Volume 24, Issue 1 (Spring 2023)
jrehab 2023, 24(1): 114-131 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hasanvand A, Darouie A, Aghadoost S, Dabirmoghaddam P, Bakhshi E. The Study of Vocal Function in Patients With Early Laryngeal Carcinoma After Transoral Laser Microsurgery. jrehab 2023; 24 (1) :114-131
URL: http://rehabilitationj.uswr.ac.ir/article-1-3153-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3153-en.html
Arezoo Hasanvand1 

 , Akbar Darouie *2
, Akbar Darouie *2 

 , Samira Aghadoost3
, Samira Aghadoost3 

 , Payman Dabirmoghaddam4
, Payman Dabirmoghaddam4 

 , Enayatollah Bakhshi5
, Enayatollah Bakhshi5 




 , Akbar Darouie *2
, Akbar Darouie *2 

 , Samira Aghadoost3
, Samira Aghadoost3 

 , Payman Dabirmoghaddam4
, Payman Dabirmoghaddam4 

 , Enayatollah Bakhshi5
, Enayatollah Bakhshi5 


1- Department of Speech Therapy, University of Social Welfare and Rehabilitation Sciences Tehran, Iran., Speech Therapy Department, University of Social Welfare and Rehabilitation Sciences, kodakyar Ave., daneshjo Blvd., Evin, Tehran, Iran.
2- Department of Speech Therapy, University of Social Welfare and Rehabilitation Sciences Tehran, Iran. ,adarouie@hotmail.com
3- Department of Speech Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran., Speech Therapy Department, School of Rehabilitation, Safi Alishah Rd, Pich-e-Shemiran, Enghelab St, Tehran, Iran
4- Otolaryngology Research Center, Tehran University of Medical Sciences, Tehran, Iran., Otolaryngology and head and neck surgery ward, Amir A’lam Hospital, Sa'adi Shomali St, Tehran, Iran.
5- Department of Biostatistics and Epidemiology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran., Biostatistics and Epidemiology Department, University of Social Welfare and Rehabilitation Sciences, kodakyar Ave., daneshjo Blvd., Evin, Tehran, Iran.
2- Department of Speech Therapy, University of Social Welfare and Rehabilitation Sciences Tehran, Iran. ,
3- Department of Speech Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran., Speech Therapy Department, School of Rehabilitation, Safi Alishah Rd, Pich-e-Shemiran, Enghelab St, Tehran, Iran
4- Otolaryngology Research Center, Tehran University of Medical Sciences, Tehran, Iran., Otolaryngology and head and neck surgery ward, Amir A’lam Hospital, Sa'adi Shomali St, Tehran, Iran.
5- Department of Biostatistics and Epidemiology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran., Biostatistics and Epidemiology Department, University of Social Welfare and Rehabilitation Sciences, kodakyar Ave., daneshjo Blvd., Evin, Tehran, Iran.
Full-Text [PDF 1964 kb]
(1411 Downloads)
| Abstract (HTML) (4577 Views)
Full-Text: (2524 Views)
Introduction
Cancers of the head and neck area are considered to be the most common malignancies of the body [1], and among its different types, it is particularly essential to pay attention to the involvement of the larynx area as the vital structure of the swallowing-respiratory system [2]. Statistics show that this type of cancer accounts for approximately 30% of all head and neck malignancies and 1% of all cancers, especially in the sixth and seventh decades of men’s lives [3, 4]. This complication is shown in the form of irregular white or red localized thickenings in the videolaryngoscopy evaluation of microscopic manifestations, and based on the American Joint Committee on Cancer (AJCC) classification known as tumor node metastasis staging system (TNM), is divided into two growth stages consisting of early cancer (tumor size 0, I and II) and advanced laryngeal cancer (tumor size III and IV) [7]. After the appearance of the first clinical manifestations, the main goal and the first line of treatment measures in the medical field is to prevent progress, remove cancer cells and save the person’s life; for this purpose, oncological treatments designed for patients with laryngeal cancer include a variety of surgical methods, radiation, and chemotherapy [8, 9] and in case of disease progression and to achieve the maximum result, a combination of the mentioned methods is prescribed for the disease control [10].
Studies show that in the early stages of disease progression, CO2 transoral laser microsurgery (CO2 TLM) is considered as one of the first options in the treatment of this complication due to fewer complications and a significant success rate of disease control [11]. While the clinical evidence of the voice field shows the spectrum experience of different severities of voice disorders in people treated with transoral laser microsurgery [14, 15], the evaluation of its different angles highly helps in choosing an approach appropriate to the individual’s conditions and providing timely voice rehabilitation courses and programs to experts in this field.
In this regard, the proposed program resulting from the joint meeting of European laryngological society (ELS) considers the comprehensive evaluation of vocal function dependent on the combined use of objective, subjective analyzes and self-perceived evaluations [18]. Among the different types of voice evaluations, acoustic analysis of voice signal samples has become an essential component in the evaluation of vocal function during the last few decades due to easy application, repeatability, non-invasiveness, quantification, and objectivity [19]. The voice handicap index (VHI) questionnaire is also one of the most widely used self-reporting tools that examine psycho-social results and a sense of disability caused by voice disorders in different physical, emotional, and functional dimensions from the patient’s point of view [29].
Regarding laryngeal cancer, the description and comparison of vocal characteristics of patients at different levels of disease progression and the evaluation of the correlation between objective evaluations and different instruments for measuring the voice-related quality of life (QoL) has been the subject of a limited number of studies. For example, the findings of Carlsen et al.’s study on 229 patients with various voice disorders, including laryngeal cancer, also show a correlation between voice handicap index and jitter, shimmer, and harmonic-to-noise ratio (HNR) parameters in this group [36].
The present study, by understanding the need for a comprehensive evaluation of voice characteristics and considering the complex nature of voice disorders, the knowledge gap, the unique features and the distinct structure of the Persian language and culture, using acoustic analysis and the voice handicap index, investigates the vocal quality, the existence of a correlation between objective evaluations and the perception of patients with early laryngeal cancers after transoral laser microsurgery and compares the findings obtained from the voice quality of healthy individuals so that it can be useful for researchers and therapists in this field by creating a clear picture of the vocal status of patients after the completion of oncological treatment courses.
Materials and Methods
The current research is a descriptive, correlational, and comparative study that was conducted cross-sectionally on 120 participants aged 18 to 65 years (with Mean±SD of age 51.72±8.681) in the form of two groups with laryngeal cancer and controls. The patient sample included 60 men with early laryngeal cancer and undergoing transoral laser mirosurgery, who were selected according to the inclusion criteria by the convenience sampling method in the routine visit of people referring to the ear, nose and throat clinic of Amir A'lam Hospital Complex. The control sample also included 60 men with normal voice quality, which was prepared by convinince sampling from healthy people of the population.
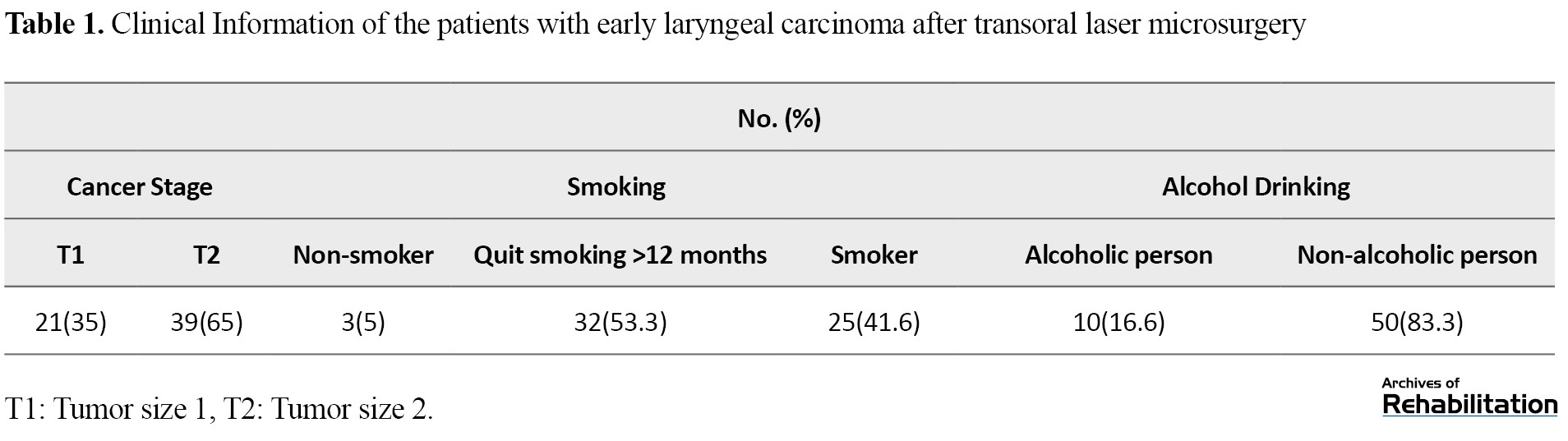
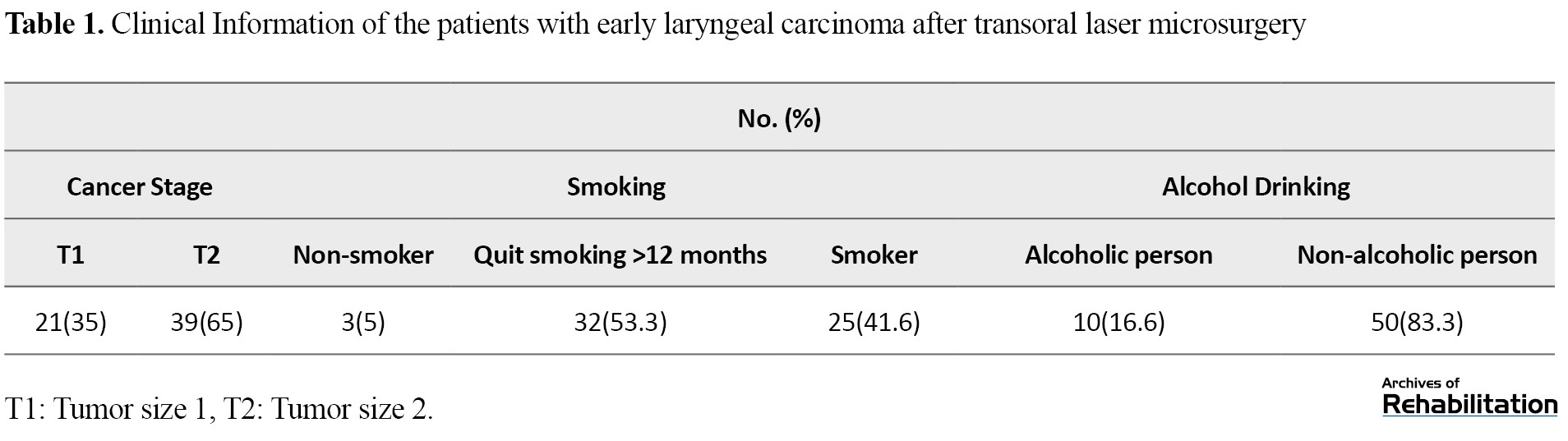
In this study, the inclusion criteria of subjects in the patient group included people who had undergone transoral laser microsurgery in glottis area due to early laryngeal cancer. It should be noted that in the present study, the characteristics of the lesion (including the stage and characteristics of the primary tumor) were determined according to the diagnosis of the ear, nose and throat specialist based on the TNM staging system [37] and based on the consensus of the results of direct laryngoscopy evaluation and the written report of the pathology laboratory from the biopsy of the lesion. The selection criteria for the control group included Farsi-speaking, no speech and language disorders, no history of any surgery in the head and neck area, and the presence of normal voice quality based on the perceptual judgment of a speech and language pathologist. In addition, in both groups, the exclusion criteria included a distortion of voice samples and the participants’ unwillingness to cooperate. Table 1 presents other clinical information of participants with early laryngeal carcinoma.
In this study, to collect acoustic data from the analysis of the signal obtained from 3-5 s of continuous stretching of the vowel /a/ by jitter, shimmer, HNR fundamental frequency, fundamental frequency and the Cepstral peak prominence smoothed (CPPS) in Praat software, version 1.6.49 was used. In this way, after understanding the process and practicing the test related to sampling, the voice of the people were recorded using a voice recorder (Zoom brand model H1n with a sampling rate of 24 bits/96 kHz) at an angle of 45 degrees and a distance of 10 cm to the mouth of the participants in WAV format. It should be noted that the data related to the CPPS parameter was extracted according to the settings suggested by Fadke [39]. Then, the Persian version with 30 items of the voice voice handicap index was provided to the participants, and how to complete the questionnaire was explained.
In the present study, data were analyzed using SPSS software, version 20. Also, using the results of Kolmogorov Smirnov test, it was found that the data follow the normal distribution. Then, descriptive statistics, including calculation of central tendency and dispersion indices, independent t-test for between-group comparison and Pearson correlation test were used to examine intragroup relationships of the studied variables at a significance level of less than 0.05.
Results
This research was conducted with 120 male participants in the form of two groups of patients (60 people) and control (60 people). Table 2 presents the age information of the participants.
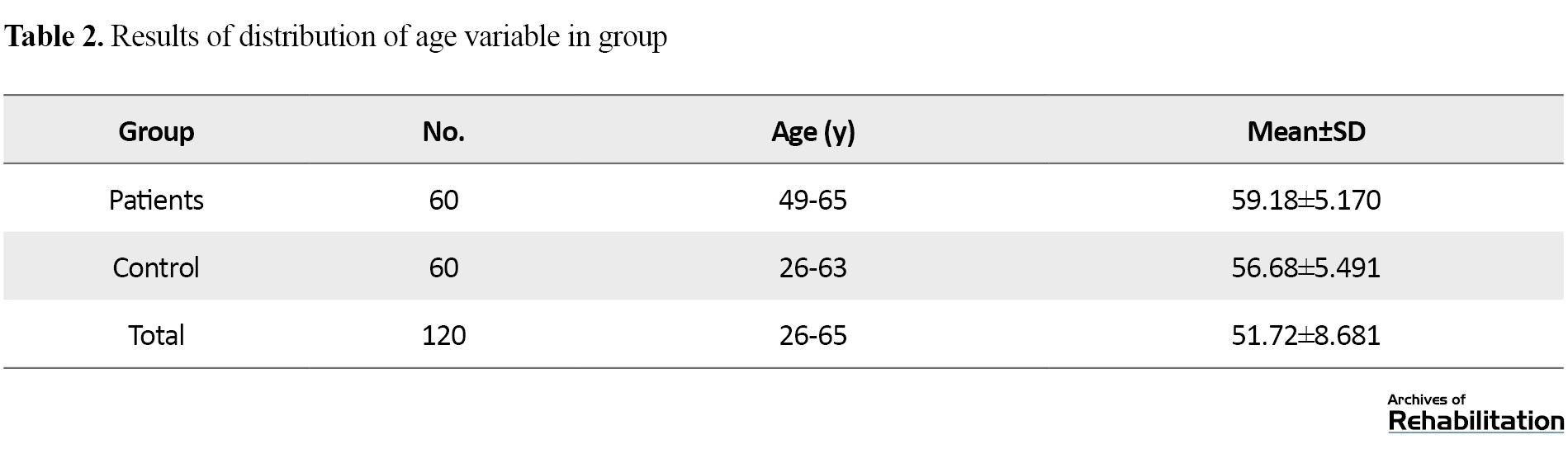
According to the descriptive findings in Table 2, the Mean±SD of the age of the patient group was 59.18±5.170 and the control group was 56.68±5.491 years. Table 3 also reports the results of the between-group comparison of acoustic parameter values.
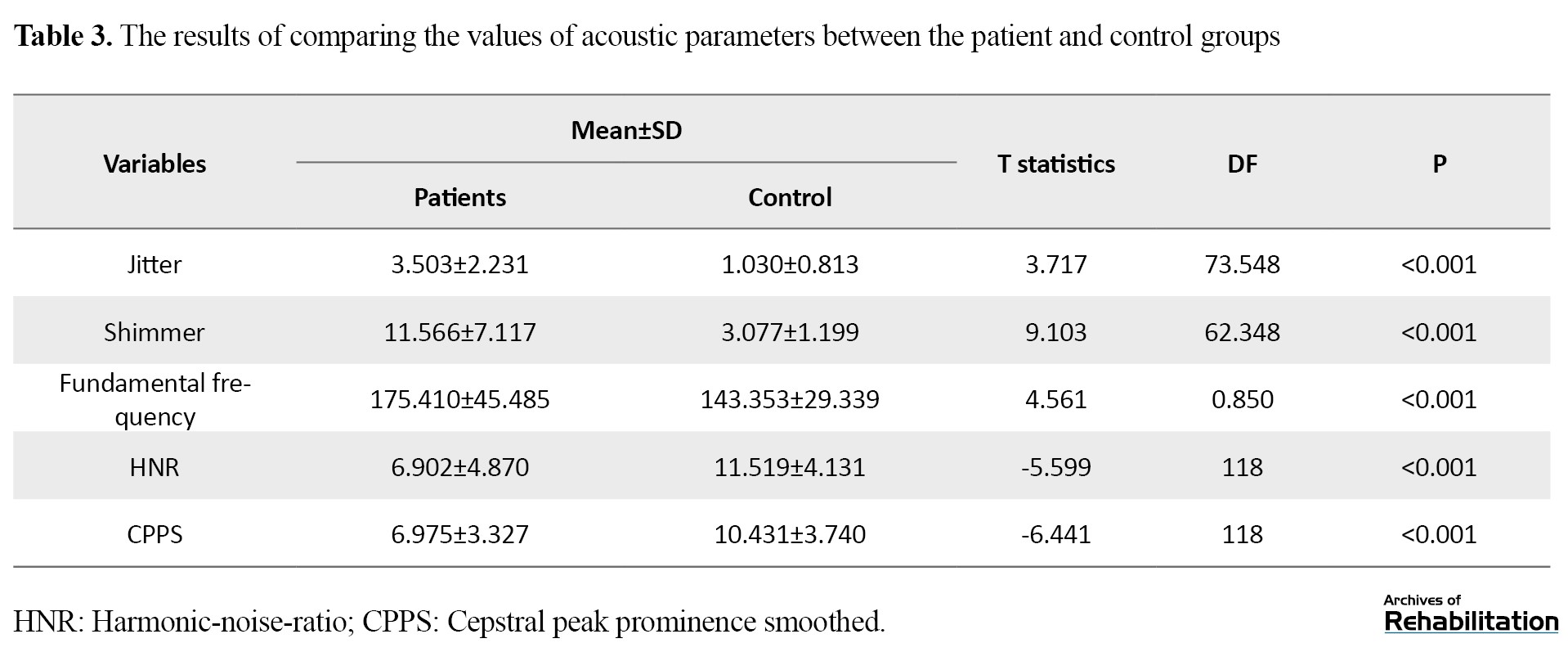
Based on the findings of the above table, the mean values of acoustic analysis parameters, including jitter, shimmer and fundamental frequency of the patient group are significantly higher compared to the control group (P<0.001). Also, the mean values of the parameters of the HNR and the CPPS of the subjects undergoing transoral laser microsurgery were lower than healthy subjects of the control group, and these differences are also statistically significant (P<0.001). Table 4 presents the results of the comparison of the mean total score and the scores of functional, physical and emotional subscales.
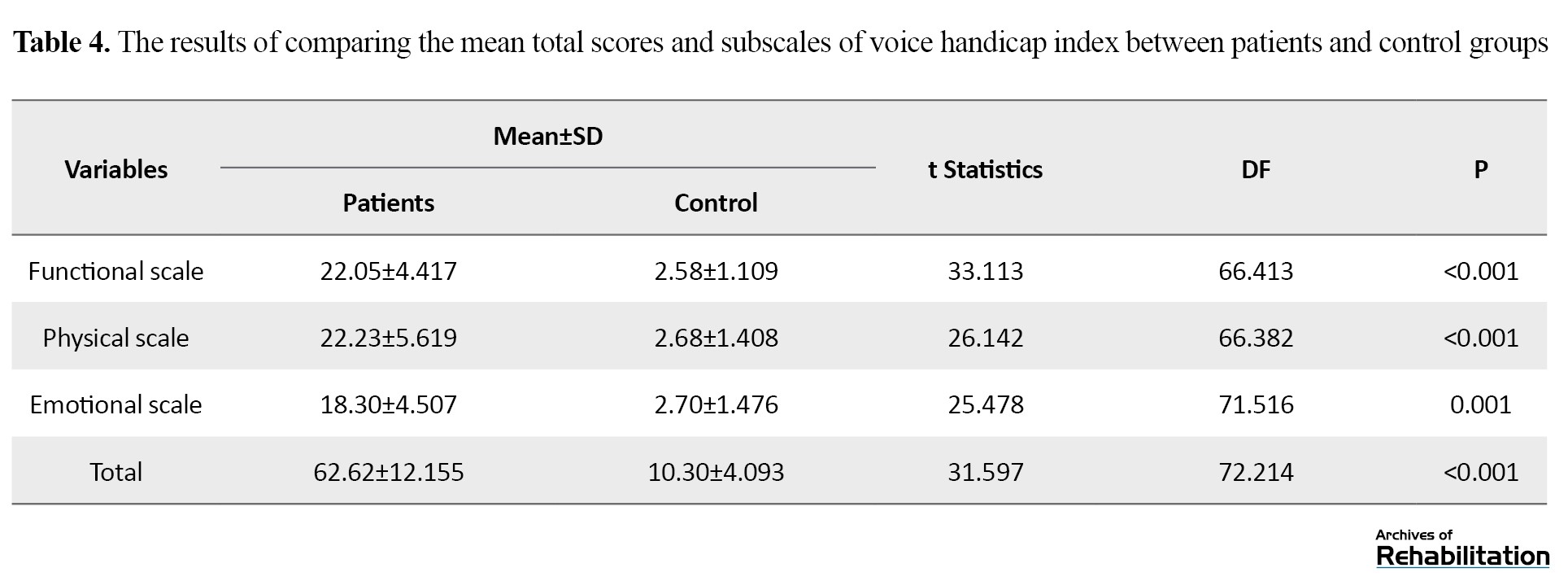
The results of the between-group comparison of the VHI average and its subscales in the above table show a statistically significant difference between the patient and control groups (P<0.001). Table 5 presents the results of the correlation between the acoustic parameters with the total score and the scores of the subscales of the voice handicap index in the patient group.
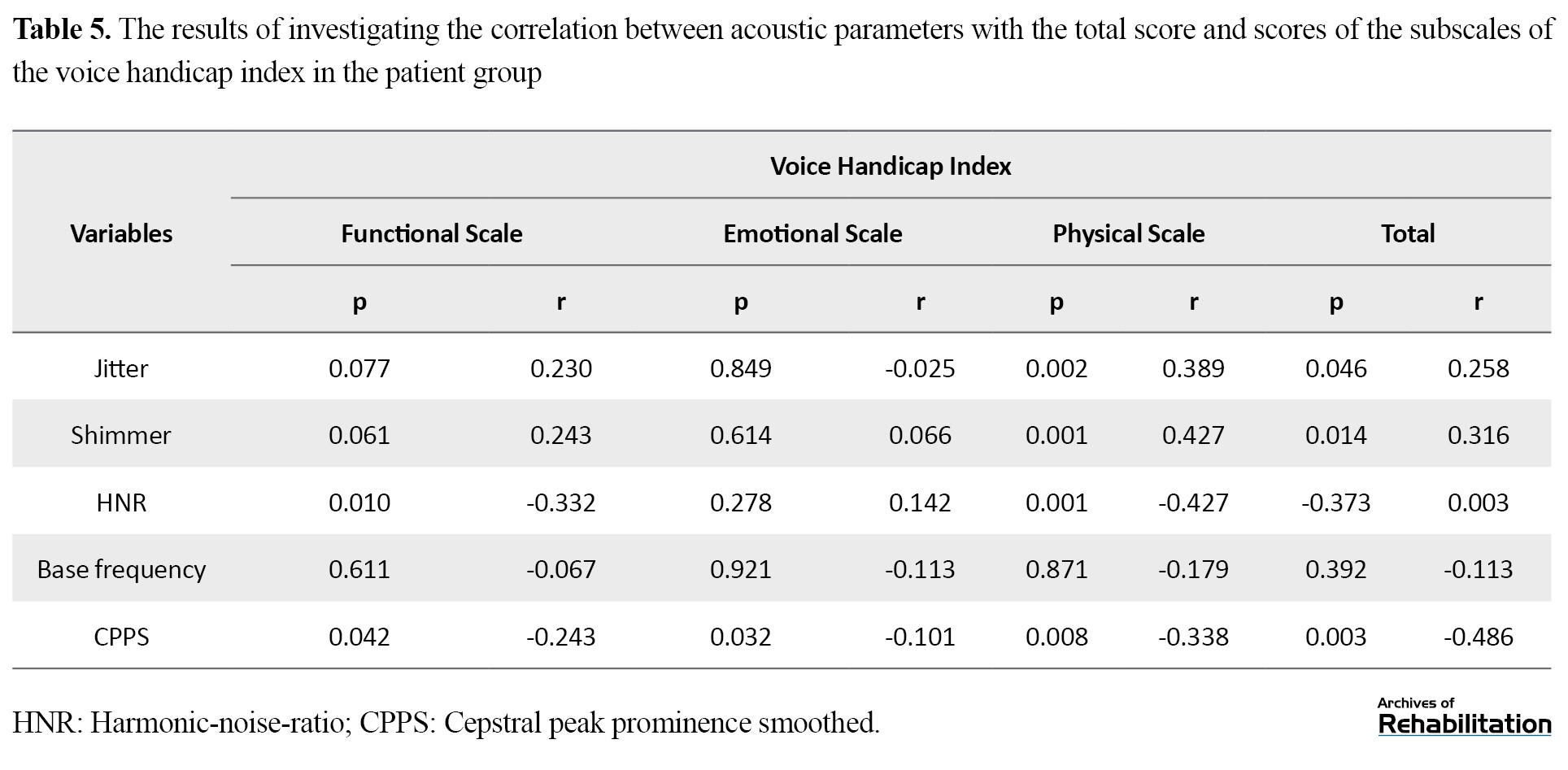
As mentioned, Pearson’s correlation coefficient was used to know the relationships between research variables in the patient group; the results indicated a direct and significant correlation between the jitter parameter and the total score (r=0.258 and P=0.046) and physical subscale scores (r=0.389 and P=0.002) of the voice handicap index. The same results were repeated regarding Shimmer and it was found that this parameter has a direct correlation with the total score (r=0.316 and P=0.014) and the physical subscale score (r=0.427 and P=0.001) of VHI. The HNR parameter has an inverse, weak and significant relationship with the total score (r=0.003 and P=-0.373) and the scores of physical (r=-0.427 and P=0.001) and functional (r=-0.332 and P=-0.010). Also, the CPPS parameter has an inverse and significant relationship with the total score (r=-0.486 and P=0.003) and the scores of three functional (r=-0.243 and P=0.042), physical (r=-0.338 and P=0.008) and emotional (r=0.486 and P=0.003) subscales of voice handicap index. On the other hand, according to the results of the correlation test, no significant relationship (P<0.05) was observed between the fundamental frequency and the subscales of the voice handicap index (Table 5). Table 6 presents the results of the correlation between the acoustic parameters with the total score and the scores of the subscales of the voice handicap index in the control group.
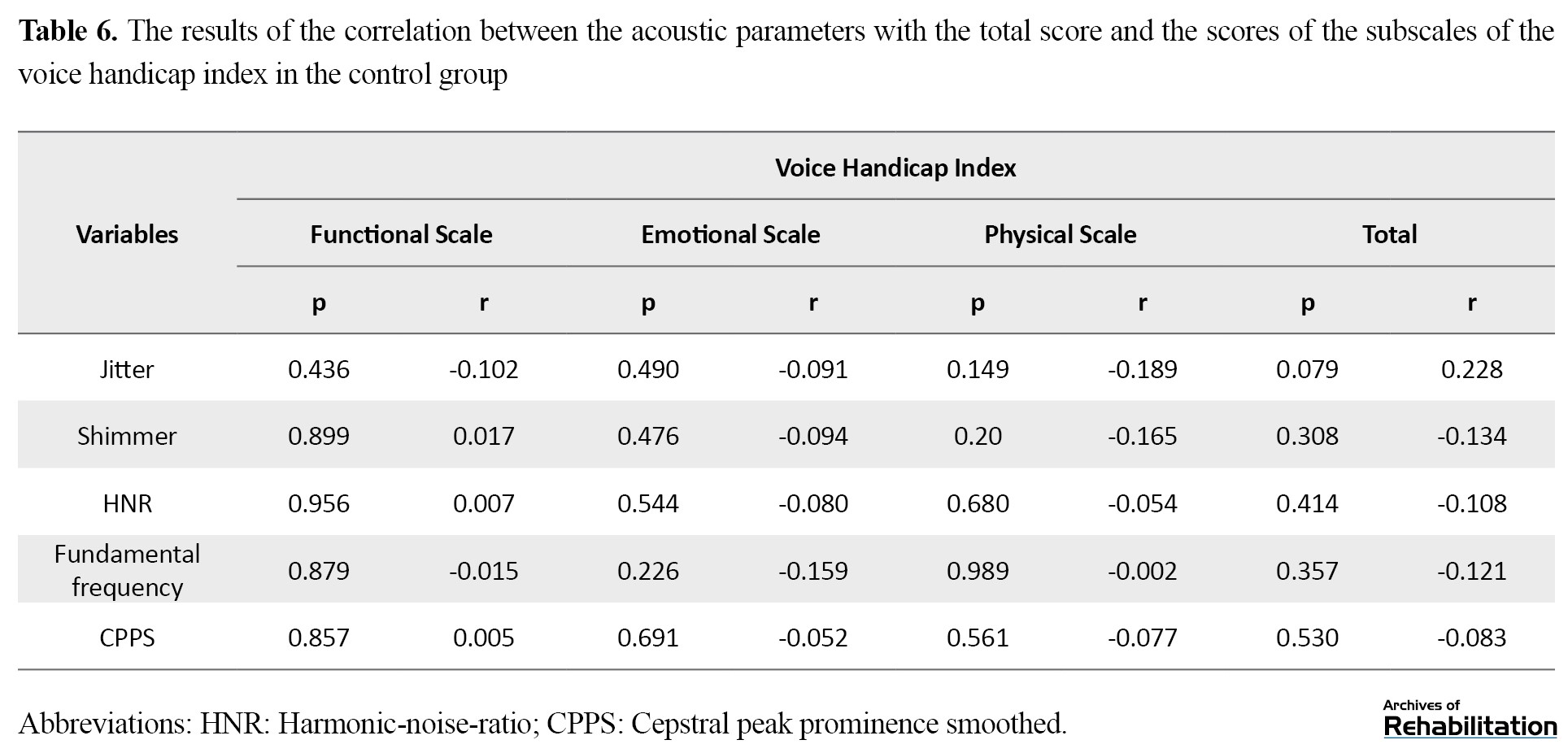
The results of Table 6 regarding the correlation test show no significant relationship between the acoustic parameters and the subscales of the voice handicap index in the control group (P<0.05).
Discussion
Squamous cell carcinoma of the larynx accounts for a significant share of head and neck cancers [2], and transoral laser microsurgery with a disease-free survival rate of 60% is one of the first control programs for this condition [42]. On the other hand, clinical evidence shows that after completing the duration of this oncological treatment, patients have faced numerous side effects in various aspects of daily life, the result of which endangers the health of vocal function and the physical, psychological and social aspects of a person’s life [43]. Therefore, in the first step of the current study, the vocal characteristics of patients with early laryngeal cancer after transoral laser microsurgery were investigated by acoustic evaluations and the self-assessment scale of the voice handicap index, and the findings were compared with the information of the control group consisting of healthy individuals with normal voice quality. Then, the correlation of the results of acoustic evaluations with the total score and subscales of VHI was studied in the patient group.
The findings of the acoustic analysis of the voice signal in the group under transoral laser microsurgery show a significant difference in jitter, shimmer, HNR and CPPS parameters compared to the control group. This finding is consistent with the research results of Haddad et al. [48], Vilaseca et al. [49] and Karlsen et al. [36]. Because inflammation, swelling and scar formation in the vocal folds are inevitable complications of transoral laser surgery and affect the health of phonation [17, 50]. This issue is considered to be one of the long-term complications of surgery in tumors of the glottis area and is the basis for a range of functional disorders; therefore, it seems that the observed difference is related to the formation of uneven scar surfaces in the vibrating parts of the vocal folds, which by changing the viscoelasticity property and reducing the vibration power [51] has led to the lack of periodicity and coordination in the vibration cycle, the result of which is evident in the acoustic analysis of the audio signal. [52]. Also, in the present study, a significant increase in the fundamental frequency parameter was observed in the patient group. This finding is consistent with the results of Luo et al.’s study [53] and inconsistent with the results of Haddad et al.’s study [48]. This issue can be justified for two reasons. The first reason is related to the factors affecting the physical changes of the fundamental frequency, which consists of the components of length, mass, and tension force of vocal folds [53]; therefore, it is expected that the fundamental frequency will increase by reducing the mass caused by vocal fold surgery. The second reason is also related to the inevitable changes in the sensory-motor components of the larynx after transoral laser microsurgery, which people compensate by hyper functioning the internal and external muscles of the larynx, which leads to a strained and hoarsed quality of voice.
Also, the results of comparing the total scores and subscales of the voice handicap index in people undergoing transoral laser microsurgery with healthy people indicated a significant difference in the QoL of patients undergoing trasoral laser microsurgery with the control group. Because voice disorders affect the communication, social interactions and QoL of a person and lead to many problems in different dimensions of emotional, social and economic life. In this way, despite the remarkable success of transoral laser microsurgery in controlling malignancy, it is necessary to pay attention to psychological issues and QoL of people by presenting an integrated program along with conventional medical interventions and voice rehabilitation.
Other findings of this study include the non-correlation of acoustic parameters and the voice handicap index in the control group and the significant inverse correlation of the total scores and the scores of the subscales of the voice handicap index with the parameter of CPPS. These results regarding the correlation of other acoustic parameters did not exist completely. A possible explanation is that cepstral analysis have been the best available method to evaluate voice quality even in samples with high degree of hoarseness due to the high correlation with breathiness and voice harshness components in both vowel and continuous speech tests [19, 54], while studies show that the accuracy of the values of time-based parameters in the mentioned samples is doubtful [55]. Therefore, it is recommended that, along with physical and functional evaluation, the patient’s experiences of his/her voice should be checked and supplemented with objective and more accurate measures, such as frequency-based analysis.
Conclusion
In the present study, acoustic analysis and voice handicap index showed a significant difference between the group undergoing transoral laser microsurgery and healthy individuals, which emphasizes the need for voice rehabilitation and attention to psychological and social issues in the treatment planning of this group of patients.
Also, a significant correlation is observed between the voice handicap index and the acoustic analysis parameters, especially the Cepstral analysis. Therefore, consensus and comprehensive examination of vocal function with subjective and objective measures and attention to patient experiences provide useful information to specialists and therapists in the field of evaluation and rehabilitation of patients with cancer and undergoing laryngeal laser microsurgery. One of the limitations of the present study was the lack of examination of women with laryngeal cancer due to the low frequency and lack of access to this population. Therefore, it is suggested to pay special attention to this group in future studies. It is also recommended that in future studies, the vocal function of patients with advanced levels of laryngeal cancer and those treated with a combination of interventions, such as radiation and chemotherapy and including a set of comprehensive evaluations, such as aerodynamic evaluations and videolaryngosteroscopy should be considered.
Ethical Considerations
Compliance with ethical guidelines
The current research has been registered by the ethics committee in Biomedical Research of the University of Social Welfare and Rehabilitation Sciences with the number IR.USWR.REC.1400.002. In line with the protection of ethical principles, after providing explanations about the purpose and process of the study, informed consent was received from all participants so that they could withdraw from the study at any time if they did not want to cooperate. Also, all the people were assured that the collected information will be used only for scientific purposes and will be recorded confidentially without mentioning names.
Funding
The present article is derived from the Phd thesis of Arezoo Hasanvand in the Speech Therapy Department of the University of Social Welfare and Rehabilitation Sciences, and has no financial support.
Authors' contributions
Conceptualization: All authors; Methodology: Arezoo Hasanvand, Akbar Darouie, Samira Aghadoost and Enayatollah Bakhshi; Supervision: Akbar Darouie, Samira Aghadoost; Analysis: Arezoo Hasanvand, Akbar Darouie and Enayatollah Bakhshi; Writing the draft: Arzoo Hasanvand; Editing and finalization of the article: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We sincerely thank and appreciate all the participants, the management and the respected staff of the Ear, Throat And nose clinic of Amir A'lam Hospital Complex who helped us in conducting this research.
References
Cancers of the head and neck area are considered to be the most common malignancies of the body [1], and among its different types, it is particularly essential to pay attention to the involvement of the larynx area as the vital structure of the swallowing-respiratory system [2]. Statistics show that this type of cancer accounts for approximately 30% of all head and neck malignancies and 1% of all cancers, especially in the sixth and seventh decades of men’s lives [3, 4]. This complication is shown in the form of irregular white or red localized thickenings in the videolaryngoscopy evaluation of microscopic manifestations, and based on the American Joint Committee on Cancer (AJCC) classification known as tumor node metastasis staging system (TNM), is divided into two growth stages consisting of early cancer (tumor size 0, I and II) and advanced laryngeal cancer (tumor size III and IV) [7]. After the appearance of the first clinical manifestations, the main goal and the first line of treatment measures in the medical field is to prevent progress, remove cancer cells and save the person’s life; for this purpose, oncological treatments designed for patients with laryngeal cancer include a variety of surgical methods, radiation, and chemotherapy [8, 9] and in case of disease progression and to achieve the maximum result, a combination of the mentioned methods is prescribed for the disease control [10].
Studies show that in the early stages of disease progression, CO2 transoral laser microsurgery (CO2 TLM) is considered as one of the first options in the treatment of this complication due to fewer complications and a significant success rate of disease control [11]. While the clinical evidence of the voice field shows the spectrum experience of different severities of voice disorders in people treated with transoral laser microsurgery [14, 15], the evaluation of its different angles highly helps in choosing an approach appropriate to the individual’s conditions and providing timely voice rehabilitation courses and programs to experts in this field.
In this regard, the proposed program resulting from the joint meeting of European laryngological society (ELS) considers the comprehensive evaluation of vocal function dependent on the combined use of objective, subjective analyzes and self-perceived evaluations [18]. Among the different types of voice evaluations, acoustic analysis of voice signal samples has become an essential component in the evaluation of vocal function during the last few decades due to easy application, repeatability, non-invasiveness, quantification, and objectivity [19]. The voice handicap index (VHI) questionnaire is also one of the most widely used self-reporting tools that examine psycho-social results and a sense of disability caused by voice disorders in different physical, emotional, and functional dimensions from the patient’s point of view [29].
Regarding laryngeal cancer, the description and comparison of vocal characteristics of patients at different levels of disease progression and the evaluation of the correlation between objective evaluations and different instruments for measuring the voice-related quality of life (QoL) has been the subject of a limited number of studies. For example, the findings of Carlsen et al.’s study on 229 patients with various voice disorders, including laryngeal cancer, also show a correlation between voice handicap index and jitter, shimmer, and harmonic-to-noise ratio (HNR) parameters in this group [36].
The present study, by understanding the need for a comprehensive evaluation of voice characteristics and considering the complex nature of voice disorders, the knowledge gap, the unique features and the distinct structure of the Persian language and culture, using acoustic analysis and the voice handicap index, investigates the vocal quality, the existence of a correlation between objective evaluations and the perception of patients with early laryngeal cancers after transoral laser microsurgery and compares the findings obtained from the voice quality of healthy individuals so that it can be useful for researchers and therapists in this field by creating a clear picture of the vocal status of patients after the completion of oncological treatment courses.
Materials and Methods
The current research is a descriptive, correlational, and comparative study that was conducted cross-sectionally on 120 participants aged 18 to 65 years (with Mean±SD of age 51.72±8.681) in the form of two groups with laryngeal cancer and controls. The patient sample included 60 men with early laryngeal cancer and undergoing transoral laser mirosurgery, who were selected according to the inclusion criteria by the convenience sampling method in the routine visit of people referring to the ear, nose and throat clinic of Amir A'lam Hospital Complex. The control sample also included 60 men with normal voice quality, which was prepared by convinince sampling from healthy people of the population.
In this study, the inclusion criteria of subjects in the patient group included people who had undergone transoral laser microsurgery in glottis area due to early laryngeal cancer. It should be noted that in the present study, the characteristics of the lesion (including the stage and characteristics of the primary tumor) were determined according to the diagnosis of the ear, nose and throat specialist based on the TNM staging system [37] and based on the consensus of the results of direct laryngoscopy evaluation and the written report of the pathology laboratory from the biopsy of the lesion. The selection criteria for the control group included Farsi-speaking, no speech and language disorders, no history of any surgery in the head and neck area, and the presence of normal voice quality based on the perceptual judgment of a speech and language pathologist. In addition, in both groups, the exclusion criteria included a distortion of voice samples and the participants’ unwillingness to cooperate. Table 1 presents other clinical information of participants with early laryngeal carcinoma.
In this study, to collect acoustic data from the analysis of the signal obtained from 3-5 s of continuous stretching of the vowel /a/ by jitter, shimmer, HNR fundamental frequency, fundamental frequency and the Cepstral peak prominence smoothed (CPPS) in Praat software, version 1.6.49 was used. In this way, after understanding the process and practicing the test related to sampling, the voice of the people were recorded using a voice recorder (Zoom brand model H1n with a sampling rate of 24 bits/96 kHz) at an angle of 45 degrees and a distance of 10 cm to the mouth of the participants in WAV format. It should be noted that the data related to the CPPS parameter was extracted according to the settings suggested by Fadke [39]. Then, the Persian version with 30 items of the voice voice handicap index was provided to the participants, and how to complete the questionnaire was explained.
In the present study, data were analyzed using SPSS software, version 20. Also, using the results of Kolmogorov Smirnov test, it was found that the data follow the normal distribution. Then, descriptive statistics, including calculation of central tendency and dispersion indices, independent t-test for between-group comparison and Pearson correlation test were used to examine intragroup relationships of the studied variables at a significance level of less than 0.05.
Results
This research was conducted with 120 male participants in the form of two groups of patients (60 people) and control (60 people). Table 2 presents the age information of the participants.
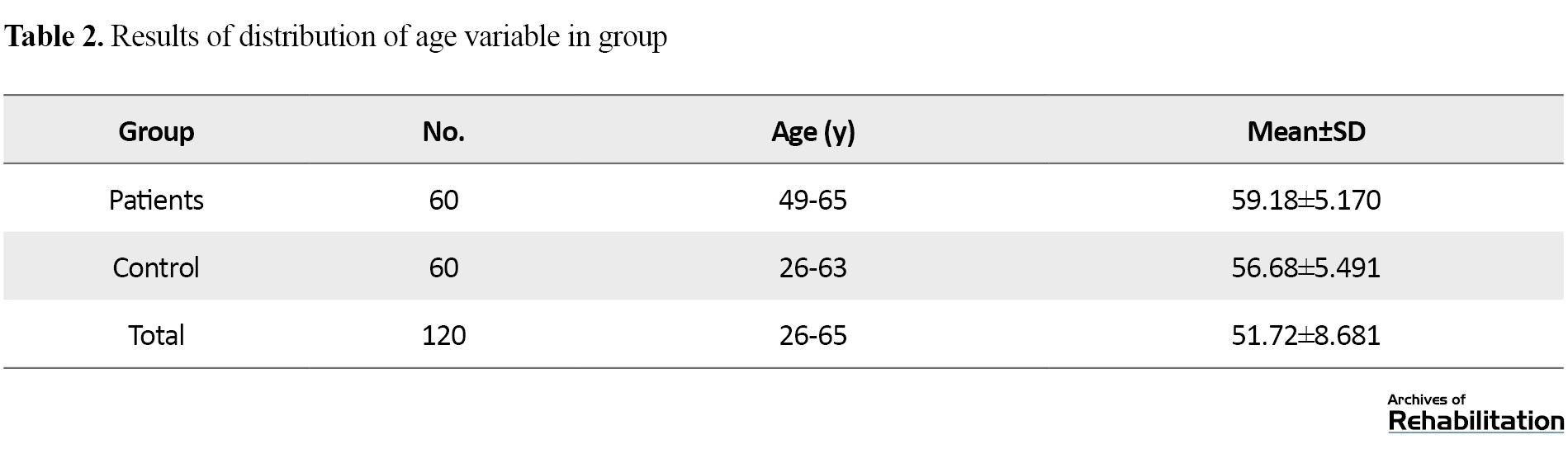
According to the descriptive findings in Table 2, the Mean±SD of the age of the patient group was 59.18±5.170 and the control group was 56.68±5.491 years. Table 3 also reports the results of the between-group comparison of acoustic parameter values.
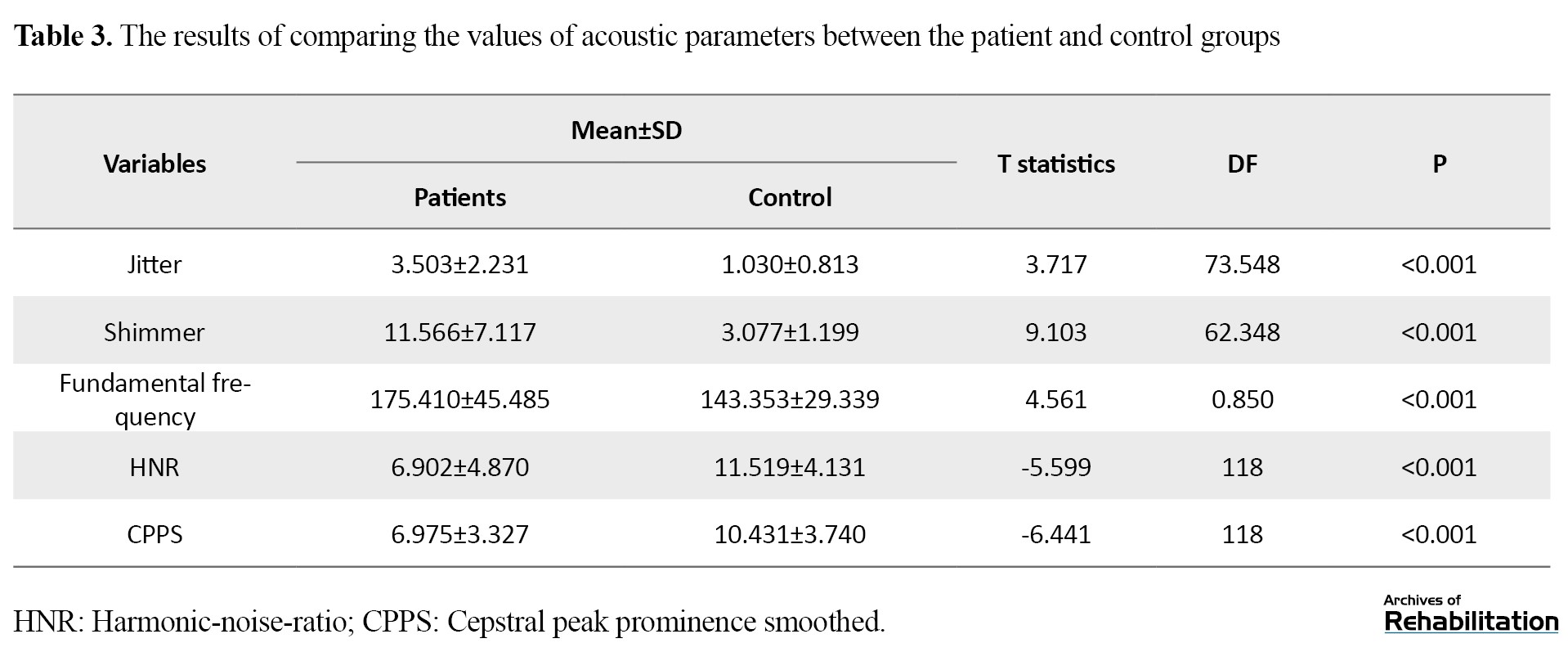
Based on the findings of the above table, the mean values of acoustic analysis parameters, including jitter, shimmer and fundamental frequency of the patient group are significantly higher compared to the control group (P<0.001). Also, the mean values of the parameters of the HNR and the CPPS of the subjects undergoing transoral laser microsurgery were lower than healthy subjects of the control group, and these differences are also statistically significant (P<0.001). Table 4 presents the results of the comparison of the mean total score and the scores of functional, physical and emotional subscales.
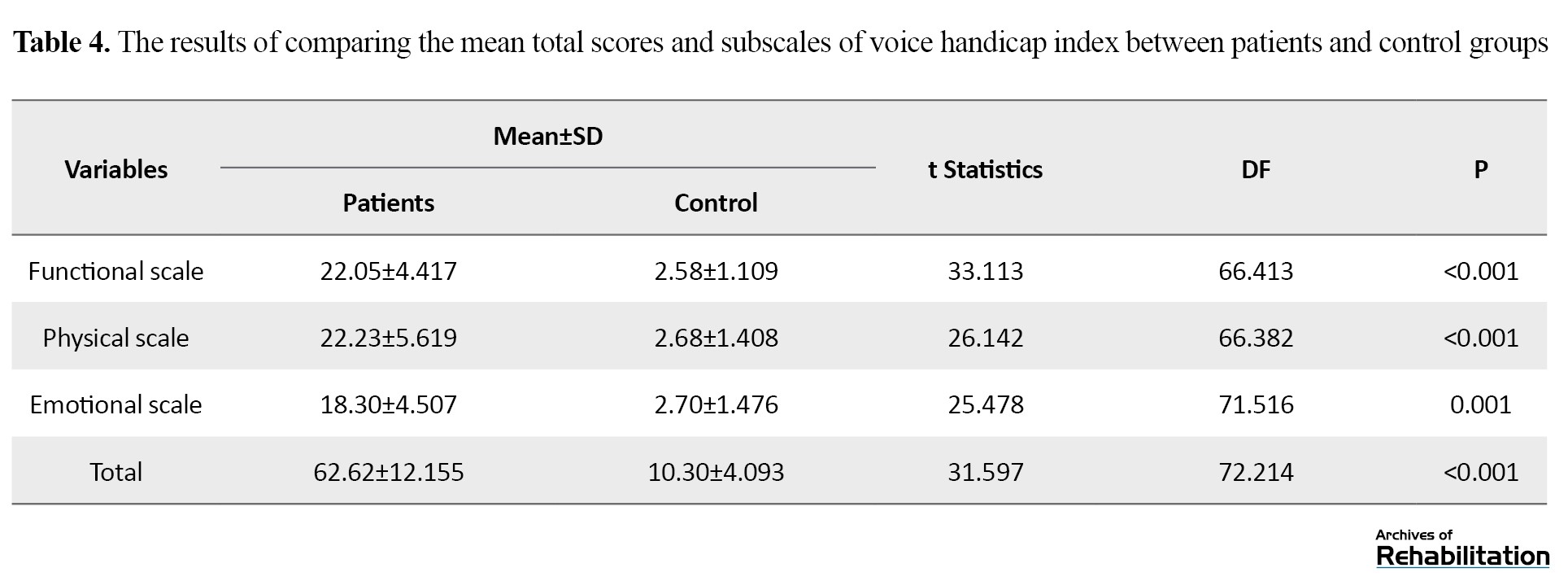
The results of the between-group comparison of the VHI average and its subscales in the above table show a statistically significant difference between the patient and control groups (P<0.001). Table 5 presents the results of the correlation between the acoustic parameters with the total score and the scores of the subscales of the voice handicap index in the patient group.
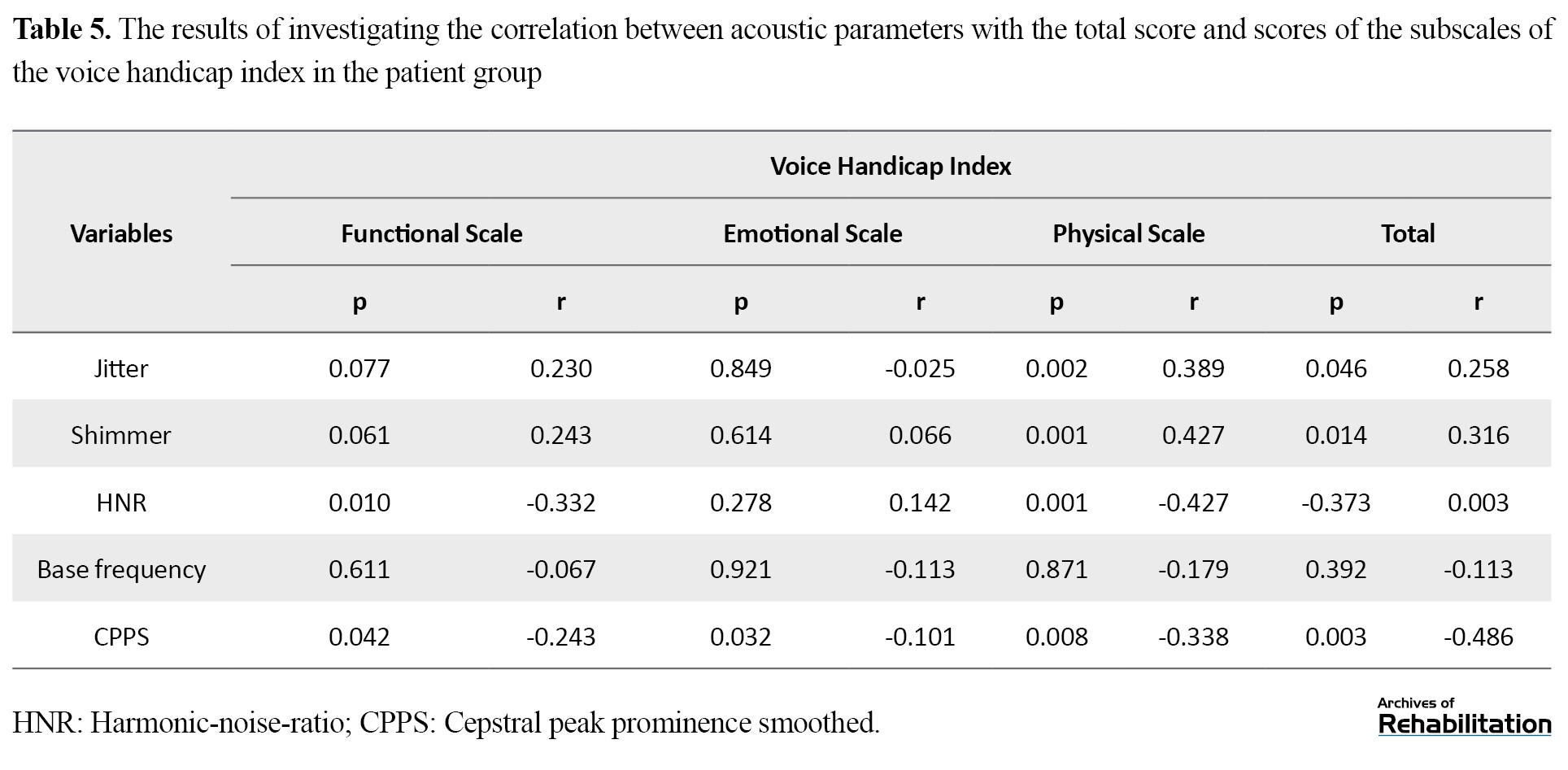
As mentioned, Pearson’s correlation coefficient was used to know the relationships between research variables in the patient group; the results indicated a direct and significant correlation between the jitter parameter and the total score (r=0.258 and P=0.046) and physical subscale scores (r=0.389 and P=0.002) of the voice handicap index. The same results were repeated regarding Shimmer and it was found that this parameter has a direct correlation with the total score (r=0.316 and P=0.014) and the physical subscale score (r=0.427 and P=0.001) of VHI. The HNR parameter has an inverse, weak and significant relationship with the total score (r=0.003 and P=-0.373) and the scores of physical (r=-0.427 and P=0.001) and functional (r=-0.332 and P=-0.010). Also, the CPPS parameter has an inverse and significant relationship with the total score (r=-0.486 and P=0.003) and the scores of three functional (r=-0.243 and P=0.042), physical (r=-0.338 and P=0.008) and emotional (r=0.486 and P=0.003) subscales of voice handicap index. On the other hand, according to the results of the correlation test, no significant relationship (P<0.05) was observed between the fundamental frequency and the subscales of the voice handicap index (Table 5). Table 6 presents the results of the correlation between the acoustic parameters with the total score and the scores of the subscales of the voice handicap index in the control group.
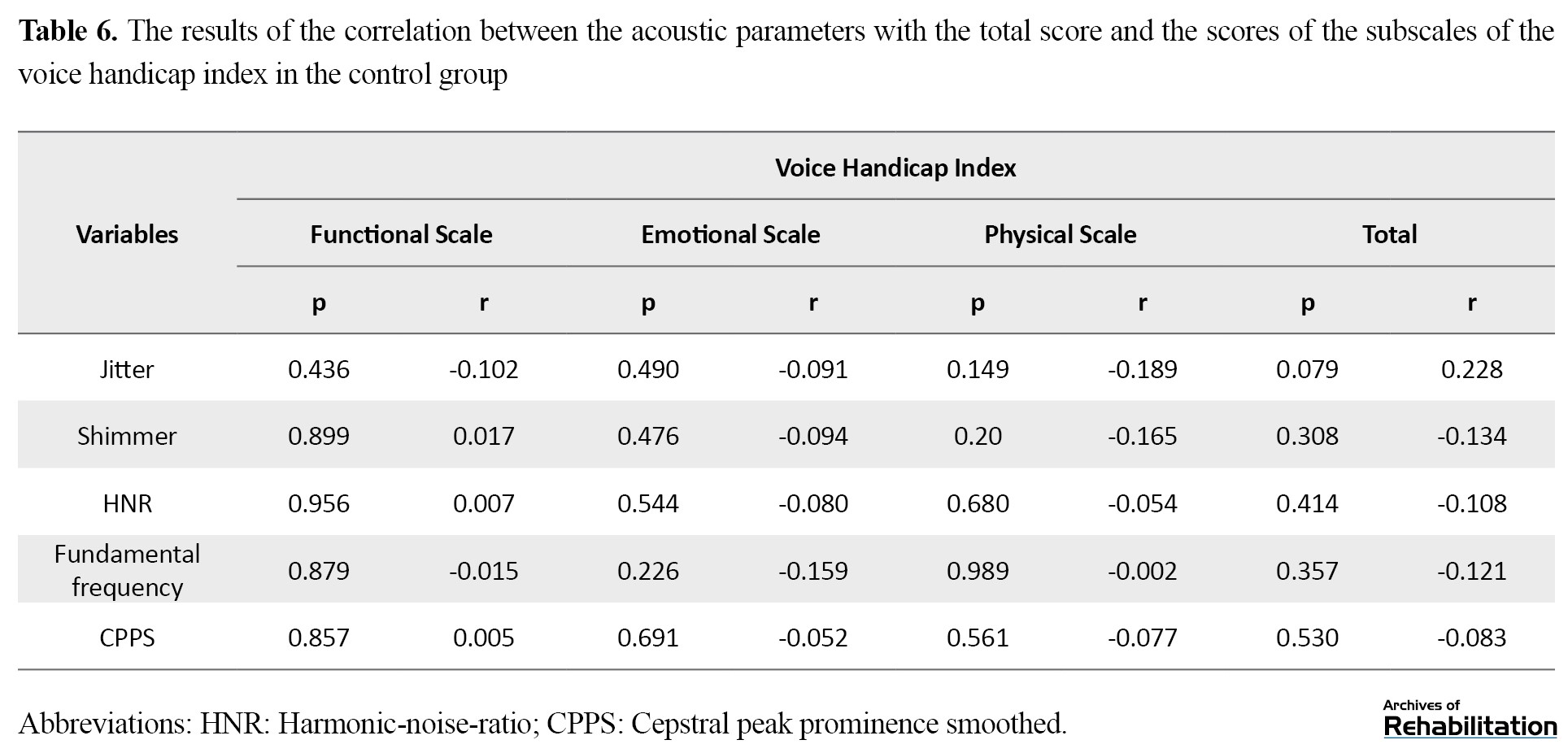
The results of Table 6 regarding the correlation test show no significant relationship between the acoustic parameters and the subscales of the voice handicap index in the control group (P<0.05).
Discussion
Squamous cell carcinoma of the larynx accounts for a significant share of head and neck cancers [2], and transoral laser microsurgery with a disease-free survival rate of 60% is one of the first control programs for this condition [42]. On the other hand, clinical evidence shows that after completing the duration of this oncological treatment, patients have faced numerous side effects in various aspects of daily life, the result of which endangers the health of vocal function and the physical, psychological and social aspects of a person’s life [43]. Therefore, in the first step of the current study, the vocal characteristics of patients with early laryngeal cancer after transoral laser microsurgery were investigated by acoustic evaluations and the self-assessment scale of the voice handicap index, and the findings were compared with the information of the control group consisting of healthy individuals with normal voice quality. Then, the correlation of the results of acoustic evaluations with the total score and subscales of VHI was studied in the patient group.
The findings of the acoustic analysis of the voice signal in the group under transoral laser microsurgery show a significant difference in jitter, shimmer, HNR and CPPS parameters compared to the control group. This finding is consistent with the research results of Haddad et al. [48], Vilaseca et al. [49] and Karlsen et al. [36]. Because inflammation, swelling and scar formation in the vocal folds are inevitable complications of transoral laser surgery and affect the health of phonation [17, 50]. This issue is considered to be one of the long-term complications of surgery in tumors of the glottis area and is the basis for a range of functional disorders; therefore, it seems that the observed difference is related to the formation of uneven scar surfaces in the vibrating parts of the vocal folds, which by changing the viscoelasticity property and reducing the vibration power [51] has led to the lack of periodicity and coordination in the vibration cycle, the result of which is evident in the acoustic analysis of the audio signal. [52]. Also, in the present study, a significant increase in the fundamental frequency parameter was observed in the patient group. This finding is consistent with the results of Luo et al.’s study [53] and inconsistent with the results of Haddad et al.’s study [48]. This issue can be justified for two reasons. The first reason is related to the factors affecting the physical changes of the fundamental frequency, which consists of the components of length, mass, and tension force of vocal folds [53]; therefore, it is expected that the fundamental frequency will increase by reducing the mass caused by vocal fold surgery. The second reason is also related to the inevitable changes in the sensory-motor components of the larynx after transoral laser microsurgery, which people compensate by hyper functioning the internal and external muscles of the larynx, which leads to a strained and hoarsed quality of voice.
Also, the results of comparing the total scores and subscales of the voice handicap index in people undergoing transoral laser microsurgery with healthy people indicated a significant difference in the QoL of patients undergoing trasoral laser microsurgery with the control group. Because voice disorders affect the communication, social interactions and QoL of a person and lead to many problems in different dimensions of emotional, social and economic life. In this way, despite the remarkable success of transoral laser microsurgery in controlling malignancy, it is necessary to pay attention to psychological issues and QoL of people by presenting an integrated program along with conventional medical interventions and voice rehabilitation.
Other findings of this study include the non-correlation of acoustic parameters and the voice handicap index in the control group and the significant inverse correlation of the total scores and the scores of the subscales of the voice handicap index with the parameter of CPPS. These results regarding the correlation of other acoustic parameters did not exist completely. A possible explanation is that cepstral analysis have been the best available method to evaluate voice quality even in samples with high degree of hoarseness due to the high correlation with breathiness and voice harshness components in both vowel and continuous speech tests [19, 54], while studies show that the accuracy of the values of time-based parameters in the mentioned samples is doubtful [55]. Therefore, it is recommended that, along with physical and functional evaluation, the patient’s experiences of his/her voice should be checked and supplemented with objective and more accurate measures, such as frequency-based analysis.
Conclusion
In the present study, acoustic analysis and voice handicap index showed a significant difference between the group undergoing transoral laser microsurgery and healthy individuals, which emphasizes the need for voice rehabilitation and attention to psychological and social issues in the treatment planning of this group of patients.
Also, a significant correlation is observed between the voice handicap index and the acoustic analysis parameters, especially the Cepstral analysis. Therefore, consensus and comprehensive examination of vocal function with subjective and objective measures and attention to patient experiences provide useful information to specialists and therapists in the field of evaluation and rehabilitation of patients with cancer and undergoing laryngeal laser microsurgery. One of the limitations of the present study was the lack of examination of women with laryngeal cancer due to the low frequency and lack of access to this population. Therefore, it is suggested to pay special attention to this group in future studies. It is also recommended that in future studies, the vocal function of patients with advanced levels of laryngeal cancer and those treated with a combination of interventions, such as radiation and chemotherapy and including a set of comprehensive evaluations, such as aerodynamic evaluations and videolaryngosteroscopy should be considered.
Ethical Considerations
Compliance with ethical guidelines
The current research has been registered by the ethics committee in Biomedical Research of the University of Social Welfare and Rehabilitation Sciences with the number IR.USWR.REC.1400.002. In line with the protection of ethical principles, after providing explanations about the purpose and process of the study, informed consent was received from all participants so that they could withdraw from the study at any time if they did not want to cooperate. Also, all the people were assured that the collected information will be used only for scientific purposes and will be recorded confidentially without mentioning names.
Funding
The present article is derived from the Phd thesis of Arezoo Hasanvand in the Speech Therapy Department of the University of Social Welfare and Rehabilitation Sciences, and has no financial support.
Authors' contributions
Conceptualization: All authors; Methodology: Arezoo Hasanvand, Akbar Darouie, Samira Aghadoost and Enayatollah Bakhshi; Supervision: Akbar Darouie, Samira Aghadoost; Analysis: Arezoo Hasanvand, Akbar Darouie and Enayatollah Bakhshi; Writing the draft: Arzoo Hasanvand; Editing and finalization of the article: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We sincerely thank and appreciate all the participants, the management and the respected staff of the Ear, Throat And nose clinic of Amir A'lam Hospital Complex who helped us in conducting this research.
References
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer Journal of Clinicians. 2020; 72(1):7-33. [DOI:10.3322/caac.21708] [PMID]
- Megwalu UC, Sikora AG. Survival outcomes in advanced laryngeal cancer. JAMA Otolaryngology-Head & Neck Surgery. 2014; 140(9):855-60. [DOI:10.1001/jamaoto.2014.1671] [PMID]
- Markou K, Christoforidou A, Karasmanis I, Tsiropoulos G, Triaridis S, Constantinidis I, et al. Laryngeal cancer: Epidemiological data from Νorthern Greece and review of the literature. Hippokratia. 2013; 17(4):313-8. [PMID] [PMCID]
- Calkovsky V, Wallenfels P, Calkovska A, Hajtman A. Laryngeal cancer: 12-year experience of a single center. In: Pokorski M, editor. Advances in respiratory cancerogenesis. Advances in respiratory cancerogenesis. Cham: Springer; 2015.[DOI:10.1007/5584_2015_201] [PMID]
- Brown K, Cherry W, Forbes W, Mcmichael A. Laryngeal cancer and consumption of alcohol and tobacco. The Lancet. 1978; 312(8099):1099-100. [DOI:10.1016/S0140-6736(78)91835-4] [PMID]
- Wagner M, Bolm-Audorff U, Hegewald J, Fishta A, Schlattmann P, Schmitt J, et al. Occupational polycyclic aromatic hydrocarbon exposure and risk of larynx cancer: A systematic review and meta-analysis. Occupational and Environmental Medicine. 2015; 72(3):226-33. [DOI:10.1136/oemed-2014-102317] [PMID]
- Lydiatt WM, Patel SG, O’Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, et al. Head and neck cancers-major changes in the American joint committee on cancer eighth edition cancer staging manual. Ca: A Cancer Journal for Clinicians. 2017; 67(2):122-37. [DOI:10.3322/caac.21389] [PMID]
- Chen AY, Schrag N, Hao Y, Flanders W D, Kepner J, Stewart A, et al. Changes in treatment of advanced laryngeal cancer 1985-2001. Otolaryngology-Head and Neck Surgery. 2006; 135(6):831-7. [DOI:10.1016/j.otohns.2006.07.012] [PMID]
- Peretti G, Piazza C, Cocco D, De Benedetto L, Del Bon F, Redaelli De Zinis LO, et al. Transoral co2 laser treatment for Tis-T3 glottic cancer: The University of Brescia experience on 595 patients. Head & Neck. 2010; 32(8):977-83. [DOI:10.1002/hed.21278] [PMID]
- Forastiere AA, Weber RS, Trotti A. Organ preservation for advanced larynx cancer: Issues and outcomes. Journal of Clinical Oncology. 2015; 33(29):3262. [DOI:10.1200/JCO.2015.61.2978] [PMID] [PMCID]
- Baird BJ, Sung CK, Beadle BM, Divi V. Treatment of early-stage laryngeal cancer: A comparison of treatment options. Oral Oncology. 2018; 87:8-16. [DOI:10.1016/j.oraloncology.2018.09.012] [PMID]
- Megwalu UC, Panossian H. Survival outcomes in early stage laryngeal cancer. Anticancer Research. 2016; 36(6):2903-7. [PMID]
- Jepsen MC, Gurushanthaiah D, Roy N, Smith ME, Gray SD, Davis RK. Voice, speech, and swallowing outcomes in laser‐treated laryngeal cancer. The Laryngoscope. 2003; 113(6):923-8. [DOI:10.1097/00005537-200306000-00001] [PMID]
- Fink DS, Sibley H, Kunduk M, Schexnaildre M, Kakade A, Sutton C, et al. Subjective and objective voice outcomes after transoral laser microsurgery for early glottic cancer. The Laryngoscope. 2016; 126(2):405-7. [DOI:10.1002/lary.25442] [PMID]
- Tomifuji M, Araki K, Niwa K, Miyagawa Y, Mizokami D, Kitagawa Y, et al. Comparison of voice quality after laser cordectomy with that after radiotherapy or chemoradiotherapy for early glottic carcinoma. ORL; Journal for Oto-Rhino-Laryngology and its Related Specialties. 2013; 75(1):18-26. [DOI:10.1159/000346934] [PMID]
- Samlan RA, Webster KT. Swallowing and speech therapy after definitive treatment for laryngeal cancer. Otolaryngologic Clinics of North America. 2002; 35(5):1115-33. [DOI:10.1016/S0030-6665(02)00033-6] [PMID]
- Branski RC, Verdolini K, Sandulache V, Rosen CA, Hebda PA. Vocal fold wound healing: A review for clinicians. Journal of Voice. 2006; 20(3):432-42. [DOI:10.1016/j.jvoice.2005.08.005] [PMID]
- Patel RR, Awan SN, Barkmeier-Kraemer J, Courey M, Deliyski D, Eadie T, et al. Recommended protocols for instrumental assessment of voice: American speech-language-hearing association expert panel to develop a protocol for instrumental assessment of vocal function. American Journal of Speech-Language Pathology. 2018; 27(3):887-905. [DOI:10.1044/2018_AJSLP-17-0009] [PMID]
- Maryn Y, Roy N, De Bodt M, Van Cauwenberge P, Corthals P. Acoustic measurement of overall voice quality: A meta-analysis. The Journal of the Acoustical Society of America. 2009; 126(5):2619-34. [DOI:10.1121/1.3224706] [PMID]
- Mahato NB, Regmi D, Bista M, Sherpa P. Acoustic analysis of voice in school teachers. JNMA; Journal of the Nepal Medical Association. 2018; 56(211):658-61. [DOI:10.31729/jnma.3626] [PMID] [PMCID]
- Bottalico P, Codino J, Cantor-Cutiva LC, Marks K, Nudelman CJ, Skeffington J, et al. Reproducibility of voice parameters: The effect of room acoustics and microphones. Journal of Voice. 2020; 34(3):320-34. [DOI:10.1016/j.jvoice.2018.10.016] [PMID] [PMCID]
- Williamson J, Ingrams D, Jones H. Quality of life after treatment of laryngeal carcinoma: A single centre cross-sectional study. The Annals of the Royal College of Surgeons of England. 2011; 93(8):591-5. [DOI:10.1308/147870811X13137608455253] [PMID] [PMCID]
- Eadie TL. Application of the ICF in communication after total laryngectomy. Seminars in Speech and Language. 2007; 28(4):291-300. [DOI:10.1055/s-2007-986526] [PMID]
- Tschiesner U, Cieza A, Rogers S, Piccirillo J, Funk G, Stucki G, et al. Developing core sets for patients with head and neck cancer based on the international classification of functioning, disability and health (ICF). European Archives of Oto-Rhino-Laryngology. 2007; 264(10):1215-22. [DOI:10.1007/s00405-007-0335-8] [PMID]
- Singer S, Danker H, Bloching M, Kluge A, Schwenke J, Oeken J, et al. [Perceived stigmatisation following laryngectomy (German)]. Psychotherapie, Psychosomatik, Medizinische Psychologie. 2007; 57(8):328-33. [DOI:10.1055/s-2006-952016] [PMID]
- Murry T, Rosen CA. Outcome measurements and quality of life in voice disorders. Otolaryngologic Clinics of North America. 2000; 33(4):905-16. [DOI:10.1016/S0030-6665(05)70251-6] [PMID]
- Behlau M, Hogikyan ND, Gasparini G. Quality of life and voice: Study of a Brazilian population using the voice-related quality of life measure. Folia Phoniatrica et Logopaedica. 2007; 59(6):286-96. [DOI:10.1159/000108335] [PMID]
- Hsiung MW, Pai L, Wang HW. Correlation between voice handicap index and voice laboratory measurements in dysphonic patients. European Archives of Oto-rhino-laryngology. 2002; 259(2):97-9. [DOI:10.1007/s004050100405] [PMID]
- Maertens K, De Jong F. The voice handicap index as a tool for assessment of the biopsychosocial impact of voice problems. B ENT. 2007; 3(2):61-6. [PMID]
- Ng ML, Chen Y, Chan EY. Differences in vocal characteristics between Cantonese and English produced by proficient Cantonese-English bilingual speakers-a long-term average spectral analysis. Journal of Voice. 2012; 26(4):e171-6. [DOI:10.1016/j.jvoice.2011.07.013] [PMID]
- Ng ML, Hsueh G, Sam Leung CS. Voice pitch characteristics of Cantonese and English produced by Cantonese-English bilingual children. International Journal of Speech-Language Pathology. 2010; 12(3):230-6. [DOI:10.3109/17549501003721080] [PMID]
- Fayers PM, Machin D. Quality of life: The assessment, analysis and interpretation of patient-reported outcomes. Hoboken: John Wiley & Sons; 2007. [Link]
- Hamzany Y, Crevier-Buchman L, Lechien JR, Bachar G, Brasnu D, Hans S. Multidimensional voice quality evaluation after transoral co2 laser cordectomy: A prospective study. Ear, Nose & Throat Journal. 2021; 100(1_suppl):27S-32. [DOI:10.1177/0145561320906328] [PMID]
- Kasper C, Schuster M, Psychogios G, Zenk J, Ströbele A, Rosanowski F, et al. Voice handicap index and voice-related quality of life in small laryngeal carcinoma. European Archives of Oto-rhino-laryngology. 2011; 268(3):401-4. [DOI:10.1007/s00405-010-1374-0] [PMID]
- Portone CR, Hapner ER, McGregor L, Otto K, Johns III MM. Correlation of the voice handicap index (VHI) and the voice-related quality of life measure (V-RQOL). Journal of Voice. 2007; 21(6):723-7. [DOI:10.1016/j.jvoice.2006.06.001] [PMID]
- Karlsen T, Sandvik L, Heimdal JH, Aarstad HJ. Acoustic voice analysis and maximum phonation time in relation to voice handicap index score and larynx disease. Journal of Voice. 2020; 34(1):161. e27-35. [DOI:10.1016/j.jvoice.2018.07.002] [PMID]
- Cancer AJCo. Larynx. In: American Joint Committee on Cancer, editor. AJCC cancer staging manual. New York: Springer; 2002. [DOI:10.1007/978-1-4757-3656-4_5]
- Archer SK, Iezzi CM, Gilpin L. Swallowing and voice outcomes in patients hospitalized with covid-19: An observational cohort study. Archives of Physical Medicine and Rehabilitation. 2021; 102(6):1084-90. [DOI:10.1016/j.apmr.2021.01.063] [PMID] [PMCID]
- Phadke KV, Laukkanen AM, Ilomäki I, Kankare E, Geneid A, Švec JG. Cepstral and perceptual investigations in female teachers with functionally healthy voice. Journal of Voice. 2020; 34(3):485. e33-43. [DOI:10.1016/j.jvoice.2018.09.010] [PMID]
- Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS, et al. The voice handicap index (VHI) development and validation. American Journal of Speech-Language Pathology. 1997; 6(3):66-70. [DOI:10.1044/1058-0360.0603.66]
- Moradi N, Pourshahbaz A, Soltani M, Javadipour S, Hashemi H, Soltaninejad N. Cross-cultural equivalence and evaluation of psychometric properties of voice handicap index into Persian. Journal of Voice. 2013; 27(2):258.e15-22. [DOI:10.1016/j.jvoice.2012.09.006] [PMID]
- De Santis R, Poon I, Lee J, Karam I, Enepekides D, Higgins K. Comparison of survival between radiation therapy and trans-oral laser microsurgery for early glottic cancer patients; a retrospective cohort study. Journal of Otolaryngology-Head & Neck Surgery. 2016; 45(1):42. [DOI:10.1186/s40463-016-0155-1] [PMID] [PMCID]
- Clements KS, Rassekh CH, Seikaly H, Hokanson JA, Calhoun KH. Communication after laryngectomy: An assessment of patient satisfaction. Archives of Otolaryngology-Head & Neck Surgery. 1997; 123(5):493-6. [DOI:10.1001/archotol.1997.01900050039004] [PMID]
- Van Houtte E, Van Lierde K, Claeys S. Pathophysiology and treatment of muscle tension dysphonia: A review of the current knowledge. Journal of Voice. 2011; 25(2):202-7. [DOI:10.1016/j.jvoice.2009.10.009] [PMID]
- Fung K, Yoo J, Leeper H, Hawkins S, Heeneman H, Doyle PC, et al. Vocal function following radiation for non-laryngeal versus laryngeal tumors of the head and neck. The Laryngoscope. 2001; 111(11):1920-4. [DOI:10.1097/00005537-200111000-00009] [PMID]
- Morrison MD, Rammage LA, Belisle GM, Pullan CB, Nichol H. Muscular tension dysphonia. The Journal of Otolaryngology. 1983; 12(5):302-6. [PMID]
- Ledda GP, Grover N, Pundir V, Masala E, Puxeddu R. Functional outcomes after co2 laser treatment of early glottic carcinoma. The Laryngoscope. 2006; 116(6):1007-11. [DOI:10.1097/01.MLG.0000217557.45491.BD] [PMID]
- Haddad L, Abrahão M, Cervantes O, Ceccon FP, Gielow I, Carvalho JR, et al. Vocal assessment in patients submited to co2 laser cordectomy. Brazilian Journal of Otorhinolaryngology. 2006; 72(3):295-301. [DOI:10.1016/S1808-8694(15)30960-5] [PMID]
- Vilaseca I, Huerta P, Blanch JL, Fernández-Planas AM, Jiménez C, Bernal-Sprekelsen M. Voice quality after co2 laser cordectomy--what can we really expect? Head Neck. 2008; 30(1):43-9. [DOI:10.1002/hed.20659] [PMID]
- Vilaseca-González I, Bernal-Sprekelsen M, Blanch-Alejandro JL, Moragas-Lluis M. Complications in transoral CO2 laser surgery for carcinoma of the larynx and hypopharynx. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck. 2003; 25(5):382-8. [DOI:10.1002/hed.10207]
- Bless DM, Welham NV. Characterization of vocal fold scar formation, prophylaxis, and treatment using animal models. Curr Opin Otolaryngol Head Neck Surg. 2010; 18(6):481-6. [DOI:10.1097/MOO.0b013e3283407d87] [PMID] [PMCID]
- Johns MM, Kolachala V, Berg E, Muller S, Creighton FX, Branski RC. Radiation fibrosis of the vocal fold: From man to mouse. Laryngoscope. 2012; 122 Suppl 5(Suppl 5):S107-25. [DOI:10.1002/lary.23735] [PMID] [PMCID]
- Luo CM, Fang TJ, Lin CY, Chang JT, Liao CT, Chen IH, et al. Transoral laser microsurgery elevates fundamental frequency in early glottic cancer. Journal of Voice. 2012; 26(5):596-601. [DOI:10.1016/j.jvoice.2011.11.006] [PMID]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. C: A Cancer Journal for Clinicians. 2016; 66(1):7-30.
- Maryn Y, Corthals P, Van Cauwenberge P, Roy N, De Bodt M. Toward improved ecological validity in the acoustic measurement of overall voice quality: Combining continuous speech and sustained vowels. Journal of Voice. 2010; 24(5):540-55. [DOI:10.1016/j.jvoice.2008.12.014] [PMID]
- Vogel AP, Fletcher J, Snyder PJ, Fredrickson A, Maruff P. Reliability, stability, and sensitivity to change and impairment in acoustic measures of timing and frequency. Journal of Voice. 2011; 25(2):137-49. [DOI:10.1016/j.jvoice.2009.09.003] [PMID]
- Titze IR, Martin DW. Principles of voice production. The Journal of the Acoustical Society of America. 1998; 104(3). [DOI:10.1121/1.424266]
Type of Study: Original |
Subject:
Speech & Language Pathology
Received: 5/07/2022 | Accepted: 13/11/2022 | Published: 1/01/2023
Received: 5/07/2022 | Accepted: 13/11/2022 | Published: 1/01/2023
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |