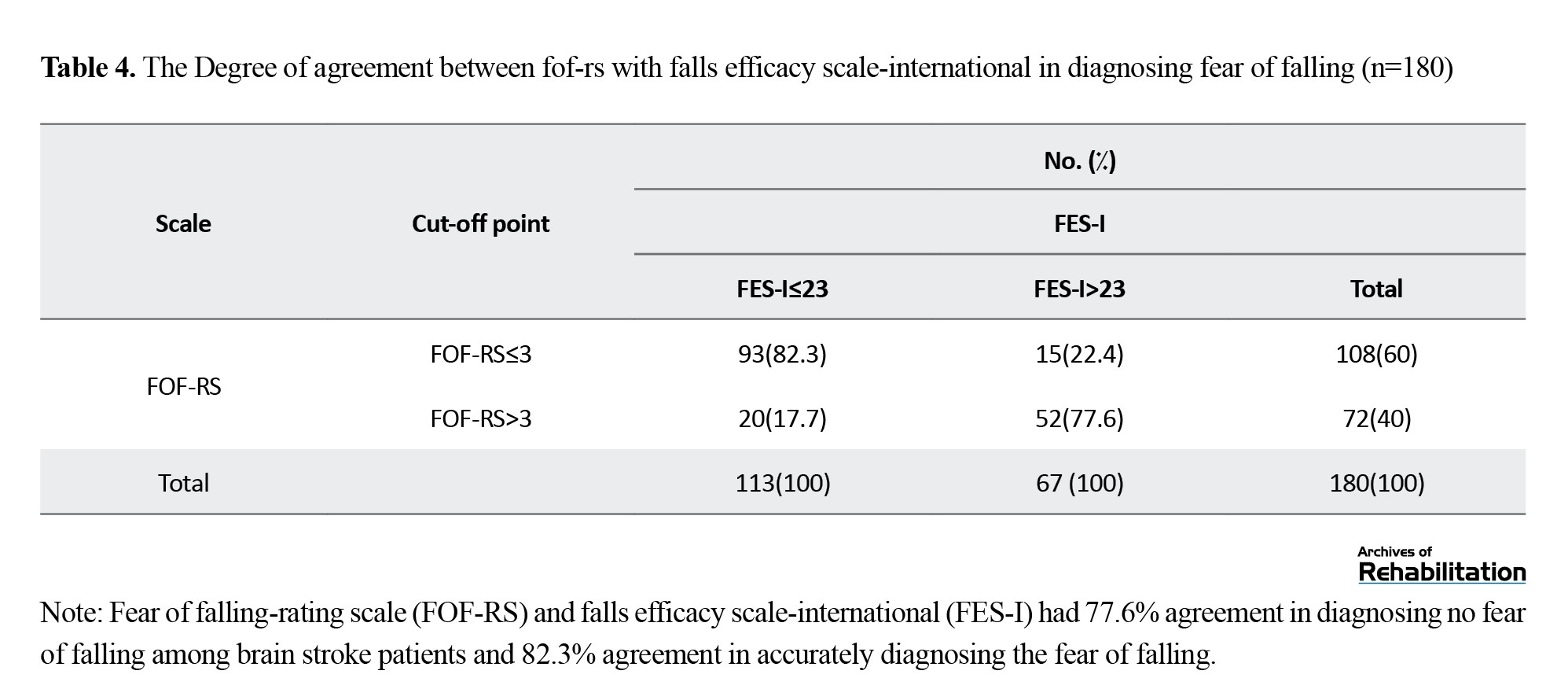
This agreement among stroke patients had acceptable compatibility levels.
Sensitivity, specificity, PPV, NPV, and AUC for Screening FOF
The sensitivity for screening for fear of falling was 77.61%. Also, specificity in this regard was 82.3% (Table 5).
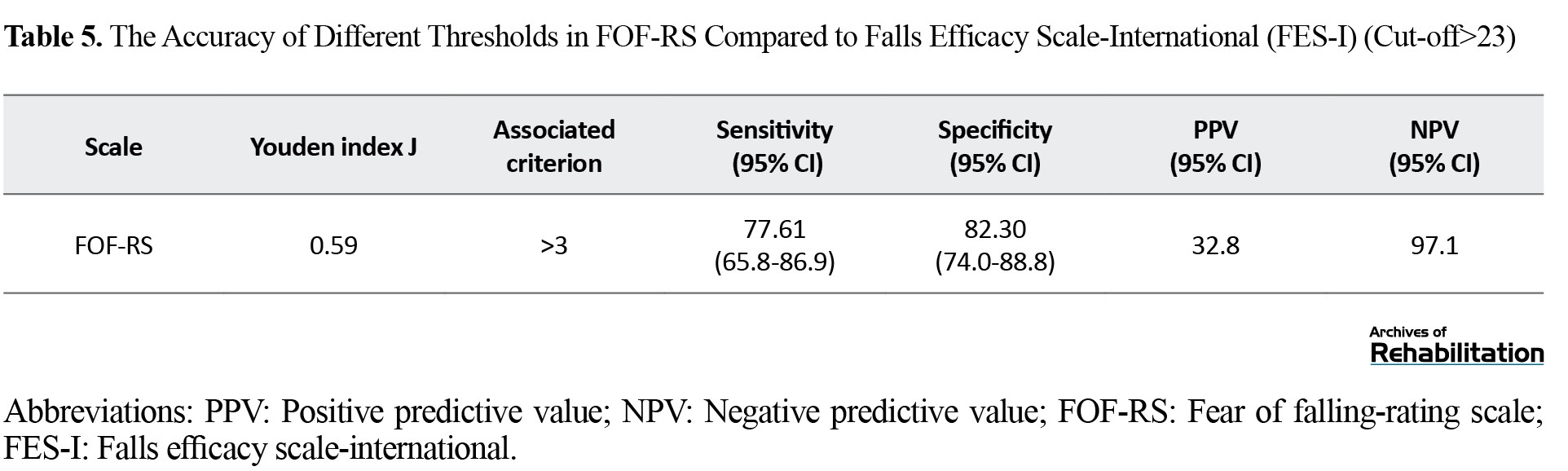
Youden index J was calculated using MedCalc (>3).
Discussion
According to the plotted ROC curve, FOF-RS showed good diagnostic accuracy for screening fear of falling in stroke patients. The cut-off point “3” for screening fear of falling in stroke patients (with controlling anxiety and depression) indicated excellent sensitivity and specificity.
This single-item scale has a unique capability of assessing and screening fear of falling in stroke patients. Belloni and Meimandi have developed single-item scales for fear of falling in older people. The current study’s results align with Belloni and Meimandi’s findings [25, 33] in older adults. However, the AUC and concordance of this scale with FES-I are higher than the single-item scale in Meimandi’s study.
It seems that the appearance and number of items in the scale of the present study are the reason for this difference. In addition to the main question, the current scale has a preparatory question at the beginning and a visual analog clarifying the question at the end (Appendix 1). Expanding the number of items on scales has been proven to enhance diagnostic precision [34, 35].
Equally important is the concept of anxiety and depression, which is common in stroke patients and disturb the assessments. Schmid [37] highlighted the importance of managing anxiety and depression by occupational therapists and associates in handling the essentials of post-stroke care [36]. Also, the impact of confounding variables on the consistency of the tests has been underlined in several studies [37, 38].
Additionally, according to conclusions in neuroscience and motor control, psychological factors like depression and anxiety act as a direct confounding factor in disturbing postural control strategy into internal attentional focus in motor control [39, 40], so as an indirect mediator in falling and FOF [9, 41].
Considering all the mentioned cases, it seems that controlling these confounding factors (anxiety, depression) in the present study can increase the scale’s diagnostic accuracy. Also, the relationship between FES-I and psychological factors such as anxiety and depression has been reported in other studies [42, 43]. Therefore, it seems that controlling these factors in the present study and matching them in two groups with a low FOF and a high FOF have increased the diagnostic accuracy of the scale.
Conclusion
Fear of falling is a critical obstacle to an individual’s social participation and communication [44-46]. It is a highly prevalent phenomenon among stroke patients. Therefore, its early and fast screening in activities of daily living is an essential factor in post-stroke treatment [47]. Regarding the findings of these studies, FOF-RS can be considered a newly developed rating scale to screen fear of falling and assessing the effectiveness of step-by-step protocols in clinical settings for stroke patients cost-efficiently in time and other required resources.
Study Limitations
There were some limitations in completing the current study: only stroke patients with acceptable levels of walking ability (10 m) and cognition (MMSE≥23) took part in the study. So, the results are less generalizable to stroke patients with lower physical abilities and cognition.
Study Suggestions
It is suggested that the same research study be done in stroke patients with lower functional levels and other neurologic disorders.
Clinical Implications:
Developing an easy-to-administer, fast, and valid scale for screening fear of falling in stroke patients (with a cut-off point) for the first time,
Facilitating the design and step-by-step assessment of interventional protocols for fear of falling,
Early identification of at-risk stroke patients and early and proper management of subsequent restrictions in activities of daily life,
The first step is to consider anxiety and depression as confounding factors in assessing the diagnostic accuracy of fear of fall scales.
Disclosure Statement
The authors report no competing interests to declare.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this study. Ethical approval was obtained from the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1397.179).
Funding
This study was funded by the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Grant number:2138).
Authors' contributions
Conceptualization, Methodology, Validation: Ghorban Taghizadeh, Zahra Ghorbanpour, Ebrahim Pishyareh and Seyed Ali Hosseini; Analysis, investigation, Resources, initial draft preparation: All authors; Editing & review, visualization: Zahra Ghorbanpour, Ebrahim Pishyareh and Reza Osqueizadeh; Supervision, project management, and funding acquisition: Seyed Ali Hosseini, Ebrahim Pishyareh and Zahra Ghorbanpour.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all individuals participated in this study and the Deputy for Research of the University of Social Welfare and Rehabilitation Sciences for the financial support.
References
- Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing. 2008; 37(1):19-24. [DOI:10.1093/ageing/afm169] [PMID]
- Larén A, Odqvist A, Hansson PO, Persson CU. Fear of falling in acute stroke: The Fall Study of Gothenburg (FallsGOT). Topics in Stroke Rehabilitation. 2018; 25(4):256-60. [DOI:10.1080/10749357.2018.1443876] [PMID]
- Liu TW, Ng GYF, Chung RCK, Ng SSM. Cognitive behavioural therapy for fear of falling and balance among older people: A systematic review and meta-analysis. Age and Ageing. 2018; 47(4):520-7. [DOI:10.1093/ageing/afy010] [PMID]
- Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. Journal of Epidemiology and Community Health. 2003; 57(9):740-4. [DOI:10.1136/jech.57.9.740] [PMID]
- Goh HT, Nadarajah M, Hamzah NB, Varadan P, Tan MP. Falls and fear of falling after stroke: A case-control study. PM&R. 2016; 8(12):1173-80. [DOI:10.1016/j.pmrj.2016.05.012] [PMID]
- Hyndman D, Ashburn A, Stack E. Fall events among people with stroke living in the community: Circumstances of falls and characteristics of fallers. Archives of Physical Medicine and Rehabilitation. 2002; 83(2):165-70. [DOI:10.1053/apmr.2002.28030] [PMID]
- Schmid AA, Rittman M. Fear of falling: An emerging issue after stroke. Topics in Stroke Rehabilitation. 2007; 14(5):46-55. [DOI:10.1310/tsr1405-46] [PMID]
- Andersson ÅG, Kamwendo K, Appelros P. Fear of falling in stroke patients: Relationship with previous falls and functional characteristics. International Journal of Rehabilitation Research. 2008; 31(3):261-4. [DOI:10.1097/MRR.0b013e3282fba390] [PMID]
- Guan Q, Jin L, Li Y, Han H, Zheng Y, Nie Z. Multifactor analysis for risk factors involved in the fear of falling in patients with chronic stroke from mainland China. Topics in Stroke Rehabilitation. 2015; 22(5):368-73. [DOI:10.1179/1074935714Z.0000000048] [PMID]
- Watanabe Y. Fear of falling among stroke survivors after discharge from inpatient rehabilitation. International Journal of Rehabilitation Research. 2005; 28(2):149-52. [DOI:10.1097/00004356-200506000-00008] [PMID]
- Kim EJ, Kim DY, Kim WH, Lee KL, Yoon YH, Park JM, et al. Fear of falling in subacute hemiplegic stroke patients: Associating factors and correlations with quality of life. Annals of Rehabilitation Medicine. 2012; 36(6):797-803. [DOI:10.5535/arm.2012.36.6.797] [PMID]
- Schmid AA, Arnold SE, Jones VA, Ritter MJ, Sapp SA, Van Puymbroeck M. Fear of falling in people with chronic stroke. The American Journal of Occupational Therapy. 2015; 69(3):6903350020. [DOI:10.5014/ajot.2015.016253] [PMID]
- Azad A, Hassani Mehraban A, Mehrpour M, Mohammadi B. Clinical assessment of fear of falling after stroke: Validity, reliability and responsiveness of the Persian version of the Fall Efficacy Scale-International. Medical Journal of the Islamic Republic of Iran. 2014; 28:131. [PMID]
- Azad A, Taghizadeh G, Mohammadian E, Mohammadinezhad T, Lajevardi L. Persian translation and Test-retest reliability of the Activities-specific Balance Confidence Scale in Iranian Chronic Stroke. Journal of Modern Rehabilitation. 2016; 10(2):74-9. [Link]
- Mosallanezhad Z, Salavati M, Hellström K, Reza Sotoudeh G, Nilsson Wikmar L, Frändin K. Cross-cultural adaptation, reliability and validity of the Persian version of the modified falls efficacy scale. Disability and Rehabilitation. 2011; 33(25-26):2446-53. [DOI:10.3109/09638288.2011.574774] [PMID]
- Moore DS, Ellis R. Measurement of fall-related psychological constructs among independent-living older adults: A review of the research literature. Aging and Mental Health. 2008; 12(6):684-99. [DOI:10.1080/13607860802148855] [PMID]
- Büla CJ, Martin E, Rochat S, Piot-Ziegler C. Validation of an adapted falls efficacy scale in older rehabilitation patients. Archives of Physical Medicine and Rehabilitation. 2008; 89(2):291-6. [DOI:10.1016/j.apmr.2007.08.152] [PMID]
- Delbaere K, Close JC, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The falls efficacy scale international (FES-I). A comprehensive longitudinal validation study. Age and Ageing. 2010; 39(2):210-6. [DOI:10.1093/ageing/afp225] [PMID]
- Billis E, Strimpakos N, Kapreli E, Sakellari V, Skelton DA, Dontas I, et al. Cross-cultural validation of the Falls Efficacy Scale International (FES-I) in Greek community-dwelling older adults. Disability and Rehabilitation. 2011; 33(19-20):1776-84. [DOI:10.3109/09638288.2010.546937] [PMID]
- Morgan MT, Friscia LA, Whitney SL, Furman JM, Sparto PJ. Reliability and validity of the Falls Efficacy Scale-International (FES-I) in individuals with dizziness and imbalance. Otology & Neurotology. 2013; 34(6):1104-8. [Link]
- Douiri A, Rudd AG, Wolfe CD. Prevalence of poststroke cognitive impairment: South London stroke register 1995-2010. Stroke. 2013; 44(1):138-45. [DOI:10.1161/STROKEAHA.112.670844] [PMID]
- Glader EL, Stegmayr B, Asplund K. Poststroke fatigue: A 2-year follow-up study of stroke patients in Sweden. Stroke. 2002; 33(5):1327-33. [DOI:10.1161/01.STR.0000014248.28711.D6] [PMID]
- Rolstad S, Adler J, Rydén A. Response burden and questionnaire length: Is shorter better? A review and meta-analysis. Value in Health. 2011; 14(8):1101-8. [DOI:10.1016/j.jval.2011.06.003] [PMID]
- Meimandi M, Fadavi-Ghaffari M, Taghizadeh G, Azad A, Lajevardi L. Falls efficacy scale and single item question: screening accuracy for older adults residing in nursing homes. Clinical Gerontologist. 2021; 44(5):544-51. [DOI:10.1080/07317115.2020.1858467] [PMID]
- Belloni G, Büla C, Santos-Eggimann B, Henchoz Y, Seematter-Bagnoud L. A single question as a screening tool to assess fear of falling in young-old community-dwelling persons. Journal of The American Medical Directors Association. 2020; 21(9):1295-301. e2. [DOI:10.1016/j.jamda.2020.01.101] [PMID]
- Cumming TB, Blomstrand C, Skoog I, Linden T. The high prevalence of anxiety disorders after stroke. The American Journal of Geriatric Psychiatry. 2016; 24(2):154-60. [DOI:10.1016/j.jagp.2015.06.003] [PMID]
- Park S, Cho OH. Fear of falling and related factors during everyday activities in patients with chronic stroke. Applied Nursing Research. 2021; 62:151492. [DOI:10.1016/j.apnr.2021.151492] [PMID]
- Friedman PJ. The star cancellation test in acute stroke. Clinical Rehabilitation. 1992; 6(1):23-30. [DOI:10.1177/026921559200600104]
- Ansari NN, Naghdi S, Hasson S, Valizadeh L, Jalaie S. Validation of a Mini-Mental State Examination (MMSE) for the Persian population: A pilot study. Applied Neuropsychology. 2010; 17(3):190-5. [PMID]
- Sheikh M, Hosseini HA. Influence of fear of falling severity measured by falls efficacy scale-international on gait and balance performance after chronic stroke. Iranian Rehabilitation Journal. 2020; 18(1):73-80. [DOI:10.32598/irj.18.1.911.1]
- Aben I, Verhey F, Lousberg R, Lodder J, Honig A. Validity of the beck depression inventory, hospital anxiety and depression scale, SCL-90, and hamilton depression rating scale as screening instruments for depression in stroke patients. Psychosomatics. 2002; 43(5):386-93. [DOI:10.1176/appi.psy.43.5.386] [PMID]
- Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health and Quality of Life Outcomes. 2003; 1:14. [DOI:10.1186/1477-7525-1-19] [PMID]
- Meimandi M, Azad A, Taghizadeh G, Mohammadi P. Validation and diagnostic accuracy of coin rotation task for manual dexterity and coordination in children with specific learning disorder. Disability and Rehabilitation. 2022; 44(10):2073-82. [DOI:10.1080/09638288.2020.1810788] [PMID]
- Carey M, Jones KA, Yoong SL, D'Este C, Boyes AW, Paul C, et al. Comparison of a single self-assessment item with the PHQ-9 for detecting depression in general practice. Family Practice. 2014; 31(4):483-9. [DOI:10.1093/fampra/cmu018] [PMID]
- Yohannes AM, Dodd M, Morris J, Webb K. Reliability and validity of a single item measure of quality of life scale for adult patients with cystic fibrosis. Health and Quality of Life Outcomes. 2011; 9:105. [DOI:10.1186/1477-7525-9-105] [PMID]
- Schmid AA, Van Puymbroeck M, Knies K, Spangler-Morris C, Watts K, Damush T, et al. Fear of falling among people who have sustained a stroke: a 6-month longitudinal pilot study. The American Journal of Occupational Therapy. 2011; 65(2):125-32. [DOI:10.5014/ajot.2011.000737] [PMID]
- Capozzi VA, Merisio C, Rolla M, Pugliese M, Morganelli G, Cianciolo A, et al. Confounding factors of transvaginal ultrasound accuracy in endometrial cancer. Journal of Obstetrics and Gynaecology. 2021; 41(5):779-84. [DOI:10.1080/01443615.2020.1799342] [PMID]
- Skelly AC, Dettori JR, Brodt ED. Assessing bias: the importance of considering confounding. Evidence-Based Spine-Care Journal. 2012; 3(1):9-12. [DOI:10.1055/s-0031-1298595] [PMID]
- Cocks AJ, Jackson RC, Bishop DT, Williams AM. Anxiety, anticipation and contextual information: A test of attentional control theory. Cognition and Emotion. 2016; 30(6):1037-48. [DOI:10.1080/02699931.2015.1044424] [PMID]
- Ghorbanpour Z, Taghizadeh G, Hosseini SA, Pishyareh E, Ghomsheh FT, Bakhshi E, et al. Overload of anxiety on postural control impairments in chronic stroke survivors: The role of external focus and cognitive task on the automaticity of postural control. Plos One. 2021; 16(7):e0252131. [PMID]
- Schinkel-Ivy A, Inness EL, Mansfield A. Relationships between fear of falling, balance confidence, and control of balance, gait, and reactive stepping in individuals with sub-acute stroke. Gait & Posture. 2016; 43:154-9. [DOI:10.1016/j.gaitpost.2015.09.015] [PMID]
- Biderman A, Cwikel J, Fried AV, Galinsky D. Depression and falls among community dwelling elderly people: A search for common risk factors. Journal of Epidemiology & Community Health. 2002; 56(8):631-6. [DOI:10.1136/jech.56.8.631] [PMID]
- Martin FC, Hart D, Spector T, Doyle DV, Harari D. Fear of falling limiting activity in young-old women is associated with reduced functional mobility rather than psychological factors. Age and Ageing. 2005; 34(3):281-7. [DOI:10.1093/ageing/afi074] [PMID]
- Barnsley L, McCluskey A, Middleton S. What people say about travelling outdoors after their stroke: A qualitative study. Australian Occupational Therapy Journal. 2012; 59(1):71-8. [DOI:10.1111/j.1440-1630.2011.00935.x] [PMID]
- Robison J, Wiles R, Ellis-Hill C, McPherson K, Hyndman D, Ashburn A.Resuming previously valued activities post-stroke: who or what helps? Disability and Rehabilitation. 2009; 31(19):1555-66. [DOI:10.1080/09638280802639327] [PMID]
- Mehdizadeh M, Martinez-Martin P, Habibi SA, Nikbakht N, Alvandi F, Bazipoor P, et al. The association of balance, fear of falling, and daily activities with drug phases and severity of disease in patients with Parkinson. Basic and Clinical Neuroscience. 2019; 10(4):355–61. [PMID]
- Schmid AA, Rittman M. Consequences of poststroke falls: activity limitation, increased dependence, and the development of fear of falling. The American Journal of Occupational Therapy. 2009; 63(3):310-6. [DOI:10.5014/ajot.63.3.310] [PMID]
- Taghizadeh G, Martinez-Martin P, Fereshtehnejad SM, Habibi SA, Nikbakht N, Alizadeh NH, et al. Psychometric properties of the Berg balance scale in idiopathic Parkinson’disease in the drug off-phase. Neurological Sciences. 2018; 39(12):2175-81. [PMID]
- Mahmoudi Asl A, Mehdizadeh M, Kulisevsky J, Sabet A, Taghavi Azar Sharabiani P, Mehdizadeh H, et al. Reliability, validity, and diagnostic accuracy of Parkinson's Disease-Cognitive Rating Scale in Iranian patients with idiopathic Parkinson's disease. Disability and Rehabilitation. 2022; 44(10):2091-8. [PMID]
Type of Study: Original |
Subject:
Occupational Therapy
Received: 1/12/2023 | Accepted: 23/04/2024 | Published: 1/01/2025
Received: 1/12/2023 | Accepted: 23/04/2024 | Published: 1/01/2025
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |