Volume 25, Issue 3 (Autumn 2024)
jrehab 2024, 25(3): 520-539 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Banan Khojasteh M, Khalkhali Zavieh M, Kalantari K K, Akbarzadeh Baghban A, Daryabor A, Mikaili S. Effect of Biofeedback Training of Hip Muscles on Pain, Muscle Strength and Their Electromyography in Patellofemoral Pain Syndrome. jrehab 2024; 25 (3) :520-539
URL: http://rehabilitationj.uswr.ac.ir/article-1-3388-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3388-en.html
Mehdi Banan Khojasteh1 

 , Minoo Khalkhali Zavieh *2
, Minoo Khalkhali Zavieh *2 

 , Khosro Khademi Kalantari3
, Khosro Khademi Kalantari3 

 , Alireza Akbarzadeh Baghban4
, Alireza Akbarzadeh Baghban4 

 , Aliyeh Daryabor5
, Aliyeh Daryabor5 

 , Saeed Mikaili3
, Saeed Mikaili3 




 , Minoo Khalkhali Zavieh *2
, Minoo Khalkhali Zavieh *2 

 , Khosro Khademi Kalantari3
, Khosro Khademi Kalantari3 

 , Alireza Akbarzadeh Baghban4
, Alireza Akbarzadeh Baghban4 

 , Aliyeh Daryabor5
, Aliyeh Daryabor5 

 , Saeed Mikaili3
, Saeed Mikaili3 


1- Department of Physiotherapy, Student Research Committee, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,minoo_kh@yahoo.com
3- Department of Physiotherapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Biostatistics, Proteomics Research Center, School of Paramedicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
5- Department of Orthotics and Prosthetics, Physiotherapy Research Center, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,
3- Department of Physiotherapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Biostatistics, Proteomics Research Center, School of Paramedicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
5- Department of Orthotics and Prosthetics, Physiotherapy Research Center, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Keywords: Biofeedback, Patellofemoral pain syndrome (PFPS), Strength, Electromyography (EMG), Hip abductor muscles, Hip external rotator muscles
Full-Text [PDF 2060 kb]
(1039 Downloads)
| Abstract (HTML) (7007 Views)
Full-Text: (1246 Views)
Introduction
Patellofemoral pain syndrome (PFPS) stands as one of the most common causes of front knee pain, and 25% of the population suffers from this disorder. It is more common in young women [1, 2]. Recent research has shown that PFPS is not necessarily caused by weakness or impaired motor control in the vastus medialis oblique muscle or improper patellar position but may be caused by weakness or movement impairment control of the proximal muscles [3, 4]. Excessive adduction of the hip when rising from a sitting position increases knee valgus, and following excessive internal rotation in a standing position, abnormal pressure is applied to the knee [5]. This bone disorder causes weakness of the hip external rotator muscles like the gluteus maximus, causing reduced strength and torque in the external rotator and hip abductor muscles of people with PFPS compared to healthy individuals [6]. In individuals suffering from PFPS compared to healthy ones during most activities, the activity level of the hip external rotator and abductor muscles is not different. However, the peak contraction of hip adductors during running and squatting is higher than that in healthy people. The hip external rotator and abductor muscles are also weaker than normal, although it is not known whether the weakness of these muscles is the cause or result of PFPS [7].
Following the PFPS, treatment goals are to maintain and promote knee joint stability, achieve optimal range of motion, strengthen knee muscles and gain normal neuromuscular control [8]. A wide range of common treatments are used for these patients, including pulse electromagnetic fields, home exercises, hip strengthening exercises, stretching exercises, stabilization exercises, aerobic exercises, neuromuscular facilitation through proprioception, and bracing use. Still, no single treatment in these patients is superior to other treatments [9]. However, a systematic study has shown that a combination of physiotherapy treatments, including strengthening the hip and knee muscles, and passive therapies, such as stretching exercises and braces, may be more effective in treating these people [10]. Systematic studies have indicated that strengthening the hip muscles could decrease pain and improve function in these individuals [11, 12]. Also, strengthening hip abductors exercises reduce pain more than quadriceps strengthening exercises. On the other hand, it has been shown that straight leg raising with ankle dorsiflexion and lateral hip rotation can improve function because of more vastus medialis oblique muscle recruitment in these patients [13]. However, limited evidence has shown the superiority of multi-articular strengthening therapy over single-joint strengthening programs in these patients [14].
Biofeedback is used to retrain normal movement patterns following an injury [8]. Electromyography (EMG) biofeedback is an approach to retraining muscle by creating a new feedback system resulting from the conversion of myoelectric signals of a muscle into auditory and visual ones [15]. This feedback can cause changes in neuromuscular control and allow the person to attain the desired muscle contraction target [16]. EMG biofeedback is often used with routine rehabilitation approaches to improve balance, proprioception and strength [17] through modulating muscle activation, improving neuromuscular control and increasing patients’ acceptance of treatment [18].
Since weakness or motor control impairment of the hip external rotator and abductor muscles can be one of the causes of PFPS [19], strengthening hip abductor muscles can improve function and reduce pain in these patients [11, 20, 21]. However, the influence of motor control exercises on these muscles during functional activities, along with using EMG feedback on pain and EMG findings of hip muscles, is not clear. In addition, no published studies have been available comparing the effect of biofeedback training with routine physiotherapy exercises in people with PFPS. Therefore, this research was conducted to evaluate the influence of routine and routine exercises and motor control exercises of EMG biofeedback of hip external rotator and abductor muscles on pain, strength, and EMG activity of these muscles in individuals with PFPS.
Materials and Methods
Study participants
Thirty people with PFPS (11 males and 19 females) aged 22 to 45 years were selected by simple non-probability sampling and allocated to the intervention and control groups. The inclusion criteria were as follows: Anterior/posterior patellar pain for at least two months [22, 23], aggravation of symptoms during stair climbing, prolonged sitting, kneeling, running, squatting and jumping [24], positive Clark’s and apprehension tests [25], and pain during active knee extension with resistance. The presence of dislocation and direct trauma to the patella, any rheumatological conditions (osteoarthritis or rheumatoid arthritis), diabetes, meniscus injury and instability of knee ligaments were exclusion criteria [22, 24].
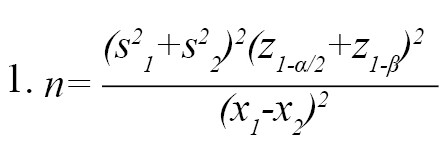
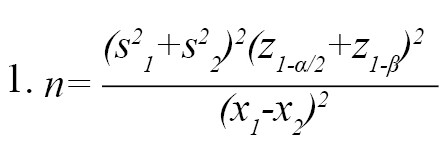
A previous study determined the sample size using the NCSS software, version 24.0.3 [26] based on the kinematics data. In this way, regarding d=2, α=0.05, and -β=0.80, the sample size was determined to be 15 in each group (Equation 1):
Study design
All participants signed the informed consent form after the Ethics Committee approved the study. After assessing the inclusion and exclusion criteria, the participants attended an initial meeting to be familiarized with the study procedure and complete the demographic survey questionnaire. In the present study, the study’s dependent variables were measured before and 8 weeks after the interventions. Dependent variables included pain measured by visual analog scale (VAS), EMG variables of hip external rotator and abductor muscles and maximum voluntary isometric contraction (MVIC) of these muscles assessed by a dynamometer (ICC>0.7) [27]. Then, the patients were randomly allocated to one of these groups by selecting one of the two envelopes written in the name of the intervention or treatment groups. The person who evaluated the samples was unaware of the subjects’ grouping for blinding. The therapist had no knowledge of the evaluation results three times before and after eight weeks of interventions.
Study tools
To measure the MVIC of muscles, the ZEMIC dynamometer model H3-C3/C4-100KG-3B was used with 10-g accuracy, which its reliability and validity had been confirmed in a previous study [28]. To assess the hip abductors, participants were placed in a position mentioned by Nakagawa et al. [29] in the lateral decubitus position (side lying) and the neutral position supported by pillows so that the dominant lower limb was upward. An adjustable non-elastic band was placed around the examination table and in the proximal iliac crest to stabilize the pelvis and individuals pushed their leg into a dynamometer placed with the examiner’s hand on the lateral condyle of the femur. The examiner asked patients to move their feet upwards with maximum effort [30]. To measure the MVIC of the hip external rotator muscles, the person sat on the edge of the bed with the thigh angle at 90 degrees flexion while holding the sides of the bed with both hands. Resistance was exerted at 5 cm close to the proximal edge of the medial malleoli against lateral pelvic rotation. The person was asked to push with maximum effort to the dynamometer in the examiner’s hand [30]. Patients were given verbal encouragement for maximum effort during the test. The mean value of three measurements with a dynamometer with an interval of 30 s was recorded as the maximum isometric contraction force of muscles. Dynamometric results of all experiments (kg) were converted to newton and normalized to body weight.
An 8-channel Megawin device was used to measure the EMG activity. Raw EMG signals with a bandwidth of 10-500 Hz were filtered. Before the test, three trials below the maximum and one maximum test were performed to familiarize the individuals. In the evaluation by dynamometer, the maximum isometric contraction force of muscle (kg) was recorded. To assess muscle EMG, the area under the EMG curve (integrated EMG) and the onset of muscle activity (the moment of onset of the EMG wave) were recorded within 5 s. To measure the integrated EMG, the total magnitude of rectilinear EMG signals was calculated from the onset to the end of the activity. To analyze EMG signals, root mean square (RMS) was calculated, and then using Mean+2SD from the recorded background signal range, the onset and offset of the muscle electrical activity were calculated. In other words, when the EMG signal exceeded the calculated threshold value of the background signal and remained higher for 25 ms, it was determined as the onset. When the EMG signal was less than the threshold limit and remained in this state for 25 ms, it was determined as the offset of electrical activity. In the EMG-RMS signal, the maximum amplitude value of the electrical activity wave was calculated and recorded from the start to the end of the electrical activity. There was a 2 minute break between each test. Regarding the statistical analysis, the mean value of 3 replications was considered, which showed an average variability of <10%. When there was a difference of >10% between trials, a fourth trial was conducted. (Equation 2 and 3)
2. (Power[N]=Power [kg]×9.81)
3. (Normalized power [N/kg]=Power [N]/Body weight [kg])
According to the surface EMG for the non-invasive assessment of muscles (SENIAM) protocol, EMG electrodes were installed for the hip external rotator muscle in the middle of the line between the sacral vertebrae and the greater trochanter and the hip abductor, in the middle of the line that connects the iliac crest to the greater trochanter, in the direction of muscle fibers. A distance of 20 mm between the electrodes and the reference electrode was placed on the spine.
Study procedure
The routine physiotherapy treatment for knee disorders [33] was administrated in the control group. This treatment included electrotherapy (including 30 minutes of conventional TENS at a 100 Hz frequency and a 50 ms duration around the knee). Patients also performed isometric exercises on gluteal and quadriceps muscles 100 times per session, along with stretching of quadriceps, iliotibial band, hamstring, hip adductor and cuff muscles. For stretching exercises in this group, active muscle stretching was performed for 30 s and 3 repetitions for each muscle under the therapist’s supervision by patients. Treatment was carried out for 8 weeks, 3 sessions per week.
In addition to routine treatments in the intervention group, functional training was performed to contract external rotator and hip abductor muscles to control the correct alignment of the femur bone and, consequently, correct knee alignment at initiation gait and descending stairs. Patients were trained to contract the external rotator and hip abductor muscles to control the femoral alignment and consequently correct knee alignment at initiation gait and in the functional activity of descending stairs. To get a basic understanding of how to do the exercise, the therapist first performed the exercises to teach the patients. After the primary functional training, the patients were asked to contract stiffer these muscles at the initial phase of walking and also when relying on an extremity during the step descending, using visual biofeedback resulting from observation of gluteal muscle EMG signals (shown to the patient by a monitor in front of the subject). Each session of motor control training using EMG biofeedback was performed for 30 minutes (including two 15 minute periods with a rest interval of 3 minutes). At least 45 contractions were taken at each training stage.
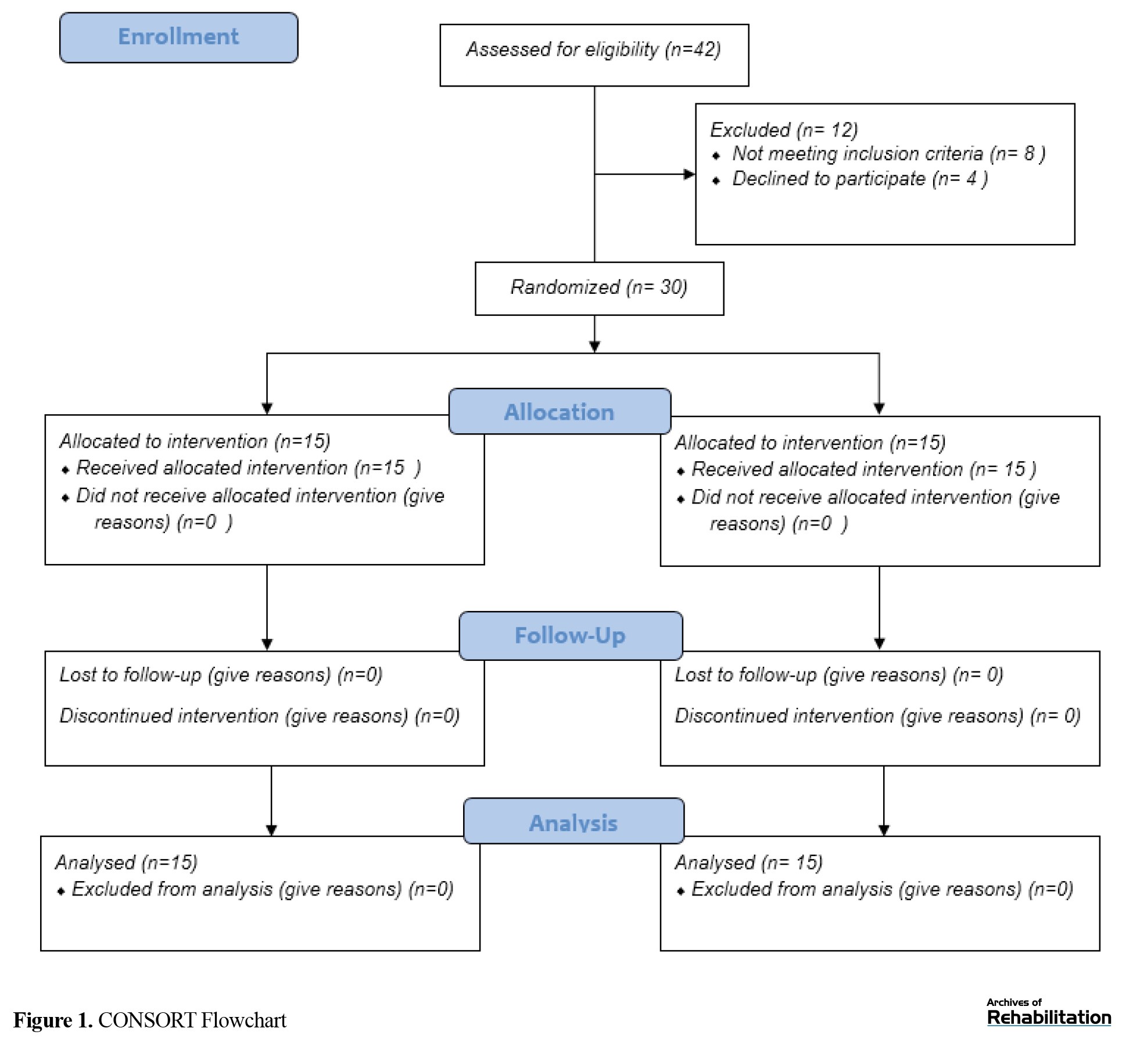
Before the main study, the reliability and validity of measurement of EMG data of hip abductor and external rotator muscles by Megawin device and MVIC of these muscles by ZEMIC dynamometer were conducted on ten subjects twice with three days intervals. The values obtained were ICC=0.66-0.65 for EMG and ICC=0.66-0.72 for dynamometer. The study steps are seen in the CONSORT flowchart (Figure 1).
Statistical analysis
For the statistical analysis, the SPSS software, version 26 was utilized. The data normality was checked using the Shapiro-Wilk test. The outcomes were presented as Mean±SD. As the data distribution was normal, the independent samples t-test was performed to compare the intergroup data, and the paired samples t-test was utilized for intragroup comparison. A P≤0.05 was considered statistically significant.
Results
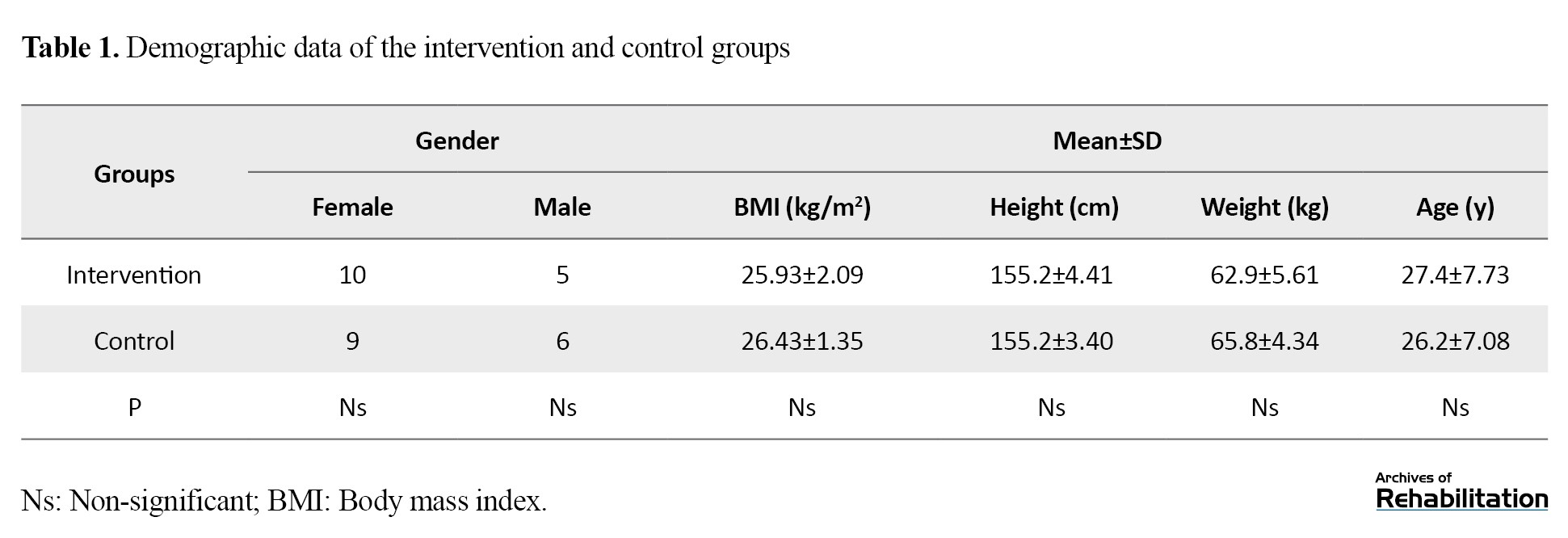
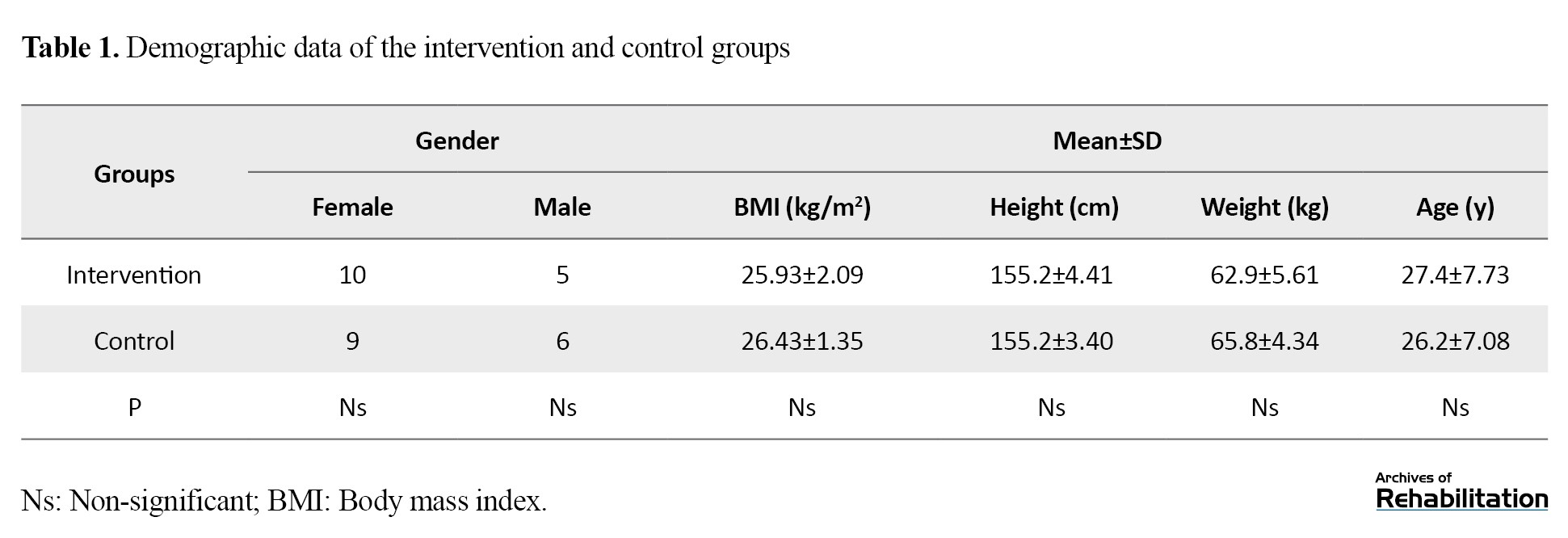
All eligible participants completed the study and were finally analyzed (Figure 1). Table 1 presents the Mean±SD of demographic data, including gender, body mass index, height, weight, and age, indicating no significant difference between the two groups (P˃0.05).
Also, no significant difference was found between the two groups for all MVIC and EMG variables in the pre-intervention conditions (P˃0.05).
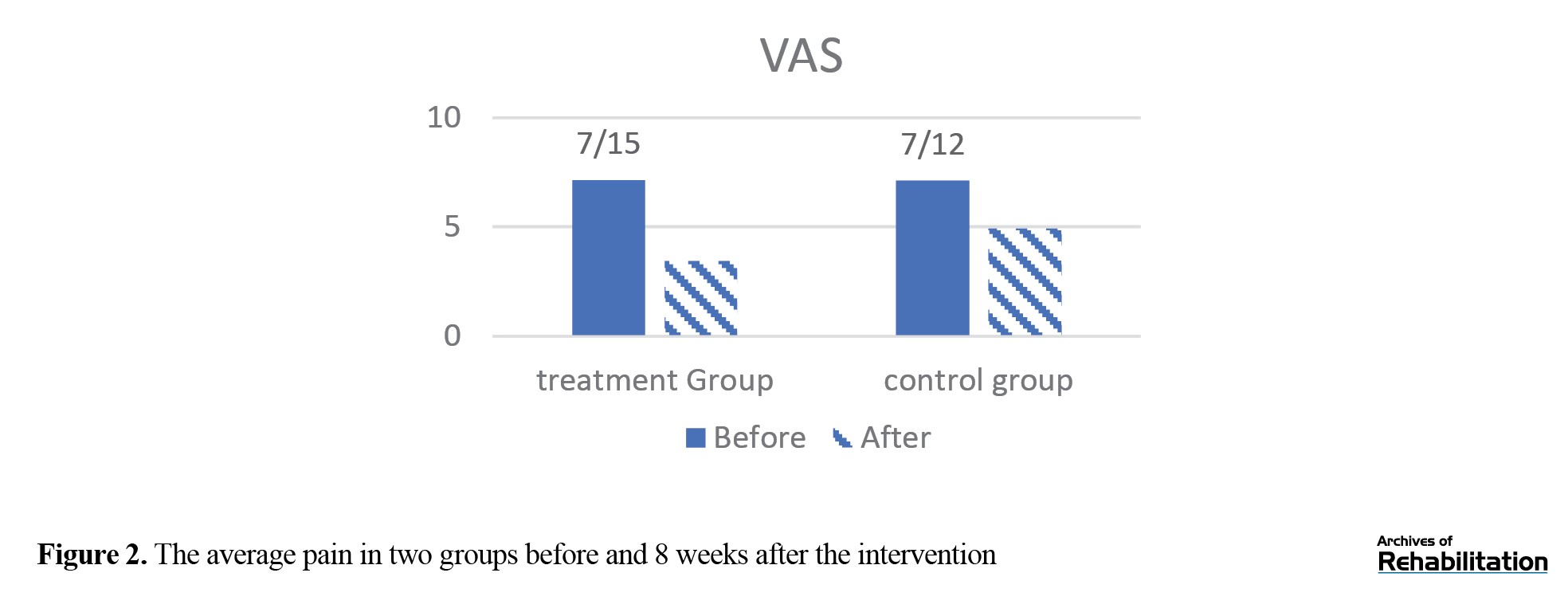
Regarding the comparison of pain between baseline assessment and 8 weeks after intervention, a significant improvement was observed in the intervention group (P=0.001) but not in the control group (P=0.146) (Figure 2). Additionally, an independent t-test for intergroup comparison after treatment showed that pain score was significantly reduced in the intervention group compared to the control group (P=0.016).
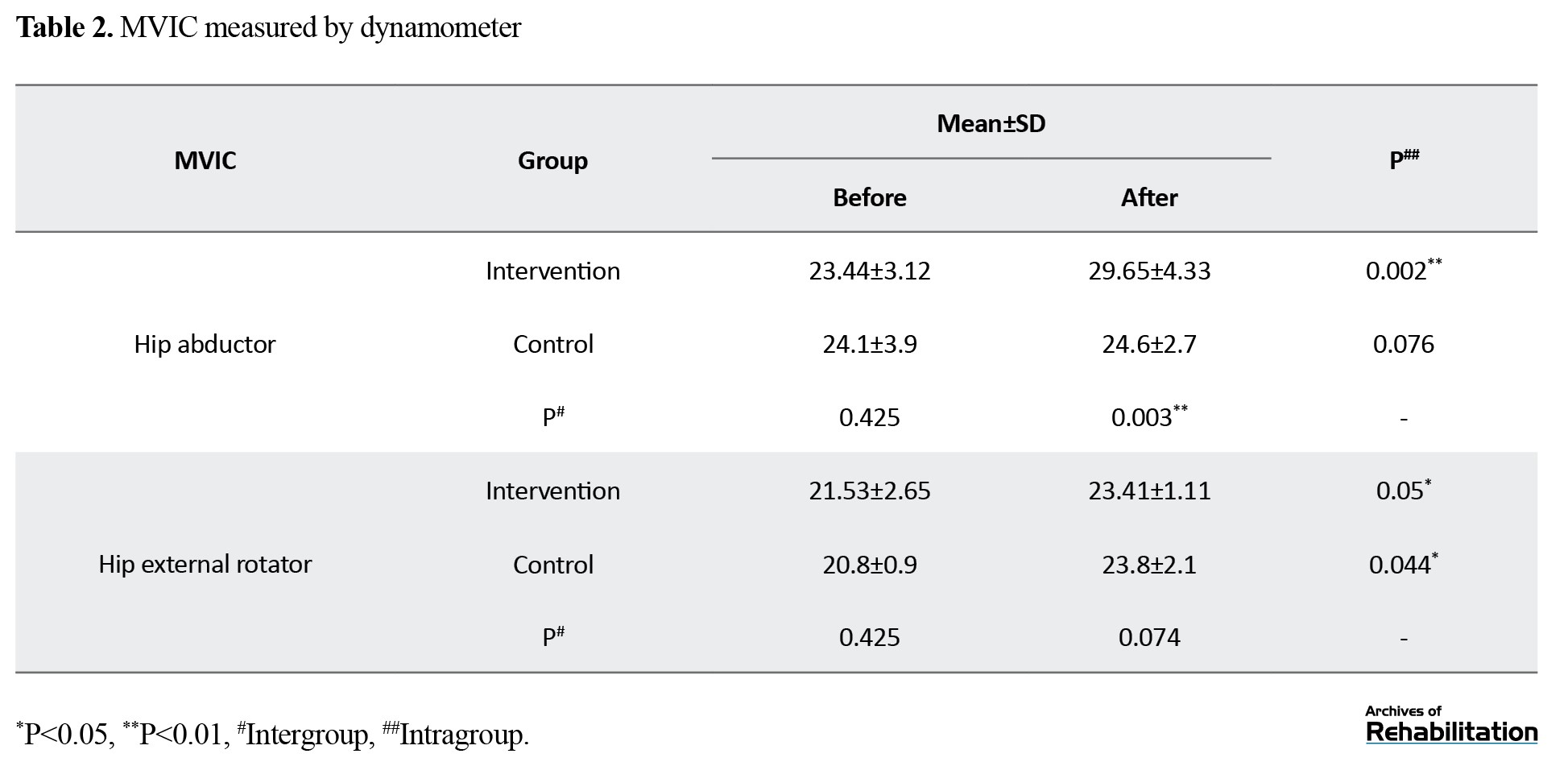
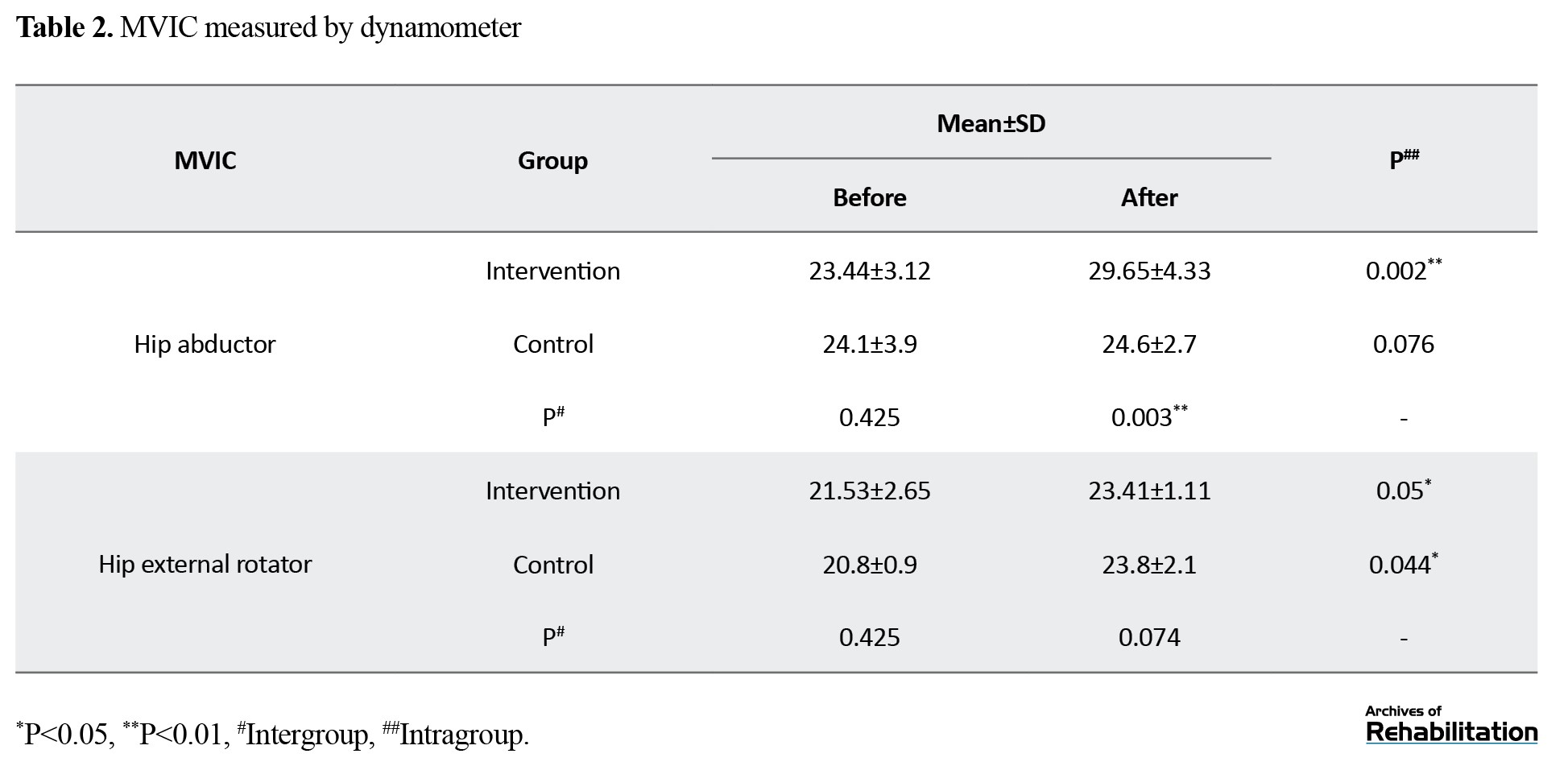
Regarding the intragroup comparison, the hip abductor MVIC significantly increased in the intervention group after 8 weeks of treatment compared to the pre-intervention stage (P=0.012). Still, the control group did not show a significant difference. On the other hand, the external rotator MVIC was significantly increased in the control (P=0.044) and intervention (P=0.05) groups compared to the pre-intervention. Also, the intergroup results showed that MVIC of hip abductor muscle in the intervention group had a significant increase in the intervention group compared with the control group, with no significant statistical change between the two groups for hip external rotator muscle (Table 2).
Based on the findings of EMG of the hip abductor muscle, the intragroup comparison showed that the maximum contraction of this muscle in the intervention and control groups was significantly improved after 8 weeks of treatment compared to pre-treatment. The results of the intergroup comparison showed that the maximum contraction after 8 weeks in the intervention group was significantly increased compared to the control group. The integrated EMG of this muscle was increased significantly only in the control group compared to the pre-treatment condition, but not for the intervention group. The intergroup comparison findings demonstrated that the hip abductor’s integrated EMG after 8 weeks in the control group was significantly higher than the intervention group. No significant change was found in the onset of this muscle for intra- and inter-group comparisons (Table 3).
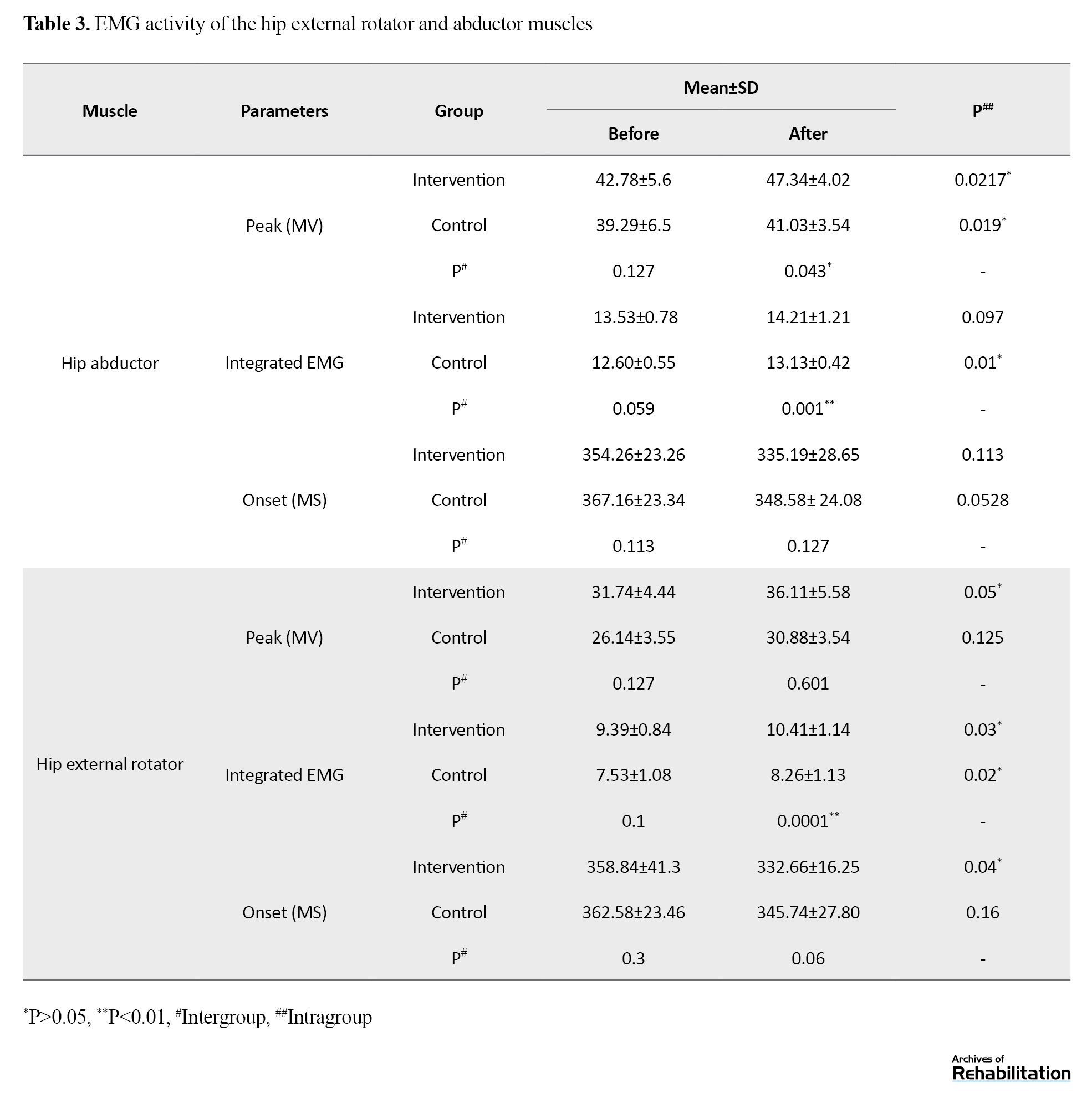
Regarding the results of EMG of the hip external rotator muscle, the maximum contraction of the control group was significantly increased following the intervention, but not for the control group. Maximum hip external rotator muscle contraction showed no change between the two groups following 8-week treatment. An intragroup comparison of the integrated EMG of this muscle showed that this parameter significantly improved in both the intervention and control groups after the 8-week treatment. The intergroup comparison results demonstrated that the integrated EMG after 8 weeks in the intervention group was significantly higher compared to the control group. The onset of muscle activity in the intervention group after 8 weeks of intervention was reduced considerably, but there was no significant change in the control group. Also, a significant change was found in intergroup comparison (Table 3).
Discussion
This research investigated the influence of EMG biofeedback training of the hip external rotator and abductor muscles on pain and muscle EMG activity in PFPS. The results of MVIC and EMG of hip abduction muscles indicated that following 8 weeks of intervention, the biofeedback group showed higher maximum EMG and MVIC activity than the control group. Therefore, hip abductor muscle biofeedback training in PFPS patients could increase the EMG activity of hip abductor muscles more than routine treatment. EMG biofeedback seems to have caused this phenomenon by facilitating treatment acceptance by patients, modulating muscle activation, and improving neuromuscular control [18]. EMG biofeedback is a method by which a person tries to activate and control muscles consciously. Research has shown that using this biofeedback in knee muscles reduces pain in people with knee osteoarthritis and decreases hyperextension in the mid-stance phase in individuals with anterior knee pain [34, 35]. The possible mechanism of these changes due to biofeedback is using more fibers with higher frequency and better cooperation between motor units of muscle that can increase the rate of contraction and muscle tension [24].
Since weakness or motor control disorder of hip abductor muscles can be one of the causes of PFPS [19], strengthening hip abductor muscles can reduce pain and improve function in patients with PFPS [11, 20, 21]. Heo et al. showed that hip abductor muscle biofeedback training can cause the requirement of this muscle in healthy individuals [36]. Kim et al. also showed that EMG biofeedback could activate quadriceps muscles in people with PFPS [37]. Considering the importance of the EMG activity of hip abductor muscles in PFPS, exercise that can increase the EMG activity of these muscles [38] can help the recovery of these patients. Therefore, according to the results of this study, biofeedback exercises can be used in these patients’ proximal muscle strengthening training programs.
In the present study, MVIC and maximum EMG activity of the hip external rotator muscle had no significant change between the two groups of intervention and control. Although a significant improvement was found in both groups after the intervention, the biofeedback group showed a greater increase than the control group. In other words, biofeedback exercises on this muscle have activated it more. Weakness or motor control impairment of the hip external rotator muscles may be one of the causes of PFPS [19]. Still, the researchers of the present study did not find any published studies that investigated the effect of hip external rotator muscle using biofeedback training in patients with PFPS. However, Govil andNoohu [39] showed that in patients with incomplete spinal cord injury, biofeedback training of the hip external rotator muscle increases the amplitude of the EMG activity of this muscle. Alonazi et al. also reported that four weeks of EMG biofeedback complementary training caused significant improvements in quadriceps muscle strength in young male athletes with PFPS [24]. Therefore, biofeedback training of hip external rotator muscles can activate these muscles in patients with PFPS.
The study’s results indicated that 8-week biofeedback training of proximal hip muscles reduced pain in these patients, while routine treatment in the control group did not significantly reduce pain. After 8 weeks of treatment, the biofeedback group had significantly less pain than the control group. Therefore, based on the present study’s findings, it can be stated that adding biofeedback training by using the proximal hip muscles as opposed to routine treatment has reduced patients’ pain. This finding means that biofeedback exercises help reduce pain in these patients. Our results are consistent with Alba-Martín et al. (in a systematic review) and Bisi-Balogun [37, 38]. They also showed that proximal lower extremity exercises reduce pain in individuals with PFPS. It should be noted that the exercises that they used were not biofeedback training. Our results also align with the study by Letafatkar et al. which showed that biofeedback exercises of the muscles around the knee combined with preparation exercises reduced pain and risk of subsequent injuries [40]. In their study, biofeedback exercises were not performed in the proximal hip area, but they were locally done in the muscles around the knee. Rabelo’s study also found that motor control exercises had no greater effect on pain relief than isolated muscle training, which is inconsistent with the results of the current study and previous studies mentioned [41]. Although the exercises in this study were motor control exercises performed with EMG biofeedback, Rabelo’s study performed these exercises without biofeedback.
In general, it seems that biofeedback training of the proximal hip muscles can increase the muscles’ recruitment and the force of these muscles, which may improve clinical symptoms such as pain in patients with PFPS by correcting the movement pattern and aligning the joints of the lower limbs. Previous research has also reported that the force of the external rotator and hip abductor muscles plays a crucial role in controlling the alignment of dynamic valgus and hip internal rotation. These are mechanical factors underlying the development of PFPS [42]. Strengthening these muscles with progressive strengthening exercises improves patients’ clinical symptoms with PFPS [43]. Still, the performance of these exercises, along with the use of EMG biofeedback, has not been investigated, according to our knowledge. So, the results of the present work demonstrated the impact of these exercises on improving the requirement of these muscles and also pain in these patients. Therefore, the use of these exercises in the treatment of people with PFPS is recommended.
The study was limited by lacking a follow-up period after the treatment. It would be beneficial to assess the long-term impacts of the interventions to understand the differences between the two treatments better. For future studies, it is recommended to compare the effects of biofeedback training on the proximal and local muscles of the knee. Additionally, considering the influence of gender on lower extremity alignment and the incidence of PFPS [44], it is recommended that future studies compare these exercises between men and women.
Conclusion
Adding 8 weeks of biofeedback training on external rotator and hip abductor muscles to routine exercise therapy in PFPS can reduce pain and improve muscle strength and performance. This change could potentially slow down the degenerative process of the patellofemoral joint.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Science (SBMU), Tehran, Iran (Code: SBMU. RETECH. REC.1399.1117). Participants were informed of the study objectives. In addition to obtaining written consent, they were assured that information obtained from them would remain confidential.
Funding
The paper was extracted from the PhD dissertation of Mehdi Banan Khojasteh, approved by the Department of Physiotherapy, School of Rehabilitation, Shahid Beheshti University of Medical Science (SBMU), Tehran, Iran. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Mehdi Banan Khojasteh and Minoo Khalkhali Zavieh; Methodology and analysis: Khosro Khademi Kalantari and Alireza Akbarzadeh Baghban; Research: Mehdi Banan Khojasteh and Saeed Mikailii; rview, editing and final approval: Aliyeh Daryabor; Supervision: Minoo Khalkhali Zavieh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Authors appreciate the Department of Physiotherapy faculty members of the School of Rehabilitation, SBMU, for their support and thank all those who participated in this study.
References
Patellofemoral pain syndrome (PFPS) stands as one of the most common causes of front knee pain, and 25% of the population suffers from this disorder. It is more common in young women [1, 2]. Recent research has shown that PFPS is not necessarily caused by weakness or impaired motor control in the vastus medialis oblique muscle or improper patellar position but may be caused by weakness or movement impairment control of the proximal muscles [3, 4]. Excessive adduction of the hip when rising from a sitting position increases knee valgus, and following excessive internal rotation in a standing position, abnormal pressure is applied to the knee [5]. This bone disorder causes weakness of the hip external rotator muscles like the gluteus maximus, causing reduced strength and torque in the external rotator and hip abductor muscles of people with PFPS compared to healthy individuals [6]. In individuals suffering from PFPS compared to healthy ones during most activities, the activity level of the hip external rotator and abductor muscles is not different. However, the peak contraction of hip adductors during running and squatting is higher than that in healthy people. The hip external rotator and abductor muscles are also weaker than normal, although it is not known whether the weakness of these muscles is the cause or result of PFPS [7].
Following the PFPS, treatment goals are to maintain and promote knee joint stability, achieve optimal range of motion, strengthen knee muscles and gain normal neuromuscular control [8]. A wide range of common treatments are used for these patients, including pulse electromagnetic fields, home exercises, hip strengthening exercises, stretching exercises, stabilization exercises, aerobic exercises, neuromuscular facilitation through proprioception, and bracing use. Still, no single treatment in these patients is superior to other treatments [9]. However, a systematic study has shown that a combination of physiotherapy treatments, including strengthening the hip and knee muscles, and passive therapies, such as stretching exercises and braces, may be more effective in treating these people [10]. Systematic studies have indicated that strengthening the hip muscles could decrease pain and improve function in these individuals [11, 12]. Also, strengthening hip abductors exercises reduce pain more than quadriceps strengthening exercises. On the other hand, it has been shown that straight leg raising with ankle dorsiflexion and lateral hip rotation can improve function because of more vastus medialis oblique muscle recruitment in these patients [13]. However, limited evidence has shown the superiority of multi-articular strengthening therapy over single-joint strengthening programs in these patients [14].
Biofeedback is used to retrain normal movement patterns following an injury [8]. Electromyography (EMG) biofeedback is an approach to retraining muscle by creating a new feedback system resulting from the conversion of myoelectric signals of a muscle into auditory and visual ones [15]. This feedback can cause changes in neuromuscular control and allow the person to attain the desired muscle contraction target [16]. EMG biofeedback is often used with routine rehabilitation approaches to improve balance, proprioception and strength [17] through modulating muscle activation, improving neuromuscular control and increasing patients’ acceptance of treatment [18].
Since weakness or motor control impairment of the hip external rotator and abductor muscles can be one of the causes of PFPS [19], strengthening hip abductor muscles can improve function and reduce pain in these patients [11, 20, 21]. However, the influence of motor control exercises on these muscles during functional activities, along with using EMG feedback on pain and EMG findings of hip muscles, is not clear. In addition, no published studies have been available comparing the effect of biofeedback training with routine physiotherapy exercises in people with PFPS. Therefore, this research was conducted to evaluate the influence of routine and routine exercises and motor control exercises of EMG biofeedback of hip external rotator and abductor muscles on pain, strength, and EMG activity of these muscles in individuals with PFPS.
Materials and Methods
Study participants
Thirty people with PFPS (11 males and 19 females) aged 22 to 45 years were selected by simple non-probability sampling and allocated to the intervention and control groups. The inclusion criteria were as follows: Anterior/posterior patellar pain for at least two months [22, 23], aggravation of symptoms during stair climbing, prolonged sitting, kneeling, running, squatting and jumping [24], positive Clark’s and apprehension tests [25], and pain during active knee extension with resistance. The presence of dislocation and direct trauma to the patella, any rheumatological conditions (osteoarthritis or rheumatoid arthritis), diabetes, meniscus injury and instability of knee ligaments were exclusion criteria [22, 24].
A previous study determined the sample size using the NCSS software, version 24.0.3 [26] based on the kinematics data. In this way, regarding d=2, α=0.05, and -β=0.80, the sample size was determined to be 15 in each group (Equation 1):
Study design
All participants signed the informed consent form after the Ethics Committee approved the study. After assessing the inclusion and exclusion criteria, the participants attended an initial meeting to be familiarized with the study procedure and complete the demographic survey questionnaire. In the present study, the study’s dependent variables were measured before and 8 weeks after the interventions. Dependent variables included pain measured by visual analog scale (VAS), EMG variables of hip external rotator and abductor muscles and maximum voluntary isometric contraction (MVIC) of these muscles assessed by a dynamometer (ICC>0.7) [27]. Then, the patients were randomly allocated to one of these groups by selecting one of the two envelopes written in the name of the intervention or treatment groups. The person who evaluated the samples was unaware of the subjects’ grouping for blinding. The therapist had no knowledge of the evaluation results three times before and after eight weeks of interventions.
Study tools
To measure the MVIC of muscles, the ZEMIC dynamometer model H3-C3/C4-100KG-3B was used with 10-g accuracy, which its reliability and validity had been confirmed in a previous study [28]. To assess the hip abductors, participants were placed in a position mentioned by Nakagawa et al. [29] in the lateral decubitus position (side lying) and the neutral position supported by pillows so that the dominant lower limb was upward. An adjustable non-elastic band was placed around the examination table and in the proximal iliac crest to stabilize the pelvis and individuals pushed their leg into a dynamometer placed with the examiner’s hand on the lateral condyle of the femur. The examiner asked patients to move their feet upwards with maximum effort [30]. To measure the MVIC of the hip external rotator muscles, the person sat on the edge of the bed with the thigh angle at 90 degrees flexion while holding the sides of the bed with both hands. Resistance was exerted at 5 cm close to the proximal edge of the medial malleoli against lateral pelvic rotation. The person was asked to push with maximum effort to the dynamometer in the examiner’s hand [30]. Patients were given verbal encouragement for maximum effort during the test. The mean value of three measurements with a dynamometer with an interval of 30 s was recorded as the maximum isometric contraction force of muscles. Dynamometric results of all experiments (kg) were converted to newton and normalized to body weight.
An 8-channel Megawin device was used to measure the EMG activity. Raw EMG signals with a bandwidth of 10-500 Hz were filtered. Before the test, three trials below the maximum and one maximum test were performed to familiarize the individuals. In the evaluation by dynamometer, the maximum isometric contraction force of muscle (kg) was recorded. To assess muscle EMG, the area under the EMG curve (integrated EMG) and the onset of muscle activity (the moment of onset of the EMG wave) were recorded within 5 s. To measure the integrated EMG, the total magnitude of rectilinear EMG signals was calculated from the onset to the end of the activity. To analyze EMG signals, root mean square (RMS) was calculated, and then using Mean+2SD from the recorded background signal range, the onset and offset of the muscle electrical activity were calculated. In other words, when the EMG signal exceeded the calculated threshold value of the background signal and remained higher for 25 ms, it was determined as the onset. When the EMG signal was less than the threshold limit and remained in this state for 25 ms, it was determined as the offset of electrical activity. In the EMG-RMS signal, the maximum amplitude value of the electrical activity wave was calculated and recorded from the start to the end of the electrical activity. There was a 2 minute break between each test. Regarding the statistical analysis, the mean value of 3 replications was considered, which showed an average variability of <10%. When there was a difference of >10% between trials, a fourth trial was conducted. (Equation 2 and 3)
2. (Power[N]=Power [kg]×9.81)
3. (Normalized power [N/kg]=Power [N]/Body weight [kg])
According to the surface EMG for the non-invasive assessment of muscles (SENIAM) protocol, EMG electrodes were installed for the hip external rotator muscle in the middle of the line between the sacral vertebrae and the greater trochanter and the hip abductor, in the middle of the line that connects the iliac crest to the greater trochanter, in the direction of muscle fibers. A distance of 20 mm between the electrodes and the reference electrode was placed on the spine.
Study procedure
The routine physiotherapy treatment for knee disorders [33] was administrated in the control group. This treatment included electrotherapy (including 30 minutes of conventional TENS at a 100 Hz frequency and a 50 ms duration around the knee). Patients also performed isometric exercises on gluteal and quadriceps muscles 100 times per session, along with stretching of quadriceps, iliotibial band, hamstring, hip adductor and cuff muscles. For stretching exercises in this group, active muscle stretching was performed for 30 s and 3 repetitions for each muscle under the therapist’s supervision by patients. Treatment was carried out for 8 weeks, 3 sessions per week.
In addition to routine treatments in the intervention group, functional training was performed to contract external rotator and hip abductor muscles to control the correct alignment of the femur bone and, consequently, correct knee alignment at initiation gait and descending stairs. Patients were trained to contract the external rotator and hip abductor muscles to control the femoral alignment and consequently correct knee alignment at initiation gait and in the functional activity of descending stairs. To get a basic understanding of how to do the exercise, the therapist first performed the exercises to teach the patients. After the primary functional training, the patients were asked to contract stiffer these muscles at the initial phase of walking and also when relying on an extremity during the step descending, using visual biofeedback resulting from observation of gluteal muscle EMG signals (shown to the patient by a monitor in front of the subject). Each session of motor control training using EMG biofeedback was performed for 30 minutes (including two 15 minute periods with a rest interval of 3 minutes). At least 45 contractions were taken at each training stage.
Before the main study, the reliability and validity of measurement of EMG data of hip abductor and external rotator muscles by Megawin device and MVIC of these muscles by ZEMIC dynamometer were conducted on ten subjects twice with three days intervals. The values obtained were ICC=0.66-0.65 for EMG and ICC=0.66-0.72 for dynamometer. The study steps are seen in the CONSORT flowchart (Figure 1).
Statistical analysis
For the statistical analysis, the SPSS software, version 26 was utilized. The data normality was checked using the Shapiro-Wilk test. The outcomes were presented as Mean±SD. As the data distribution was normal, the independent samples t-test was performed to compare the intergroup data, and the paired samples t-test was utilized for intragroup comparison. A P≤0.05 was considered statistically significant.
Results
All eligible participants completed the study and were finally analyzed (Figure 1). Table 1 presents the Mean±SD of demographic data, including gender, body mass index, height, weight, and age, indicating no significant difference between the two groups (P˃0.05).
Also, no significant difference was found between the two groups for all MVIC and EMG variables in the pre-intervention conditions (P˃0.05).
Regarding the comparison of pain between baseline assessment and 8 weeks after intervention, a significant improvement was observed in the intervention group (P=0.001) but not in the control group (P=0.146) (Figure 2). Additionally, an independent t-test for intergroup comparison after treatment showed that pain score was significantly reduced in the intervention group compared to the control group (P=0.016).
Regarding the intragroup comparison, the hip abductor MVIC significantly increased in the intervention group after 8 weeks of treatment compared to the pre-intervention stage (P=0.012). Still, the control group did not show a significant difference. On the other hand, the external rotator MVIC was significantly increased in the control (P=0.044) and intervention (P=0.05) groups compared to the pre-intervention. Also, the intergroup results showed that MVIC of hip abductor muscle in the intervention group had a significant increase in the intervention group compared with the control group, with no significant statistical change between the two groups for hip external rotator muscle (Table 2).
Based on the findings of EMG of the hip abductor muscle, the intragroup comparison showed that the maximum contraction of this muscle in the intervention and control groups was significantly improved after 8 weeks of treatment compared to pre-treatment. The results of the intergroup comparison showed that the maximum contraction after 8 weeks in the intervention group was significantly increased compared to the control group. The integrated EMG of this muscle was increased significantly only in the control group compared to the pre-treatment condition, but not for the intervention group. The intergroup comparison findings demonstrated that the hip abductor’s integrated EMG after 8 weeks in the control group was significantly higher than the intervention group. No significant change was found in the onset of this muscle for intra- and inter-group comparisons (Table 3).
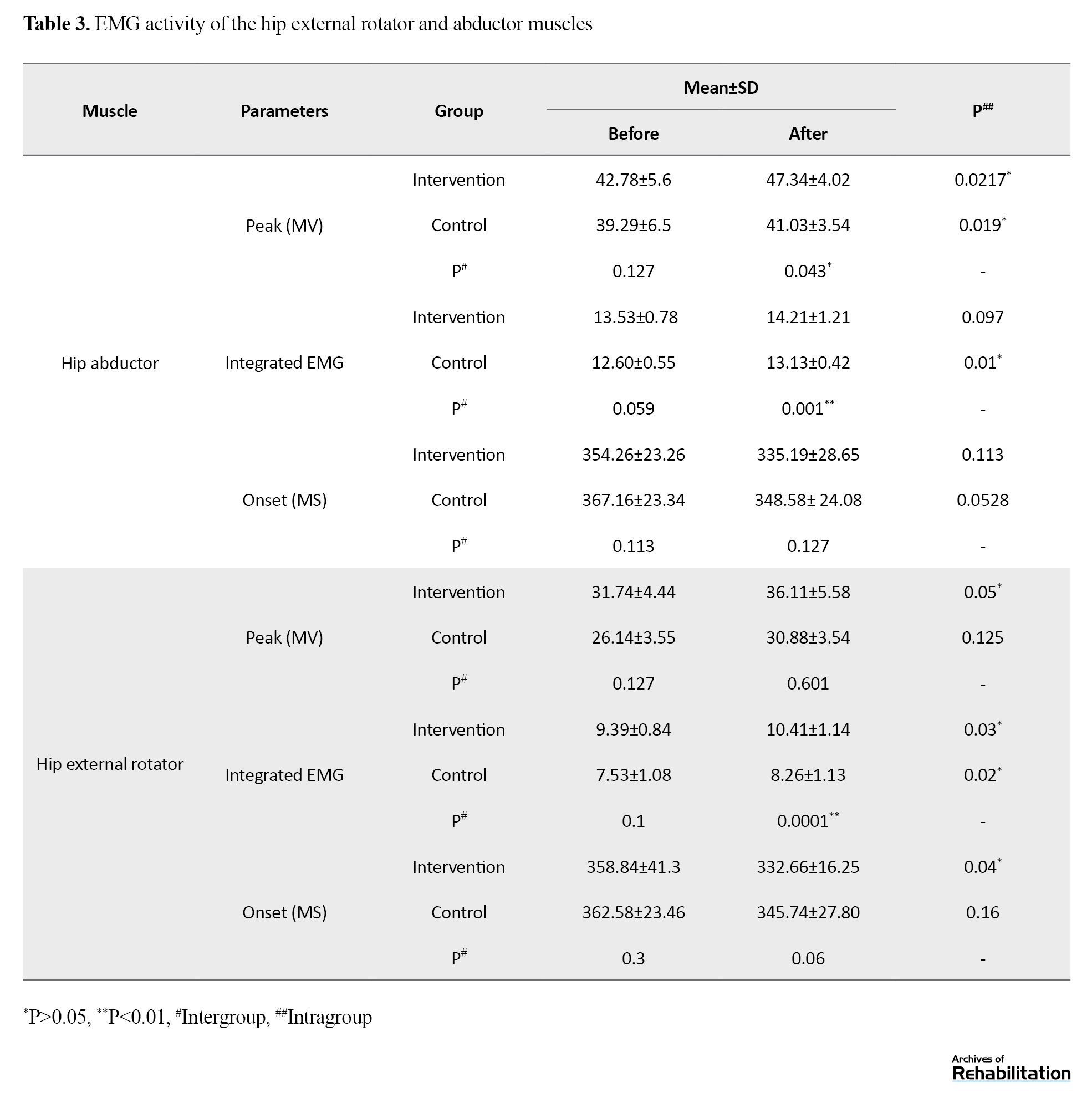
Regarding the results of EMG of the hip external rotator muscle, the maximum contraction of the control group was significantly increased following the intervention, but not for the control group. Maximum hip external rotator muscle contraction showed no change between the two groups following 8-week treatment. An intragroup comparison of the integrated EMG of this muscle showed that this parameter significantly improved in both the intervention and control groups after the 8-week treatment. The intergroup comparison results demonstrated that the integrated EMG after 8 weeks in the intervention group was significantly higher compared to the control group. The onset of muscle activity in the intervention group after 8 weeks of intervention was reduced considerably, but there was no significant change in the control group. Also, a significant change was found in intergroup comparison (Table 3).
Discussion
This research investigated the influence of EMG biofeedback training of the hip external rotator and abductor muscles on pain and muscle EMG activity in PFPS. The results of MVIC and EMG of hip abduction muscles indicated that following 8 weeks of intervention, the biofeedback group showed higher maximum EMG and MVIC activity than the control group. Therefore, hip abductor muscle biofeedback training in PFPS patients could increase the EMG activity of hip abductor muscles more than routine treatment. EMG biofeedback seems to have caused this phenomenon by facilitating treatment acceptance by patients, modulating muscle activation, and improving neuromuscular control [18]. EMG biofeedback is a method by which a person tries to activate and control muscles consciously. Research has shown that using this biofeedback in knee muscles reduces pain in people with knee osteoarthritis and decreases hyperextension in the mid-stance phase in individuals with anterior knee pain [34, 35]. The possible mechanism of these changes due to biofeedback is using more fibers with higher frequency and better cooperation between motor units of muscle that can increase the rate of contraction and muscle tension [24].
Since weakness or motor control disorder of hip abductor muscles can be one of the causes of PFPS [19], strengthening hip abductor muscles can reduce pain and improve function in patients with PFPS [11, 20, 21]. Heo et al. showed that hip abductor muscle biofeedback training can cause the requirement of this muscle in healthy individuals [36]. Kim et al. also showed that EMG biofeedback could activate quadriceps muscles in people with PFPS [37]. Considering the importance of the EMG activity of hip abductor muscles in PFPS, exercise that can increase the EMG activity of these muscles [38] can help the recovery of these patients. Therefore, according to the results of this study, biofeedback exercises can be used in these patients’ proximal muscle strengthening training programs.
In the present study, MVIC and maximum EMG activity of the hip external rotator muscle had no significant change between the two groups of intervention and control. Although a significant improvement was found in both groups after the intervention, the biofeedback group showed a greater increase than the control group. In other words, biofeedback exercises on this muscle have activated it more. Weakness or motor control impairment of the hip external rotator muscles may be one of the causes of PFPS [19]. Still, the researchers of the present study did not find any published studies that investigated the effect of hip external rotator muscle using biofeedback training in patients with PFPS. However, Govil andNoohu [39] showed that in patients with incomplete spinal cord injury, biofeedback training of the hip external rotator muscle increases the amplitude of the EMG activity of this muscle. Alonazi et al. also reported that four weeks of EMG biofeedback complementary training caused significant improvements in quadriceps muscle strength in young male athletes with PFPS [24]. Therefore, biofeedback training of hip external rotator muscles can activate these muscles in patients with PFPS.
The study’s results indicated that 8-week biofeedback training of proximal hip muscles reduced pain in these patients, while routine treatment in the control group did not significantly reduce pain. After 8 weeks of treatment, the biofeedback group had significantly less pain than the control group. Therefore, based on the present study’s findings, it can be stated that adding biofeedback training by using the proximal hip muscles as opposed to routine treatment has reduced patients’ pain. This finding means that biofeedback exercises help reduce pain in these patients. Our results are consistent with Alba-Martín et al. (in a systematic review) and Bisi-Balogun [37, 38]. They also showed that proximal lower extremity exercises reduce pain in individuals with PFPS. It should be noted that the exercises that they used were not biofeedback training. Our results also align with the study by Letafatkar et al. which showed that biofeedback exercises of the muscles around the knee combined with preparation exercises reduced pain and risk of subsequent injuries [40]. In their study, biofeedback exercises were not performed in the proximal hip area, but they were locally done in the muscles around the knee. Rabelo’s study also found that motor control exercises had no greater effect on pain relief than isolated muscle training, which is inconsistent with the results of the current study and previous studies mentioned [41]. Although the exercises in this study were motor control exercises performed with EMG biofeedback, Rabelo’s study performed these exercises without biofeedback.
In general, it seems that biofeedback training of the proximal hip muscles can increase the muscles’ recruitment and the force of these muscles, which may improve clinical symptoms such as pain in patients with PFPS by correcting the movement pattern and aligning the joints of the lower limbs. Previous research has also reported that the force of the external rotator and hip abductor muscles plays a crucial role in controlling the alignment of dynamic valgus and hip internal rotation. These are mechanical factors underlying the development of PFPS [42]. Strengthening these muscles with progressive strengthening exercises improves patients’ clinical symptoms with PFPS [43]. Still, the performance of these exercises, along with the use of EMG biofeedback, has not been investigated, according to our knowledge. So, the results of the present work demonstrated the impact of these exercises on improving the requirement of these muscles and also pain in these patients. Therefore, the use of these exercises in the treatment of people with PFPS is recommended.
The study was limited by lacking a follow-up period after the treatment. It would be beneficial to assess the long-term impacts of the interventions to understand the differences between the two treatments better. For future studies, it is recommended to compare the effects of biofeedback training on the proximal and local muscles of the knee. Additionally, considering the influence of gender on lower extremity alignment and the incidence of PFPS [44], it is recommended that future studies compare these exercises between men and women.
Conclusion
Adding 8 weeks of biofeedback training on external rotator and hip abductor muscles to routine exercise therapy in PFPS can reduce pain and improve muscle strength and performance. This change could potentially slow down the degenerative process of the patellofemoral joint.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Science (SBMU), Tehran, Iran (Code: SBMU. RETECH. REC.1399.1117). Participants were informed of the study objectives. In addition to obtaining written consent, they were assured that information obtained from them would remain confidential.
Funding
The paper was extracted from the PhD dissertation of Mehdi Banan Khojasteh, approved by the Department of Physiotherapy, School of Rehabilitation, Shahid Beheshti University of Medical Science (SBMU), Tehran, Iran. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Mehdi Banan Khojasteh and Minoo Khalkhali Zavieh; Methodology and analysis: Khosro Khademi Kalantari and Alireza Akbarzadeh Baghban; Research: Mehdi Banan Khojasteh and Saeed Mikailii; rview, editing and final approval: Aliyeh Daryabor; Supervision: Minoo Khalkhali Zavieh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Authors appreciate the Department of Physiotherapy faculty members of the School of Rehabilitation, SBMU, for their support and thank all those who participated in this study.
References
- Vora M, Curry E, Chipman A, Matzkin E, Li X. Patellofemoral pain syndrome in female athletes: A review of diagnoses, etiology and treatment options. Orthopedic Reviews. 2018; 9(4):7281. [PMID]
- Almeida GP, Silva AP, França FJ, Magalhães MO, Burke TN, Marques AP. Q-angle in patellofemoral pain: Relationship with dynamic knee valgus, hip abductor torque, pain and function. Revista Brasileira de Ortopedia. 2016; 51(2):181-6. [DOI:10.1016/j.rboe.2016.01.010] [PMID]
- Boling MC, Padua DA, Alexander Creighton R. Concentric and eccentric torque of the hip musculature in individuals with and without patellofemoral pain. Journal of Athletic Training. 2009; 44(1):7-13. [DOI:10.4085/1062-6050-44.1.7] [PMID]
- Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. Journal of Orthopaedic & Sports Physical Therapy. 2003; 33(11):671-6. [DOI:10.2519/jospt.2003.33.11.671] [PMID]
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. Journal of Orthopaedic & Sports Physical Therapy. 2003; 33(11):639-46. [DOI:10.2519/jospt.2003.33.11.639] [PMID]
- Conneely M, O’Sullivan K. Gluteus maximus and gluteus medius in pelvic and hip stability: Isolation or synergistic activation? Physiotherapy Ireland. 2008; 29:6-10. [Link]
- Xie P, István B, Liang M. The relationship between patellofemoral pain syndrome and hip biomechanics: A systematic review with meta-analysis. Healthcare. 2022; 11(1):99. [DOI:10.3390/healthcare11010099] [PMID]
- Afzal MR, Oh MK, Choi HY, Yoon J. A novel balance training system using multimodal biofeedback. Biomedical Engineering Online. 2016; 15:42. [DOI:10.1186/s12938-016-0160-7] [PMID]
- Saltychev M, Dutton RA, Laimi K, Beaupré GS, Virolainen P, Fredericson M. Effectiveness of conservative treatment for patellofemoral pain syndrome: A systematic review and meta-analysis. Journal of Rehabilitation Medicine. 2018; 50(5):393-401. [DOI:10.2340/16501977-2295] [PMID]
- Pollatos D, Chandolias K, Giordamni MK, Chalkia A, Trevlaki E. Review of new data in physiotherapeutic approach to Patellofemoral Pain Syndrome (PFPS). Journal of Biosciences and Medicines. 2021; 9(2):103. [DOI:10.4236/jbm.2021.92010]
- Rogan S, Haehni M, Luijckx E, Dealer J, Reuteler S, Taeymans J. Effects of hip abductor muscles exercises on pain and function in patients with Patellofemoral pain: A systematic review and meta-analysis. Journal of Strength and Conditioning Research. 2019; 33(11):3174-87. [DOI:10.1519/JSC.0000000000002658] [PMID]
- Santos TR, Oliveira BA, Ocarino JM, Holt KG, Fonseca ST. Effectiveness of hip muscle strengthening in patellofemoral pain syndrome patients: A systematic review. Brazilian Journal of Physical Therapy. 2015; 19(3):167-76. [DOI:10.1590/bjpt-rbf.2014.0089] [PMID]
- Mikaili S, Khademi Kalantari K, KhalkhaliZavieh M, Daryabor A, Banan Khojasteh M, Akbarzadeh Baghban A. [Ultrasonography of knee muscles during SLR with different positions of hip and ankle in patellofemoral pain syndrome (Persian)]. Archives of Rehabilitation. 2023; 24(2):284-307. [DOI:10.32598/RJ.24.2.3670.1]
- Scali K, Roberts J, McFarland M, Marino K, Murray L. Is multi-joint or single joint strengthening more effective in reducing pain and improving function in women with patellofemoral pain syndrome? A systematic review and meta-analysis. International Journal of sports Physical Therapy. 2018; 13(3):321-34. [PMID]
- Duarte-Moreira RJ, Castro KV, Luz-Santos C, Martins JVP, Sá KN, Baptista AF. Electromyographic biofeedback in motor function recovery after peripheral nerve injury: An integrative review of the literature. Applied Psychophysiology and Biofeedback. 2018; 43(4):247-57. [DOI:10.1007/s10484-018-9403-7] [PMID]
- Karaborklu Argut S, Celik D, Yasacı Z. Effectiveness of therapeutic electromyographic biofeedback after orthopedic knee surgeries: A systematic review. Disability and Rehabilitation. 2022; 44(14):3364-72. [DOI:10.1080/09638288.2020.1867904] [PMID]
- Ogul A, Ercan S, ÇETİN C, Canbulut A, Ergan M, Acar HT, et al. The effect of biofeedback exercises for the quadriceps muscle on the muscle strength, balance, and proprioception. Medicina Dello Sport. 2022; 75(1):29-44. [DOI:10.23736/S0025-7826.22.03894-7]
- Kiefer AW, Kushner AM, Groene J, Williams C, Riley MA, Myer GD. A commentary on real-time biofeedback to augment neuromuscular training for ACL injury prevention in adolescent athletes. Journal of Sports Science & Medicine. 2015; 14(1):1-8.[PMID]
- Anwer, S, Quddus N, Miraj M, Equebal A. Effectiveness of electromyographic biofeedback training on quadriceps muscle strength in osteoarthritis of knee. Hong Kong Physiotherapy Journal. 2011; 29(2):86-93. [DOI:10.1016/j.hkpj.2011.06.006]
- Khayambashi K, Mohammadkhani Z, Ghaznavi K, Lyle MA, Powers CM. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: A randomized controlled trial. Journal of Orthopaedic & Sports Physical Therapy. 2012; 42(1):22-9. [DOI:10.2519/jospt.2012.3704] [PMID]
- Jamali N, Khayambashi K, Lenjannejadian S, Esmaeili H. [Effect of hip abductor and external rotator muscles strengthening on pain, hip muscles strength, and lower extremity kinematics in patients with patellofemoral pain (Persian)]. The Scientific Journal of Rehabilitation Medicine. 2020; 9(2):79-92. [Link]
- Dursun N, Dursun E, Kiliç Z. Electromyographic biofeedback-controlled exercise versus conservative care for patellofemoral pain syndrome. Archives of Physical Medicine and Rehabilitation. 2001; 82(12):1692-5. [DOI:10.1053/apmr.2001.26253] [PMID]
- Nejati P, Forogh B, Moeineddin R, Baradaran HR, Nejati M. Patellofemoral pain syndrome in Iranian female athletes. Acta Medica Iranica. 2011; 49(3):169-72. [PMID]
- Alonazi A, Hasan S, Anwer S, Jamal A, Parvez S, Alfaiz FAS, et al. Efficacy of electromyographic-biofeedback supplementation training with patellar taping on quadriceps strengthening in patellofemoral pain syndrome among young adult male athletes. International Journal of Environmental Research and Public Health. 2021; 18(9):4514. [DOI:10.3390/ijerph18094514] [PMID]
- Yip SL, Ng GY. Biofeedback supplementation to physiotherapy exercise programme for rehabilitation of patellofemoral pain syndrome: A randomized controlled pilot study. Clinical Rehabilitation. 2006; 20(12): 1050-7. [DOI:10.1177/0269215506071259] [PMID]
- Richards R, van den Noort JC, van der Esch M, Booij MJ, Harlaar J. Gait retraining using real-time feedback in patients with medial knee osteoarthritis: Feasibility and effects of a six-week gait training program. The Knee. 2018; 25(5):814-24. [DOI:10.1016/j.knee.2018.05.014] [PMID]
- Mentiplay BF, Perraton LG, Bower KJ, Adair B, Pua YH, Williams GP, et al. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: A reliability and validity study. Plos One. 2015; 10(10):e0140822. [DOI:10.1371/journal.pone.0140822] [PMID]
- Mikaili S, Khademi-Kalantari K, Rezasoltani A, Arzani P, Baghban AA. Quadriceps force production during straight leg raising at different hip positions with and without concomitant ankle dorsiflexion. Journal of Bodywork and Movement Therapies. 2018; 22(4):904-8. [DOI:10.1016/j.jbmt.2017.11.006] [PMID]
- Nakagawa TH, Moriya ET, Maciel CD, Serrão FV. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. Journal of Orthopaedic & Sports Physical Therapy. 2012; 42(6):491-501. [DOI:10.2519/jospt.2012.3987] [PMID]
- Thorborg K, Petersen J, Magnusson SP, Hölmich P. Clinical assessment of hip strength using a hand-held dynamometer is reliable. Scandinavian Journal of Medicine & Science in Sports. 2010; 20(3):493-501. [DOI:10.1111/j.1600-0838.2009.00958.x] [PMID]
- Baldon Rde M, Serrão FV, Scattone Silva R, Piva SR. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: A randomized clinical trial. The Journal of Orthopaedic and Sports Physical Therapy. 2014; 44(4): p. 240-51.[DOI:10.2519/jospt.2014.4940] [PMID]
- Eid MA, Aly SM, El-Shamy SM. Effect of electromyographic biofeedback training on pain, quadriceps muscle strength, and functional ability in juvenile rheumatoid arthritis. American Journal of Physical Medicine & Rehabilitation. 2016; 95(12):921-30. [DOI:10.1097/PHM.0000000000000524] [PMID]
- Petruzzello SJ, Landers DM, Salazar W. Biofeedback and sport/exercise performance: Applications and limitations. Behavior Therapy. 1991; 22(3):379-92. [DOI:10.1016/S0005-7894(05)80372-7]
- Heo HJ, An DH, Yoo WG, Oh JS. EMG analysis of gluteus medius subdivisions during modified unilateral biofeedback exercises for the lower limbs. Journal of Physical Therapy Science. 2013; 25(1):85-8. [DOI:10.1589/jpts.25.85]
- Kim JH. Effects of EMG-biofeedback using closed kinetic chain exercise on Q-angle and quadriceps muscle activation in patellofemoral pain syndrome. The Journal of Korean Physical Therapy. 2016; 28(2):65-70. [Link]
- Barton CJ, Lack S, Malliaras P, Morrissey D. Gluteal muscle activity and patellofemoral pain syndrome: A systematic review. British Journal of Sports Medicine. 2013; 47(4):207-14. [DOI:10.1136/bjsports-2012-090953] [PMID]
- Alba-Martín P, Gallego-Izquierdo T, Plaza-Manzano G, Romero-Franco N, Núñez-Nagy S, Pecos-Martín D. Effectiveness of therapeutic physical exercise in the treatment of patellofemoral pain syndrome: A systematic review. Journal of Physical Therapy Science. 2015; 27(7):2387-90. [DOI:10.1589/jpts.27.2387] [PMID]
- Bisi-Balogun A, Torlak F. Outcomes following hip and quadriceps strengthening exercises for patellofemoral syndrome: A systematic review and meta-analysis. Sports. 2015; 3(4):281-301. [DOI:10.3390/sports3040281]
- Govil K, Noohu MM. Effect of EMG biofeedback training of gluteus maximus muscle on gait parameters in incomplete spinal cord injury. NeuroRehabilitation. 2013; 33(1):147-52. [PMID]
- Letafatkar A, Rabiei P, Farivar N, Alamouti G. Long-term efficacy of conditioning training program combined with feedback on kinetics and kinematics in male runners. Scandinavian Journal of Medicine & Science in Sports. 2020; 30(3):429-41. [DOI:10.1111/sms.13587] [PMID]
- Rabelo NDDA, Costa LOP, Lima BM, Dos Reis AC, Bley AS, Fukuda TY, et al. Adding motor control training to muscle strengthening did not substantially improve the effects on clinical or kinematic outcomes in women with patellofemoral pain: A randomised controlled trial. Gait & Posture. 2017; 58:280-6. [DOI:10.1016/j.gaitpost.2017.08.018] [PMID]
- Sahrmann, S. Movement system impairment syndromes of the extremities, cervical and thoracic spines. Amsterdam: Elsevier Health Sciences; 2010. [Link]
- Raisi A, Shojaedin S S, Habibi R. The effect and durability of hip and core exercises on pain and performance in females with patellofemoral pain syndrome.Physical Treatments - Specific Physical Therapy Journal. 2020; 10(3):145-58. [DOI:10.32598/ptj.10.3.431.1]
- Jacobs CA, Uhl TL, Mattacola CG, Shapiro R, Rayens WS. Hip abductor function and lower extremity landing kinematics: Sex differences. Journal of Athletic Training. 2007; 42(1):76-83. [PMID]
Type of Study: Original |
Subject:
Physical Therapy
Received: 8/11/2023 | Accepted: 4/03/2024 | Published: 31/07/2024
Received: 8/11/2023 | Accepted: 4/03/2024 | Published: 31/07/2024
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |