Volume 25, Issue 3 (Autumn 2024)
jrehab 2024, 25(3): 476-499 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alipour F, Arabkari Z, Mardani M, Ahmadi S, Afsharpouya H, Shoaa Kazemi M. Exploring Challenges and Obstacles in Psychosocial Rehabilitation for Individuals With Chronic Mental Disorders: A Qualitative Study. jrehab 2024; 25 (3) :476-499
URL: http://rehabilitationj.uswr.ac.ir/article-1-3385-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3385-en.html
Fardin Alipour1 

 , Zoleikha Arabkari *2
, Zoleikha Arabkari *2 

 , Mostafa Mardani1
, Mostafa Mardani1 

 , Shokoufeh Ahmadi3
, Shokoufeh Ahmadi3 
 , Hosein Afsharpouya1
, Hosein Afsharpouya1 
 , Mehrangiz Shoaa Kazemi4
, Mehrangiz Shoaa Kazemi4 




 , Zoleikha Arabkari *2
, Zoleikha Arabkari *2 

 , Mostafa Mardani1
, Mostafa Mardani1 

 , Shokoufeh Ahmadi3
, Shokoufeh Ahmadi3 
 , Hosein Afsharpouya1
, Hosein Afsharpouya1 
 , Mehrangiz Shoaa Kazemi4
, Mehrangiz Shoaa Kazemi4 


1- Department of Social Work, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Social Work, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,z.arabgari@gmail.com
3- Health in Emergency and Disaster Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Women’s and Family Studies, Faculty of Social Sciences and Economics, Alzahra University, Tehran, Iran.
2- Department of Social Work, School of Social Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Health in Emergency and Disaster Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Women’s and Family Studies, Faculty of Social Sciences and Economics, Alzahra University, Tehran, Iran.
Keywords: Chronic mental patients, Social rehabilitation, Psychosocial rehabilitation, Qualitative study
Full-Text [PDF 1810 kb]
(1343 Downloads)
| Abstract (HTML) (6586 Views)
Full-Text: (2483 Views)
Introduction
Health encompasses various dimensions, including psychological well-being, which can profoundly influence individuals’ lives, encompassing their social functioning and extending to their families and communities. Mental illness brings about significant disruptions in cognition, emotional regulation and behavior, often impairing crucial aspects of life [1]. In 2019, global statistics indicated that one in every eight individuals had a mental disorder, amounting to approximately 970 million people worldwide [2]. The prevalence of these disorders has surged with the COVID-19 pandemic, exacerbating vulnerabilities in affected populations [3, 4]. Individuals grappling with chronic mental disorders encounter multifaceted challenges, including discrimination and diminished social quality of life (QoL) [5]. They are frequently subjected to physical or emotional violence and misconceptions, compounding their struggles. Moreover, societal stigma often labels them as disorganized, destructive, or aggressive [6], leading to adverse consequences such as disrupted treatment, hindered recovery [7, 8], effects on personal, familial, educational, emotional, and occupational aspects[9] and heightened suicide risks [10].
Additionally, they face significant disparities in healthcare, with life expectancy estimates trailing the general population by up to 20 years [11]. The integral role of families in the care of individuals with mental disorders becomes apparent as they serve as primary caregivers, spending significant amounts of time providing direct and indirect support. This familial responsibility brings forth many challenges, ranging from reduced social interactions and experiences of ostracism to practical difficulties like limited access to public transportation, further complicating the caregiving dynamic [12] and potentially necessitating specialized services for family members [13].
Recent studies have delved into the challenges faced by families of individuals with mental disorders [14], as well as the psychological and social hurdles encountered by youth with chronic illnesses [15] and migrants during the pandemic [16]. Moreover, there’s emerging research on the interplay between psychological disorders and medical conditions [17], such as cardiovascular diseases [18]. Despite this scholarly attention, there remains a noticeable gap in understanding the psychosocial rehabilitation process for these individuals, highlighting the need for further investigation. Psychosocial rehabilitation, in tandem with therapeutic interventions, holds promise for expediting and enhancing the reintegration of individuals with mental disorders into mainstream social life. Relying solely on medication-based treatments while neglecting psychosocial interventions risks impeding their path to relative independence. Social workers, alongside other supportive professionals, play a pivotal role in facilitating this process, leveraging their expertise within treatment teams. Psychiatric hospitals serve as key settings where social workers assess and fortify social support systems, provide interventions to reduce caregiving burdens, and foster a supportive environment for patients and their families.
Identifying and addressing the psychological and social challenges inherent in rehabilitating this group is crucial for improving their overall well-being. Examining these challenges from the perspectives of patients, family members, and professionals promises positive outcomes for all stakeholders involved in the rehabilitation process.
Materials and Methods
This study employed a qualitative research method with a contractual content analysis approach. Participants were selected using purposive sampling from November 2021 to December 2021 to achieve maximum diversity. The inclusion criteria for participants required individuals to have a chronic psychiatric illness (such as depression, schizophrenia, or bipolar disorder), a minimum of three years of experience living with the illness, and the capacity to undergo an interview diagnosed by a psychiatrist. For families, the inclusion criteria included having at least one family member with the aforementioned characteristics willing to participate in the study.
Additionally, specialists such as social workers, psychiatrists, and psychologists with at least three years of experience working in psychiatric treatment centers were included. Based on these inclusion criteria, individuals with chronic mental disorders in psychiatric hospitals in Tehran City, Iran (such as Razi and Roozbeh hospitals) who expressed interest in participating were invited for interviews through coordination with their treating physician. Sampling continued until saturation was reached, meaning no new data emerged from the interviews. The participants in this study comprised 13 individuals diagnosed with chronic mental illnesses, 3 family members (spouse, father and mother) and 6 specialists (social worker, psychiatrist, and psychologist).
Following the acquisition of ethical approval and introduction letters, interviews were conducted and recorded with participants’ consent, outlining the objectives clearly. The interview questions centered on psychosocial needs both during hospitalization and after discharge. Data collection occurred through in-depth and semi-structured interviews conducted within hospital settings. Open-ended questions were employed during interviews, and data analysis followed the Graneheim and Lundman (2004) method across several stages.
Initially, interviews were transcribed verbatim, then meticulously condensed into concise units aligned with research goals. Subsequently, each sentence or paragraph was coded and codes representing common themes were organized into subcategories, which formed main categories. This iterative process was repeated to derive main categories and subcategories. To ensure validity, findings from 9 interviews were shared with 3 participants to ensure alignment with their experiences. Additionally, interviews underwent peer review with two colleagues alongside the extracted codes. Confidence and validation criteria were upheld throughout the study by having a researcher analyze the data. Credibility was maintained by thoughtfully selecting participants based on sampling criteria, maximizing diversity, holding multiple sessions to resolve coding differences and identify themes, summarizing and revising interviews with participants, and reviewing data and codes by the research team and professors. Field notes and reminders alongside interviews were utilized, underscoring the researchers’ focus. Adherence to ethical research principles included obtaining consent from participants for recording interviews and selecting interview environments based on participants’ comfort in the hospital, with assurance of confidentiality and withdrawing from the study at any time.
Results
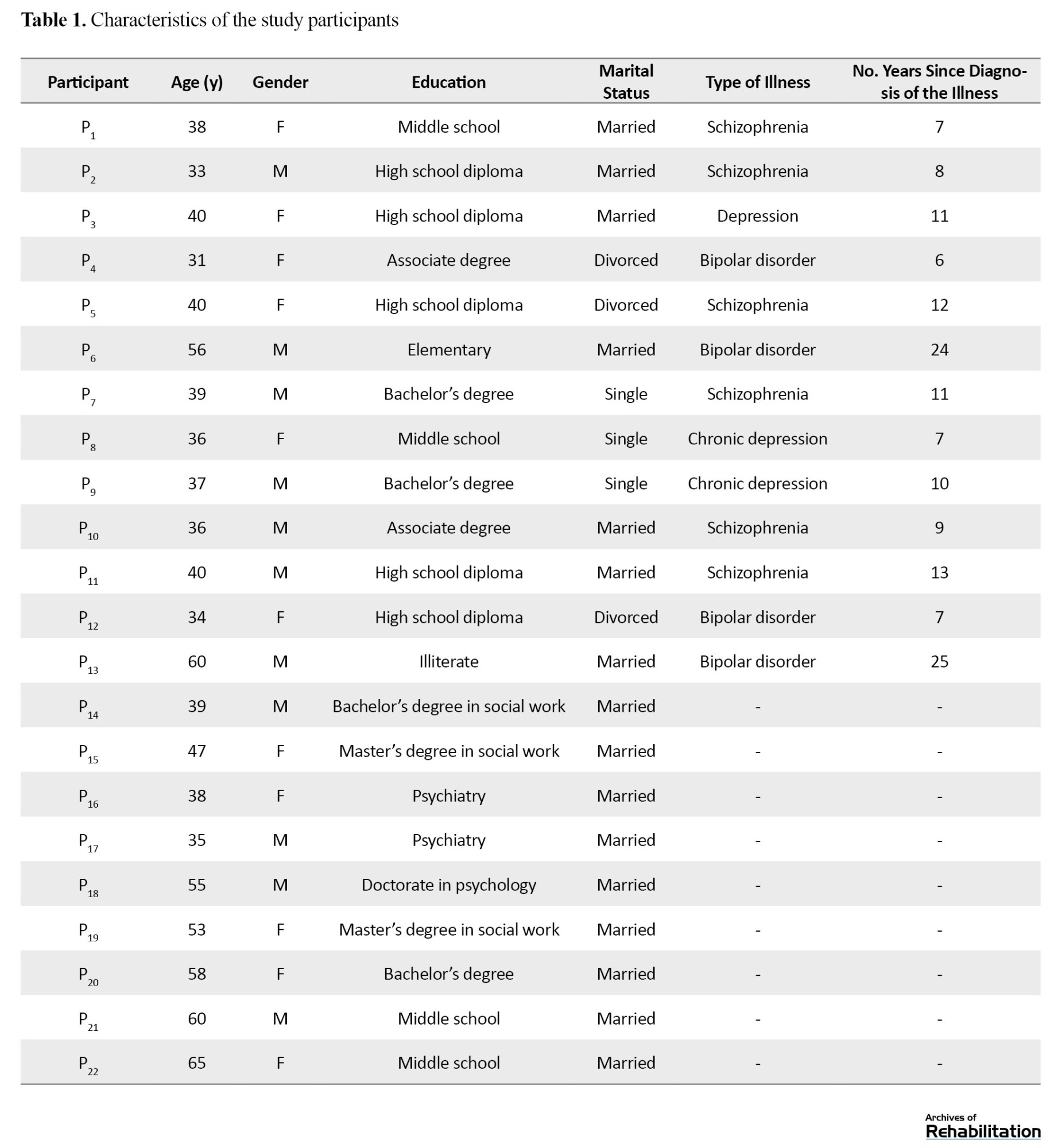
This research was conducted to study the psychosocial rehabilitation challenges of individuals with chronic mental disorders. The average age of female participants was 40 years; for males, it was 41 years. Among all participants, there were 11 men and 10 women. Sixteen participants were married. Educationally, 6 participants had education below high school, 5 had a high school diploma, 2 had an associate degree, 4 had a bachelor’s degree, 2 had a master’s degree and 3 had a doctoral degree (Table 1).
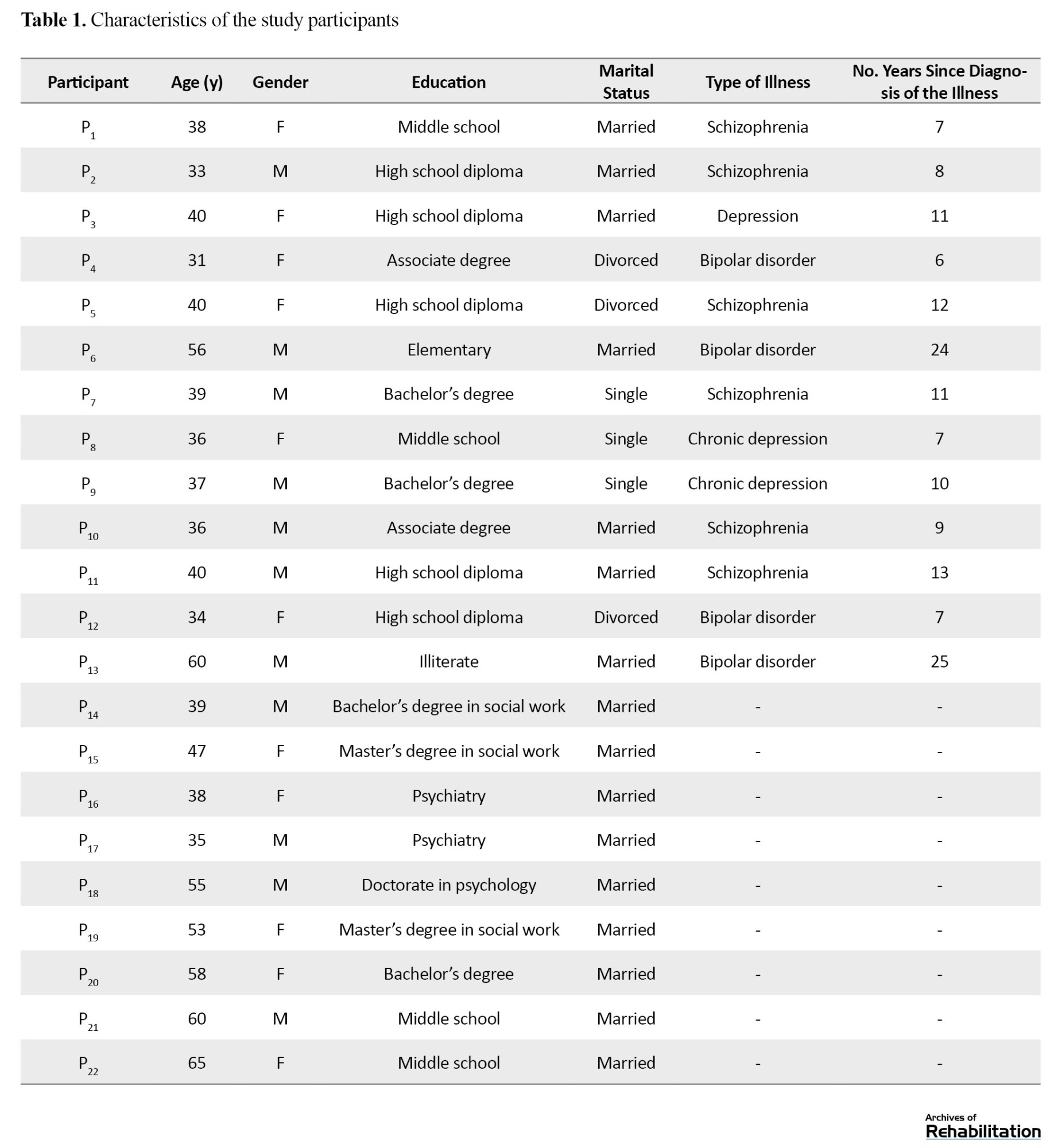
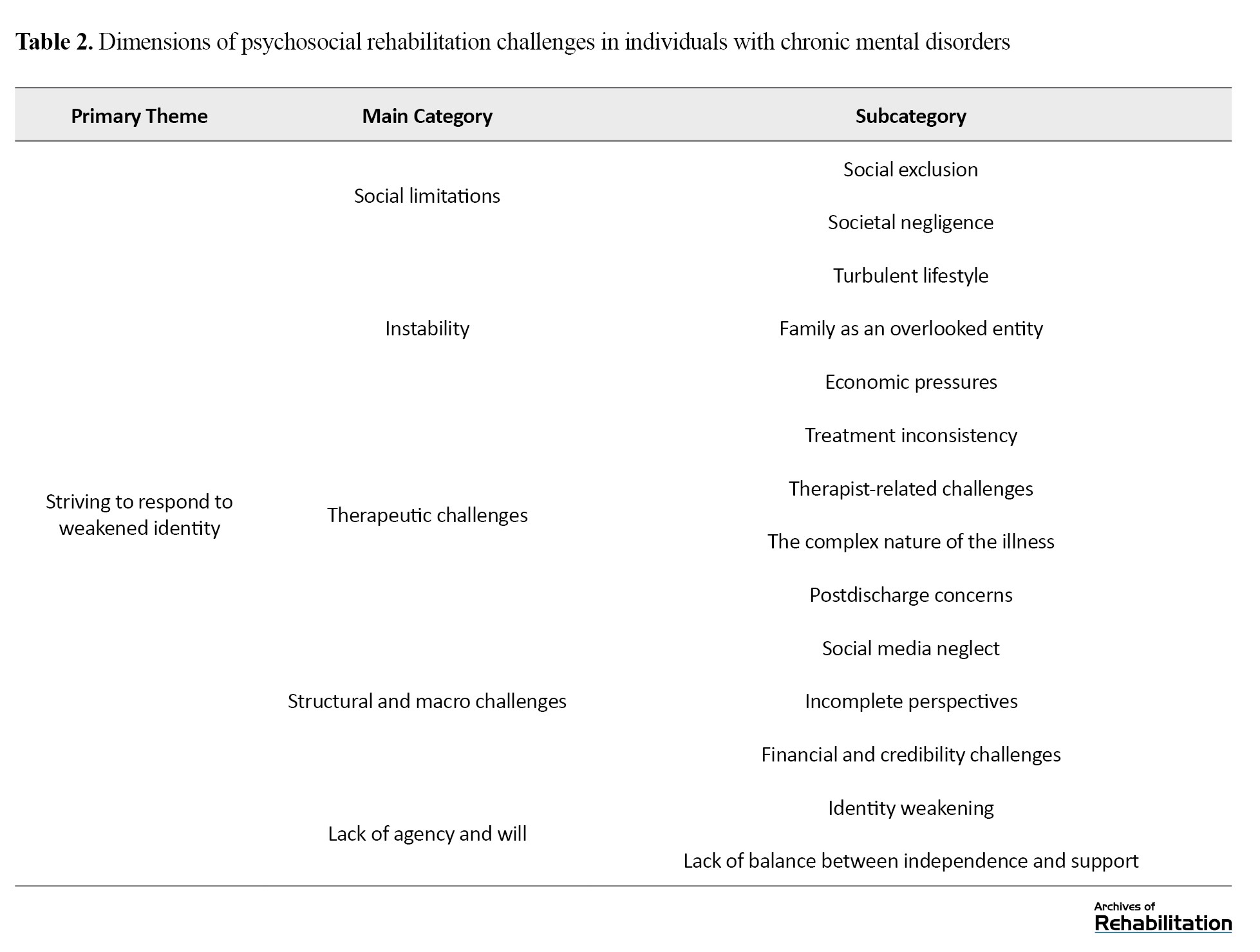
After analyzing the data and codes, 5 main Categories with 15 subcategories were extracted: 1) Social limitations (social exclusion, societal negligence); 2) Instability (turbulent lifestyle, family as an overlooked entity, and economic pressures); 3) Therapeutic challenges (treatment inconsistency, therapist-related challenges, the complex nature of the illness, and postdischarge concerns); 4) Structural and macro challenges (social media neglect, incomplete perspectives, financial and credibility challenges); 5) Loss of agency and volition (identity weakening, lack of balance between independence and support). Additionally, the primary theme of this research, “ striving to respond to weakened identity,” emerged from the aforementioned categories. These categories, along with subcategories, are presented in Table 2.
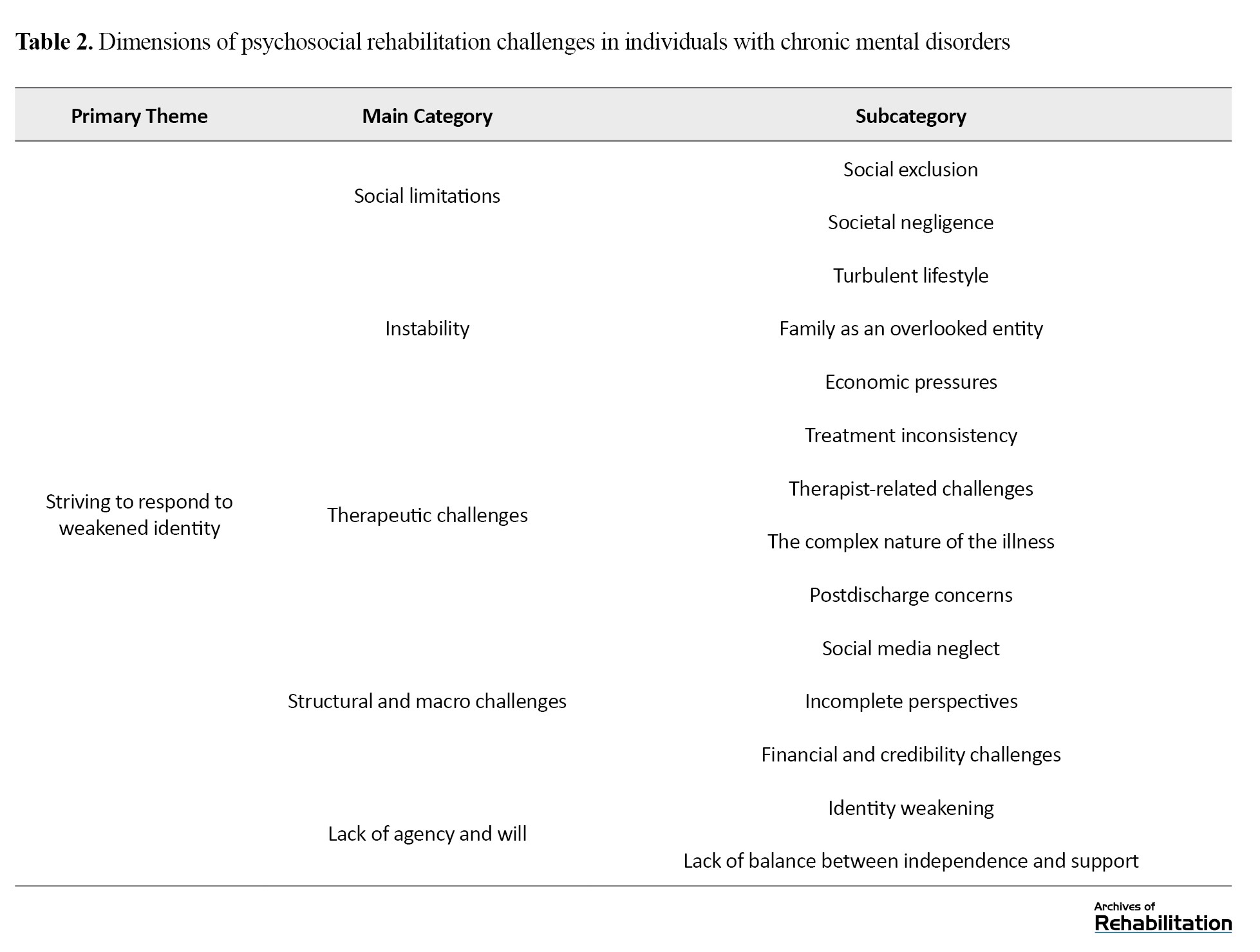
The primary focus of this study was the “striving to respond to weakened identity,” indicating that the rehabilitation process for individuals with chronic mental disorders is a complex endeavor characterized by both facilitating and hindering factors. Patients, their families, and rehabilitation teams aim to improve illness and stabilize their life situations. However, various challenges at different levels have resulted in conflicts, leading to delays in this improvement and stability. Some of the most significant challenges are outlined as follows.
Subcategory 1: Social exclusion
Participants and their families in this study perceived chronic mental illness accompanied by social stigma and discrimination, resulting in significant disruptions in their social relationships. Participant 1 describes the initial stages of illness as follows:
“Since I was diagnosed with this illness, my world completely changed; their behavior towards me completely changed. They would distance themselves from me as much as possible, and their interaction with me decreased significantly. Suddenly, I was excluded from many gatherings, left aside; even some of my closest friends abandoned me when I told them about my illness.”
Communication problems were among the recurring issues that paved the way for social ostracism:
“When I saw my family or friends, I felt anxious, and sometimes I didn’t want to see anyone” (Participant No. 7 [P7]).
This issue affects the individual and extends to the individual’s family. One family member describes the issue as follows:
“Visiting and socializing with family has become difficult for us, and we are afraid he may react inappropriately and cause trouble. Many have reduced their connection with us, or we have reduced it and in fact, we have become somewhat isolated” (P13).
Subcategory 2: Societal negligence
Another social constraint experienced directly by participants, primarily from their families and acquaintances, was the lack of social support. Participant No. 5 described his perception of the lack of social support as follows:
“Gradually, attention and looks towards me decreased, friends and acquaintances reduced their relationships, and suddenly, you feel like only a handful of people left around you, and you feel alone.”
Instability
The findings from this category include turbulent lifestyle, family as an overlooked entity, and economic pressures.
Subcategory 1: Turbulent lifestyle
One of the personal challenges faced by individuals with chronic mental disorders and their families is the disruption of lifestyle, which is facilitated by factors such as the lack of attention to other physical illnesses, time mismanagement, and poor self-management.
P6 (a mental patient) described this issue as follows:
“Since I became ill, many of my daily routines have been disrupted. From eating and sleeping to studying and working. Now, because I take medication, I often sleep until noon, and this often makes my day chaotic.”
Regarding the lack of attention to the physical illnesses of these individuals, one psychiatrist (P16) expresses:
“Some of these patients have diseases such as diabetes, cardiovascular diseases, nutritional problems, and even sexual problems that are mostly overlooked.”
Additionally, regarding the importance of education in this regard, P17 (a psychiatrist) stated:
“It is very important for patients to be aware of their condition, help themselves improve their situation, and prevent it from deteriorating. If they can control or even understand some aspects of their illness themselves, they will have fewer problems.”
Subcategory 2: Family as an overlooked entity
Families are often recognized as the primary caregivers, burdened with caregiving responsibilities in the treatment process, which, in addition to social pressures, disrupts the functioning of the family. This condition sometimes leads to neglect as an overlooked institution, and sometimes, one family member bears a heavier caregiving burden, leading to experiencing more problems. A mother of one of the patients expressed in this regard:
“Since he became ill, we have all been deeply shocked, and all our plans and activities have been affected. We were very stressed and worried. Everyone was somehow involved in this illness and its accompanying problems.”
The lack of knowledge and sufficient education exacerbate these conditions. The mother and caregiver of a patient said:
“No one told us anything, what expectations we should have, what we should do about his work, studies, recreation.”
Subcategory 3: Economic pressures
The findings of this study indicate that chronic mental illnesses, in addition to treatment costs, also have other economic problems, such as job disruption or unemployment, which exacerbate instability. Participant No. 11 (a patient) expressed in this regard:
“With the situation we have, we usually have two options: Either we have to lie to the employer and somehow hide it and not tell anything about our illness, or we have to tell the truth. If we talk about the illness, they often either don’t hire us, give us less wages, or give us meaningless tasks. If we don’t say anything about the illness, we are always stressed about what to do if they find out or if any signs or symptoms of the illness occur.”
In this regard, one of the specialists (social worker) expressed his opinion about the employment problems of people with a mental health condition as follows:
“One of the important areas for rehabilitation and stability in the lives of this group of patients is employment. However, the important point, in my opinion, is that the attitude and perspective of patients and their families towards employment should be adjusted, and they should not expect these individuals to work full-time or even as before. Instead, they should have reasonable expectations in line with the patient’s condition to avoid putting too much pressure on these individuals.” (Participant No. 19).
Therapeutic challenges
The category of therapeutic challenges in this study consists of four subcategories: Treatment inconsistency, therapist-related challenges, the complex nature of the illness, and postdischarge concerns, which will be addressed in this section.
Subcategory 1: Treatment inconsistency
One of the extracted subcategories related to the therapeutic challenges of individuals with mental illness was the absence of a comprehensive and cohesive treatment plan. Participants in this study considered the lack of a long-term view of the treatment plan and the dominance of medical interventions over psychological and social interventions as the most important factors contributing to therapeutic challenges for them. A specialist (psychiatrist) described these conditions as follows:
“In hospitals where psychiatric patients are hospitalized, especially in the case of chronic patients, there is no cohesive program for integrating various treatment and rehabilitation units, and most of the time, the goal is simply to keep the patients in the same conditions. Although psychological and social interventions are somewhat performed for these patients, they have not yet reached the level of coherence and coordination with other treatment programs that would be most effective.” (Participant No. 17).
Subcategory 2: Therapist-related challenges
In addition to individuals and families, therapists also face many challenges in the treatment process, which may lead to demotivation and despair from treatment. One of the specialists (psychologist) described these conditions as follows:
“Indeed, working properly and professionally with these patients is difficult. Unfortunately, some colleagues do not have the necessary motivation due to various problems in society and the work environment. They may become somewhat tired and may experience neglect and despair about their treatment situation.”
On the other hand, ignoring referrals and disregarding them in the treatment process is one of the challenges faced by individuals with chronic mental illness. Participants in this study emphasized the importance of paying attention to the presence and participation of patients themselves in treatment programs and demanded awareness of their treatment status and progress:
“Every day, many people in white coats come and go. Sometimes, they say things we don’t understand, and sometimes we fear our condition may worsen. I wish we knew what would happen next and when we would be discharged. How are we doing?” (P3, mental patient).
Subcategory 3: The complex nature of the illness
The prolongation of the treatment process and the time-consuming nature of adapting to the disease are among the challenges related to the disease in patients with mental disorders, which some participants describe as follows:
“Well, at first, we thought that after a few months of treatment and being here, our work would be done, and we would be discharged. But the more time passes, the more we realize that we still have work and are stuck and have to deal with these conditions.” (P8, mental patient).
Subcategory 4: Postdischarge concerns
Given that during the period when the individual lives outside the treatment environments, challenges such as relapse and discontinuation of medication treatments may occur. Many participants have concerns about discharge and independent living. One of the participating patients expressed:
“After we leave the hospital, things will be different, and I have to be able to manage my affairs myself. But honestly, I am always afraid that with the condition I have and with the medications I take, I can manage my life.” In this regard, a specialist No. 21 (social worker) stated:
“In fact, discharge plans for patients, especially psychiatric patients, should be designed and considered from the beginning of their entry, which unfortunately is not the case here. We should educate patients and their families in a way that they are prepared for discharge, and a successful discharge is one that does not cause much harm to the patient and does not lead to the patient’s quick return to the hospital. Of course, a successful discharge also depends on the family and social environment and the cultural networks of the people, which should be systematically considered in all these aspects.”
Structural and macro challenges
Alongside individual, familial, and professional influential factors, structural and macro-level factors were among the recurring themes of this study. This category includes three subcategories: Incomplete perspectives, social media neglect, and financial and credibility challenges.
Subcategory 1: Incomplete perspectives
One of the challenges in this domain is the attitude of policymakers and health planners, which lacks a comprehensive and systematic approach. A participant (social worker) in this regard expressed:
“Our officials do not consider the importance of mental health in society, how much budget is allocated to this area, what infrastructure we have, and if the view of these patients is seen as troublemakers for society and nothing is done for them, the situation will remain the same as we see it.”
Subcategory 2: Social media neglect
The professional handling of the media, along with their precision and sensitivity in the dissemination of news related to mental illnesses, is one of the important issues that participants have pointed out. Participant No. 12 (an individual with a mental disorder) describes this issue as follows:
“Unfortunately, sometimes in movies and series, words like crazy, lunatic, etc. are highlighted, and there are fewer movies and series that educate people on how to accept these patients, how to support them, how to behave with them and their families to reduce the burden of the disease.”
Subcategory 3: Financial and credibility challenges
One of the challenges mentioned by all participants, especially professionals in providing comprehensive rehabilitation services to the target group, is facing low allocations compared to service recipients. P18 (specialist-psychologist) acknowledged this:
“Rehabilitation services in psychological and social levels are essential for individuals and even their families, but we are faced with minimal funding and budget, which greatly affects the entire rehabilitation team and their services.”
Loss of agency and volition
This category addresses challenges that individuals experience regarding their abilities and willpower. Loss of agency includes two subcategories: Identity weakening and lack of balance between independence and support, which, according to the findings of this study, indicates that a significant role for these individuals should be considered in the rehabilitation process and their return to family and society.
Subcategory 1: Identity weakening
Some of the psychological challenges these individuals face endanger their identity, manifesting in negative psychological feelings. Participants in this study referred to feelings of worthlessness, ineffectiveness, and despair that distress them. P1 described this distressing situation as follows:
“Sometimes all this illness and medications make one weary. I feel like I’m useless. I don’t see any positive outcomes.”
Subcategory 2: Lack of balance between independence and support
The balance between independence and support in dealing with individuals and families with mental disorders acts like a double-edged sword that can greatly impact their situation. P16 (psychiatrist) expressed in this regard:
“Supporting these patients and their families can be helpful and effective in various ways. However, in some cases, this support is observed to move towards a direction where the patient’s rights and roles are not considered and somewhat neglected in the treatment or rehabilitation process. It should not proceed so patients have no role and freedom in major life choices.”
Discussion
The current study aimed to delve deeply into the psychological and social challenges encountered by individuals with chronic mental illnesses, their family caregivers, and professionals in the field on the path to rehabilitation. In essence, 5 primary themes and 15 secondary themes were distilled from the data. Themes such as “social limitation,” “instability,” “therapeutic challenges,” “structural and macro challenges,” and “loss of agency and volition” were instrumental in identifying the obstacles present in the journey of psychological and social rehabilitation for individuals with chronic mental illnesses. Broadly speaking, a notable portion of these challenges, like the first, third, and fourth themes, pertained to structural and social dimensions. In contrast, the second and fifth themes highlighted individual and familial issues. The first theme, “social limitations,” signifies challenges rooted in societal dynamics, involving the ostracism of individuals and their families by society and peers and deficiencies in social support structures—a pivotal aspect of the rehabilitation process. These individuals and their families contend with issues like societal stigma and discrimination, leading to a form of social alienation [19-21]. Moreover, the relationships of individuals and families affected by mental illness are impacted by this phenomenon, resulting in a lack of social support. Put differently, families encounter difficulties in addressing the challenges of a member’s mental illness due to inadequacies in support frameworks and assistance measures, thereby constraining their communication and facing significant hurdles in seeking aid and assistance [21-23]. The second main theme of this study was “instability,” which highlights challenges specifically encountered by families. These challenges and difficulties include unhealthy and turbulent family lifestyles, the neglect of families within support and healthcare systems, as well as economic pressures faced by families. In a way, families with a member experiencing a mental disorder, in addition to the caregiving burden [21، 24], also grapple with disruptions in their functioning, deviating from the natural course and undergoing changes in their structure at various levels such as marital relationships, parenting systems, familial dynamics, and various economic issues [21]. Examining the results of other studies, it can be observed that individuals with mental illness also confront serious challenges in their life trajectory regarding instability, including the onset of symptoms, medication side effects, and poor academic progress, leading to significant hurdles in their educational, occupational and personal stability [25-27]. Within the third theme, labeled “therapeutic challenges,” study participants acknowledged that dealing with disease-related issues and navigating treatment approaches were among the most significant and complex obstacles encountered in the journey of psychosocial rehabilitation. In essence, the lack of coherence in treatment plans and therapeutic interventions, coupled with factors such as deficient team coordination, can present substantial hurdles for all involved parties [28, 29]. Notably, the nature of the illness and its intricate and unpredictable trajectory can leave individuals bewildered and uncertain about timely discharge. Worries regarding disease relapse, discontinuation of medication, anxieties about transitioning to independent living, and uncertainties surrounding treatment and discharge constitute some of the challenges discussed in the realm of treatment and rehabilitation. It is important to highlight the challenges stemming from patients’ limited access to medications due to their complex nature and ongoing concerns among patients, caregivers, and professionals regarding medication adherence postdischarge, compounded by a lack of comprehensive information about postdischarge medication duration and potential side effects, all contributing to individuals’ struggles along this path [28, 29]. Moreover, mental health practitioners face various challenges arising from larger healthcare system structures. Structural barriers hindering timely and adequate service provision, insufficient medical, psychological, and social support resources for individuals and their caregivers, and administrative red tape all impact mental health service delivery [30]. Additionally, individuals and their primary caregivers grapple with challenges and obstacles in their interactions with healthcare providers, with a significant portion of these issues attributed to misdiagnosis by specialists, inadequate time allocated for patient consultations and the absence of conducive environments for active patient and caregiver involvement in the treatment process [22].
In the fourth theme, challenges assumed a structural and overarching form, targeting the highest echelons of the healthcare system and society. Often, the dissemination of non-scientific information regarding individuals with mental disorders leads to the perpetuation of discrimination and social stigma. In this context, social media platforms often depict individuals with mental disorders as more prone to violent crimes, influencing the perceptions of their audience. However, some studies indicate that the use of media by professionals and peer groups for accurate awareness-raising can mitigate social stigma toward individuals with mental disorders and provide access to reliable information in this field [31]. Notably, the lack of consensus between policy-making and implementation systems, alongside insufficient funding allocation and insurance support, poses significant challenges to therapeutic and rehabilitation objectives at macro and structural levels [32, 33].
Another discovery from this research, falling into the category of “loss of agency and volition,” highlights the imbalance between independence and assistance. This subcategory indicates that individuals with mental disorders and their families often feel a sense of deprivation of their will and autonomy, despite receiving support. In line with this, findings from a study suggest that caregivers frequently emotionally over-involve with individuals with mental disorders and strive to fulfill their wishes excessively [22].
Among the constraints of this study, we can mention issues, such as the illness of the primary participants, difficulty accessing individuals with mental disorders, their families, and social work specialists with adequate experience and expertise in the fields of mental health and social work. To address the first constraint, efforts were made to conduct interviews in collaboration with a psychiatrist under conditions where the individual had sufficient mental stability. The participants of this study were chosen from among hospitalized patients in psychiatric hospitals, and since many of them confront severe mental and social challenges and have been marginalized by their families, this could potentially influence the research outcomes. It is recommended that in future research, the challenges of family caregivers and specialized individuals in this field be separately addressed, and participants from the community level be selected in various centers.
Conclusion
This study aimed to understand the challenges faced by individuals with chronic mental illness from the perspectives of those with disorders, family caregivers and experts in the field. The findings demonstrate that participants in this study encounter various problems and challenges throughout the rehabilitation process, which do not depend on a single factor but emerge at different levels in individual, interpersonal, familial, societal, and structural dimensions. Therefore, addressing them requires consideration of various aspects.
Efforts to alleviate social limitations, address structural challenges, strengthen therapeutic and rehabilitation interventions, promote patient and family independence and empowerment, emphasize participatory approaches in therapeutic teams, and involve families and communities, as well as orient media programs, develop and establish support for non-governmental organizations in the field of psychosocial rehabilitation of people with a mental health condition, are among the most important points. These efforts can accelerate the improvement of patients and families by strengthening the process of mental and social rehabilitation. Policymakers and planners in the country’s health, family, welfare, and well-being sectors should pay special attention to this target group and their families to provide a foundation for reducing stigma, facilitating community integration, equalizing opportunities in society, enhancing community and family understanding of illnesses and patients’ capabilities, rehabilitating patients and families psychologically and socially, and reducing the caregiving burden and treatment costs for healthcare providers and families.
Social limitations
The main theme extracted from this study is social limitations experienced directly or indirectly by individuals with chronic mental illness. Social limitations encompass two subcategories: Social exclusion and societal negligence.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1400.098). Before taking part, all participants received an informed consent form to read and sign. No ethical concerns arose throughout the study, and there were no dropouts. Participants were assured of the confidentiality of their data throughout and after the study.
Funding
This research was funded by funded by Office of Social Welfare of Iran Ministry of Health and Medical Education.
Authors' contributions
Study design: Fardin Alipour, Zoliekha Arabkari, Shokoufeh Ahmadi and Mostafa Mardani; Conceptualization and formal analysis: Fardin Alipour, Zoliekha Arabkari and Hosein Afsharpouya; Data curation: Fardin Alipour, Zoliekha Arabkari, Shokoufeh Ahmadi, and Mostafa Mardani; Review and editing: Fardin Alipour, Mostafa Mardani and Mehrangiz Shoaa Kazemi; Investigation, methodology, resources, visualization and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Authors want to express their sincere gratitude to all participants, experts and officials who contributed to the implementation of this research.
References
Health encompasses various dimensions, including psychological well-being, which can profoundly influence individuals’ lives, encompassing their social functioning and extending to their families and communities. Mental illness brings about significant disruptions in cognition, emotional regulation and behavior, often impairing crucial aspects of life [1]. In 2019, global statistics indicated that one in every eight individuals had a mental disorder, amounting to approximately 970 million people worldwide [2]. The prevalence of these disorders has surged with the COVID-19 pandemic, exacerbating vulnerabilities in affected populations [3, 4]. Individuals grappling with chronic mental disorders encounter multifaceted challenges, including discrimination and diminished social quality of life (QoL) [5]. They are frequently subjected to physical or emotional violence and misconceptions, compounding their struggles. Moreover, societal stigma often labels them as disorganized, destructive, or aggressive [6], leading to adverse consequences such as disrupted treatment, hindered recovery [7, 8], effects on personal, familial, educational, emotional, and occupational aspects[9] and heightened suicide risks [10].
Additionally, they face significant disparities in healthcare, with life expectancy estimates trailing the general population by up to 20 years [11]. The integral role of families in the care of individuals with mental disorders becomes apparent as they serve as primary caregivers, spending significant amounts of time providing direct and indirect support. This familial responsibility brings forth many challenges, ranging from reduced social interactions and experiences of ostracism to practical difficulties like limited access to public transportation, further complicating the caregiving dynamic [12] and potentially necessitating specialized services for family members [13].
Recent studies have delved into the challenges faced by families of individuals with mental disorders [14], as well as the psychological and social hurdles encountered by youth with chronic illnesses [15] and migrants during the pandemic [16]. Moreover, there’s emerging research on the interplay between psychological disorders and medical conditions [17], such as cardiovascular diseases [18]. Despite this scholarly attention, there remains a noticeable gap in understanding the psychosocial rehabilitation process for these individuals, highlighting the need for further investigation. Psychosocial rehabilitation, in tandem with therapeutic interventions, holds promise for expediting and enhancing the reintegration of individuals with mental disorders into mainstream social life. Relying solely on medication-based treatments while neglecting psychosocial interventions risks impeding their path to relative independence. Social workers, alongside other supportive professionals, play a pivotal role in facilitating this process, leveraging their expertise within treatment teams. Psychiatric hospitals serve as key settings where social workers assess and fortify social support systems, provide interventions to reduce caregiving burdens, and foster a supportive environment for patients and their families.
Identifying and addressing the psychological and social challenges inherent in rehabilitating this group is crucial for improving their overall well-being. Examining these challenges from the perspectives of patients, family members, and professionals promises positive outcomes for all stakeholders involved in the rehabilitation process.
Materials and Methods
This study employed a qualitative research method with a contractual content analysis approach. Participants were selected using purposive sampling from November 2021 to December 2021 to achieve maximum diversity. The inclusion criteria for participants required individuals to have a chronic psychiatric illness (such as depression, schizophrenia, or bipolar disorder), a minimum of three years of experience living with the illness, and the capacity to undergo an interview diagnosed by a psychiatrist. For families, the inclusion criteria included having at least one family member with the aforementioned characteristics willing to participate in the study.
Additionally, specialists such as social workers, psychiatrists, and psychologists with at least three years of experience working in psychiatric treatment centers were included. Based on these inclusion criteria, individuals with chronic mental disorders in psychiatric hospitals in Tehran City, Iran (such as Razi and Roozbeh hospitals) who expressed interest in participating were invited for interviews through coordination with their treating physician. Sampling continued until saturation was reached, meaning no new data emerged from the interviews. The participants in this study comprised 13 individuals diagnosed with chronic mental illnesses, 3 family members (spouse, father and mother) and 6 specialists (social worker, psychiatrist, and psychologist).
Following the acquisition of ethical approval and introduction letters, interviews were conducted and recorded with participants’ consent, outlining the objectives clearly. The interview questions centered on psychosocial needs both during hospitalization and after discharge. Data collection occurred through in-depth and semi-structured interviews conducted within hospital settings. Open-ended questions were employed during interviews, and data analysis followed the Graneheim and Lundman (2004) method across several stages.
Initially, interviews were transcribed verbatim, then meticulously condensed into concise units aligned with research goals. Subsequently, each sentence or paragraph was coded and codes representing common themes were organized into subcategories, which formed main categories. This iterative process was repeated to derive main categories and subcategories. To ensure validity, findings from 9 interviews were shared with 3 participants to ensure alignment with their experiences. Additionally, interviews underwent peer review with two colleagues alongside the extracted codes. Confidence and validation criteria were upheld throughout the study by having a researcher analyze the data. Credibility was maintained by thoughtfully selecting participants based on sampling criteria, maximizing diversity, holding multiple sessions to resolve coding differences and identify themes, summarizing and revising interviews with participants, and reviewing data and codes by the research team and professors. Field notes and reminders alongside interviews were utilized, underscoring the researchers’ focus. Adherence to ethical research principles included obtaining consent from participants for recording interviews and selecting interview environments based on participants’ comfort in the hospital, with assurance of confidentiality and withdrawing from the study at any time.
Results
This research was conducted to study the psychosocial rehabilitation challenges of individuals with chronic mental disorders. The average age of female participants was 40 years; for males, it was 41 years. Among all participants, there were 11 men and 10 women. Sixteen participants were married. Educationally, 6 participants had education below high school, 5 had a high school diploma, 2 had an associate degree, 4 had a bachelor’s degree, 2 had a master’s degree and 3 had a doctoral degree (Table 1).
After analyzing the data and codes, 5 main Categories with 15 subcategories were extracted: 1) Social limitations (social exclusion, societal negligence); 2) Instability (turbulent lifestyle, family as an overlooked entity, and economic pressures); 3) Therapeutic challenges (treatment inconsistency, therapist-related challenges, the complex nature of the illness, and postdischarge concerns); 4) Structural and macro challenges (social media neglect, incomplete perspectives, financial and credibility challenges); 5) Loss of agency and volition (identity weakening, lack of balance between independence and support). Additionally, the primary theme of this research, “ striving to respond to weakened identity,” emerged from the aforementioned categories. These categories, along with subcategories, are presented in Table 2.
The primary focus of this study was the “striving to respond to weakened identity,” indicating that the rehabilitation process for individuals with chronic mental disorders is a complex endeavor characterized by both facilitating and hindering factors. Patients, their families, and rehabilitation teams aim to improve illness and stabilize their life situations. However, various challenges at different levels have resulted in conflicts, leading to delays in this improvement and stability. Some of the most significant challenges are outlined as follows.
Subcategory 1: Social exclusion
Participants and their families in this study perceived chronic mental illness accompanied by social stigma and discrimination, resulting in significant disruptions in their social relationships. Participant 1 describes the initial stages of illness as follows:
“Since I was diagnosed with this illness, my world completely changed; their behavior towards me completely changed. They would distance themselves from me as much as possible, and their interaction with me decreased significantly. Suddenly, I was excluded from many gatherings, left aside; even some of my closest friends abandoned me when I told them about my illness.”
Communication problems were among the recurring issues that paved the way for social ostracism:
“When I saw my family or friends, I felt anxious, and sometimes I didn’t want to see anyone” (Participant No. 7 [P7]).
This issue affects the individual and extends to the individual’s family. One family member describes the issue as follows:
“Visiting and socializing with family has become difficult for us, and we are afraid he may react inappropriately and cause trouble. Many have reduced their connection with us, or we have reduced it and in fact, we have become somewhat isolated” (P13).
Subcategory 2: Societal negligence
Another social constraint experienced directly by participants, primarily from their families and acquaintances, was the lack of social support. Participant No. 5 described his perception of the lack of social support as follows:
“Gradually, attention and looks towards me decreased, friends and acquaintances reduced their relationships, and suddenly, you feel like only a handful of people left around you, and you feel alone.”
Instability
The findings from this category include turbulent lifestyle, family as an overlooked entity, and economic pressures.
Subcategory 1: Turbulent lifestyle
One of the personal challenges faced by individuals with chronic mental disorders and their families is the disruption of lifestyle, which is facilitated by factors such as the lack of attention to other physical illnesses, time mismanagement, and poor self-management.
P6 (a mental patient) described this issue as follows:
“Since I became ill, many of my daily routines have been disrupted. From eating and sleeping to studying and working. Now, because I take medication, I often sleep until noon, and this often makes my day chaotic.”
Regarding the lack of attention to the physical illnesses of these individuals, one psychiatrist (P16) expresses:
“Some of these patients have diseases such as diabetes, cardiovascular diseases, nutritional problems, and even sexual problems that are mostly overlooked.”
Additionally, regarding the importance of education in this regard, P17 (a psychiatrist) stated:
“It is very important for patients to be aware of their condition, help themselves improve their situation, and prevent it from deteriorating. If they can control or even understand some aspects of their illness themselves, they will have fewer problems.”
Subcategory 2: Family as an overlooked entity
Families are often recognized as the primary caregivers, burdened with caregiving responsibilities in the treatment process, which, in addition to social pressures, disrupts the functioning of the family. This condition sometimes leads to neglect as an overlooked institution, and sometimes, one family member bears a heavier caregiving burden, leading to experiencing more problems. A mother of one of the patients expressed in this regard:
“Since he became ill, we have all been deeply shocked, and all our plans and activities have been affected. We were very stressed and worried. Everyone was somehow involved in this illness and its accompanying problems.”
The lack of knowledge and sufficient education exacerbate these conditions. The mother and caregiver of a patient said:
“No one told us anything, what expectations we should have, what we should do about his work, studies, recreation.”
Subcategory 3: Economic pressures
The findings of this study indicate that chronic mental illnesses, in addition to treatment costs, also have other economic problems, such as job disruption or unemployment, which exacerbate instability. Participant No. 11 (a patient) expressed in this regard:
“With the situation we have, we usually have two options: Either we have to lie to the employer and somehow hide it and not tell anything about our illness, or we have to tell the truth. If we talk about the illness, they often either don’t hire us, give us less wages, or give us meaningless tasks. If we don’t say anything about the illness, we are always stressed about what to do if they find out or if any signs or symptoms of the illness occur.”
In this regard, one of the specialists (social worker) expressed his opinion about the employment problems of people with a mental health condition as follows:
“One of the important areas for rehabilitation and stability in the lives of this group of patients is employment. However, the important point, in my opinion, is that the attitude and perspective of patients and their families towards employment should be adjusted, and they should not expect these individuals to work full-time or even as before. Instead, they should have reasonable expectations in line with the patient’s condition to avoid putting too much pressure on these individuals.” (Participant No. 19).
Therapeutic challenges
The category of therapeutic challenges in this study consists of four subcategories: Treatment inconsistency, therapist-related challenges, the complex nature of the illness, and postdischarge concerns, which will be addressed in this section.
Subcategory 1: Treatment inconsistency
One of the extracted subcategories related to the therapeutic challenges of individuals with mental illness was the absence of a comprehensive and cohesive treatment plan. Participants in this study considered the lack of a long-term view of the treatment plan and the dominance of medical interventions over psychological and social interventions as the most important factors contributing to therapeutic challenges for them. A specialist (psychiatrist) described these conditions as follows:
“In hospitals where psychiatric patients are hospitalized, especially in the case of chronic patients, there is no cohesive program for integrating various treatment and rehabilitation units, and most of the time, the goal is simply to keep the patients in the same conditions. Although psychological and social interventions are somewhat performed for these patients, they have not yet reached the level of coherence and coordination with other treatment programs that would be most effective.” (Participant No. 17).
Subcategory 2: Therapist-related challenges
In addition to individuals and families, therapists also face many challenges in the treatment process, which may lead to demotivation and despair from treatment. One of the specialists (psychologist) described these conditions as follows:
“Indeed, working properly and professionally with these patients is difficult. Unfortunately, some colleagues do not have the necessary motivation due to various problems in society and the work environment. They may become somewhat tired and may experience neglect and despair about their treatment situation.”
On the other hand, ignoring referrals and disregarding them in the treatment process is one of the challenges faced by individuals with chronic mental illness. Participants in this study emphasized the importance of paying attention to the presence and participation of patients themselves in treatment programs and demanded awareness of their treatment status and progress:
“Every day, many people in white coats come and go. Sometimes, they say things we don’t understand, and sometimes we fear our condition may worsen. I wish we knew what would happen next and when we would be discharged. How are we doing?” (P3, mental patient).
Subcategory 3: The complex nature of the illness
The prolongation of the treatment process and the time-consuming nature of adapting to the disease are among the challenges related to the disease in patients with mental disorders, which some participants describe as follows:
“Well, at first, we thought that after a few months of treatment and being here, our work would be done, and we would be discharged. But the more time passes, the more we realize that we still have work and are stuck and have to deal with these conditions.” (P8, mental patient).
Subcategory 4: Postdischarge concerns
Given that during the period when the individual lives outside the treatment environments, challenges such as relapse and discontinuation of medication treatments may occur. Many participants have concerns about discharge and independent living. One of the participating patients expressed:
“After we leave the hospital, things will be different, and I have to be able to manage my affairs myself. But honestly, I am always afraid that with the condition I have and with the medications I take, I can manage my life.” In this regard, a specialist No. 21 (social worker) stated:
“In fact, discharge plans for patients, especially psychiatric patients, should be designed and considered from the beginning of their entry, which unfortunately is not the case here. We should educate patients and their families in a way that they are prepared for discharge, and a successful discharge is one that does not cause much harm to the patient and does not lead to the patient’s quick return to the hospital. Of course, a successful discharge also depends on the family and social environment and the cultural networks of the people, which should be systematically considered in all these aspects.”
Structural and macro challenges
Alongside individual, familial, and professional influential factors, structural and macro-level factors were among the recurring themes of this study. This category includes three subcategories: Incomplete perspectives, social media neglect, and financial and credibility challenges.
Subcategory 1: Incomplete perspectives
One of the challenges in this domain is the attitude of policymakers and health planners, which lacks a comprehensive and systematic approach. A participant (social worker) in this regard expressed:
“Our officials do not consider the importance of mental health in society, how much budget is allocated to this area, what infrastructure we have, and if the view of these patients is seen as troublemakers for society and nothing is done for them, the situation will remain the same as we see it.”
Subcategory 2: Social media neglect
The professional handling of the media, along with their precision and sensitivity in the dissemination of news related to mental illnesses, is one of the important issues that participants have pointed out. Participant No. 12 (an individual with a mental disorder) describes this issue as follows:
“Unfortunately, sometimes in movies and series, words like crazy, lunatic, etc. are highlighted, and there are fewer movies and series that educate people on how to accept these patients, how to support them, how to behave with them and their families to reduce the burden of the disease.”
Subcategory 3: Financial and credibility challenges
One of the challenges mentioned by all participants, especially professionals in providing comprehensive rehabilitation services to the target group, is facing low allocations compared to service recipients. P18 (specialist-psychologist) acknowledged this:
“Rehabilitation services in psychological and social levels are essential for individuals and even their families, but we are faced with minimal funding and budget, which greatly affects the entire rehabilitation team and their services.”
Loss of agency and volition
This category addresses challenges that individuals experience regarding their abilities and willpower. Loss of agency includes two subcategories: Identity weakening and lack of balance between independence and support, which, according to the findings of this study, indicates that a significant role for these individuals should be considered in the rehabilitation process and their return to family and society.
Subcategory 1: Identity weakening
Some of the psychological challenges these individuals face endanger their identity, manifesting in negative psychological feelings. Participants in this study referred to feelings of worthlessness, ineffectiveness, and despair that distress them. P1 described this distressing situation as follows:
“Sometimes all this illness and medications make one weary. I feel like I’m useless. I don’t see any positive outcomes.”
Subcategory 2: Lack of balance between independence and support
The balance between independence and support in dealing with individuals and families with mental disorders acts like a double-edged sword that can greatly impact their situation. P16 (psychiatrist) expressed in this regard:
“Supporting these patients and their families can be helpful and effective in various ways. However, in some cases, this support is observed to move towards a direction where the patient’s rights and roles are not considered and somewhat neglected in the treatment or rehabilitation process. It should not proceed so patients have no role and freedom in major life choices.”
Discussion
The current study aimed to delve deeply into the psychological and social challenges encountered by individuals with chronic mental illnesses, their family caregivers, and professionals in the field on the path to rehabilitation. In essence, 5 primary themes and 15 secondary themes were distilled from the data. Themes such as “social limitation,” “instability,” “therapeutic challenges,” “structural and macro challenges,” and “loss of agency and volition” were instrumental in identifying the obstacles present in the journey of psychological and social rehabilitation for individuals with chronic mental illnesses. Broadly speaking, a notable portion of these challenges, like the first, third, and fourth themes, pertained to structural and social dimensions. In contrast, the second and fifth themes highlighted individual and familial issues. The first theme, “social limitations,” signifies challenges rooted in societal dynamics, involving the ostracism of individuals and their families by society and peers and deficiencies in social support structures—a pivotal aspect of the rehabilitation process. These individuals and their families contend with issues like societal stigma and discrimination, leading to a form of social alienation [19-21]. Moreover, the relationships of individuals and families affected by mental illness are impacted by this phenomenon, resulting in a lack of social support. Put differently, families encounter difficulties in addressing the challenges of a member’s mental illness due to inadequacies in support frameworks and assistance measures, thereby constraining their communication and facing significant hurdles in seeking aid and assistance [21-23]. The second main theme of this study was “instability,” which highlights challenges specifically encountered by families. These challenges and difficulties include unhealthy and turbulent family lifestyles, the neglect of families within support and healthcare systems, as well as economic pressures faced by families. In a way, families with a member experiencing a mental disorder, in addition to the caregiving burden [21، 24], also grapple with disruptions in their functioning, deviating from the natural course and undergoing changes in their structure at various levels such as marital relationships, parenting systems, familial dynamics, and various economic issues [21]. Examining the results of other studies, it can be observed that individuals with mental illness also confront serious challenges in their life trajectory regarding instability, including the onset of symptoms, medication side effects, and poor academic progress, leading to significant hurdles in their educational, occupational and personal stability [25-27]. Within the third theme, labeled “therapeutic challenges,” study participants acknowledged that dealing with disease-related issues and navigating treatment approaches were among the most significant and complex obstacles encountered in the journey of psychosocial rehabilitation. In essence, the lack of coherence in treatment plans and therapeutic interventions, coupled with factors such as deficient team coordination, can present substantial hurdles for all involved parties [28, 29]. Notably, the nature of the illness and its intricate and unpredictable trajectory can leave individuals bewildered and uncertain about timely discharge. Worries regarding disease relapse, discontinuation of medication, anxieties about transitioning to independent living, and uncertainties surrounding treatment and discharge constitute some of the challenges discussed in the realm of treatment and rehabilitation. It is important to highlight the challenges stemming from patients’ limited access to medications due to their complex nature and ongoing concerns among patients, caregivers, and professionals regarding medication adherence postdischarge, compounded by a lack of comprehensive information about postdischarge medication duration and potential side effects, all contributing to individuals’ struggles along this path [28, 29]. Moreover, mental health practitioners face various challenges arising from larger healthcare system structures. Structural barriers hindering timely and adequate service provision, insufficient medical, psychological, and social support resources for individuals and their caregivers, and administrative red tape all impact mental health service delivery [30]. Additionally, individuals and their primary caregivers grapple with challenges and obstacles in their interactions with healthcare providers, with a significant portion of these issues attributed to misdiagnosis by specialists, inadequate time allocated for patient consultations and the absence of conducive environments for active patient and caregiver involvement in the treatment process [22].
In the fourth theme, challenges assumed a structural and overarching form, targeting the highest echelons of the healthcare system and society. Often, the dissemination of non-scientific information regarding individuals with mental disorders leads to the perpetuation of discrimination and social stigma. In this context, social media platforms often depict individuals with mental disorders as more prone to violent crimes, influencing the perceptions of their audience. However, some studies indicate that the use of media by professionals and peer groups for accurate awareness-raising can mitigate social stigma toward individuals with mental disorders and provide access to reliable information in this field [31]. Notably, the lack of consensus between policy-making and implementation systems, alongside insufficient funding allocation and insurance support, poses significant challenges to therapeutic and rehabilitation objectives at macro and structural levels [32, 33].
Another discovery from this research, falling into the category of “loss of agency and volition,” highlights the imbalance between independence and assistance. This subcategory indicates that individuals with mental disorders and their families often feel a sense of deprivation of their will and autonomy, despite receiving support. In line with this, findings from a study suggest that caregivers frequently emotionally over-involve with individuals with mental disorders and strive to fulfill their wishes excessively [22].
Among the constraints of this study, we can mention issues, such as the illness of the primary participants, difficulty accessing individuals with mental disorders, their families, and social work specialists with adequate experience and expertise in the fields of mental health and social work. To address the first constraint, efforts were made to conduct interviews in collaboration with a psychiatrist under conditions where the individual had sufficient mental stability. The participants of this study were chosen from among hospitalized patients in psychiatric hospitals, and since many of them confront severe mental and social challenges and have been marginalized by their families, this could potentially influence the research outcomes. It is recommended that in future research, the challenges of family caregivers and specialized individuals in this field be separately addressed, and participants from the community level be selected in various centers.
Conclusion
This study aimed to understand the challenges faced by individuals with chronic mental illness from the perspectives of those with disorders, family caregivers and experts in the field. The findings demonstrate that participants in this study encounter various problems and challenges throughout the rehabilitation process, which do not depend on a single factor but emerge at different levels in individual, interpersonal, familial, societal, and structural dimensions. Therefore, addressing them requires consideration of various aspects.
Efforts to alleviate social limitations, address structural challenges, strengthen therapeutic and rehabilitation interventions, promote patient and family independence and empowerment, emphasize participatory approaches in therapeutic teams, and involve families and communities, as well as orient media programs, develop and establish support for non-governmental organizations in the field of psychosocial rehabilitation of people with a mental health condition, are among the most important points. These efforts can accelerate the improvement of patients and families by strengthening the process of mental and social rehabilitation. Policymakers and planners in the country’s health, family, welfare, and well-being sectors should pay special attention to this target group and their families to provide a foundation for reducing stigma, facilitating community integration, equalizing opportunities in society, enhancing community and family understanding of illnesses and patients’ capabilities, rehabilitating patients and families psychologically and socially, and reducing the caregiving burden and treatment costs for healthcare providers and families.
Social limitations
The main theme extracted from this study is social limitations experienced directly or indirectly by individuals with chronic mental illness. Social limitations encompass two subcategories: Social exclusion and societal negligence.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1400.098). Before taking part, all participants received an informed consent form to read and sign. No ethical concerns arose throughout the study, and there were no dropouts. Participants were assured of the confidentiality of their data throughout and after the study.
Funding
This research was funded by funded by Office of Social Welfare of Iran Ministry of Health and Medical Education.
Authors' contributions
Study design: Fardin Alipour, Zoliekha Arabkari, Shokoufeh Ahmadi and Mostafa Mardani; Conceptualization and formal analysis: Fardin Alipour, Zoliekha Arabkari and Hosein Afsharpouya; Data curation: Fardin Alipour, Zoliekha Arabkari, Shokoufeh Ahmadi, and Mostafa Mardani; Review and editing: Fardin Alipour, Mostafa Mardani and Mehrangiz Shoaa Kazemi; Investigation, methodology, resources, visualization and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Authors want to express their sincere gratitude to all participants, experts and officials who contributed to the implementation of this research.
References
- WHO. Mental disorders. Geneva: WHO; 2022. [Link]
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx).USA: Institute for Health Metrics and Evaluatio; 2021. [Link]
- Mojarrad Kahani AH, Ghanbari Hashem Abadi BA, Modares Gharavi M. [The efficacy of group psycho educational interventions in promoting quality of life and quality of relationships on family of patients with bipolar disorders (Persian)]. Journal of Research in Behavioural Sciences. 2012; 10(2):114-23. [Link]
- Sukut O, Ayhan Balik CH. The impact of COVID-19 pandemic on people with severe mental illness. Perspectives in Psychiatric Care. 2021; 57(2):953-6. [DOI:10.1111/ppc.12618] [PMID]
- Tong Chien W, Thompson DR, Fong Leung S, Bressington D. Quality of life, symptom severity and level of functioning in people with severe mental illness ready for hospital discharge. Journal of Psychiatric and Mental Health Nursing. 2022; 29(1):14-24. [DOI:10.1111/jpm.12703] [PMID]
- Tanyuy CB, Aguocha CM, Nwefoh EC, Wankam MG. Social representation of abuse of persons with severe mental illness in Jakiri, Cameroon: A qualitative study. International Journal of social Psychiatry. 2021; 67(7):946-54. [DOI:10.1177/0020764020972432] [PMID]
- Möhring M, Krick NK, Ditze A. The influence of social support and characteristics of the stigmatisers on stigmatising attitudes towards people with mental illness. European Journal of Health Communication. 2021; 2(2):66-96. [DOI:10.47368/ejhc.2021.204]
- Díaz-Mandado O, Periáñez JA. An effective psychological intervention in reducing internalized stigma and improving recovery outcomes in people with severe mental illness. Psychiatry Research. 2021; 295:113635. [DOI:10.1016/j.psychres.2020.113635] [PMID]
- Emami Z, Kajbaf MB. [The effectiveness of quality of life therapy on anxiety and depression in female high school students (Persian)]. Research in Cognitive and Behavioral Sciences. 2015; 4(2):89-102. [Link]
- Fu XL, Qian Y, Jin XH, Yu HR, Wu H, Du L, et al. Suicide rates among people with serious mental illness: A systematic review and meta-analysis. Psychological Medicine. 2023; 53(2):351-61.[DOI:10.1017/S0033291721001549] [PMID]
- Spanakis P, Peckham E, Mathers A, Shiers D, Gilbody S. The digital divide: Amplifying health inequalities for people with severe mental illness in the time of COVID-19. The British Journal of Psychiatry. 2021; 219(4):529-31. [DOI:10.1192/bjp.2021.56] [PMID]
- Torabi Z, Eghlima M, Khanke HR, Reza Soltani P. [Examine between family burden and family function (family with chronic neurosis children) (Persian)]. Social Welfare Quarterly. 2014; 13(51):133-49. [Link]
- Mojarad Kahani AH, Ghanabari Hashem Abadi BA. [The efficacy of group psycho educational interventions on family performance of patients with mood disorders (Persian)]. Journal of Family Counseling & Psychotherapy. 2012; 1(3):399-412. [Link]
- Akbari M, Alavi M, Irajpour A, Maghsoudi J. Challenges of family caregivers of patients with mental disorders in Iran: A narrative review. Iranian Journal of Nursing and Midwifery Research. 2018; 23(5):329-37. [DOI:10.4103/ijnmr.IJNMR_122_17] [PMID]
- Serlachius A, Badawy SM, Thabrew H. Psychosocial challenges and opportunities for youth with chronic health conditions during the COVID-19 pandemic. JMIR Pediatrics and Parenting. 2020; 3(2):e23057. [DOI:10.2196/23057] [PMID]
- Singh GP. Psychosocial and mental health issues of the migrants amidst covid-19 pandemic in India: A narrative review. Indian Journal of Psychological Medicine. 2021; 43(6):473-8. [DOI:10.1177/02537176211044802] [PMID]
- Momen NC, Plana-Ripoll O, Agerbo E, Benros ME, Børglum AD, Christensen MK, et al. Association between mental disorders and subsequent medical conditions. The New England Journal of Medicine. 2020; 382(18):1721-31. [DOI:10.1056/NEJMoa1915784] [PMID]
- De Hert M, Detraux J, Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues in Clinical Neuroscience. 2018; 20(1):31-40. [PMID]
- Vaghee S, Salarhaji A. [Stigma in family caregivers of patients with schizophrenia hospitalized in Ibn-Sina Psychiatric Hospital of Mashhad in 2014-2015 (Persian)]. Journal of Torbat Heydariyeh University of Medical Sciences. 2015; 3(3):23-30. [Link]
- Koschorke M, Padmavati R, Kumar S, Cohen A, Weiss HA, Chatterjee S, et al. Experiences of stigma and discrimination faced by family caregivers of people with schizophrenia in India. Social Science & Medicine. 2017; 178:66-77. [DOI:10.1016/j.socscimed.2017.01.061] [PMID]
- Jourshari RR, Aria AM, Alavizadeh SM, Entezari S, Hosseinkhanzadeh AA, Amirizadeh SM. Structural relationships between assertiveness and parenting styles with mediating self-esteem and anxiety of singleton children. Iranian Rehabilitation Journal. 2022; 20(4):539. [Link]
- Dolatfard A, Fathi M. [Experiences and challenges of families with mental disorders (Persian)]. Research Journal on Social Work. 2021; 8(27):97-124. [Link]
- Sadeghi M, Kaviani H, Rezai R. [Stigma of mental disorder among families of patients with major depressive disorder, bipolar disorder and schizophrenia (Persian)]. Journal of Advances in Cognitive Sciences. 2003; 5(2):16-25. [Link]
- Nouri Khajavi M, Ardeshirzadeh M, Doulatshahi B, Afgheh S. [Comparative evaluation of psychological burden in caregivers of patients with chronic schizophrenia and caregivers of patients with chronic bipolar disorder (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2008; 14(1 (52)):80-4. [Link]
- Thomas TL, Prasad Muliyala K, Jayarajan D, Angothu H, Thirthalli J. Vocational challenges in severe mental illness: A qualitative study in persons with professional degrees. Asian Journal of Psychiatry. 2019; 42:48-54. [DOI:10.1016/j.ajp.2019.03.011] [PMID]
- Folb N, Lund C, Fairall LR, Timmerman V, Levitt NS, Steyn K, et al. Socioeconomic predictors and consequences of depression among primary care attenders with non-communicable diseases in the Western Cape, South Africa: Cohort study within a randomised trial. BMC Public Health. 2015; 15:1194. [DOI:10.1186/s12889-015-2509-4] [PMID]
- Booysen D, Mahe-Poyo P, Grant R. The experiences and perceptions of mental health service provision at a primary health centre in the Eastern Cape. South African Journal of Psychiatry. 2021; 27:1641. [DOI:10.4102/sajpsychiatry.v27i0.1641] [PMID]
- Rose LE, Gerson L, Carbo C. Transitional care for seriously mentally ill persons: A pilot study. Archives of Psychiatric Nursing. 2007; 21(6):297-308. [DOI:10.1016/j.apnu.2007.06.010] [PMID]
- Velligan DI, Roberts DL, Sierra C, Fredrick MM, Roach MJ. What patients with severe mental illness transitioning from hospital to community have to say about care and shared decision-making. Issues in Mental Health Nursing. 2016; 37(6):400-5. [DOI:10.3109/01612840.2015.1132289] [PMID]
- Sarikhani Y, Bastani P, Rafiee M, Kavosi Z, Ravangard R. Key barriers to the provision and utilization of mental health services in low-and middle-income countries: A scope study. Community Mental Health Journal. 2021; 57:836-52. [DOI:10.1007/s10597-020-00619-2] [PMID]
- Battaglia AM, Mamak M, Goldberg JO. The impact of social media coverage on attitudes towards mental illness and violent offending. Journal of Community Psychology. 2022; 50(7):2938-49. [DOI:10.1002/jcop.22807] [PMID]
- Betton V, Borschmann R, Docherty M, Coleman S, Brown M, Henderson C. The role of social media in reducing stigma and discrimination. The British Journal of Psychiatry. 2015; 206(6):443-4. [DOI:10.1192/bjp.bp.114.152835] [PMID]
- Saha K, Torous J, Ernala SK, Rizuto C, Stafford A, De Choudhury M. A computational study of mental health awareness campaigns on social media. Translational Behavioral Medicine. 2019; 9(6):1197-207. [DOI:10.1093/tbm/ibz028] [PMID]
Type of Study: Original |
Subject:
Social Worker
Received: 2/11/2023 | Accepted: 15/04/2024 | Published: 1/10/2024
Received: 2/11/2023 | Accepted: 15/04/2024 | Published: 1/10/2024
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |