Volume 24, Issue 1 (Spring 2023)
jrehab 2023, 24(1): 76-95 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kavyani Boroujeni M, Karimi M T, sharifmoradi K, Akbari-Aghdam H. Evaluation of Static and Dynamic Stability and Its Relationship With Fear of Falling in Patients With Mild to Moderate Knee Osteoarthritis. jrehab 2023; 24 (1) :76-95
URL: http://rehabilitationj.uswr.ac.ir/article-1-3028-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3028-en.html
1- Musculoskeletal Research Center, Isfahan University of Medical Sciences, Isfahan, Iran. , mahsakaviani7@gmail.com
2- Department of Orthotics and Prosthetics, Rehabilitation Faculty, Shiraz University of Medical Sciences, Shiraz, Iran.
3- Department of Sport Sciences, Faculty of Humanities, University of Kashan, Kashan, Iran.
4- Department of Orthopedic, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Orthotics and Prosthetics, Rehabilitation Faculty, Shiraz University of Medical Sciences, Shiraz, Iran.
3- Department of Sport Sciences, Faculty of Humanities, University of Kashan, Kashan, Iran.
4- Department of Orthopedic, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran.
Full-Text [PDF 2534 kb]
(1543 Downloads)
| Abstract (HTML) (4256 Views)
Full-Text: (2281 Views)
Introduction
Osteoarthritis is one of the most common knee joint disorders. Epidemiological studies show that about 17% of Iran’s population has knee osteoarthritis [1]. Knee osteoarthritis is considered one of the risk factors for falling in elderly people [2, 3, 4]. Vision disorders, decreased muscle strength and activity, knee joint proprioceptive disorder, and balance disorder are the most important factors affecting falls in patients with knee osteoarthritis [4, 5, 6]. Whether injured or not, patients who fall are afraid of falling again and therefore limit their functional activities to prevent a possible fall. This condition will restrict patients’ mobility, cause muscle weakness, and increase the risk of falling in the future [7]. It has also been stated that there is a fear of falling in adults with or without a history of falling [8].
Maintaining balance is essential for daily activities [9, 10]. Several studies have shown that patients with knee osteoarthritis have greater postural fluctuations than healthy people [9, 11, 12, 13]. Afferent sensory data from vision, vestibular, and somatosensory systems participate in balance control. The central processing of this information leads to a neuromuscular response that maintains the body’s center of gravity within the range of body support [14]. Therefore, balance disorder increases the risk of falling and reduces the ability to walk.
One of the methods to evaluate postural balance is using a force plate that measures postural fluctuations during standing or walking [15, 16, 17, 18]. Confusion of postural volatility is the main cause of falling and fear of its recurrence in patients with knee osteoarthritis; also, falling is the cause of secondary injuries to patients. Therefore, evaluating the relationship between balance and the fear of falling in patients with knee osteoarthritis can lead to diagnosing the mechanism of disability and falling and help find effective treatment methods for them [9, 19].
Several studies have investigated postural balance and the risk of falling in elderly people and patients with knee osteoarthritis [19-25]. In these studies, the balance has been evaluated with several clinical tests [20, 21, 22], including the functional reach test, step test [21], and timed up and go test [19, 20]. Also, systems such as NeuroCom Balance Master [21] and Biodex are used in this regard [19, 23, 24]. In these studies, balance and its relationship with the fear of falling have often been measured using clinical tests. In contrast, the NeuroCom and the Biodex balance systems are used to assess postural balance, and balance during walking has not been used in all previous studies. Therefore, the current study aims to evaluate the dynamic balance of patients with knee osteoarthritis compared to healthy people (exclusively during walking and based on the fluctuations of the body’s center of pressure and the body’s center of gravity) and to evaluate the static balance using biomechanical parameters (fluctuations of the plantar pressure center) and its relationship with fear of falling.
Materials and Methods
The current research is descriptive cross-sectional. Regarding confounding variables, 15 patients with mild to moderate knee osteoarthritis and 15 healthy individuals matched with the patient group participated in this study (Table 1).
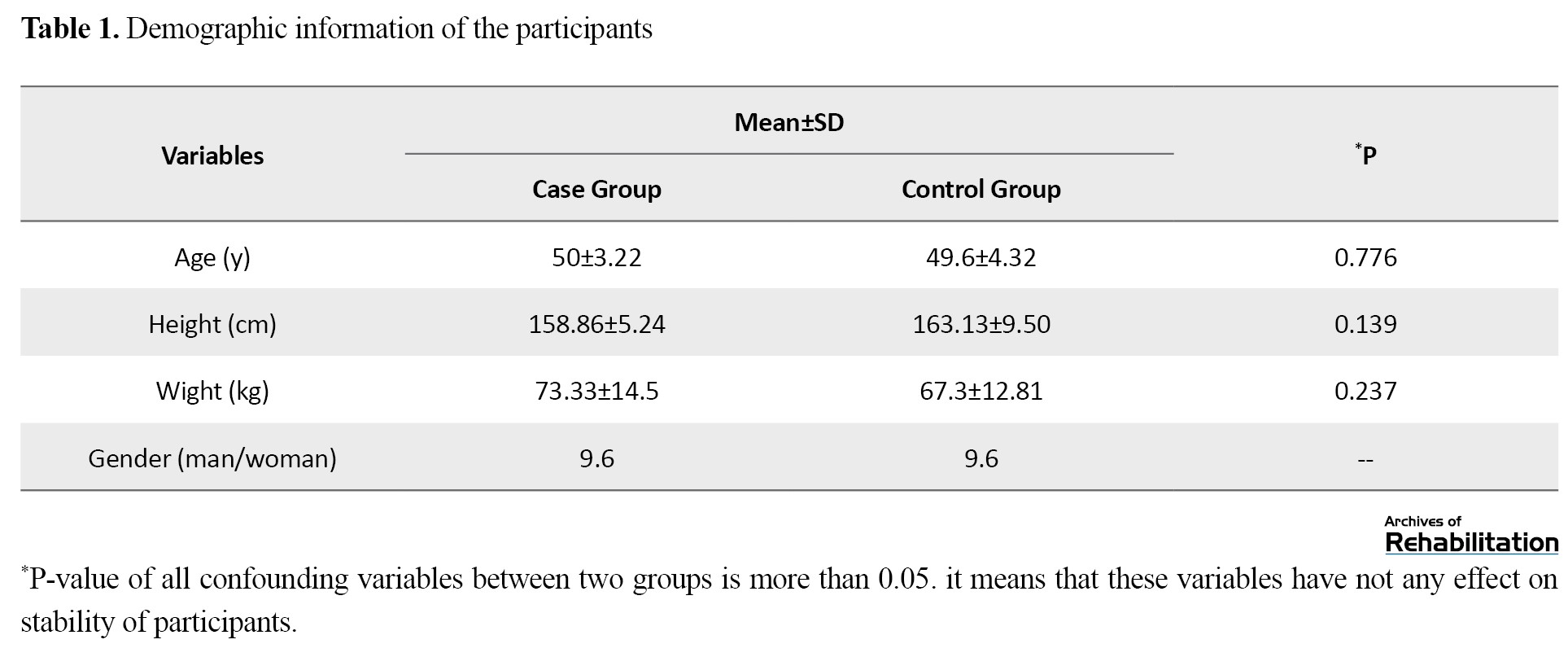
The P>0.05 for all confounding variables between the two groups, which means that the variables are ineffective in the balance of the participants.
The inclusion criteria in the selected patients were as follows: having mild to moderate severity of knee osteoarthritis, mild to moderate pain intensity (based on the VAS scale, mild pain=0-3, moderate pain=4-6) [26, 27], being independent in performing daily activities, lacking any skeletal-muscular disorder affecting people’s ability to walk and stand, and the ability to walk without any assistive devices. Patients with a history of knee surgery and lower limb fracture, a history of falls, and patients undergoing physiotherapy treatment or drug treatment affecting balance, such as sedatives, were excluded from the study.
The international fall efficacy scale (FES-I) was used to assess the fear of falling. The patients’ balance was evaluated in static and dynamic situations (standing and walking, respectively).
The process of performing the balance test
To check the static balance of the participants in the study, a Kistler force plate (60×50 cm, model 9260AA, manufactured by Kistler, Switzerland) was used to collect the data of the center of body pressure (COP) along the x and y axes, which represent the anterior-posterior and internal-external directions, respectively. The data were collected with a frequency of 100 Hz and filtered with a Butterworth low-pass filter with a cut off frequency of 10 hz [28, 29].
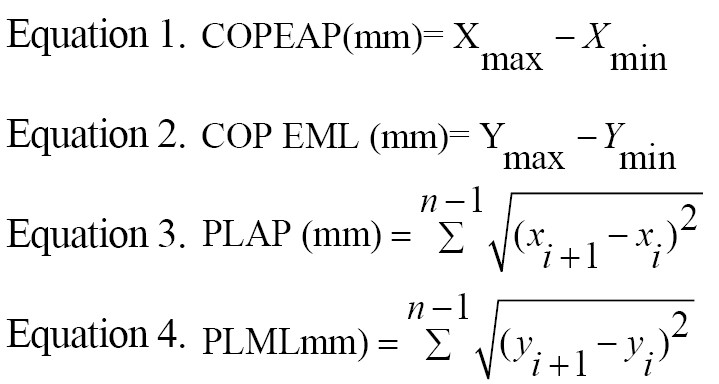
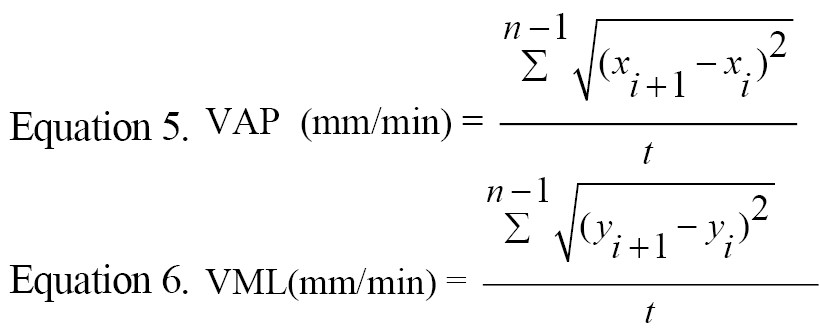
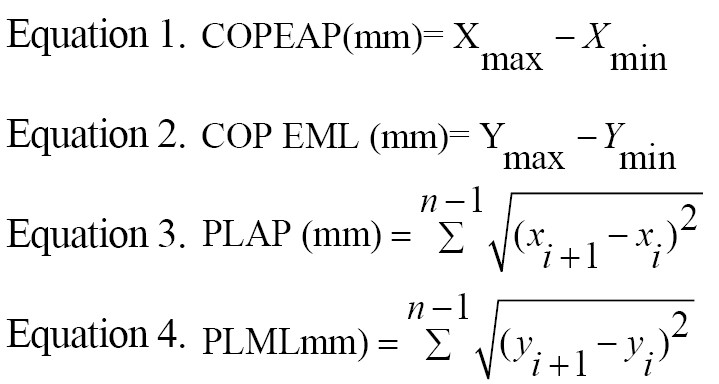
Standing stability of participants in study was measured based on following equations (Equations 1-6):
COPEAP: Center of pressure excursion in the anteroposterior direction, COPEML: Center of pressure excursion in the mediolateral direction, PLAP: Path length of COP in the anteroposterior direction, LML: Path length of COP in the mediolateral direction, VAP: Velocity of center of pressure sways in the anteroposterior plane, VML: Velocity of center of pressure sways in the mediolateral plane.
The dynamic balance of the participants in the study was determined based on the relationship between the body’s center of mass (COM) and the range of the base of support (BOS) in anterior-posterior and internal-external directions [30, 31, 32]. The kinematic information of people’s walking was collected using the Qualisys motion analysis system equipped with 7 cameras and a frequency of 100 Hz. Twenty reflective markers with a diameter of 14 mm were pasted on the anatomical landmarks [31]. Markers were named and defined in Tract Manager software version 2.7 (Analysis Motion Capture Company, Gothenburg, Sweden). The right and left legs, both sides of the calf, pelvis, trunk, and head, were modeled. The main parameters for assessing dynamic balance are the normalized displacement of the body’s COM in anterior-posterior, internal-external, and vertical directions and walking speed.
Statistical analysis of data was done with SPSS software, version 16 (Chicago, SPSS Inc). To check the normal distribution of data, the Shapiro-Wilk test was used. To compare the balance of patients and healthy people, the independent samples t-test was used. The relationship between static and dynamic balance parameters and fear of falling was measured using the Pearson correlation coefficient.
Results
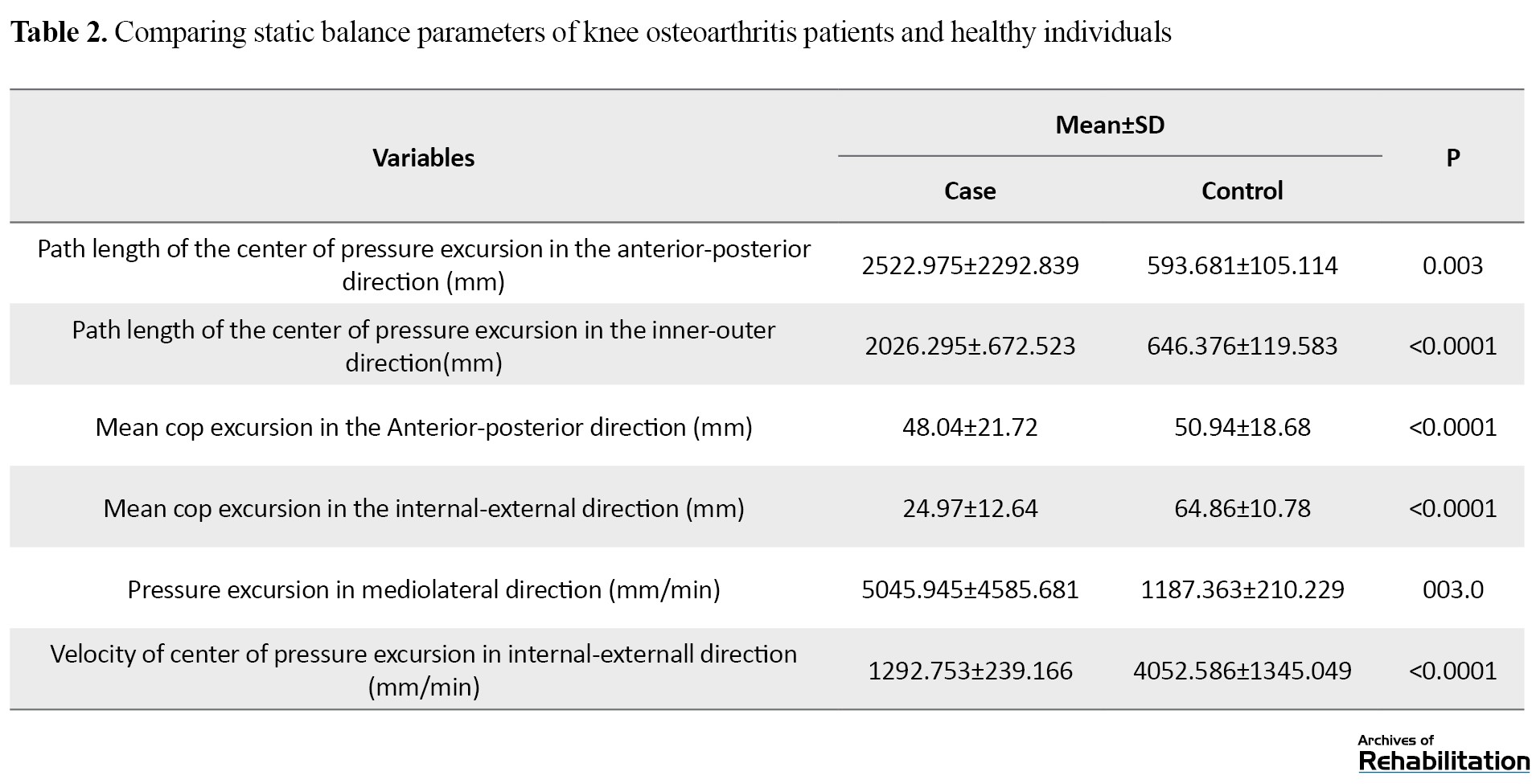
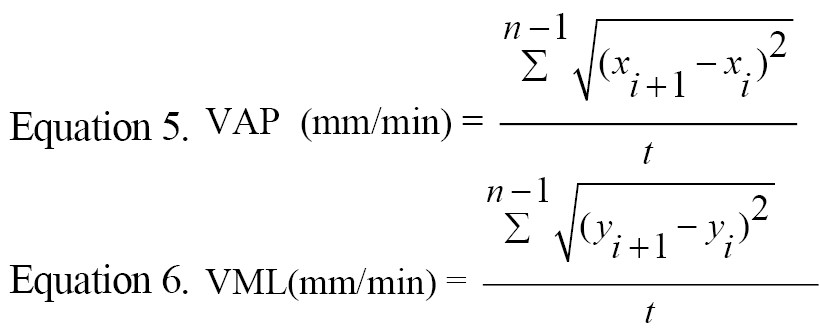
The static balance variables of healthy people and patients with knee osteoarthritis are shown in Table 2.
The relationship between the static balance variables and the fear of falling scale is shown in Table 3.
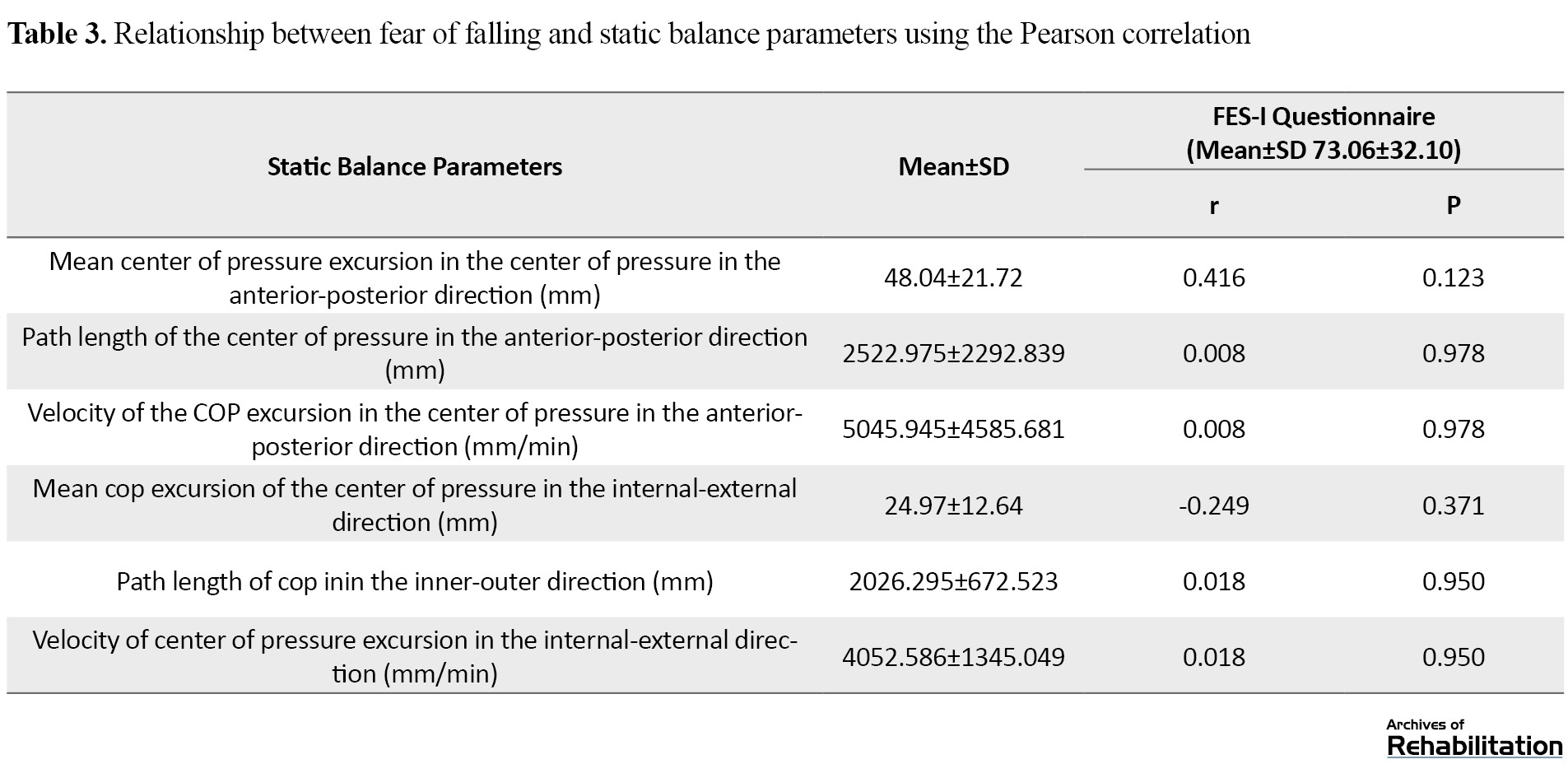
Based on the results of the present study, there is a significant statistical difference between the static balance parameters of the two study groups (P>0.05). Also, based on the results of the balance analysis of the patients, there was a direct relationship between the fluctuations of the body pressure center in the anterior-posterior direction and the scale of fear of falling, but it was not statistically significant (r=0.416, P=0.123). An inverse relationship existed between the fluctuations of the body’s center of pressure in the internal-external direction and the fear of falling scale (r=0.249, P=0.371). Also, no relationship was found between other parameters of the body pressure center and FES (r=0).
Dynamic balance parameters of patients compared to healthy people are presented in Table 4.
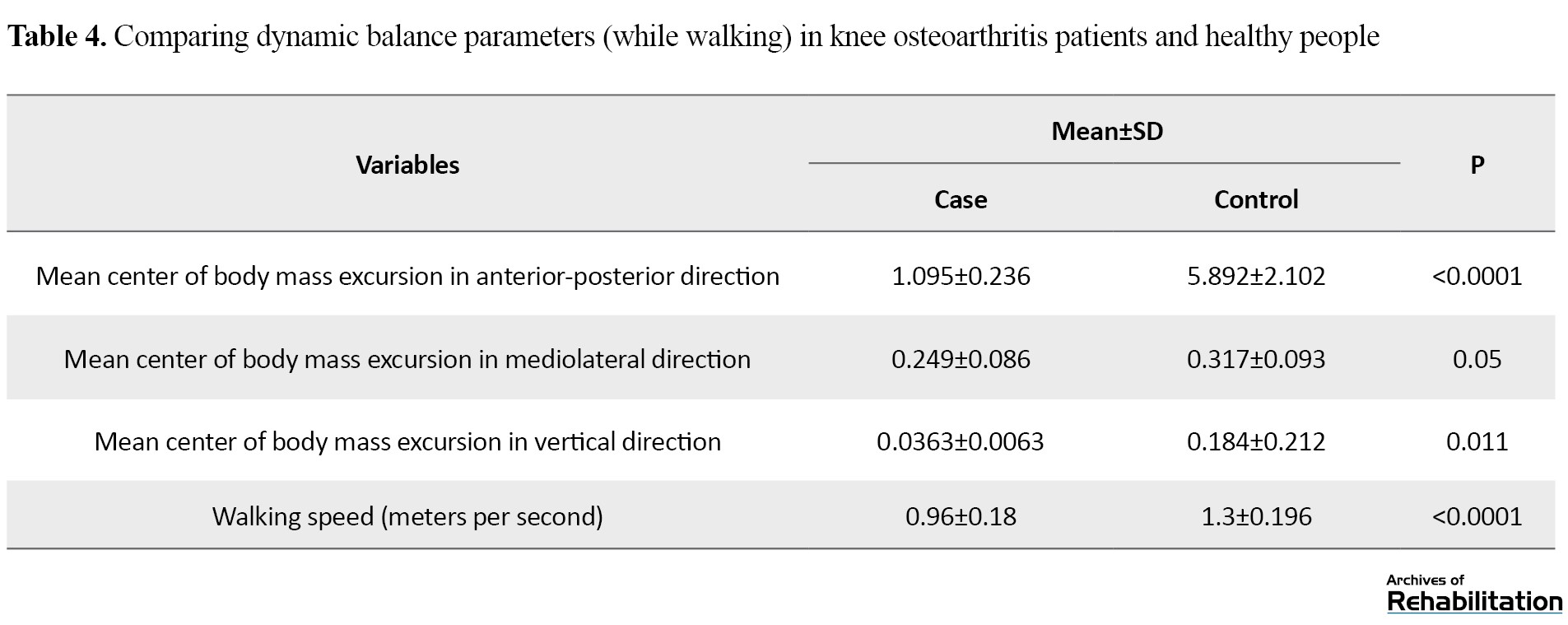
Based on the results, the number of parameters related to the fluctuations of the body’s center of mass in patients was significantly lower than the healthy individuals. Also, the measurement of the participants’ walking speed in the study showed that the amount of this variable in patients is significantly lower than in healthy people (0.96±0.18 compared to 1.3±0.196, P<0.05). The mean parameters of body center of gravity fluctuations and their relationship with the fear of falling scale are shown in Table 5.
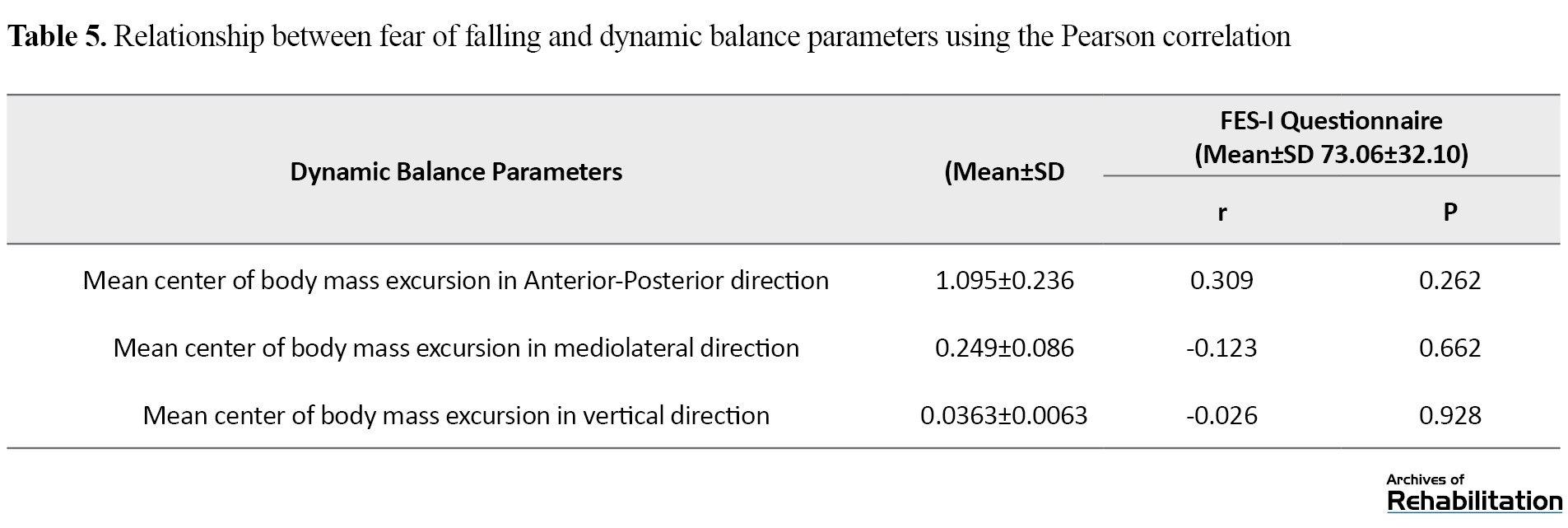
The relationship between the center of body mass fluctuations in the anterior-posterior, internal-external, and vertical directions and the fear of falling scale were obtained at 0.309, -0.123, and -0.026, respectively. However, these relationships were not statistically significant (P<0.05).
Based on the results, the Mean±SD FES scores in patients and healthy subjects were 32.73±10.06 and 18.13±1.35, respectively (P<0.05).
Discussion
Maintaining balance while standing and walking is important for daily activities. Many studies have shown that measuring balance during standing and walking can predict the risk of falling in people [33, 34]. The results of the present study showed that the COP in patients with knee osteoarthritis greatly fluctuates during standing, and therefore these patients have less static balance than healthy people (Table 1). This finding aligns with studies investigating the static balance of patients with knee osteoarthritis [9, 11, 12, 13, 35, 36, 37, 38]. The main reason for the decrease in the static balance of these patients compared to healthy people can be related to their limbs, disturbance in proprioception, and the decrease in patients’ muscle strength compared to healthy people.
The results of the present study showed that the fluctuations of the plantar pressure center in the anterior-posterior and internal-external directions have a direct and inverse relationship with the scale of fear of falling, respectively. However, this relationship was not statistically significant. The present study’s results align with the results of Taglietti et al. [13]. In their study, as in the current study, no significant relationship was found between the parameters of the plantar pressure center and the FES scale. This result may happen because the plantar pressure center variables do not represent performance. Therefore it is incorrect to relate the plantar pressure center variables to people’s confidence to perform daily activities [13]. It has also been stated that people’s emotions and stress affect the results of the FES questionnaire [24]. Therefore, although in the current study, similar to previous studies, the stability of knee osteoarthritis patients is less than in normal people, there was no significant statistical relationship between the variables of the body’s COP and the variables of the body’s center of mass with the FES scale. Another reason for this finding could be the inclusion of people with unilateral osteoarthritis in the current study so that in some studies reporting balance disorders in these patients, people with bilateral knee osteoarthritis were examined [19, 25, 36]. Also, the current study’s balance measurement tool differs from previous studies.
Another variable examined in the present study was dynamic balance. Based on the results, the fluctuation in the body’s center of mass and walking speed in patients were lower than that of healthy people (Table 4). Walking speed is an important variable in evaluating the dynamic balance of people [32]. A higher walking speed requires more dynamic balance [39, 40]. If the walking speed were constant, the decrease in the body’s center of mass fluctuations would indicate increased dynamic balance during walking [32]. In contrast, the decrease in the body’s center of mass fluctuations in both anterior-posterior and internal-external directions was obtained with a decrease in walking speed. In patients, this issue indicates a decreased dynamic balance [32]. The decrease in the walking speed of these patients compared to healthy people can be due to their greater fear of falling [41] or due to the presence of posture flexion in the joints of the lower limbs of patients with knee osteoarthritis (ankle dorsiflexion and joint flexion, knee, and hip) and therefore decrease the range of motion of these joints in the sagittal plane (flexion-extension of hip and knee joints) compared to healthy people [35].
Based on the results of the present study, there is no significant relationship between the body’s center of mass during walking and the fear of falling (P>0.05). In other words, the dynamic balance of knee osteoarthritis patients is not responsible for their fear of falling during daily activities. One of the factors affecting the fear of falling is pain. Pain affects muscle strength and coordination, postural fluctuations, strength, movement, and the ability to walk and increases the risk of falling [12, 42]. Therefore, in the present study, considering the lack of correlation between balance parameters and fear of falling, patients’ mild to moderate pain can be a possible reason for their greater fear of falling during daily activities compared to healthy people. Therefore, it is recommended that in future studies, in addition to investigating the effect of different severities of osteoarthritis on patients’ balance, the variable of pain also be measured as a risk factor in the occurrence of falls and the fear of falling. Also, to determine the net effect of balance disorder on the level of fear of falling in these patients, it is necessary to investigate and control other factors that are effective in causing falls, such as visual, vestibular, somatosensory, proprioceptive, and muscle strength disorders.
Conclusion
Based on the results of the present study, patients with knee osteoarthritis have less balance during standing and walking than healthy people. There is no significant relationship between the static and dynamic balance variables of people with mild to moderate knee osteoarthritis (respectively, based on the body pressure center and center of body mass) and the fear of falling scale. Therefore, to improve the functional abilities of these patients, the therapist should focus on other parameters affecting falls, such as reducing pain, improving muscle strength, and proprioception.
Ethical Considerations
Compliance with ethical guidelines
Research approved by Isfahan University of Medical Sciences (Code: 042.2.1396.REC.MUI.IRIs). Before conducting the test, all participants were informed completelly about the purpose and the study method. A consent form was taken from them. Also to the participants were allowed to excluded from the study whenever willing to stop the cooperation.
Funding
This project was funded by Isfahan University of Medical Sciences (Grant No.: 296042).
Authors' contributions
Conceptualization and idea: Mahsa Kavyani Boroujeni and Mohammad Taghi Karimi; Research and review: Mahsa Kavyani Boroujeni, Mohammad Taghi Karimi and Hossein Akbari Aghdam, Analysis: Mahsa Kaviani and Kivan Sharif Moradi; Editing and finalisiation: Mahsa Kavyani Boroujeni and Mohammad Taghi Karimi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants took part in this research.
References
Osteoarthritis is one of the most common knee joint disorders. Epidemiological studies show that about 17% of Iran’s population has knee osteoarthritis [1]. Knee osteoarthritis is considered one of the risk factors for falling in elderly people [2, 3, 4]. Vision disorders, decreased muscle strength and activity, knee joint proprioceptive disorder, and balance disorder are the most important factors affecting falls in patients with knee osteoarthritis [4, 5, 6]. Whether injured or not, patients who fall are afraid of falling again and therefore limit their functional activities to prevent a possible fall. This condition will restrict patients’ mobility, cause muscle weakness, and increase the risk of falling in the future [7]. It has also been stated that there is a fear of falling in adults with or without a history of falling [8].
Maintaining balance is essential for daily activities [9, 10]. Several studies have shown that patients with knee osteoarthritis have greater postural fluctuations than healthy people [9, 11, 12, 13]. Afferent sensory data from vision, vestibular, and somatosensory systems participate in balance control. The central processing of this information leads to a neuromuscular response that maintains the body’s center of gravity within the range of body support [14]. Therefore, balance disorder increases the risk of falling and reduces the ability to walk.
One of the methods to evaluate postural balance is using a force plate that measures postural fluctuations during standing or walking [15, 16, 17, 18]. Confusion of postural volatility is the main cause of falling and fear of its recurrence in patients with knee osteoarthritis; also, falling is the cause of secondary injuries to patients. Therefore, evaluating the relationship between balance and the fear of falling in patients with knee osteoarthritis can lead to diagnosing the mechanism of disability and falling and help find effective treatment methods for them [9, 19].
Several studies have investigated postural balance and the risk of falling in elderly people and patients with knee osteoarthritis [19-25]. In these studies, the balance has been evaluated with several clinical tests [20, 21, 22], including the functional reach test, step test [21], and timed up and go test [19, 20]. Also, systems such as NeuroCom Balance Master [21] and Biodex are used in this regard [19, 23, 24]. In these studies, balance and its relationship with the fear of falling have often been measured using clinical tests. In contrast, the NeuroCom and the Biodex balance systems are used to assess postural balance, and balance during walking has not been used in all previous studies. Therefore, the current study aims to evaluate the dynamic balance of patients with knee osteoarthritis compared to healthy people (exclusively during walking and based on the fluctuations of the body’s center of pressure and the body’s center of gravity) and to evaluate the static balance using biomechanical parameters (fluctuations of the plantar pressure center) and its relationship with fear of falling.
Materials and Methods
The current research is descriptive cross-sectional. Regarding confounding variables, 15 patients with mild to moderate knee osteoarthritis and 15 healthy individuals matched with the patient group participated in this study (Table 1).
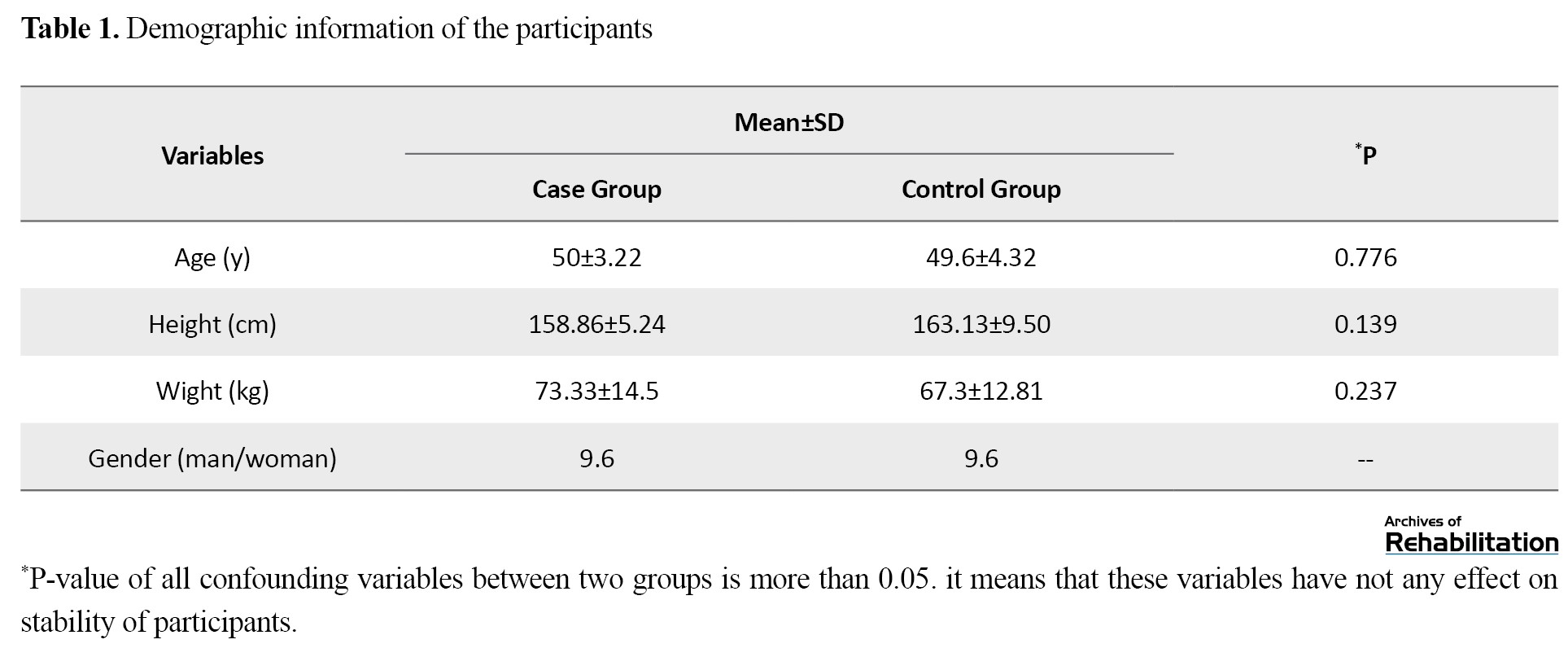
The P>0.05 for all confounding variables between the two groups, which means that the variables are ineffective in the balance of the participants.
The inclusion criteria in the selected patients were as follows: having mild to moderate severity of knee osteoarthritis, mild to moderate pain intensity (based on the VAS scale, mild pain=0-3, moderate pain=4-6) [26, 27], being independent in performing daily activities, lacking any skeletal-muscular disorder affecting people’s ability to walk and stand, and the ability to walk without any assistive devices. Patients with a history of knee surgery and lower limb fracture, a history of falls, and patients undergoing physiotherapy treatment or drug treatment affecting balance, such as sedatives, were excluded from the study.
The international fall efficacy scale (FES-I) was used to assess the fear of falling. The patients’ balance was evaluated in static and dynamic situations (standing and walking, respectively).
The process of performing the balance test
To check the static balance of the participants in the study, a Kistler force plate (60×50 cm, model 9260AA, manufactured by Kistler, Switzerland) was used to collect the data of the center of body pressure (COP) along the x and y axes, which represent the anterior-posterior and internal-external directions, respectively. The data were collected with a frequency of 100 Hz and filtered with a Butterworth low-pass filter with a cut off frequency of 10 hz [28, 29].
Standing stability of participants in study was measured based on following equations (Equations 1-6):
COPEAP: Center of pressure excursion in the anteroposterior direction, COPEML: Center of pressure excursion in the mediolateral direction, PLAP: Path length of COP in the anteroposterior direction, LML: Path length of COP in the mediolateral direction, VAP: Velocity of center of pressure sways in the anteroposterior plane, VML: Velocity of center of pressure sways in the mediolateral plane.
The dynamic balance of the participants in the study was determined based on the relationship between the body’s center of mass (COM) and the range of the base of support (BOS) in anterior-posterior and internal-external directions [30, 31, 32]. The kinematic information of people’s walking was collected using the Qualisys motion analysis system equipped with 7 cameras and a frequency of 100 Hz. Twenty reflective markers with a diameter of 14 mm were pasted on the anatomical landmarks [31]. Markers were named and defined in Tract Manager software version 2.7 (Analysis Motion Capture Company, Gothenburg, Sweden). The right and left legs, both sides of the calf, pelvis, trunk, and head, were modeled. The main parameters for assessing dynamic balance are the normalized displacement of the body’s COM in anterior-posterior, internal-external, and vertical directions and walking speed.
Statistical analysis of data was done with SPSS software, version 16 (Chicago, SPSS Inc). To check the normal distribution of data, the Shapiro-Wilk test was used. To compare the balance of patients and healthy people, the independent samples t-test was used. The relationship between static and dynamic balance parameters and fear of falling was measured using the Pearson correlation coefficient.
Results
The static balance variables of healthy people and patients with knee osteoarthritis are shown in Table 2.
The relationship between the static balance variables and the fear of falling scale is shown in Table 3.
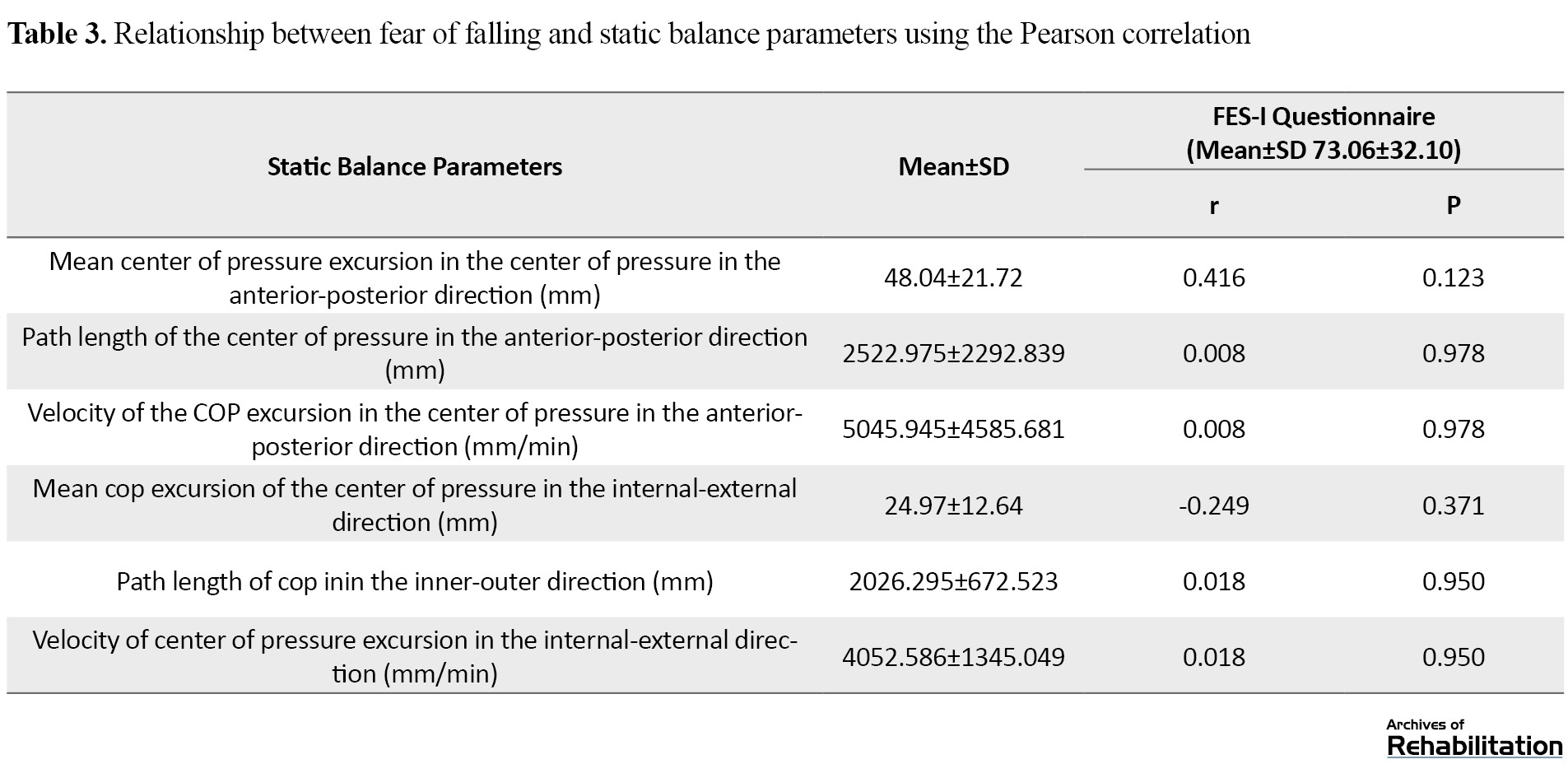
Based on the results of the present study, there is a significant statistical difference between the static balance parameters of the two study groups (P>0.05). Also, based on the results of the balance analysis of the patients, there was a direct relationship between the fluctuations of the body pressure center in the anterior-posterior direction and the scale of fear of falling, but it was not statistically significant (r=0.416, P=0.123). An inverse relationship existed between the fluctuations of the body’s center of pressure in the internal-external direction and the fear of falling scale (r=0.249, P=0.371). Also, no relationship was found between other parameters of the body pressure center and FES (r=0).
Dynamic balance parameters of patients compared to healthy people are presented in Table 4.
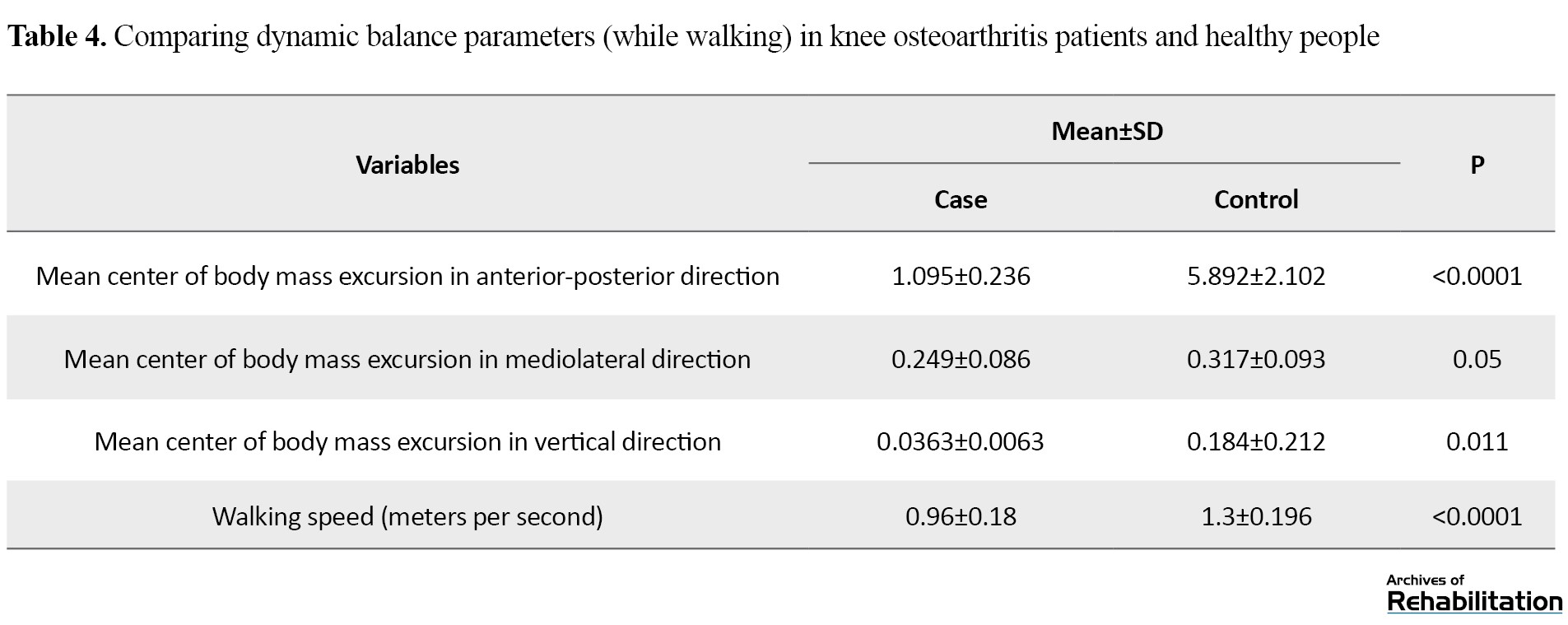
Based on the results, the number of parameters related to the fluctuations of the body’s center of mass in patients was significantly lower than the healthy individuals. Also, the measurement of the participants’ walking speed in the study showed that the amount of this variable in patients is significantly lower than in healthy people (0.96±0.18 compared to 1.3±0.196, P<0.05). The mean parameters of body center of gravity fluctuations and their relationship with the fear of falling scale are shown in Table 5.
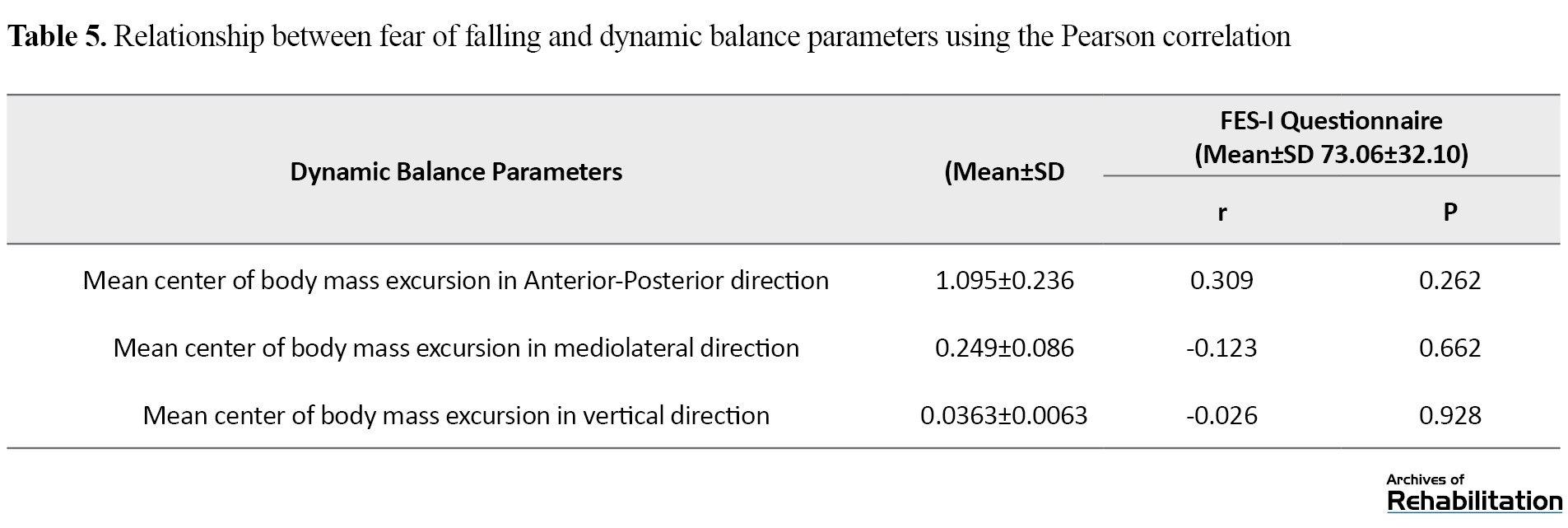
The relationship between the center of body mass fluctuations in the anterior-posterior, internal-external, and vertical directions and the fear of falling scale were obtained at 0.309, -0.123, and -0.026, respectively. However, these relationships were not statistically significant (P<0.05).
Based on the results, the Mean±SD FES scores in patients and healthy subjects were 32.73±10.06 and 18.13±1.35, respectively (P<0.05).
Discussion
Maintaining balance while standing and walking is important for daily activities. Many studies have shown that measuring balance during standing and walking can predict the risk of falling in people [33, 34]. The results of the present study showed that the COP in patients with knee osteoarthritis greatly fluctuates during standing, and therefore these patients have less static balance than healthy people (Table 1). This finding aligns with studies investigating the static balance of patients with knee osteoarthritis [9, 11, 12, 13, 35, 36, 37, 38]. The main reason for the decrease in the static balance of these patients compared to healthy people can be related to their limbs, disturbance in proprioception, and the decrease in patients’ muscle strength compared to healthy people.
The results of the present study showed that the fluctuations of the plantar pressure center in the anterior-posterior and internal-external directions have a direct and inverse relationship with the scale of fear of falling, respectively. However, this relationship was not statistically significant. The present study’s results align with the results of Taglietti et al. [13]. In their study, as in the current study, no significant relationship was found between the parameters of the plantar pressure center and the FES scale. This result may happen because the plantar pressure center variables do not represent performance. Therefore it is incorrect to relate the plantar pressure center variables to people’s confidence to perform daily activities [13]. It has also been stated that people’s emotions and stress affect the results of the FES questionnaire [24]. Therefore, although in the current study, similar to previous studies, the stability of knee osteoarthritis patients is less than in normal people, there was no significant statistical relationship between the variables of the body’s COP and the variables of the body’s center of mass with the FES scale. Another reason for this finding could be the inclusion of people with unilateral osteoarthritis in the current study so that in some studies reporting balance disorders in these patients, people with bilateral knee osteoarthritis were examined [19, 25, 36]. Also, the current study’s balance measurement tool differs from previous studies.
Another variable examined in the present study was dynamic balance. Based on the results, the fluctuation in the body’s center of mass and walking speed in patients were lower than that of healthy people (Table 4). Walking speed is an important variable in evaluating the dynamic balance of people [32]. A higher walking speed requires more dynamic balance [39, 40]. If the walking speed were constant, the decrease in the body’s center of mass fluctuations would indicate increased dynamic balance during walking [32]. In contrast, the decrease in the body’s center of mass fluctuations in both anterior-posterior and internal-external directions was obtained with a decrease in walking speed. In patients, this issue indicates a decreased dynamic balance [32]. The decrease in the walking speed of these patients compared to healthy people can be due to their greater fear of falling [41] or due to the presence of posture flexion in the joints of the lower limbs of patients with knee osteoarthritis (ankle dorsiflexion and joint flexion, knee, and hip) and therefore decrease the range of motion of these joints in the sagittal plane (flexion-extension of hip and knee joints) compared to healthy people [35].
Based on the results of the present study, there is no significant relationship between the body’s center of mass during walking and the fear of falling (P>0.05). In other words, the dynamic balance of knee osteoarthritis patients is not responsible for their fear of falling during daily activities. One of the factors affecting the fear of falling is pain. Pain affects muscle strength and coordination, postural fluctuations, strength, movement, and the ability to walk and increases the risk of falling [12, 42]. Therefore, in the present study, considering the lack of correlation between balance parameters and fear of falling, patients’ mild to moderate pain can be a possible reason for their greater fear of falling during daily activities compared to healthy people. Therefore, it is recommended that in future studies, in addition to investigating the effect of different severities of osteoarthritis on patients’ balance, the variable of pain also be measured as a risk factor in the occurrence of falls and the fear of falling. Also, to determine the net effect of balance disorder on the level of fear of falling in these patients, it is necessary to investigate and control other factors that are effective in causing falls, such as visual, vestibular, somatosensory, proprioceptive, and muscle strength disorders.
Conclusion
Based on the results of the present study, patients with knee osteoarthritis have less balance during standing and walking than healthy people. There is no significant relationship between the static and dynamic balance variables of people with mild to moderate knee osteoarthritis (respectively, based on the body pressure center and center of body mass) and the fear of falling scale. Therefore, to improve the functional abilities of these patients, the therapist should focus on other parameters affecting falls, such as reducing pain, improving muscle strength, and proprioception.
Ethical Considerations
Compliance with ethical guidelines
Research approved by Isfahan University of Medical Sciences (Code: 042.2.1396.REC.MUI.IRIs). Before conducting the test, all participants were informed completelly about the purpose and the study method. A consent form was taken from them. Also to the participants were allowed to excluded from the study whenever willing to stop the cooperation.
Funding
This project was funded by Isfahan University of Medical Sciences (Grant No.: 296042).
Authors' contributions
Conceptualization and idea: Mahsa Kavyani Boroujeni and Mohammad Taghi Karimi; Research and review: Mahsa Kavyani Boroujeni, Mohammad Taghi Karimi and Hossein Akbari Aghdam, Analysis: Mahsa Kaviani and Kivan Sharif Moradi; Editing and finalisiation: Mahsa Kavyani Boroujeni and Mohammad Taghi Karimi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants took part in this research.
References
- Davatchi F, Sandoughi M, Moghimi N, Jamshidi AR, Tehrani Banihashemi A, Zakeri Z, et al. Epidemiology of rheumatic diseases in Iran from analysis of four COPCORD studies. International Journal of Rheumatic Diseases. 2016; 19(11):1056-62. [DOI:10.1111/1756-185X.12809] [PMID]
- Hawker GA. Osteoarthritis is a serious disease. Clinical and Experimental Rheumatology. 2019; 37(Suppl 120):3-6. [PMID]
- Jadelis K, Miller ME, Ettinger Jr WH, Messier SP. Strength, balance, and the modifying effects of obesity and knee pain: Results from the observational arthritis study in seniors (OASIS). Journal of the American Geriatrics Society. 2001; 49(7):884-91. [DOI:10.1046/j.1532-5415.2001.49178.x] [PMID]
- Martin JA, Buckwalter JA. Aging, articular cartilage chondrocyte senescence and osteoarthritis. Biogerontology. 2002; 3(5):257-64. [DOI:10.1023/A:1020185404126] [PMID]
- Loeser RF. The role of aging in the development of osteoarthritis. Transactions of the American Clinical and Climatological Association. 2017; 128:44. [PMID] [PMCID]
- Khalaj N, Abu Osman NA, Mokhtar AH, Mehdikhani M, Wan Abas WA. Balance and risk of fall in individuals with bilateral mild and moderate knee osteoarthritis. Plos One. 2014; 9(3):e92270. [DOI:10.1371/journal.pone.0092270] [PMID] [PMCID]
- Alkan BM, Fidan F, Tosun A, Ardıçoğlu Ö. Quality of life and self-reported disability in patients with knee osteoarthritis. Modern Rheumatology. 2014; 24(1):166-71. [DOI:10.3109/14397595.2013.854046] [PMID]
- Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009; 302(20):2214-21. [DOI:10.1001/jama.2009.1738] [PMID] [PMCID]
- Ng CT, Tan MP. Osteoarthritis and falls in the older person. Age and Ageing. 2013; 42(5):561-6. [DOI:10.1093/ageing/aft070] [PMID]
- Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR. Physiological risk factors for falls in older people with lower limb arthritis. The Journal of Rheumatology. 2004; 31(11):2272-9. [PMID]
- Brand C, Aw J, Lowe A, Morton C. Prevalence, outcome and risk for falling in 155 ambulatory patients with rheumatic disease. APLAR Journal of Rheumatology. 2005; 8(2):99-105. [DOI:10.1111/j.1479-8077.2005.00136.x]
- Williams SB, Brand CA, Hill KD, Hunt SB, Moran H. Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: A pilot study. Archives of Physical Medicine and Rehabilitation. 2010; 91(1):106-14. [DOI:10.1016/j.apmr.2009.08.150] [PMID]
- Rombaut L, Malfait F, De Wandele I, Thijs Y, Palmans T, De Paepe A, et al. Balance, gait, falls, and fear of falling in women with the hypermobility type of Ehlers-Danlos syndrome. Arthritis Care & Research. 2011; 63(10):1432-9. [DOI:10.1002/acr.20557] [PMID]
- Scheffer AC, Schuurmans MJ, Van Dijk N, Van Der Hooft T, De Rooij SE. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing. 2008; 37(1):19-24. [DOI:10.1093/ageing/afm169] [PMID]
- Lord SR, Menz HB, Tiedemann A. A physiological profile approach to falls risk assessment and prevention. Physical Therapy. 2003; 83(3):237-52. [DOI:10.1093/ptj/83.3.237] [PMID]
- Manlapaz DG, Sole G, Jayakaran P, Chapple CM. Risk factors for falls in adults with knee osteoarthritis: A systematic review. PM&R. 2019; 11(7):745-57. [DOI:10.1002/pmrj.12066] [PMID]
- Hinman R, Bennell K, Metcalf B, Crossley K. Balance impairments in individuals with symptomatic knee osteoarthritis: A comparison with matched controls using clinical tests. Rheumatology. 2002; 41(12):1388-94. [DOI:10.1093/rheumatology/41.12.1388] [PMID]
- Takacs J, Carpenter MG, Garland SJ, Hunt MA. The role of neuromuscular changes in aging and knee osteoarthritis on dynamic postural control. Aging and Disease. 2013; 4(2):84. [PMID] [PMCID]
- Foley S, Lord SR, Srikanth V, Cooley H, Jones G. Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian older adult cohort study. Osteoarthritis and Cartilage. 2006; 14(6):533-9. [DOI:10.1016/j.joca.2005.12.007] [PMID]
- de Zwart AH, van der Esch M, Pijnappels MA, Hoozemans MJ, van der Leeden M, Roorda LD, et al. Falls associated with muscle strength in patients with knee osteoarthritis and self-reported knee instability. The Journal of Rheumatology. 2015; 42(7):1218-23. [DOI:10.3899/jrheum.140517] [PMID]
- Prata MG, Scheicher ME. Correlation between balance and the level of functional independence among elderly people. Sao Paulo Medical Journal. 2012; 130:97-101. [DOI:10.1590/S1516-31802012000200005] [PMID]
- Masui T, Hasegawa Y, Yamaguchi J, Kanoh T, Ishiguro N, Suzuki S. Increasing postural sway in rural-community-dwelling elderly persons with knee osteoarthritis. Journal of Orthopaedic Science. 2006; 11(4):353-8. [DOI:10.1007/s00776-006-1034-9] [PMID]
- Hassan B, Mockett S, Doherty M. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Annals of the Rheumatic Diseases. 2001; 60(6):612-8. [DOI:10.1136/ard.60.6.612] [PMID] [PMCID]
- Taglietti M, Bela LFD, Dias JM, Pelegrinelli ARM, Nogueira JF, Júnior JPB, et al. Postural sway, balance confidence, and fear of falling in women with knee osteoarthritis in comparison to matched controls. PM&R. 2017; 9(8):774-80. [DOI:10.1016/j.pmrj.2016.11.003] [PMID]
- Gaerlan MG. The role of visual, vestibular, and somatosensory systems in postural balance [MSc thesis]. Las Vegas: University of Nevada; 2010. [DOI:10.1111/j.1745-7599.2012.00699.x]
- Browne J, O’Hare N. Review of the different methods for assessing standing balance. Physiotherapy. 2001; 87(9):489-95. [DOI:10.1016/S0031-9406(05)60696-7]
- Karlsson A, Frykberg G. Correlations between force plate measures for assessment of balance. Clinical Biomechanics. 2000; 15(5):365-9. [DOI:10.1016/S0268-0033(99)00096-0] [PMID]
- Wikstrom EA, Tillman MD, Smith AN, Borsa PA. A new force-plate technology measure of dynamic postural stability: The dynamic postural stability index. Journal of Athletic Training. 2005; 40(4):305-9. [PMID] [PMCID]
- Lee CH, Sun TL. Evaluation of postural stability based on a force plate and inertial sensor during static balance measurements. Journal of Physiological Anthropology. 2018; 37(1):1-16. [DOI:10.1186/s40101-018-0187-5] [PMID] [PMCID]
- Niino N, Tsuzuku S, Ando F, Shimokata H. Frequencies and circumstances of falls in the national institute for longevity sciences, longitudinal study of aging (NILS-LSA). Journal of Epidemiology. 2000; 10(1sup):90-4. [DOI:10.2188/jea.10.1sup_90] [PMID]
- Higuchi Y, Sudo H, Tanaka N, Fuchioka S, Hayashi Y. Does fear of falling relate to low physical function in frail elderly persons?: Associations of fear of falling, balance, and gait. Journal of the Japanese Physical Therapy Association. 2004; 7(1):41-7. [DOI:10.1298/jjpta.7.41] [PMID] [PMCID]
- Hill KD, Williams SB, Chen J, Moran H, Hunt S, Brand C. Balance and falls risk in women with lower limb osteoarthritis or rheumatoid arthritis. Journal of Clinical Gerontology and Geriatrics. 2013; 4(1):22-8. [DOI:10.1016/j.jcgg.2012.10.003]
- Sánchez-Herán Á, Agudo-Carmona D, Ferrer-Peña R, López-de-Uralde-Villanueva I, Gil-Martínez A, Paris-Alemany A, et al. Postural stability in osteoarthritis of the knee and hip: Analysis of association with pain catastrophizing and fear-avoidance beliefs. PM&R. 2016; 8(7):618-28. [DOI:10.1016/j.pmrj.2015.11.002] [PMID]
- Hsieh RL, Lee WC, Lo MT, Liao WC. Postural stability in patients with knee osteoarthritis: Comparison with controls and evaluation of relationships between postural stability scores and international classification of functioning, disability and health components. Archives of Physical Medicine and Rehabilitation. 2013; 94(2):340-6. [DOI:10.1016/j.apmr.2012.09.022] [PMID]
- Aydoğ E, Bal A, Aydoğ ST, Çakci A. Evaluation of dynamic postural balance using the biodex stability system in rheumatoid arthritis patients. Clinical Rheumatology. 2006; 25(4):462. [DOI:10.1007/s10067-005-0074-4] [PMID]
- Wegener L, Kisner C, Nichols D. Static and dynamic balance responses in persons with bilateral knee osteoarthritis. Journal of Orthopaedic & Sports Physical Therapy. 1997; 25(1):13-8. [DOI:10.2519/jospt.1997.25.1.13] [PMID]
- Almeida GPL, Monteiro IO, Marizeiro DF, Maia LB, de Paula Lima PO. Y balance test has no correlation with the stability index of the biodex balance system. Musculoskeletal Science and Practice. 2017; 27:1-6. [DOI:10.1016/j.msksp.2016.11.008] [PMID]
- Arifin N, Osman NAA, Abas WABW. Intrarater test-retest reliability of static and dynamic stability indexes measurement using the biodex stability system during unilateral stance. Journal of Applied Biomechanics. 2014; 30(2):300-4. [DOI:10.1123/jab.2013-0130] [PMID]
- McAndrew Young PM, Wilken JM, Dingwell JB. Dynamic margins of stability during human walking in destabilizing environments. Journal of Biomechanics. 2012; 45(6):1053-9. [DOI:10.1016/j.jbiomech.2011.12.027] [PMID] [PMCID]
- Bhatt T, Espy D, Yang F, Pai YC. Dynamic gait stability, clinical correlates, and prognosis of falls among community-dwelling older adults. Archives of Physical Medicine and Rehabilitation. 2011; 92(5):799-805. [DOI:10.1016/j.apmr.2010.12.032] [PMID]
- Toebes MJ, Hoozemans MJ, Furrer R, Dekker J, van Dieën JH. Local dynamic stability and variability of gait are associated with fall history in elderly subjects. Gait & Posture. 2012; 36(3):527-31. [DOI:10.1016/j.gaitpost.2012.05.016] [PMID]
- Torres L, Dunlop DD, Peterfy C, Guermazi A, Prasad P, Hayes KW, et al. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis and Cartilage. 2006; 14(10):1033-40. [DOI:10.1016/j.joca.2006.03.015] [PMID]
- Krebs EE, Carey TS, Weinberger M. Accuracy of the pain numeric rating scale as a screening test in primary care. Journal of general Internal Medicine. 2007; 22(10):1453-8. [DOI:10.1007/s11606-007-0321-2] [PMID] [PMCID]
- Mosallanezhad Z, Salavati M, Hellström K, Reza Sotoudeh G, Nilsson Wikmar L, Frändin K. Cross-cultural adaptation, reliability and validity of the Persian version of the modified falls efficacy scale. Disability and Rehabilitation. 2011; 33(25-26):2446-53. [DOI:10.3109/09638288.2011.574774] [PMID]
- Mat S, Ng CT, Fadzil F, Rozalli FI, Tan MP. The mediating role of psychological symptoms on falls risk among older adults with osteoarthritis. Clinical Interventions in Aging. 2017; 12:2025. [DOI:10.2147/CIA.S149991] [PMID] [PMCID]
- Akbari Aghdam H, Kavyani M, Bosak M, Karimi MT, Motififard M. Evaluation of the stability of the subjects with anterior cruciate injuries reconstruction. The Journal of Knee Surgery. 2021; 34(14):1527-30. [DOI:10.1055/s-0040-1710374] [PMID]
- Salavati M, Hadian MR, Mazaheri M, Negahban H, Ebrahimi I, Talebian S, et al. Test-retest reliabty of center of pressure measures of postural stability during quiet standing in a group with musculoskeletal disorders consisting of low back pain, anterior cruciate ligament injury and functional ankle instability. Gait & Posture. 2009; 29(3):460-4. [DOI:10.1016/j.gaitpost.2008.11.016] [PMID]
- Doyle TL, Newton RU, Burnett AF. Reliability of traditional and fractal dimension measures of quiet stance center of pressure in young, healthy people. Archives of Physical Medicine and Rehabilitation. 2005; 86(10):2034-40. [DOI:10.1016/j.apmr.2005.05.014] [PMID]
- Swanenburg J, de Bruin ED, Favero K, Uebelhart D, Mulder T. The reliability of postural balance measures in single and dual tasking in elderly fallers and non-fallers. BMC Musculoskeletal disorders. 2008; 9. [DOI:10.1186/1471-2474-9-162] [PMID] [PMCID]
- Lafond D, Corriveau H, Hébert R, Prince F. Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people. Archives of Physical Medicine and Rehabilitation. 2004; 85(6):896-901. [DOI:10.1016/j.apmr.2003.08.089] [PMID]
- Karimi M, Kaviani Borojeni M. Stability analysis theories, strategies and mechanisms of evaluation. Sunnyvale: Lap Lambert Academic Publishing; 2016. [Link]
- Karimi M, Kargar H, Zolaktaf V. Evaluation of the dynamic stability of individuals with spinal cord injury. Technology and Disability. 2015; 27(4):155-60. [DOI:10.3233/TAD-160437]
- Sharifmoradi K, Farahpour N, Karimi MT, Bahram A. Analysis of dynamic balance during walking in patients with parkinson’s disease & able-bodied elderly people. Physical Treatments-Specific Physical Therapy Journal. 2015; 4(4):191-8. [Link]
- Perry SD, Bombardier E, Radtke A, Tiidus PM. Hormone replacement and strength training positively influence balance during gait in post-menopausal females: A pilot study. Journal of Sports Science & Medicine. 2005; 4(4):372. [PMID] [PMCID]
- Perry SD, Radtke A, Goodwin CR. Influence of footwear midsole material hardness on dynamic balance control during unexpected gait termination. Gait & Posture. 2007; 25(1):94-8. [DOI:10.1016/j.gaitpost.2006.01.005] [PMID]
- Morris R, Harwood RH, Baker R, Sahota O, Armstrong S, Masud T. A comparison of different balance tests in the prediction of falls in older women with vertebral fractures: A cohort study. Age and Ageing; 2007; 36(1):78–83. [DOI:10.1093/ageing/afl147] [PMID]
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Physical Therapy. 2000; 80(9):896-903. [DOI:10.1093/ptj/80.9.896] [PMID]
- Kim HS, Yun DH, Yoo SD, Kim DH, Jeong YS, Yun JS, et al. Balance control and knee osteoarthritis severity. Annals of Rehabilitation Medicine. 2011; 35(5):701-9. [DOI:10.5535/arm.2011.35.5.701] [PMID] [PMCID]
- Park HJ, Ko S, Hong HM, Ok E, Lee JI. Factors related to standing balance in patients with knee osteoarthritis. Annals of Rehabilitation Medicine. 2013; 37(3):373-8. [DOI:10.5535/arm.2013.37.3.373] [PMID] [PMCID]
- Santos BR, Delisle A, Larivière C, Plamondon A, Imbeau D. Reliability of centre of pressure summary measures of postural steadiness in healthy young adults. Gait & Posture. 2008; 27(3):408-15. [DOI:10.1016/j.gaitpost.2007.05.008] [PMID]
- Esrafilian A, Karimi MT, Amiri P, Fatoye F. Performance of subjects with knee osteoarthritis during walking: Differential parameters. Rheumatology International. 2013; 33(7):1753-61. [DOI:10.1007/s00296-012-2639-2] [PMID]
- Lawson T, Morrison A, Blaxland S, Wenman M, Schmidt CG, Hunt MA. Laboratory-based measurement of standing balance in individuals with knee osteoarthritis: A systematic review. Clinical Biomechanics. 2015; 30(4):330-42. [DOI:10.1016/j.clinbiomech.2015.02.011] [PMID]
- Buzzi UH, Ulrich BD. Dynamic stability of gait cycles as a function of speed and system constraints. Motor Control. 2004; 8(3):241-54. [DOI:10.1123/mcj.8.3.241] [PMID] [PMCID]
- Dingwell JB, Cusumano JP, Sternad D, Cavanagh PR. Slower speeds in patients with diabetic neuropathy lead to improved local dynamic stability of continuous overground walking. Journal of Biomechanics. 2000; 33(10):1269-77. [DOI:10.1016/S0021-9290(00)00092-0] [PMID]
- Chamberlin ME, Fulwider BD, Sanders SL, Medeiros JM. Does fear of falling influence spatial and temporal gait parameters in elderly persons beyond changes associated with normal aging? The Journals of Gerontology Series A. 2005; 60(9):1163-7. [DOI:10.1093/gerona/60.9.1163] [PMID]
- Al-Zahrani K, Bakheit A. A study of the gait characteristics of patients with chronic osteoarthritis of the knee. Disability and Rehabilitation. 2002; 24(5):275-80. [DOI:10.1080/09638280110087098] [PMID]
Type of Study: Original |
Subject:
Elderly
Received: 31/10/2021 | Accepted: 15/03/2022 | Published: 1/01/2023
Received: 31/10/2021 | Accepted: 15/03/2022 | Published: 1/01/2023
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |