Volume 25, Issue 3 (Autumn 2024)
jrehab 2024, 25(3): 448-463 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseini S M S, Rostami M H, Bakhtiari M, Soltanian A, Nurani Gharaborghe S. The Effect of Pelvic Floor Muscle Exercises on Urinary Incontinence and Leisure Time Activities of Women With Multiple Sclerosis. jrehab 2024; 25 (3) :448-463
URL: http://rehabilitationj.uswr.ac.ir/article-1-3399-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3399-en.html
Seyed Mohammad Sadegh Hosseini1 

 , Mohammad Hadi Rostami1
, Mohammad Hadi Rostami1 

 , Mahsa Bakhtiari1
, Mahsa Bakhtiari1 

 , Alireza Soltanian2
, Alireza Soltanian2 

 , Sahar Nurani Gharaborghe *3
, Sahar Nurani Gharaborghe *3 




 , Mohammad Hadi Rostami1
, Mohammad Hadi Rostami1 

 , Mahsa Bakhtiari1
, Mahsa Bakhtiari1 

 , Alireza Soltanian2
, Alireza Soltanian2 

 , Sahar Nurani Gharaborghe *3
, Sahar Nurani Gharaborghe *3 


1- Department of Occupational Therapy, School of Rehabilitation Sciences, Hamadan University of Medical Sciences, Hamadan, Iran.
2- Department of Biostatistics and Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran.
3- Department of Occupational Therapy, School of Rehabilitation Sciences, Hamadan University of Medical Sciences, Hamadan, Iran. ,saharnurani@yahoo.com
2- Department of Biostatistics and Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran.
3- Department of Occupational Therapy, School of Rehabilitation Sciences, Hamadan University of Medical Sciences, Hamadan, Iran. ,
Keywords: Pelvic floor training, Fatigue, Recreation, Neurological disorders, Bladder control problems
Full-Text [PDF 1298 kb]
(781 Downloads)
| Abstract (HTML) (8487 Views)
Full-Text: (950 Views)
Introduction
Multiple sclerosis (MS) is a disorder characterized by an initial immune attack on the brain and spinal cord. This attack ultimately results in demyelination [1]. Clinical manifestations of MS can vary from person to person, but common symptoms include fatigue, urinary incontinence, and limitations in social activities [2].
Urinary incontinence poses social and hygiene challenges and can manifest as urge incontinence, stress incontinence, or mixed incontinence, with the mixed type being most common in MS patients.
The prevalence of urinary and reproductive system disorders in patients with MS is a significant concern, with approximately 90% of individuals with MS experiencing urinary symptoms [3]. Urinary incontinence poses social and hygiene challenges [4] and can manifest as urge incontinence, stress incontinence, or mixed incontinence [5], with the mixed type being most common in MS patients [6].
Knowing leisure time and its aspects is important and can improve people’s quality of life (QoL) and well-being [7]. On the other hand, leisure time is one of the first areas of life that the patient overlooks [8]. The presence of disability leads to less diversity in participation, especially participation in leisure time and these people do most of their work inside the home and create less social contact [9].
Fatigue is one of the most prevalent symptoms that affects nearly 80% of patients with MS. Additionally, approximately 55% of individuals describe fatigue as one of the most challenging symptoms they experience [10]. In MS, fatigue is categorized into primary and secondary types, and from a pathogenic perspective, distinctions can be observed between these two forms [11]. Within the first year of the disease, fatigue levels can escalate up to 85% and with disease progression, it can increase even further, reaching up to 95% [12].
Several treatment approaches can be considered to tackle the issues mentioned above in patients with MS. Traditional pelvic floor exercises such as Kegel exercises, biofeedback techniques, the use of vaginal perineometers, and ultrasound stimulation have all been explored. Research studies have found that teaching Kegel exercises alone can alleviate urinary incontinence symptoms among MS patients. Engaging in pelvic floor muscle strengthening exercises using the mentioned methods brings about positive changes in the QoL, severity of bladder symptoms, proximal contraction, as well as levels of anxiety and depression in patients [13]. It has been shown that strengthening the pelvic floor muscles through vaginal perineometer can effectively manage and improve urinary incontinence symptoms in women with MS. Techniques such as biofeedback, electromyography, and neuromuscular stimulation targeted at the pelvic floor muscles have also been found to be beneficial in improving urinary incontinence [14].
Exercises targeting the pelvic floor muscles are initially performed in three positions: Lying down, sitting, and standing. The contractions begin after a 3-second hold and continue for 10 seconds. Patients perform these exercises consecutively for 12 weeks at home, gradually increasing the number of contractions to reach 90 to 100 contractions per day [13]. In a study by Stiff et al. the effects of three exercises (plank, leg lift, bird dog) on postpartum women’s pelvic floor muscles were examined, demonstrating that these exercises could serve as a viable alternative to the Kegel method [15]. Given the challenges concerning urinary control in female patients with MS and its implications on their daily activities, coupled with the existing research gap in this field, this study seeks to explore the therapeutic benefits of these pelvic floor muscle exercises on urinary incontinence and leisure activities in women with MS.
Materials and Methods
Study design and population
This study implemented a quasi-experimental design The study participants were selected from the MS patient population in Hamadan City, Iran. The sample selection was done using a simple non-probability sampling method. To determine the appropriate sample size, G*Power software, version 3.1.9.7 was utilized, taking into account the chosen statistical test and considering effect size d=0.7, α=0.05, and power=0.80. Ultimately, it resulted in a sample size of 15 individuals.
This study was conducted at the Clinical Rehabilitation Clinic of Farshchian Hospital in Hamadan City, Iran, in 2022. Participants were selected based on specific inclusion criteria, including having an EDSS score of seven or less, being able to read and write and lacking any other orthopedic or neurological diseases. The exclusion criteria were established to consider factors such as participants’ dissatisfaction with any stage of the research implementation.
Study procedure
In this study, a therapeutic program was implemented to strengthen the pelvic floor muscles in participants. The program consisted of three specific exercises: Bird dog, plank and leg lift. The exercises were conducted in sets of 10 repetitions, alternating between exercises, and were done three times a day. Participants were instructed to perform one session in the clinic and two sessions at home, totaling 3 days per week for 8 weeks. A table was provided in a booklet for patients to record their exercise sessions. These exercises were supervised by occupational therapists and conducted through telephone follow-ups. It is important to note that no other interventions, such as medication therapy, physiotherapy, or occupational therapy, were implemented. Participants were encouraged to continue their routine treatment alongside the pelvic floor exercises.
Study outcomes
International consultation on incontinence questionnaire-urinary incontinence short form (ICIQ-UI SF)
Avery et al. developed this research tool for this study. It evaluates various aspects of urinary incontinence, such as frequency, amount of leakage, impact on QoL and duration. The total score is derived by summing scores from questions pertaining to frequency, leakage amount, and impact on QoL. The scale encompasses 0 to 21 variables. The final question addresses the type of incontinence but is not assigned a numerical score. Greater scores signify increased severity of incontinence [16]. Hajebrahimi et al. translated this questionnaire into multiple languages and validated it in Iran [17].
Fatigue severity scale (FSS)
This questionnaire measures the severity of excessive fatigue in daily functioning. It includes 9 questions rated on a scale of 1 to 7. The questionnaire is highly reliable in assessing fatigue severity in patients with MS [18]. It provides a comprehensive evaluation of fatigue, with the score directly reflecting the level and intensity of fatigue experienced by the patient. The Persian version of the questionnaire has been validated and confirmed for its validity and reliability by Azimian et al. [19].
Iranian-developed version of the leisure questionnaire for people with MS
This tool has been developed by Hosseini et al. to measure the level of leisure time activity in MS patients. It consists of 50 items that are scored on a Likert scale, ranging from “often,” “sometimes,” “usually,” “rarely,” to “never” [20]. The content validity, convergent validity, and differential validity of this tool have been calculated, and it has been shown to have an acceptable level of validity [21]. In this study, all patients completed questionnaires before and after the treatment program.
Data analysis
The data have been entered into SPSS software, version 23 for activity analysis. For each variable, the data will be compared before and after the exercises using the Wilcoxon test. Additionally, the relationship between variables will be examined using the Spearman correlation test.
Results
The study patients have an Mean±SD age of 8.18±43.83 years. Their expanded disability status scale (EDSS) scores Mean±SD, 1.88±4.25. Furthermore, the duration of diagnosis in months Mean±SD, 73.22±121.33. Comprehensive demographic information about the patients is available in Table 1.
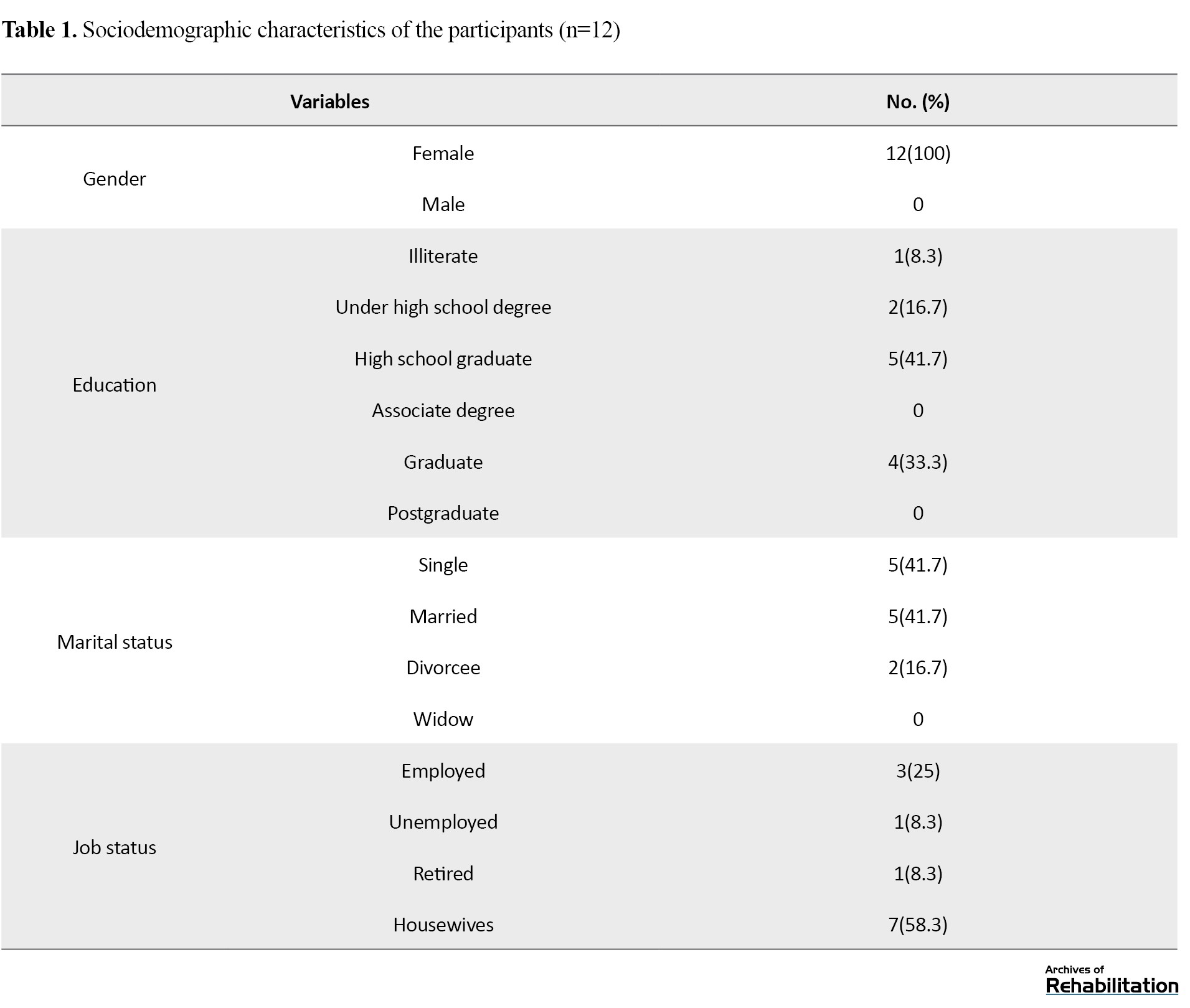
During the research, three individuals could not complete the study (one due to disease relapse and two due to lack of interest in continuing the exercises). Consequently, data from 12 patients were entered into SPSS software, version 23. The analysis revealed a calculated value of <0.05. To examine the impact of pelvic floor exercises on patients’ urinary control and leisure time, the study employed the Wilcoxon statistical test and the resulting findings are presented in Table 2.
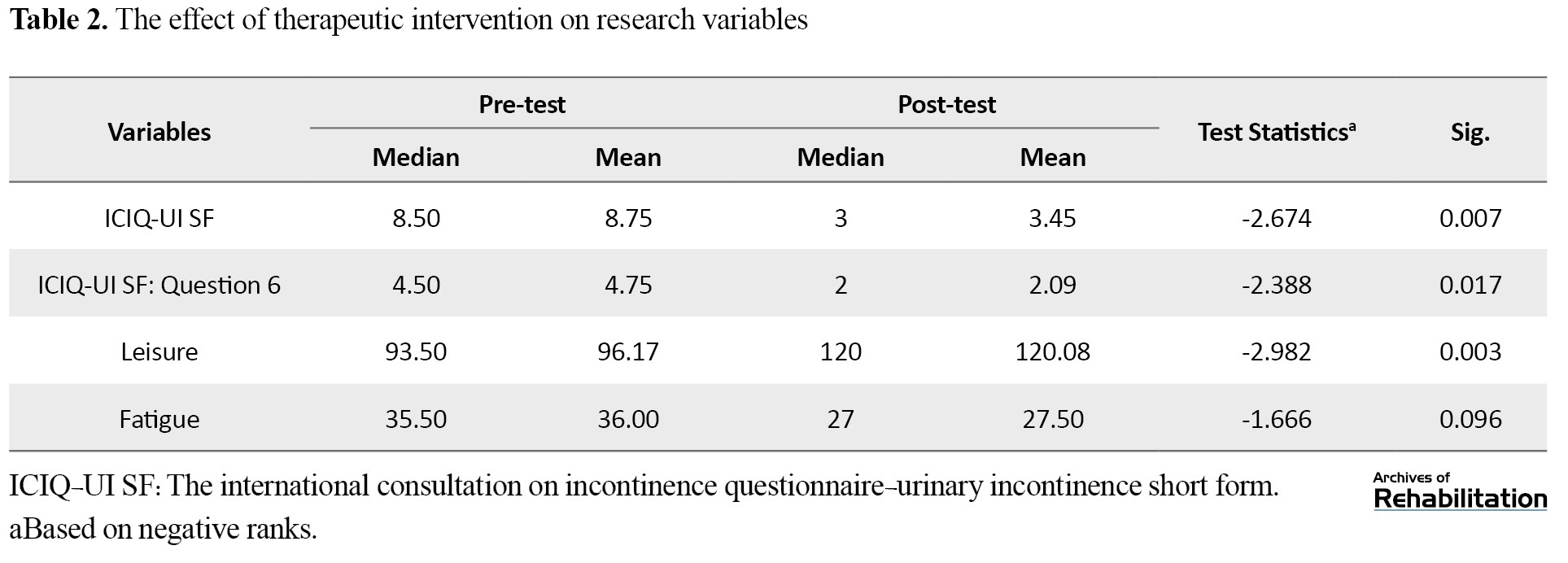
Indeed, as observed in Table 2, pelvic floor exercises effectively improve patients’ urinary control and leisure time. However, their fatigue levels showed no significant impact (P=0.05).
Discussion
This study found that pelvic floor exercises can be beneficial for managing urinary incontinence in women with MS. The results showed a significant improvement in symptoms after implementing a structured exercise program.
This study is significant because it focuses on women with MS, who often face specific challenges in managing urinary symptoms. The positive results indicate that pelvic floor exercises can be an effective non-pharmacological intervention for improving urinary control in this group [22]. The improvements are attributed to the strengthening of pelvic floor muscles, which play a crucial role in maintaining continence [23]. Regular exercise targeting these muscles can increase muscle tone and improve bladder control in women with MS [24].
Multiple studies have investigated the effects of pelvic floor exercises on urinary incontinence in women with MS. Pérez et al. [25] found similar results to the present research, showing a significant reduction in symptoms with a structured exercise program [25]. This alignment strengthens the evidence for the effectiveness of this intervention. Additionally, Lucio et al. [26] demonstrated that combining pelvic floor exercises with a vaginal perineometer had a greater impact on urinary incontinence compared to using the perineometer alone .
Chen et al. [27] further supported the effectiveness of a comprehensive approach combining pelvic floor exercises, bladder training, and lifestyle modifications for improved outcomes in managing urinary incontinence in women with MS.
Existing research backs the beneficial effects of pelvic floor exercises on urinary incontinence in women with MS. However, it is important to consider variations in study design, exercise protocols, sample sizes and additional interventions that may affect outcomes. This study also explores the effects of pelvic floor exercises on leisure activities in women with MS. Leisure activities are crucial for maintaining a good QoL. Still, MS can present challenges that hinder participation. Understanding the relationship between pelvic floor exercises and leisure activities can contribute to a holistic approach to managing MS. The study found a positive association between pelvic floor exercises and improvements in leisure activities among women with MS. Regular exercise increases participation and enjoyment in social gatherings and hobbies. This outcome may be attributed to improved physical functioning, reduced urinary symptoms, increased confidence, and enhanced ability to engage in recreational activities. Strengthening the pelvic floor muscles through exercise can improve balance, stability, and coordination, facilitating active participation in leisure activities.
Limited research has specifically examined the effects of pelvic floor exercises on leisure activities in women with MS. However, Rafii et al. [28] investigated the impact of physical exercise interventions, including pelvic floor exercises, on QoL in individuals with MS. Although leisure activities were not specifically studied, the research reported significant improvements in overall QoL, including physical and social well-being. These findings indirectly suggest that physical exercise interventions, such as pelvic floor exercises, may also positively influence leisure activities [28]. Additionally, Petajan et al. [29] demonstrated that aerobic exercises can improve bowel and bladder control and leisure time in patients with MS.
Miletta et al. [30] examined the effects of a multidisciplinary management approach, including pelvic floor exercises, on functional outcomes in individuals with MS. The research reported improvements in pelvic floor functioning, which could positively impact the ability to engage in leisure activities. Nevertheless, the study did not directly assess the influence on leisure activities, underscoring the necessity for additional research in this domain. It is crucial to acknowledge the scarcity of targeted studies on the impact of pelvic floor exercises on leisure activities in women with MS. Further research would enhance comprehension of how pelvic floor exercises affect leisure activities. Despite the initial hypothesis, the study did not observe a notable decrease in fatigue levels after pelvic floor exercise interventions. Factors such as the heterogeneity of MS symptoms, individual variations in disease progression, and the duration and intensity of the exercise interventions may have influenced these results. Other factors, such as psychological or lifestyle-related aspects, that were not considered in the study could have also influenced fatigue outcomes.
Only one study identified that specifically investigated the influence of pelvic floor exercises on fatigue levels in individuals with MS. This study, conducted by Ghafari and colleagues [31], illustrated a positive impact of pelvic floor exercises on fatigue in patients with urinary incontinence. The discrepancy in results between the provided treatment protocol and Ghafari’s study may account for the observed differences. A review of existing studies indicates the necessity for further research to comprehensively grasp the impact of pelvic floor exercises on fatigue in women with MS.
One limitation of this study is the inability to reach the desired number of participants in the study group and the inability to sample randomly, mainly due to limited access to the target population at research centers and inclusion and exclusion criteria. It is suggested that further research be conducted to determine appropriate exercise protocols, duration, and frequency for achieving the best results in women with MS. Furthermore, it is recommended that these exercises be included in the therapeutic program for patients.
Conclusion
Although this study offers evidence on how pelvic floor exercises can help decrease urinary incontinence and improve leisure activities in women with MS, caution should be exercised in generalizing the results due to the limited number of participants. Additionally, researching the long-term effects and sustainability of the intervention would offer valuable insights for healthcare professionals and patients, enhancing our understanding of the enduring benefits of pelvic floor exercises.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Hamadan University of Medical Sciences (Code: IR.UMSHA.REC.1399.080) and also approved by Iranian Registry of Clinical Trials (IRCT) (Code:IRCT20200509047370N1).
Funding
This study was supported by the Research Deputy of Hamadan University of Medical Sciences (Grand No.: 9909256560).
Authors' contributions
Conceptualization: Seyed Mohammad Sadegh Hosseini and Sahar Nurani Gharaborghe; Research and review: All authors; Review, editing and final approval: Seyed Mohammad Sadegh Hosseini and Sahar Nurani Gharaborghe.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers wish to extend their appreciation to the patients who took part in this study.
Refrences
Multiple sclerosis (MS) is a disorder characterized by an initial immune attack on the brain and spinal cord. This attack ultimately results in demyelination [1]. Clinical manifestations of MS can vary from person to person, but common symptoms include fatigue, urinary incontinence, and limitations in social activities [2].
Urinary incontinence poses social and hygiene challenges and can manifest as urge incontinence, stress incontinence, or mixed incontinence, with the mixed type being most common in MS patients.
The prevalence of urinary and reproductive system disorders in patients with MS is a significant concern, with approximately 90% of individuals with MS experiencing urinary symptoms [3]. Urinary incontinence poses social and hygiene challenges [4] and can manifest as urge incontinence, stress incontinence, or mixed incontinence [5], with the mixed type being most common in MS patients [6].
Knowing leisure time and its aspects is important and can improve people’s quality of life (QoL) and well-being [7]. On the other hand, leisure time is one of the first areas of life that the patient overlooks [8]. The presence of disability leads to less diversity in participation, especially participation in leisure time and these people do most of their work inside the home and create less social contact [9].
Fatigue is one of the most prevalent symptoms that affects nearly 80% of patients with MS. Additionally, approximately 55% of individuals describe fatigue as one of the most challenging symptoms they experience [10]. In MS, fatigue is categorized into primary and secondary types, and from a pathogenic perspective, distinctions can be observed between these two forms [11]. Within the first year of the disease, fatigue levels can escalate up to 85% and with disease progression, it can increase even further, reaching up to 95% [12].
Several treatment approaches can be considered to tackle the issues mentioned above in patients with MS. Traditional pelvic floor exercises such as Kegel exercises, biofeedback techniques, the use of vaginal perineometers, and ultrasound stimulation have all been explored. Research studies have found that teaching Kegel exercises alone can alleviate urinary incontinence symptoms among MS patients. Engaging in pelvic floor muscle strengthening exercises using the mentioned methods brings about positive changes in the QoL, severity of bladder symptoms, proximal contraction, as well as levels of anxiety and depression in patients [13]. It has been shown that strengthening the pelvic floor muscles through vaginal perineometer can effectively manage and improve urinary incontinence symptoms in women with MS. Techniques such as biofeedback, electromyography, and neuromuscular stimulation targeted at the pelvic floor muscles have also been found to be beneficial in improving urinary incontinence [14].
Exercises targeting the pelvic floor muscles are initially performed in three positions: Lying down, sitting, and standing. The contractions begin after a 3-second hold and continue for 10 seconds. Patients perform these exercises consecutively for 12 weeks at home, gradually increasing the number of contractions to reach 90 to 100 contractions per day [13]. In a study by Stiff et al. the effects of three exercises (plank, leg lift, bird dog) on postpartum women’s pelvic floor muscles were examined, demonstrating that these exercises could serve as a viable alternative to the Kegel method [15]. Given the challenges concerning urinary control in female patients with MS and its implications on their daily activities, coupled with the existing research gap in this field, this study seeks to explore the therapeutic benefits of these pelvic floor muscle exercises on urinary incontinence and leisure activities in women with MS.
Materials and Methods
Study design and population
This study implemented a quasi-experimental design The study participants were selected from the MS patient population in Hamadan City, Iran. The sample selection was done using a simple non-probability sampling method. To determine the appropriate sample size, G*Power software, version 3.1.9.7 was utilized, taking into account the chosen statistical test and considering effect size d=0.7, α=0.05, and power=0.80. Ultimately, it resulted in a sample size of 15 individuals.
This study was conducted at the Clinical Rehabilitation Clinic of Farshchian Hospital in Hamadan City, Iran, in 2022. Participants were selected based on specific inclusion criteria, including having an EDSS score of seven or less, being able to read and write and lacking any other orthopedic or neurological diseases. The exclusion criteria were established to consider factors such as participants’ dissatisfaction with any stage of the research implementation.
Study procedure
In this study, a therapeutic program was implemented to strengthen the pelvic floor muscles in participants. The program consisted of three specific exercises: Bird dog, plank and leg lift. The exercises were conducted in sets of 10 repetitions, alternating between exercises, and were done three times a day. Participants were instructed to perform one session in the clinic and two sessions at home, totaling 3 days per week for 8 weeks. A table was provided in a booklet for patients to record their exercise sessions. These exercises were supervised by occupational therapists and conducted through telephone follow-ups. It is important to note that no other interventions, such as medication therapy, physiotherapy, or occupational therapy, were implemented. Participants were encouraged to continue their routine treatment alongside the pelvic floor exercises.
Study outcomes
International consultation on incontinence questionnaire-urinary incontinence short form (ICIQ-UI SF)
Avery et al. developed this research tool for this study. It evaluates various aspects of urinary incontinence, such as frequency, amount of leakage, impact on QoL and duration. The total score is derived by summing scores from questions pertaining to frequency, leakage amount, and impact on QoL. The scale encompasses 0 to 21 variables. The final question addresses the type of incontinence but is not assigned a numerical score. Greater scores signify increased severity of incontinence [16]. Hajebrahimi et al. translated this questionnaire into multiple languages and validated it in Iran [17].
Fatigue severity scale (FSS)
This questionnaire measures the severity of excessive fatigue in daily functioning. It includes 9 questions rated on a scale of 1 to 7. The questionnaire is highly reliable in assessing fatigue severity in patients with MS [18]. It provides a comprehensive evaluation of fatigue, with the score directly reflecting the level and intensity of fatigue experienced by the patient. The Persian version of the questionnaire has been validated and confirmed for its validity and reliability by Azimian et al. [19].
Iranian-developed version of the leisure questionnaire for people with MS
This tool has been developed by Hosseini et al. to measure the level of leisure time activity in MS patients. It consists of 50 items that are scored on a Likert scale, ranging from “often,” “sometimes,” “usually,” “rarely,” to “never” [20]. The content validity, convergent validity, and differential validity of this tool have been calculated, and it has been shown to have an acceptable level of validity [21]. In this study, all patients completed questionnaires before and after the treatment program.
Data analysis
The data have been entered into SPSS software, version 23 for activity analysis. For each variable, the data will be compared before and after the exercises using the Wilcoxon test. Additionally, the relationship between variables will be examined using the Spearman correlation test.
Results
The study patients have an Mean±SD age of 8.18±43.83 years. Their expanded disability status scale (EDSS) scores Mean±SD, 1.88±4.25. Furthermore, the duration of diagnosis in months Mean±SD, 73.22±121.33. Comprehensive demographic information about the patients is available in Table 1.
During the research, three individuals could not complete the study (one due to disease relapse and two due to lack of interest in continuing the exercises). Consequently, data from 12 patients were entered into SPSS software, version 23. The analysis revealed a calculated value of <0.05. To examine the impact of pelvic floor exercises on patients’ urinary control and leisure time, the study employed the Wilcoxon statistical test and the resulting findings are presented in Table 2.
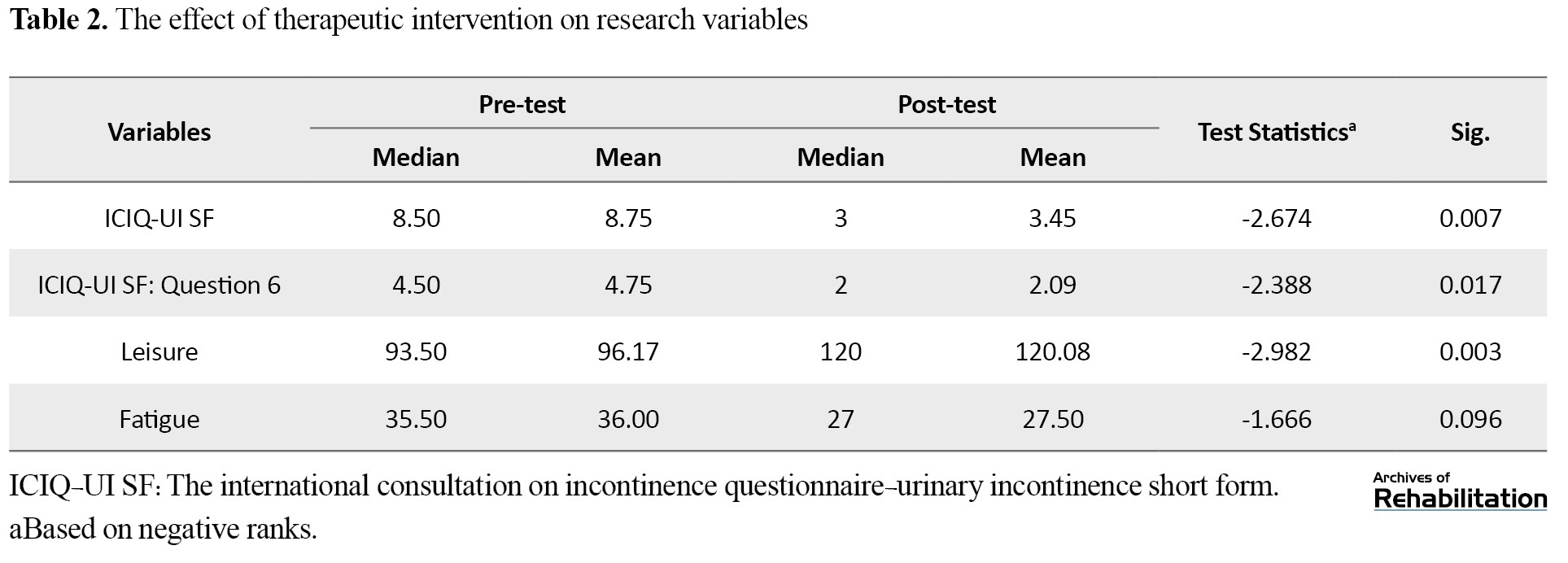
Indeed, as observed in Table 2, pelvic floor exercises effectively improve patients’ urinary control and leisure time. However, their fatigue levels showed no significant impact (P=0.05).
Discussion
This study found that pelvic floor exercises can be beneficial for managing urinary incontinence in women with MS. The results showed a significant improvement in symptoms after implementing a structured exercise program.
This study is significant because it focuses on women with MS, who often face specific challenges in managing urinary symptoms. The positive results indicate that pelvic floor exercises can be an effective non-pharmacological intervention for improving urinary control in this group [22]. The improvements are attributed to the strengthening of pelvic floor muscles, which play a crucial role in maintaining continence [23]. Regular exercise targeting these muscles can increase muscle tone and improve bladder control in women with MS [24].
Multiple studies have investigated the effects of pelvic floor exercises on urinary incontinence in women with MS. Pérez et al. [25] found similar results to the present research, showing a significant reduction in symptoms with a structured exercise program [25]. This alignment strengthens the evidence for the effectiveness of this intervention. Additionally, Lucio et al. [26] demonstrated that combining pelvic floor exercises with a vaginal perineometer had a greater impact on urinary incontinence compared to using the perineometer alone .
Chen et al. [27] further supported the effectiveness of a comprehensive approach combining pelvic floor exercises, bladder training, and lifestyle modifications for improved outcomes in managing urinary incontinence in women with MS.
Existing research backs the beneficial effects of pelvic floor exercises on urinary incontinence in women with MS. However, it is important to consider variations in study design, exercise protocols, sample sizes and additional interventions that may affect outcomes. This study also explores the effects of pelvic floor exercises on leisure activities in women with MS. Leisure activities are crucial for maintaining a good QoL. Still, MS can present challenges that hinder participation. Understanding the relationship between pelvic floor exercises and leisure activities can contribute to a holistic approach to managing MS. The study found a positive association between pelvic floor exercises and improvements in leisure activities among women with MS. Regular exercise increases participation and enjoyment in social gatherings and hobbies. This outcome may be attributed to improved physical functioning, reduced urinary symptoms, increased confidence, and enhanced ability to engage in recreational activities. Strengthening the pelvic floor muscles through exercise can improve balance, stability, and coordination, facilitating active participation in leisure activities.
Limited research has specifically examined the effects of pelvic floor exercises on leisure activities in women with MS. However, Rafii et al. [28] investigated the impact of physical exercise interventions, including pelvic floor exercises, on QoL in individuals with MS. Although leisure activities were not specifically studied, the research reported significant improvements in overall QoL, including physical and social well-being. These findings indirectly suggest that physical exercise interventions, such as pelvic floor exercises, may also positively influence leisure activities [28]. Additionally, Petajan et al. [29] demonstrated that aerobic exercises can improve bowel and bladder control and leisure time in patients with MS.
Miletta et al. [30] examined the effects of a multidisciplinary management approach, including pelvic floor exercises, on functional outcomes in individuals with MS. The research reported improvements in pelvic floor functioning, which could positively impact the ability to engage in leisure activities. Nevertheless, the study did not directly assess the influence on leisure activities, underscoring the necessity for additional research in this domain. It is crucial to acknowledge the scarcity of targeted studies on the impact of pelvic floor exercises on leisure activities in women with MS. Further research would enhance comprehension of how pelvic floor exercises affect leisure activities. Despite the initial hypothesis, the study did not observe a notable decrease in fatigue levels after pelvic floor exercise interventions. Factors such as the heterogeneity of MS symptoms, individual variations in disease progression, and the duration and intensity of the exercise interventions may have influenced these results. Other factors, such as psychological or lifestyle-related aspects, that were not considered in the study could have also influenced fatigue outcomes.
Only one study identified that specifically investigated the influence of pelvic floor exercises on fatigue levels in individuals with MS. This study, conducted by Ghafari and colleagues [31], illustrated a positive impact of pelvic floor exercises on fatigue in patients with urinary incontinence. The discrepancy in results between the provided treatment protocol and Ghafari’s study may account for the observed differences. A review of existing studies indicates the necessity for further research to comprehensively grasp the impact of pelvic floor exercises on fatigue in women with MS.
One limitation of this study is the inability to reach the desired number of participants in the study group and the inability to sample randomly, mainly due to limited access to the target population at research centers and inclusion and exclusion criteria. It is suggested that further research be conducted to determine appropriate exercise protocols, duration, and frequency for achieving the best results in women with MS. Furthermore, it is recommended that these exercises be included in the therapeutic program for patients.
Conclusion
Although this study offers evidence on how pelvic floor exercises can help decrease urinary incontinence and improve leisure activities in women with MS, caution should be exercised in generalizing the results due to the limited number of participants. Additionally, researching the long-term effects and sustainability of the intervention would offer valuable insights for healthcare professionals and patients, enhancing our understanding of the enduring benefits of pelvic floor exercises.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Hamadan University of Medical Sciences (Code: IR.UMSHA.REC.1399.080) and also approved by Iranian Registry of Clinical Trials (IRCT) (Code:IRCT20200509047370N1).
Funding
This study was supported by the Research Deputy of Hamadan University of Medical Sciences (Grand No.: 9909256560).
Authors' contributions
Conceptualization: Seyed Mohammad Sadegh Hosseini and Sahar Nurani Gharaborghe; Research and review: All authors; Review, editing and final approval: Seyed Mohammad Sadegh Hosseini and Sahar Nurani Gharaborghe.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers wish to extend their appreciation to the patients who took part in this study.
Refrences
- Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mörk S, Bö L. Axonal transection in the lesions of multiple sclerosis. New England Journal of Medicine. 1998; 338(5):278-85. [DOI:10.1056/NEJM199801293380502] [PMID]
- Radomski MV, Trombly CA. Occupational therapy for physical dysfunction. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2008. [Link]
- Amarenco G, de Sèze M, Ruffion A, Sheikh Ismael S. Clinical and urodynamic evaluations of urinary disorders in multiple sclerosis. Annals of Physical and Rehabilitation Medicine. 2014; 57(5):277-87. [DOI:10.1016/j.rehab.2014.05.006] [PMID]
- Karapolat H, EYİGÖR S, Akkoc Y, Yesil H, Sagduyu A. [Quality of life in multiple sclerosis patients with urinary disorders: reliability and validity of the Turkish version of Qualiveen (Turkish)]. Journal of Neurological Sciences. 2010; 27(1):043-9
- Lebre AT, Mendes MF, Tilbery CP, Almeida AL, Scatolini Neto A. [Relation between fatigue and autonomic disturbances in multiple sclerosis (Portuguese)]. Arquivos de Neuro-Psiquiatria. 2007; 65(3A):663-8. [PMID]
- Corcos J. A urological challenge: Voiding dysfunction in multiple sclerosis. Canadian Urological Association Journal. 2013; 7(9-10 Suppl 4):S181-2. [DOI:10.5489/cuaj.1618] [PMID]
- Agahi N. Leisure in late life: Patterns of participation and relationship with health [PhD dissertation]. Stockholm: Karolinska Institute; 2008. [Link]
- Bier N, Dutil E, Couture M. Factors affecting leisure participation after a traumatic brain injury: An exploratory study. The Journal of Head Trauma Rehabilitation. 2009; 24(3):187-94. [DOI:10.1097/HTR.0b013e3181a0b15a] [PMID]
- Law M. Participation in the occupations of everyday life. The American Journal of Occupational Therapy. 2002; 56(6):640-9. [DOI:10.5014/ajot.56.6.640] [PMID]
- Fisk JD, Pontefract A, Ritvo PG, Archibald CJ, Murray T. The impact of fatigue on patients with multiple sclerosis. Canadian Journal of Neurological Sciences. 1994; 21(1):9-14. [DOI:10.1017/S0317167100048691]
- Kos D, Kerckhofs E, Nagels G, D’hooghe M, Ilsbroukx S. Origin of fatigue in multiple sclerosis: Review of the literature. Neurorehabilitation and Neural Repair. 2008; 22(1):91-100. [DOI:10.1177/1545968306298934] [PMID]
- Fiest KM, Fisk JD, Patten SB, Tremlett H, Wolfson C, Warren S, et al. Fatigue and comorbidities in multiple sclerosis. International Journal of MS Care. 2016; 18(2):96-104. [DOI:10.7224/1537-2073.2015-070] [PMID]
- Rafii F, Shareinia H, Seyedalshohahadaee M, Sarraf P, Mahmoodi F. [The effect of pelvic floor muscle exercise training on urinary incontinence in patients with multiple sclerosis (Persian)]. Iran Journal of Nursing. 2014; 27(87):43-54. [DOI:10.29252/ijn.27.87.43]
- Lúcio AC, Campos RM, Perissinotto MC, Miyaoka R, Damasceno BP, D’ancona CAL. Pelvic floor muscle training in the treatment of lower urinary tract dysfunction in women with multiple sclerosis. Neurourology and Urodynamics. 2010; 29(8):1410-3. [DOI:10.1002/nau.20941] [PMID]
- Siff LN, Hill AJ, Walters SJ, Walters G, Walters MD. The effect of commonly performed exercises on the levator hiatus area and the length and strength of pelvic floor muscles in postpartum women. Female Pelvic Medicine & Reconstructive Surgery. 2020; 26(1):61-6. [DOI:10.1097/SPV.0000000000000590] [PMID]
- Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourology and Urodynamics: Official Journal of the International Continence Society. 2004; 23(4):322-30. [DOI:10.1002/nau.20041] [PMID]
- Hajebrahimi S, Nourizadeh D, Hamedani R, Pezeshki MZ. Validity and reliability of the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form and its correlation with urodynamic findings. Urology Journal. 2012; 9(4):685-90. [PMID]
- Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, et al. Development of a fatigue scale. Journal of Psychosomatic Research. 1993; 37(2):147-53. [DOI:10.1016/0022-3999(93)90081-P] [PMID]
- Azimian M, Farahani AS, Dadkhah A, Fallahpour M, Karimlu M. Fatigue Severity Scale: The Psychometric Properties of the Persian-Version in Patients with Multiple Sclerosis. Research Journal of Biological Sciences. 2009; 4(9):974-7. [Link]
- Hosseini SMS, Nurani Gharaborghe S, Asgari A. Leisure Questionnaire of people with multiple sclerosis. Journal of Rehabilitation Sciences & Research. 2023; 10(2):70-4. [DOI:10.30476/jrsr.2022.93525.1239]
- Hosseini SMS, Nurani Gharaborghe S. Validity and Reliability of Leisure Questionnaire of People with Multiple Sclerosis: Psychometric properties. Current Journal of Neurology. 2024; 23(1):15-20.
- Kajbafvala M, Ashnagar Z, Lucio A, Firoozeh F, Salehi R, Pashazadeh F, et al. Pelvic floor muscle training in multiple sclerosis patients with lower urinary tract dysfunction: A systematic review and meta-analysis. Multiple Sclerosis and Related Disorders. 2022; 59:103559. [DOI:10.1016/j.msard.2022.103559] [PMID]
- Fan HL, Chan SS, Law TS, Cheung RY, Chung TK. Pelvic floor muscle training improves quality of life of women with urinary incontinence: A prospective study. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2013; 53(3):298-304. [DOI:10.1111/ajo.12075] [PMID]
- Lúcio A, Dancona CA, Perissinotto MC, McLean L, Damasceno BP, de Moraes Lopes MH. Pelvic floor muscle training with and without electrical stimulation in the treatment of lower urinary tract symptoms in women with multiple sclerosis. Journal of Wound Ostomy & Continence Nursing. 2016; 43(4):414-9. [DOI:10.1097/WON.0000000000000223] [PMID]
- Pérez DC, Chao CW, Jiménez LL, Fernández IM, de la Llave Rincón AI. Pelvic floor muscle training adapted for urinary incontinence in multiple sclerosis: A randomized clinical trial. International Urogynecology Journal. 2020; 31(2):267-75. [DOI:10.1007/s00192-019-03993-y] [PMID]
- Lúcio AC, Perissinoto MC, Natalin RA, Prudente A, Damasceno BP, D'ancona CA. A comparative study of pelvic floor muscle training in women with multiple sclerosis: Its impact on lower urinary tract symptoms and quality of life. Clinics. 2011; 66(9):1563-8. [DOI:10.1590/S1807-59322011000900010] [PMID]
- Chen S, Wang S, Liu S, Wang S, Xuan L, Gao Y. Efficacy of electrical pudendal nerve stimulation versus pelvic floor muscle training in treating postradical prostatectomy urinary incontinence: Study protocol for a randomised controlled trial. BMJ Open. 2023; 13(1):e062323. [DOI:10.1136/bmjopen-2022-062323] [PMID]
- Rafii F, Sajjadi M, Shareinia H, Sarraf P, Seyedalshohahadaee M. Effects of pelvic floor muscle exercises on urinary incontinence and quality of life in patients with multiple sclerosis. Middle East Journal of Family Medicine. 2018; 16(1):62-5. [DOI:10.5742/MEWFM.2018.93199]
- Petajan JH, Gappmaier E, White AT, Spencer MK, Mino L, Hicks RW. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Annals of Neurology. 1996; 39(4):432-41. [DOI:10.1002/ana.410390405] [PMID]
- Miletta M, Bogliatto F, Bacchio L. Multidisciplinary management of sexual dysfunction, perineal pain, and elimination dysfunction in a woman with multiple sclerosis. International Journal of MS Care. 2017; 19(1):25-8. [DOI:10.7224/1537-2073.2015-082] [PMID]
- Ghafari Z, Noorizadeh Dehkordi S, Nikjooy A, Mousavi Khatir SR, Moghaddasi M. The effect of pelvic floor muscle exercises therapy on the fatigue and quality of life in multiple sclerosis women with urinary disorders. Function and Disability Journal. 2022; 5(1):65. [DOI:10.32598/fdj.5.65]
Type of Study: Original |
Subject:
Occupational Therapy
Received: 28/11/2023 | Accepted: 28/03/2024 | Published: 1/10/2024
Received: 28/11/2023 | Accepted: 28/03/2024 | Published: 1/10/2024
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |