Volume 24, Issue 4 (Winter 2024)
jrehab 2024, 24(4): 458-471 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Morovati Z, Fatorehchy S, Hosseini S A. Treatment Priorities of Parents of Children With Cerebral Palsy: A Scoping Review. jrehab 2024; 24 (4) :458-471
URL: http://rehabilitationj.uswr.ac.ir/article-1-3253-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3253-en.html
1- Department of Occupational Therapy, Pediatric Neurorehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Occupational Therapy, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,alihosse@gmail.com
2- Department of Occupational Therapy, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Full-Text [PDF 2448 kb]
(1249 Downloads)
| Abstract (HTML) (7298 Views)
Full-Text: (15816 Views)
Introduction
Cerebral palsy (CP) refers to a group of non-progressive disorders in movement and posture that occur after a nerve injury and are accompanied by neurological and motor deficits, deformities, and functional limitations. In addition to movement and posture defects, these children suffer from sensory, perceptual, cognitive, communication, and behavioral problems, as well as epilepsy, causing limitations in individual actions and reducing participation in activities [1]. Occupational therapists use different methods to treat these children, such as neuro-developmental therapy, motor learning, and skill acquisition [2]. Also, depending on the existing needs, several approaches such as sensory integration therapy, transfer training approach, behavior approach (training and shaping behavior), forced restraint therapy, therapy using horses, and the vital and integrated tantric approach (VITA) method are used [3]. In most of these methods, evaluation and intervention are done based on the child’s abilities, but in some cases, the therapists do not estimate these children’s abilities correctly [4]. On the other hand, due to the full-time presence of the parents with the children and full knowledge of the condition, it seems necessary to cooperate between the therapist and the family and pay attention to the children’s priorities and needs for their comprehensive development. Also, the family’s participation in the evaluation and treatment process makes them active in obtaining useful information to improve daily life activities, participation, play, and other areas. Transferring learning from the treatment environment to the home and school environment is also done more easily [5].
One of the approaches used in occupational therapy is the family-centered approach, which encourages therapists and families to identify meaningful therapeutic goals and emphasizes a dynamic model of care that follows changes in the context, needs, and priorities of children and parents over time [6]. This approach encourages therapists and families to identify significant treatment goals [7]. This comprehensive attention also increases children’s satisfaction and improves their performance; therefore, in family-oriented occupational therapy, respect for clients and their participation in decision-making are essential treatment factors [8].
Another critical point is that parents have the most knowledge about their child, and this issue can help to set treatment goals in terms of functional levels that are more focused on the child’s participation and activity, facilitating the child’s participation in society and independence in everyday life [9]. Therefore, our study evaluates and combines different documents in the field of priorities and finally reaches the needs of children with cerebral palsy from the perspective of their parents in various age ranges and based on their motor function level. Examining different views of parents can encourage therapists to pay more attention to the family-centered approach. It will also help them find the area of work that needs the most treatment. And finally, considering that no study has been done in this field, it will help us to conduct more studies.
Materials and Methods
This scoping review method was compiled to obtain helpful background information and fill the gaps in the literature. In the current study, this method was used, presented by Arksey et al. [10] in 5 steps as follows:
Identification of the research questions
The present research questions were as follows: How many studies have been related to the treatment preferences of parents of children with cerebral palsy? What are the priorities reported in these studies?
Identification of related studies
To find related studies in English, PubMed, Scopus, OT seeker, and Google Scholar search engines were used to search English keywords: “Cerebral palsy”, “parents’ priority”, and “family needs”. The equivalent Persian keywords were searched in the SID database and the country’s medical sciences databases to search for Persian studies.
Selection of studies
The inclusion criteria included articles whose main topic was the treatment priorities of parents of children with cerebral palsy, published between 2000 and 2022 in English and Farsi. Since this study examines the treatment preferences of parents, considering the advancement of technology in the last two decades and changes in the process of education and treatment, examining parents’ preferences in articles before 2000 is unproductive. Therefore, the previous 22 years were considered as the search period. The exclusion criteria were review studies in languages other than English and Farsi.
Steps for selecting studies
After searching for relevant keywords, duplicate articles and studies whose titles did not match the inclusion criteria were removed. In the following step, the remaining articles were examined in full text. In the end, the studies that did not present an intervention or did not describe the implementation of the interventions were excluded.
Charting the data
At this stage, the flowchart of the research process was set, and the number of studies and their reasons were also discussed (Figure 1).

Summarizing and reporting the findings
After reviewing the full text of the articles in the results section, the studies were described based on the type of priorities and the factors that influenced them.
Results
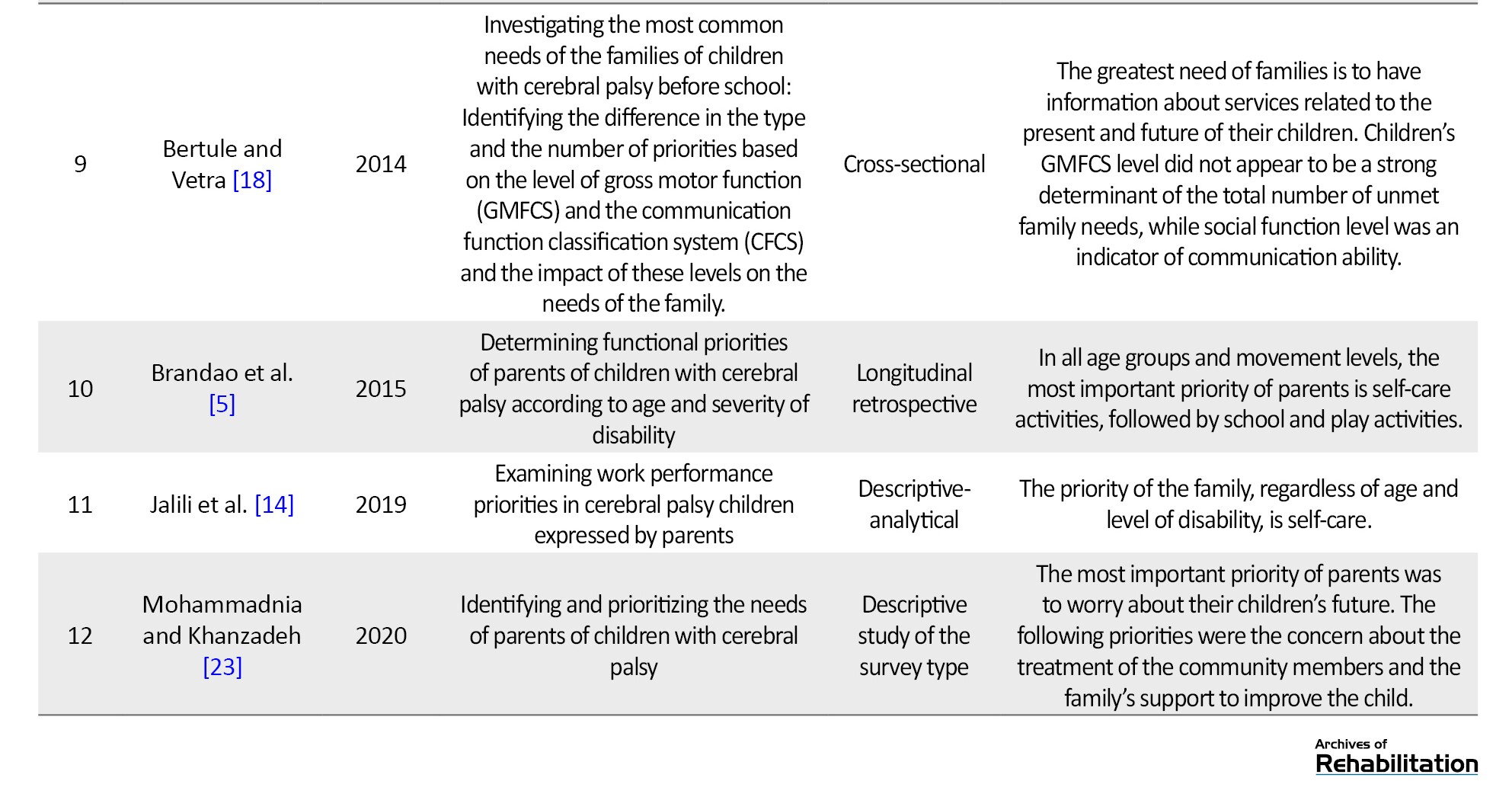
In the review of the mentioned databases, 104 articles were obtained, among which 12 studies matched the desired criteria and were subjected to final review and analysis (Table 1).
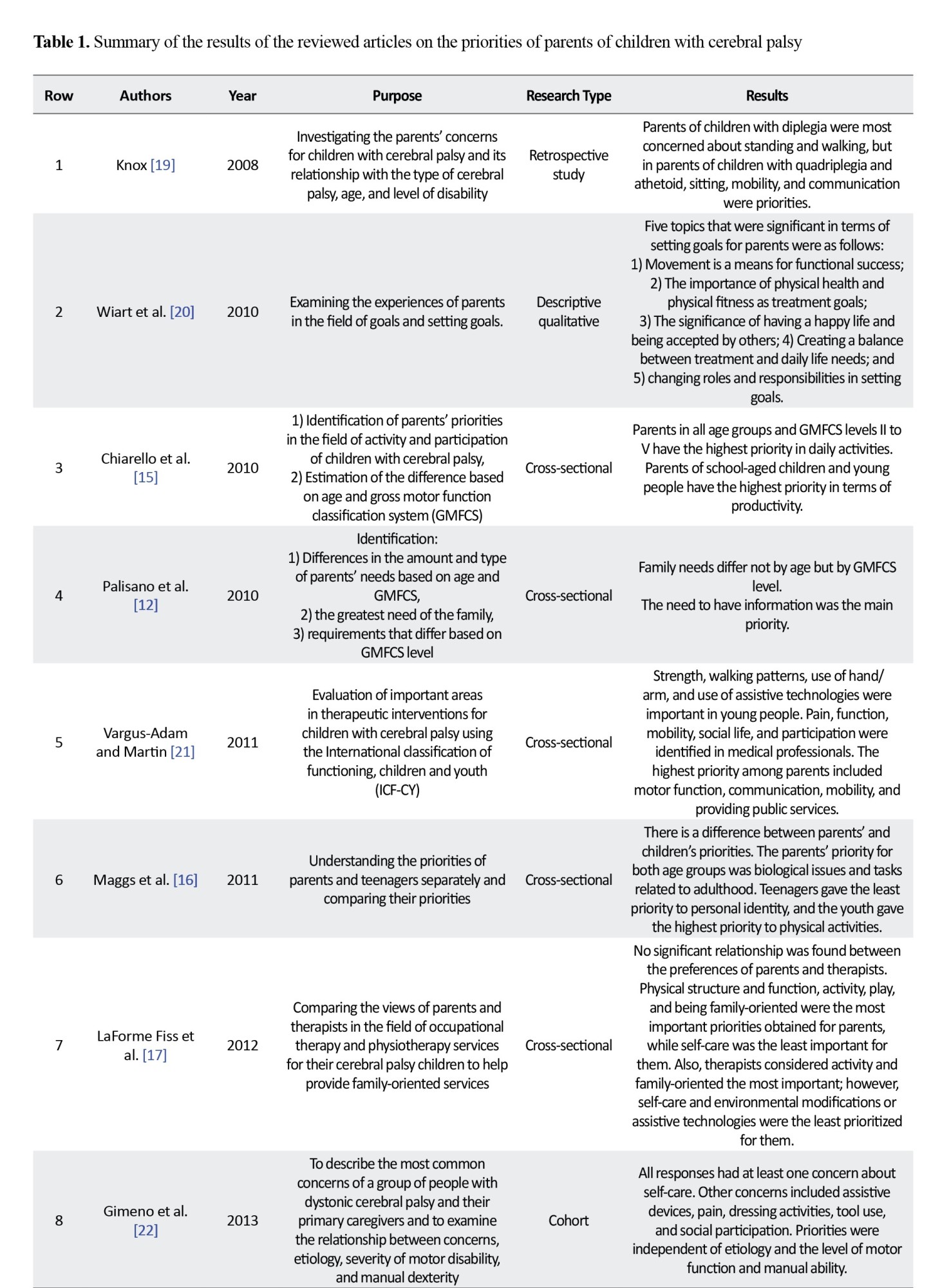
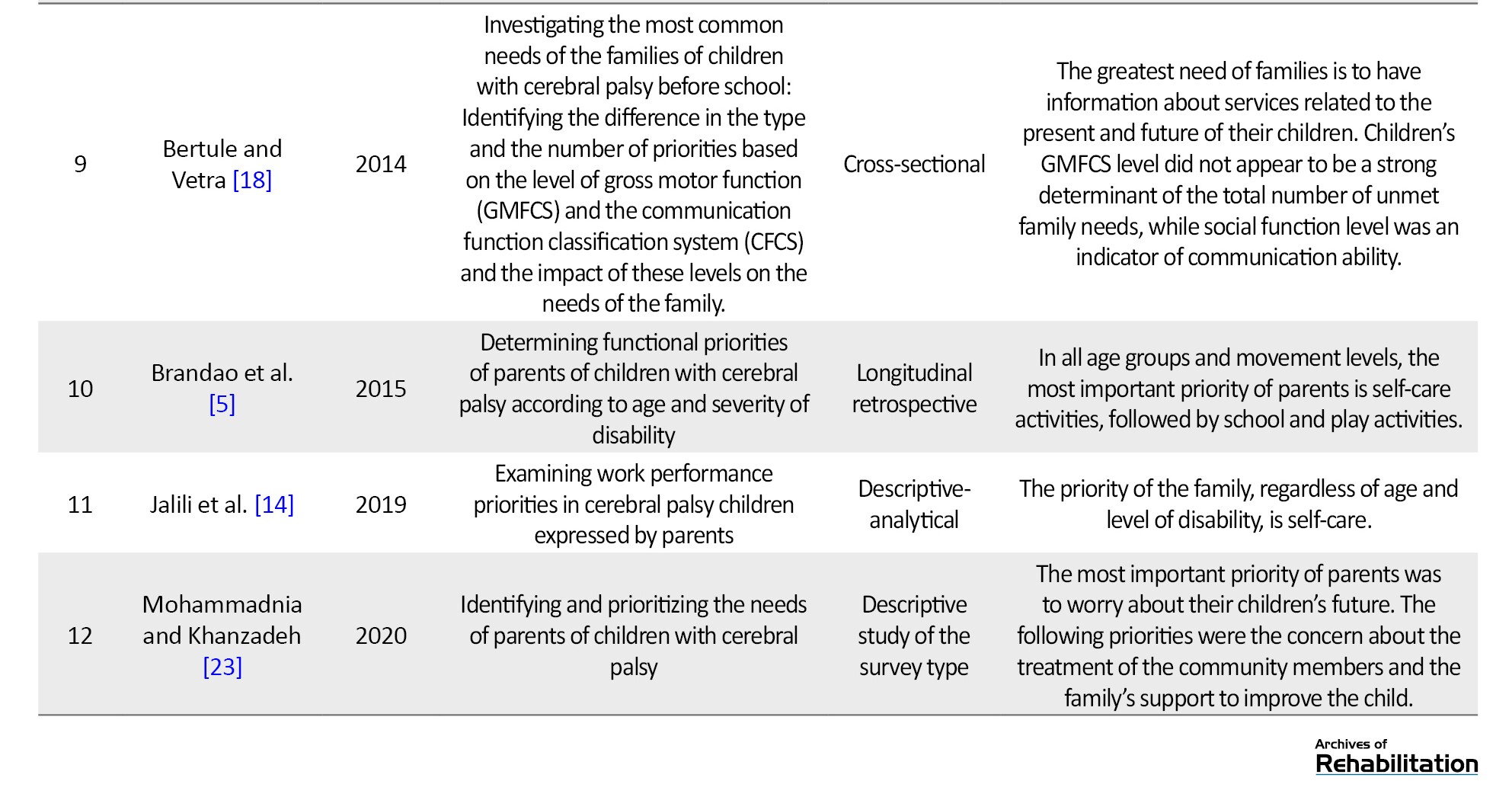
Occupational therapy employs different approaches; some are bottom-up, and some are top-down. Bottom-up approaches focus on body structures and body functions, while top-down approaches emphasize activities/participation [11]. Many occupational therapists do not prioritize top-down approaches to treatment and use bottom-up approaches that focus on the structures and components of disorders, while the primary goal of rehabilitation is to promote the child’s participation in essential contexts of life and treatment; steps should be taken in this direction [5]. So, it is essential for therapists to be aware of the child’s priorities and needs from the parent’s point of view. The evidence shows the importance of therapists’ and families’ cooperation to identify needs and coordinate their services [12]. The level of gross motor performance of children with cerebral palsy affects parents’ preferences. The level is determined by the gross motor function classification system (GMFCS). It is divided into five levels, where level I denotes the maximum independence and level V the minimum independence [13]. In a study conducted by Palisano et al. in 2009, it was found that the needs of families of children with cerebral palsy are highest in levels IV and V and lowest at levels I and II. In this research, more than 50% of parents expressed the need for information about the present and future of services, planning for the future, help identifying and locating social activities, and having more personal time [12]. Jalili et al. conducted a qualitative study to investigate work performance priorities in children with cerebral palsy from parents’ perspective using the Canadian occupation performance measure (COPM) in three areas: Self-care, productivity, and leisure time. They measured the parents’ priorities, indicating that regardless of the children’s gross motor level and age, personal care is the first important priority of the parents. The second most important priority, the only priority affecting the child’s gross motor function, is mobility. Both these priorities are in the field of self-care [14]. In the study by Brandao et al., which was conducted in 2014, the functional priorities of the parents of 75 children aged 3 to 16 with cerebral palsy were investigated. The data showed that, in general, the most functional needs were in the field of self-care activities, and only in the parents of children with severe motor impairment (level V) was the greatest need in the field of play [5]. Contrary to the mentioned studies, which were the same in almost all functional levels and at different ages, Chiarello et al. found that parents’ preferences for children with cerebral palsy differed depending on the level of gross motor performance and their age. However, self-care was the most important priority in all movement levels and ages. In particular, it can be stated that the parents of children with gross motor levels I, II, and III, as well as school-aged children and young people, showed the highest priority in being productive. Levels II to V also showed the highest priority in daily activities [15]. Maggs et al. conducted a study to compare the priorities of parents and their children, and regardless of the age of their children, parents had the greatest need in the field of life and tasks related to adults [16]. Although the results of most articles show the importance of self-care activities, in a study conducted by Fiss et al. in the field of comparing the priorities of parents and therapists of children with cerebral palsy in America, self-care activities were the least important factors for parents, while physical structure and function, activity, play, and being family-oriented were among the important priorities of their children’s treatment [17]. Also, in Bertule and Vetra’s study, the information about their children’s current and future services at all levels of movement was the most critical factor for parents, and this amount of attention can be related to the age range of 2- to 7-year-old children (before school). In the first years of diagnosis, parents are confused and seek to receive information mostly about their child’s recovery [18]. As a result, in addition to the movement levels, the child’s age is one of the factors influencing the parents’ priorities, which Knox studied in more detail. In this study, two peaks were recorded in the graph of parents’ concerns about their children’s standing and walking, who were 2 to 4 and 6 years old. Also, at 6 years and older, there is more concern for the deterioration of walking, which can result from increased muscle stiffness. In addition to age, different diagnoses and disability levels would affect priorities, showing each child’s uniqueness according to his special characteristics [19].
Discussion
Children with cerebral palsy need help to master life and meet their needs, and parents, as the first defenders of their children, should provide the necessary opportunities to improve their conditions. Suppose the therapists do not consider the parents’ priorities and needs. In that case, the anxiety caused by their efforts to meet the needs of their children will increase, which can affect their self-esteem and hinder the achievement of treatment goals [24]. Therefore, the present study was compiled to collect and summarize parents’ priorities for children with cerebral palsy. In the review of related articles, the highest priority raised by parents in all age groups and with each level of gross motor function was self-care activities. These personal care matters in childhood play a significant role in children’s independence and are one of the most important challenges for children with cerebral palsy and their parents [14]. Carrying out care activities requires the child’s mobility, which is one of the other obvious priorities of parents, and in fact, these two priorities are interdependent [20]. On the other hand, parents put forward complete information on current and future services as their priorities. In this regard, health professionals play a role in helping the family prepare for the key periods in the life of children with cerebral palsy [12].
Conclusion
Generally, based on the studies conducted in all age groups with different disabilities, parents’ highest priority and concern was in self-care activities, which shows the importance of independence and participation in individual life. Also, mobility is important for performing daily activities and gaining individual independence, so it is one of the most important priorities for parents, and it has been proposed as a means for functional success. Nevertheless, the concerns raised in assisting technologies and environmental reforms can indicate the desire to have independence and not necessarily mobility. In addition to the mentioned cases, parents need to be reassured about their children’s future, and in obtaining information in this direction, they have tried to reduce their level of concern. Due to this diversity in the results of different studies, therapists should pay attention to the priorities of the parents of these children, which are unique and reflect the needs of their children, to help increase the quality of life of these children to achieve appropriate treatment goals.
Ethical Considerations
Compliance with ethical guidelines
The present study is a review with no human or animal samples.
Funding
This research has not received financial support from funding organizations in different sectors.
Authors' contributions
Conceptualization: All authors; Methodology: Zahra Morovati and Saeid Fatorehchy; Research and review: Zahra Marvoti; Editing and finalization: Saeid Fatorehchy; Project supervision and management: Seyed Ali Hosseini and Saeid Fatorehchy.
Conflict of interest
The authors declared no conflict of interest.
References
Cerebral palsy (CP) refers to a group of non-progressive disorders in movement and posture that occur after a nerve injury and are accompanied by neurological and motor deficits, deformities, and functional limitations. In addition to movement and posture defects, these children suffer from sensory, perceptual, cognitive, communication, and behavioral problems, as well as epilepsy, causing limitations in individual actions and reducing participation in activities [1]. Occupational therapists use different methods to treat these children, such as neuro-developmental therapy, motor learning, and skill acquisition [2]. Also, depending on the existing needs, several approaches such as sensory integration therapy, transfer training approach, behavior approach (training and shaping behavior), forced restraint therapy, therapy using horses, and the vital and integrated tantric approach (VITA) method are used [3]. In most of these methods, evaluation and intervention are done based on the child’s abilities, but in some cases, the therapists do not estimate these children’s abilities correctly [4]. On the other hand, due to the full-time presence of the parents with the children and full knowledge of the condition, it seems necessary to cooperate between the therapist and the family and pay attention to the children’s priorities and needs for their comprehensive development. Also, the family’s participation in the evaluation and treatment process makes them active in obtaining useful information to improve daily life activities, participation, play, and other areas. Transferring learning from the treatment environment to the home and school environment is also done more easily [5].
One of the approaches used in occupational therapy is the family-centered approach, which encourages therapists and families to identify meaningful therapeutic goals and emphasizes a dynamic model of care that follows changes in the context, needs, and priorities of children and parents over time [6]. This approach encourages therapists and families to identify significant treatment goals [7]. This comprehensive attention also increases children’s satisfaction and improves their performance; therefore, in family-oriented occupational therapy, respect for clients and their participation in decision-making are essential treatment factors [8].
Another critical point is that parents have the most knowledge about their child, and this issue can help to set treatment goals in terms of functional levels that are more focused on the child’s participation and activity, facilitating the child’s participation in society and independence in everyday life [9]. Therefore, our study evaluates and combines different documents in the field of priorities and finally reaches the needs of children with cerebral palsy from the perspective of their parents in various age ranges and based on their motor function level. Examining different views of parents can encourage therapists to pay more attention to the family-centered approach. It will also help them find the area of work that needs the most treatment. And finally, considering that no study has been done in this field, it will help us to conduct more studies.
Materials and Methods
This scoping review method was compiled to obtain helpful background information and fill the gaps in the literature. In the current study, this method was used, presented by Arksey et al. [10] in 5 steps as follows:
Identification of the research questions
The present research questions were as follows: How many studies have been related to the treatment preferences of parents of children with cerebral palsy? What are the priorities reported in these studies?
Identification of related studies
To find related studies in English, PubMed, Scopus, OT seeker, and Google Scholar search engines were used to search English keywords: “Cerebral palsy”, “parents’ priority”, and “family needs”. The equivalent Persian keywords were searched in the SID database and the country’s medical sciences databases to search for Persian studies.
Selection of studies
The inclusion criteria included articles whose main topic was the treatment priorities of parents of children with cerebral palsy, published between 2000 and 2022 in English and Farsi. Since this study examines the treatment preferences of parents, considering the advancement of technology in the last two decades and changes in the process of education and treatment, examining parents’ preferences in articles before 2000 is unproductive. Therefore, the previous 22 years were considered as the search period. The exclusion criteria were review studies in languages other than English and Farsi.
Steps for selecting studies
After searching for relevant keywords, duplicate articles and studies whose titles did not match the inclusion criteria were removed. In the following step, the remaining articles were examined in full text. In the end, the studies that did not present an intervention or did not describe the implementation of the interventions were excluded.
Charting the data
At this stage, the flowchart of the research process was set, and the number of studies and their reasons were also discussed (Figure 1).

Summarizing and reporting the findings
After reviewing the full text of the articles in the results section, the studies were described based on the type of priorities and the factors that influenced them.
Results
In the review of the mentioned databases, 104 articles were obtained, among which 12 studies matched the desired criteria and were subjected to final review and analysis (Table 1).
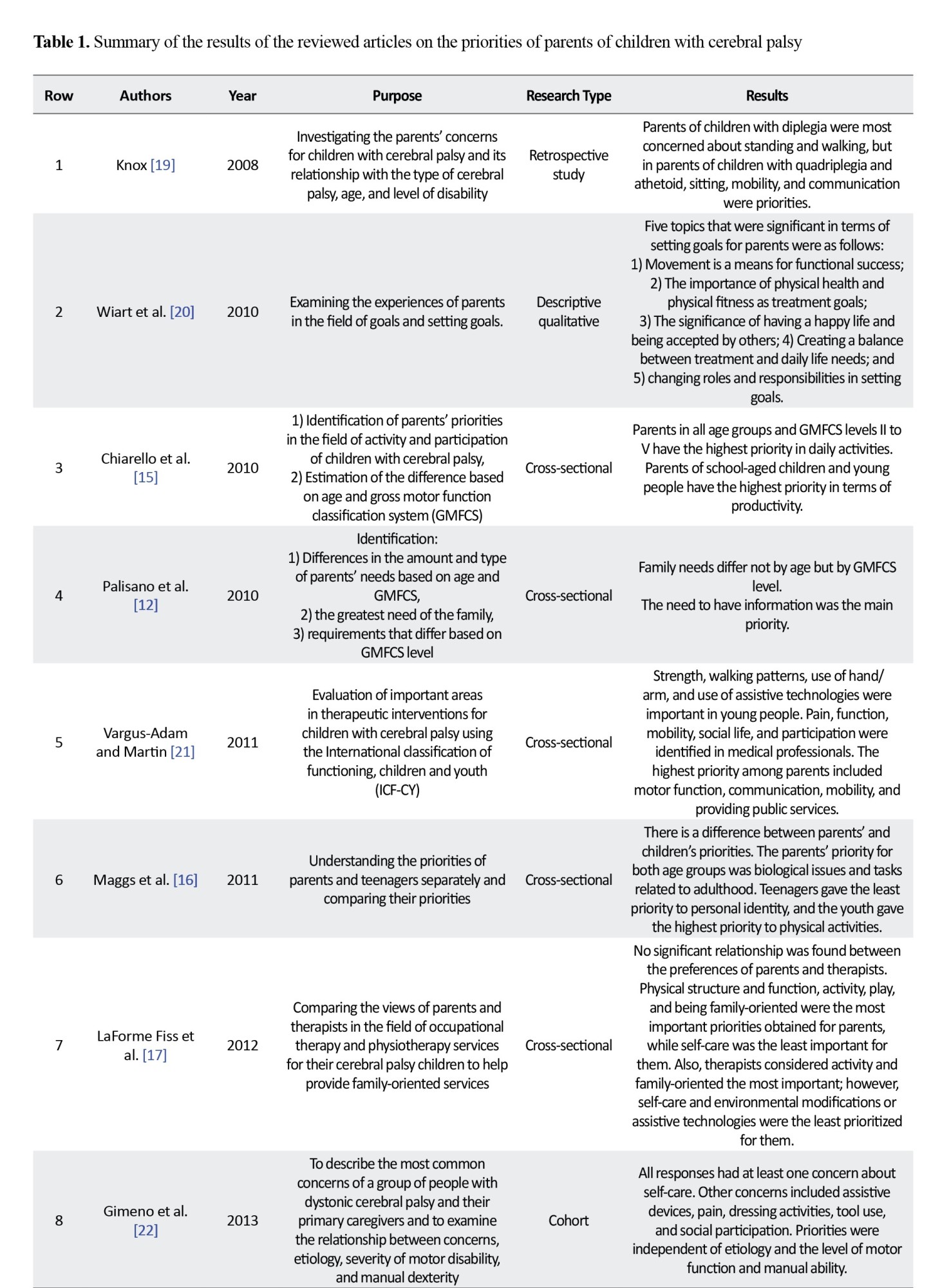
Occupational therapy employs different approaches; some are bottom-up, and some are top-down. Bottom-up approaches focus on body structures and body functions, while top-down approaches emphasize activities/participation [11]. Many occupational therapists do not prioritize top-down approaches to treatment and use bottom-up approaches that focus on the structures and components of disorders, while the primary goal of rehabilitation is to promote the child’s participation in essential contexts of life and treatment; steps should be taken in this direction [5]. So, it is essential for therapists to be aware of the child’s priorities and needs from the parent’s point of view. The evidence shows the importance of therapists’ and families’ cooperation to identify needs and coordinate their services [12]. The level of gross motor performance of children with cerebral palsy affects parents’ preferences. The level is determined by the gross motor function classification system (GMFCS). It is divided into five levels, where level I denotes the maximum independence and level V the minimum independence [13]. In a study conducted by Palisano et al. in 2009, it was found that the needs of families of children with cerebral palsy are highest in levels IV and V and lowest at levels I and II. In this research, more than 50% of parents expressed the need for information about the present and future of services, planning for the future, help identifying and locating social activities, and having more personal time [12]. Jalili et al. conducted a qualitative study to investigate work performance priorities in children with cerebral palsy from parents’ perspective using the Canadian occupation performance measure (COPM) in three areas: Self-care, productivity, and leisure time. They measured the parents’ priorities, indicating that regardless of the children’s gross motor level and age, personal care is the first important priority of the parents. The second most important priority, the only priority affecting the child’s gross motor function, is mobility. Both these priorities are in the field of self-care [14]. In the study by Brandao et al., which was conducted in 2014, the functional priorities of the parents of 75 children aged 3 to 16 with cerebral palsy were investigated. The data showed that, in general, the most functional needs were in the field of self-care activities, and only in the parents of children with severe motor impairment (level V) was the greatest need in the field of play [5]. Contrary to the mentioned studies, which were the same in almost all functional levels and at different ages, Chiarello et al. found that parents’ preferences for children with cerebral palsy differed depending on the level of gross motor performance and their age. However, self-care was the most important priority in all movement levels and ages. In particular, it can be stated that the parents of children with gross motor levels I, II, and III, as well as school-aged children and young people, showed the highest priority in being productive. Levels II to V also showed the highest priority in daily activities [15]. Maggs et al. conducted a study to compare the priorities of parents and their children, and regardless of the age of their children, parents had the greatest need in the field of life and tasks related to adults [16]. Although the results of most articles show the importance of self-care activities, in a study conducted by Fiss et al. in the field of comparing the priorities of parents and therapists of children with cerebral palsy in America, self-care activities were the least important factors for parents, while physical structure and function, activity, play, and being family-oriented were among the important priorities of their children’s treatment [17]. Also, in Bertule and Vetra’s study, the information about their children’s current and future services at all levels of movement was the most critical factor for parents, and this amount of attention can be related to the age range of 2- to 7-year-old children (before school). In the first years of diagnosis, parents are confused and seek to receive information mostly about their child’s recovery [18]. As a result, in addition to the movement levels, the child’s age is one of the factors influencing the parents’ priorities, which Knox studied in more detail. In this study, two peaks were recorded in the graph of parents’ concerns about their children’s standing and walking, who were 2 to 4 and 6 years old. Also, at 6 years and older, there is more concern for the deterioration of walking, which can result from increased muscle stiffness. In addition to age, different diagnoses and disability levels would affect priorities, showing each child’s uniqueness according to his special characteristics [19].
Discussion
Children with cerebral palsy need help to master life and meet their needs, and parents, as the first defenders of their children, should provide the necessary opportunities to improve their conditions. Suppose the therapists do not consider the parents’ priorities and needs. In that case, the anxiety caused by their efforts to meet the needs of their children will increase, which can affect their self-esteem and hinder the achievement of treatment goals [24]. Therefore, the present study was compiled to collect and summarize parents’ priorities for children with cerebral palsy. In the review of related articles, the highest priority raised by parents in all age groups and with each level of gross motor function was self-care activities. These personal care matters in childhood play a significant role in children’s independence and are one of the most important challenges for children with cerebral palsy and their parents [14]. Carrying out care activities requires the child’s mobility, which is one of the other obvious priorities of parents, and in fact, these two priorities are interdependent [20]. On the other hand, parents put forward complete information on current and future services as their priorities. In this regard, health professionals play a role in helping the family prepare for the key periods in the life of children with cerebral palsy [12].
Conclusion
Generally, based on the studies conducted in all age groups with different disabilities, parents’ highest priority and concern was in self-care activities, which shows the importance of independence and participation in individual life. Also, mobility is important for performing daily activities and gaining individual independence, so it is one of the most important priorities for parents, and it has been proposed as a means for functional success. Nevertheless, the concerns raised in assisting technologies and environmental reforms can indicate the desire to have independence and not necessarily mobility. In addition to the mentioned cases, parents need to be reassured about their children’s future, and in obtaining information in this direction, they have tried to reduce their level of concern. Due to this diversity in the results of different studies, therapists should pay attention to the priorities of the parents of these children, which are unique and reflect the needs of their children, to help increase the quality of life of these children to achieve appropriate treatment goals.
Ethical Considerations
Compliance with ethical guidelines
The present study is a review with no human or animal samples.
Funding
This research has not received financial support from funding organizations in different sectors.
Authors' contributions
Conceptualization: All authors; Methodology: Zahra Morovati and Saeid Fatorehchy; Research and review: Zahra Marvoti; Editing and finalization: Saeid Fatorehchy; Project supervision and management: Seyed Ali Hosseini and Saeid Fatorehchy.
Conflict of interest
The authors declared no conflict of interest.
References
- Morris C. Definition and classification of cerebral palsy: A historical perspective. Developmental Medicine and Child Neurology. 2007; 109:3-7. [DOI:10.1111/j.1469-8749.2007.tb12609.x] [PMID]
- Schell B, Gillen G. Willard and Spackman’s occupational therapy. Alphen aan den Rijn: Wolters Kluwer Health; 2003. [Link]
- Patel DR. Therapeutic interventions in cerebral palsy. Indian Journal of Pediatrics. 2005; 72(11):979-83. [DOI:10.1007/BF02731676] [PMID]
- Spencer J, Krefting L, Mattingly C. Incorporation of ethnographic methods in occupational therapy assessment. The American Journal of Occupational Therapy. 1993; 47(4):303-9. [DOI:10.5014/ajot.47.4.303] [PMID]
- Brandão MB, Oliveira RH, Mancini MC. Functional priorities reported by parents of children with cerebral palsy: Contribution to the pediatric rehabilitation process. Brazilian Journal of Physical Therapy. 2014; 18(6):563-71. [DOI:10.1590/bjpt-rbf.2014.0064][PMID]
- Rosenbaum P, King S, Law M, King G, Evans J. Family-centred service: A conceptual framework and research review. In: Law M, editor. Family-centred assessment and intervention in pediatric rehabilitation. Milton Park: Routledge; 2014. [Link]
- Darrah J, Law M, Pollock N. Family-centered functional therapy-a choice for children with motor dysfunction. Infants & Young Children. 2001; 13(4):79-87. [DOI:10.1097/00001163-200113040-00014]
- King S, Teplicky R, King G, Rosenbaum P. Family-centered service for children with cerebral palsy and their families: A review of the literature. Seminars in Pediatric Neurology. 2004; 11(1):78-86. [DOI:10.1016/j.spen.2004.01.009] [PMID]
- Law M, Darrah J, Pollock N, Rosenbaum P, Russell D, Walter SD, et al. Focus on function - a randomized controlled trial comparing two rehabilitation interventions for young children with cerebral palsy. BMC Pediatrics. 2007; 7:31. [DOI:10.1186/1471-2431-7-31] [PMID]
- Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005; 8(1):19-32. [DOI:10.1080/1364557032000119616]
- Trombly C. Anticipating the future: Assessment of occupational function. The American Journal of Occupational Therapy. 1993; 47(3):253-7. [DOI:10.5014/ajot.47.3.253] [PMID]
- Palisano RJ, Almarsi N, Chiarello LA, Orlin MN, Bagley A, Maggs J. Family needs of parents of children and youth with cerebral palsy. Child. 2010; 36(1):85-92. [DOI:10.1111/j.1365-2214.2009.01030.x] [PMID]
- Morris C, Kurinczuk JJ, Fitzpatrick R, Rosenbaum PL. Who best to make the assessment? Professionals' and families' classifications of gross motor function in cerebral palsy are highly consistent. Archives of Disease in Childhood. 2006; 91(8):675-9. [DOI:10.1136/adc.2005.090597] [PMID]
- Jalili N, Nasr Z, Zare R, Sattari M, Hosseini A. [Occupational performance priorities of children with cerebral palsy from the parents’ perspective (Persian)]. Archives of Rehabilitation. 2019; 19(4):370-9. [DOI:10.32598/rj.19.4.370]
- Chiarello LA, Palisano RJ, Maggs JM, Orlin MN, Almasri N, Kang LJ, et al. Family priorities for activity and participation of children and youth with cerebral palsy. Physical Therapy. 2010; 90(9):1254-64. [DOI:10.2522/ptj.20090388] [PMID]
- Maggs J, Palisano R, Chiarello L, Orlin M, Chang HJ, Polansky M. Comparing the priorities of parents and young people with cerebral palsy. Disability and Rehabilitation. 2011; 33(17-18):1650-8. [DOI:10.3109/09638288.2010.542875] [PMID]
- LaForme Fiss AC, McCoy SW, Chiarello LA; Move Play Study Team. Comparison of family and therapist perceptions of physical and occupational therapy services provided to young children with cerebral palsy. Physical & Occupational Therapy in Pediatrics. 2012; 32(2):210-26. [DOI:10.3109/01942638.2011.619250] [PMID]
- Bertule D, Vetra A. The family needs of parents of preschool children with cerebral palsy: The impact of child's gross motor and communications functions. Medicina. 2014; 50(6):323-8.[DOI:10.1016/j.medici.2014.11.005] [PMID]
- Knox V. Do parents of children with cerebral palsy express different concerns in relation to their child’s type of cerebral palsy, age and level of disability? Physiotherapy. 2008; 94(1):56-62. [DOI:10.1016/j.physio.2007.04.005]
- Wiart L, Ray L, Darrah J, Magill-Evans J. Parents' perspectives on occupational therapy and physical therapy goals for children with cerebral palsy. Disability and Rehabilitation. 2010; 32(3):248-58. [DOI:10.3109/09638280903095890] [PMID]
- Vargus-Adams JN, Martin LK. Domains of importance for parents, medical professionals and youth with cerebral palsy considering treatment outcomes. Child. 2011; 37(2):276-81. [DOI:10.1111/j.1365-2214.2010.01121.x] [PMID]
- Gimeno H, Gordon A, Tustin K, Lin JP. Functional priorities in daily life for children and young people with dystonic movement disorders and their families. European Journal of Paediatric Neurology. 2013; 17(2):161-8. [DOI:10.1016/j.ejpn.2012.07.007] [PMID]
- Mohammadnia M, Hosseinkhanzadeh AA. Identifying and prioritizing the needs of parents of children with cerebral palsy. Quarterly Journal of Child Mental Health. 2020; 7(1):181-92. [DOI:10.29252/jcmh.7.1.16]
- Russell F. Starting school: The importance of parents’ expectations. Journal of Research in Special Educational Needs. 2005; 5(3):118-26. [DOI:10.1111/j.1471-3802.2005.00051.x]
Type of Study: Systematic Review |
Subject:
Occupational Therapy
Received: 27/01/2023 | Accepted: 6/06/2023 | Published: 1/01/2024
Received: 27/01/2023 | Accepted: 6/06/2023 | Published: 1/01/2024
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |