Volume 21, Issue 4 (Winter 2021)
jrehab 2021, 21(4): 488-507 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Maarouf A, Norasteh A A, Daneshmandi H, Ebrahimi Atri A. The Effect of a Corrective Exercise Program Based on Scapula Stability on Scapular Upward Rotation and Scapulohumeral Rhythm in Wheelchair Basketball Athletes With Bilateral Scapula Rotational Syndrome. jrehab 2021; 21 (4) :488-507
URL: http://rehabilitationj.uswr.ac.ir/article-1-2720-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-2720-en.html
1- Department of Sports Injuries & Corrective Exercise, School of Physical Education and Sport Sciences, University of Guilan, Rasht, Iran. , abed.maaroof93@gmail.com
2- Department of Sports Injuries & Corrective Exercise, School of Physical Education and Sport Sciences, University of Guilan, Rasht, Iran.
3- Department of Sports Injuries & Corrective Exercise, School of Physical Education and Sport Sciences, Ferdowsi University, Mashhad, Iran.
2- Department of Sports Injuries & Corrective Exercise, School of Physical Education and Sport Sciences, University of Guilan, Rasht, Iran.
3- Department of Sports Injuries & Corrective Exercise, School of Physical Education and Sport Sciences, Ferdowsi University, Mashhad, Iran.
Full-Text [PDF 7004 kb]
(2418 Downloads)
| Abstract (HTML) (6107 Views)
Full-Text: (6369 Views)
Introduction
thletes who mainly use their upper limbs in sports usually complain of shoulder disorders and pain [1, 2]. Inman et al. were the first to measure scapulohumeral rhythm by radiography and suggested a 2:1 ratio for glenohumeral elevation and scapulothoracic upward rotation [3]. Some of the literature suggests the 2:1 ratio is not consistent across an entire arc of shoulder elevation and that variability in this ratio may increase when considering the scapulohumeral rhythm exhibited by shoulder injured subjects [5, 4]. Some previous studies have suggested that scapula muscle dysfunction can lead to abnormal alignment and upper limb dysfunction [6, 7]. One of the scapula’s abnormal problems is its low rotation syndrome, which causes the scapula to fall, drain, and tilt [8, 9]. Previous research in people who use wheelchairs examined their scapulae condition in activities such as translocation and weight loss [10, 11, 12]. According to these studies, changes in the scapula directions and movements and arm during these activities reduce the space under the acromion, which increases the risk of injury [10, 11, 12]. Transmissions in people who use wheelchairs are performed with compensatory changes in the scapula kinematics, maintaining space under the acromion during activity [11].
The previous scapula kinematics results of wheelchair drivers are mainly concluded from studies that have examined the scapula movements unilaterally (right or left) [13, 14, 15]. But wheelchair driving is a bilateral activity that requires coordination of both upper limbs, and therefore its symmetry cannot be ignored [16]. Although previous data show scapula asymmetry when driving in a wheelchair [16, 17, 18, 19, 20], we still need to research scapula movements bilaterally (right and left). Wheelchair players are at risk of overworked shoulder injuries due to the frequent use of their upper limbs to drive wheelchairs. Repeated wheelchair mechanisms cause repetitive scapular protrusions that can lead to postural changes, stabilizing muscle weakness, and anterior muscle stiffness. Compensatory muscle imbalances may be due to prolonged wheelchair use or defects in the rotator cuff and scapula stabilizers’ strength training programs. This condition can lead to musculoskeletal injuries in athletes who require different movement patterns (such as swimming, throwing, or racket sports) [21, 22]. However, it is unknown whether activation has a protective effect on the musculoskeletal system [23]. Previous studies in this field have investigated the scapulohumeral rhythm in injured people and healthy athletes. However, no studies have been performed on wheelchair basketball players, and the effect of exercise interventions on the scapula in these people has not been studied. Thus, we aimed to investigate the indexes of scapular upward rotation and scapulohumeral rhythm in wheelchair basketball players and see the exercise program’s results based on scapula stability on these indexes.
Materials and Methods
The research method is quasi-experimental. According to the research conditions, 24 wheelchair basketball players with spinal cord injuries participated in this study. First, 8 players from each sports class (sports class 1 to 1.5, sports class 2 to 2.5, and sports class 3 to 4.5) were selected. Then, four people from each sports class were randomly assigned to the control or experimental group (12 control and 12 experimental). Thus, an equal number of three sports classes were present in each group. Wheelchair basketball players were professional players in the Mashhad City League, Iran. The participants were classified according to the IWBF classification and the relevant sports classification from the Veterans and Disabled Sports Federation of the Islamic Republic of Iran (IRISFD), both of which are required for people with physical disabilities to participate in competitions. Individuals with a history of shoulder surgery, injury, and pain were excluded from the study 6 months before the test. Two digital inclinometers were used to measure the motion of the arm and scapula range at rest position and 45°, 90°, and 135° shoulder abduction angles at the scapula scaption surface. The study’s final results to measure the scapular upward rotation in resting positions (ICC=0.89) and angles 45° (ICC=0.88), 90° (ICC=0.89), and 135° (ICC=0.82), arm abduction had internal reliability between tests.
The exercise group performed a corrective exercise program based on scapula stability for eight weeks to strengthen and stretch the scapula stabilizing muscles. In the first session, all subjects received about one hour of training on how to do the exercises, and also each subject was given written instructions and a picture of how to do the exercises for guidance at home. The training program included five days a week, daily stretching exercises, and three days of strength training. Each training session consisted of a maximum of 60 minutes (10 minutes of warm-up, 10 minutes of stretching and range of movement after warm-up or cooling, and a maximum of 30 minutes of strength and postural exercises based on scapula stability and 10 minutes of cooling). In each training session, the examiner and a bodybuilding instructor were present to guide the subjects. This exercise program has been prepared using Gym exercises for people with spinal cord injury provided by Harborview Medical Center and following The American College of Sports Medicine (ACSM). guidelines for these people [24, 25]. The independent t-test, Aanalysis of Variance (ANOVA), and Analysis of Covariance (ANCOVA) were used to analyze the data. The significance level was determined at P≤0.05 in all tests.
Results
Table 1 presents the demographic information of the subjects.
.jpg)
Tables 2 and 4 show the scapular upward rotation and the scapulohumeral rhythm before and after the exercise program in the control and exercise groups.
.jpg)
.jpg)
ANCOVA showed a significant difference between the control and exercise groups in the scapular upward rotation in resting positions and 45°, 90°, and 135° shoulder abduction angles after exercise in preferred and non-preferred hands. The results showed a significant improvement in scapulohumeral rhythm ratio after non-preferred hand training at 90° and 135° shoulder abduction angles. The results showed no significant asymmetry between the preferred and non-preferred shoulder in the scapular upward rotation (Figure 1) at different shoulder angles, but there was a significant difference in the scapulohumeral rhythm ratio at the 45° angle of shoulder abduction in the preferred and non-preferred shoulder (Table 3).
.jpg)
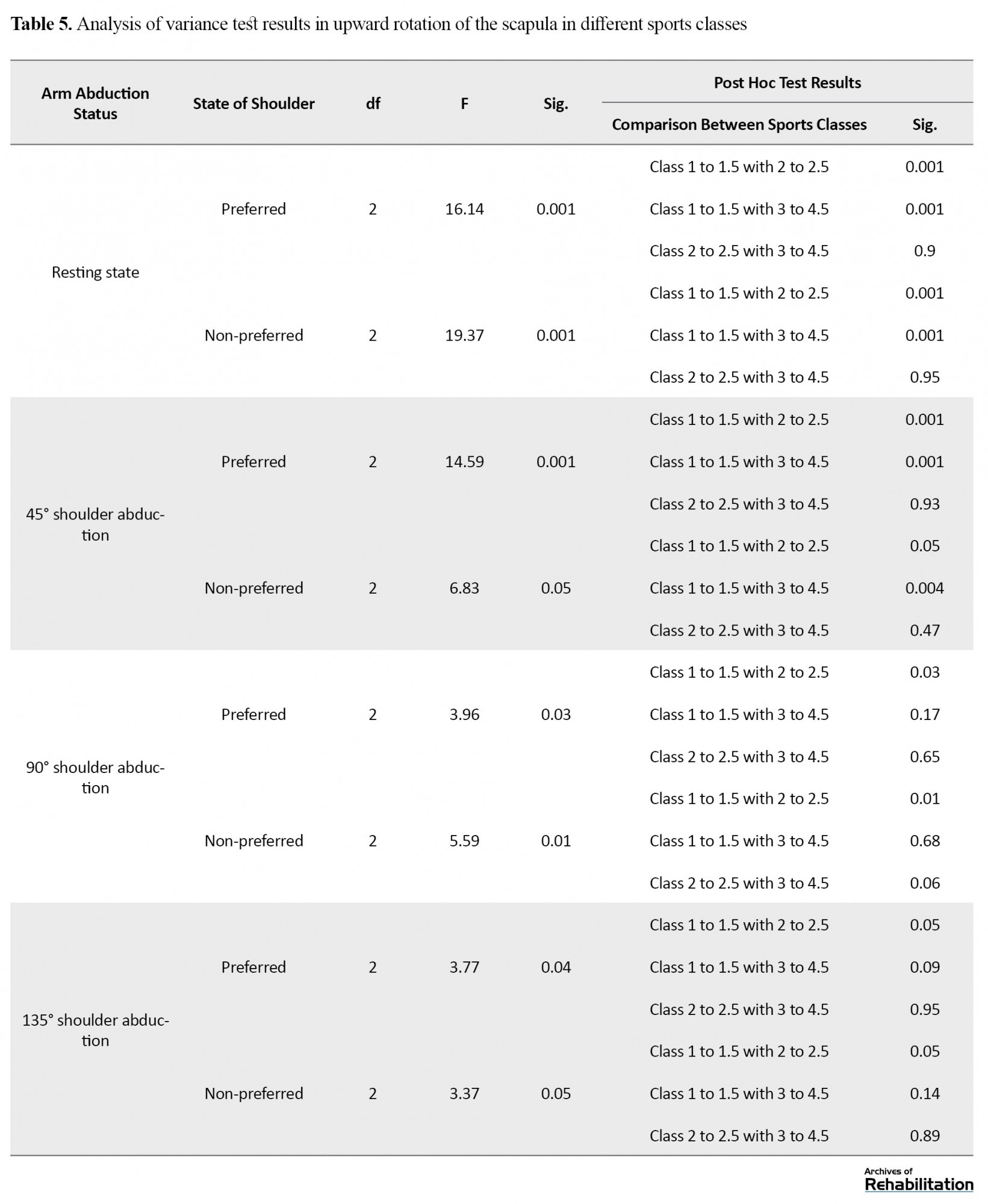
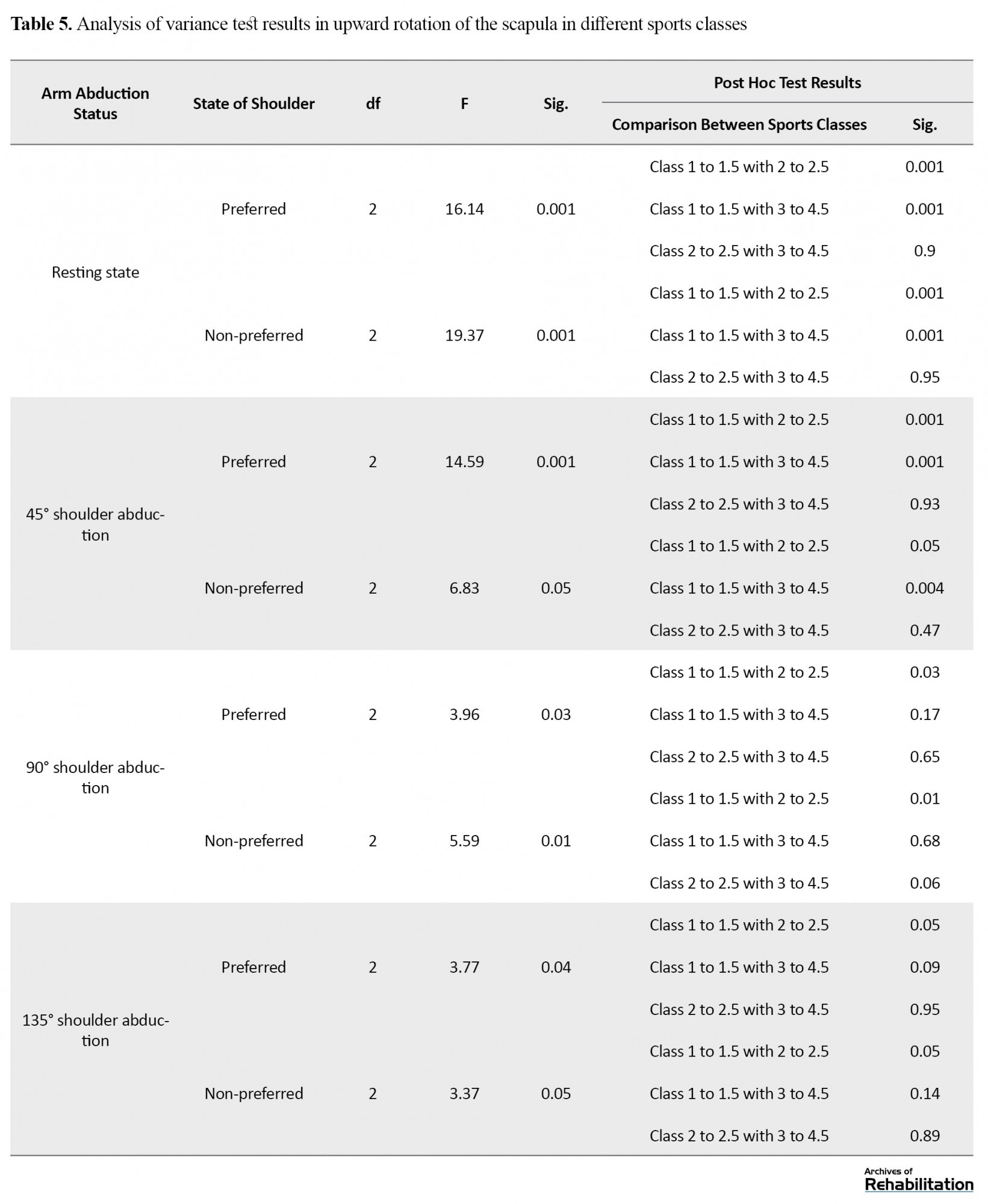
Based on the variance test results analysis, there was a significant difference in the scapular upward rotation and scapulohumeral rhythm in different sports classes at resting position, 45°, 90°, and 135° shoulder abduction (Table 5).
Discussion and Conclusion
This study aimed to investigate the indexes of scapular upward rotation and scapulohumeral rhythm in wheelchair basketball players and measure the effectiveness of an exercise program based on scapula stability on these indexes.
The results showed no significant asymmetry in the scapular upward rotation in different degrees of shoulder abduction between the preferred and non-preferred shoulders in these athletes. At a 45-degree shoulder abduction angle, the scapulohumeral rhythm ratio in the preferred shoulder was lower than that in the non-preferred shoulder. The scapula in the preferred shoulder of athletes with lower sports classes (2 to 2.5 and 3 to 4.5) had a less low rotation at resting position and more upward rotation at 45°, 90°, and 135° shoulder abduction angles.
The ratio of scapulohumeral rhythm in athletes with different sports classes was not significantly different. The scapula’s further upward rotation was observed as the arm elevation increased in the frontal plane, which corresponds to the scapula’s role in overhead activities to optimize performance. At resting position, the lower rotation was observed some more. But at different degrees of shoulder abduction, less upward rotation was observed in the scapula. Almost like the scapulohumeral rhythm, the share of the scapular upward rotation in the entire shoulder elevation arch is different, consistent with previous reports [26, 27]. Some kinematic studies have shown differences in the scapula position and movements on both sides [28, 29, 30, 31, 32, 33], while others suggest symmetry in the scapula kinematics in the preferred and non-preferred shoulder [27, 34].
Barry et al. reported internal rotation, upward rotation, and anterior scapular tilt during wheelchair driving [35]. Martin et al. showed wheelchair tennis players had a more posterior tilt in the scapula during arm elevation and lowering it to the preferred than non-preferred position [36]. The scapula in these individuals had more upward rotation to the preferred side during the arm’s elevation on the scapula plate than those with shoulder involvement [36, 37, 38, 39]. It can be concluded that asymmetry, especially an anterior tilt pattern or the internal scapula rotation, is associated with shoulder pathology or its susceptibility. It seems that one of the reasons for the anterior glenohumeral instability in athletes is throwing, which can make them prone to shear stress and damage to the capsule anterior structure and labrum.
The results showed no significant difference between the preferred and non-preferred shoulders of wheelchair basketball players in the scapula resting position. However, the scapula had lower rotation in the preferred shoulder than the non-preferred shoulder. These results are probably due to adaptations to the particular position used in the musculoskeletal system, such as muscle length imbalances in the scapulothoracic muscles due to repeated but different frequency and movement patterns in the preferred and non-preferred shoulder [6, 29, 40]. It was also observed the mean amount of the scapular upward rotation at resting position, 45°, 90°, and 135° angles of arm abduction in the preferred shoulder of wheelchair basketball athletes with different sports classes was significantly different, which may be due to muscle imbalance.
People with lower exercise classes have better muscle control over the trunk, and the trunk-scapular muscles provide more scapular stability during arm elevation. This study showed that a corrective exercise program based on scapula stability improved scapular upward rotation in wheelchair basketball players. After the training program, the scapular downward rotation decreased in dominant and non-dominant shoulder in the resting position (effect size respectively, 0.33, 0.52) and scapular upward rotation had a significant increase in 45º and 135º of shoulder abduction in dominant side (effect size respectively, 0.3, 0.22) and had a significant increase in 45º, 90º and 135º of shoulder abduction in non-dominant side (effect size respectively, 0.52, 0.25, 0.47). Although no significant improvement was observed in the scapulohumeral rhythm ratio in the preferred shoulder, it improved in the non-preferred shoulder at 90° and 135° angles of arm abduction (effect size, 0.27, 0.28, respectively).
The scapula muscle strengthening was associated with a significant increase in its upward rotation angle and a significant decrease in scapulohumeral rhythm. According to this study results, the scapula direction, as described by Kendall et al. [41], deviated somewhat from the normal state. Therefore, a corrective exercise program based on scapula stability can maintain and restore the scapula’s normal position and possibly repair and improve the standard muscle length in the upper rotator scapula muscles.
Overall, this study showed that wheelchair basketball players have some asymmetry in the upward scapular rotation and the ratio of the scapulohumeral rhythm between the preferred and non-preferred shoulder. It is due to specific adaptations to imposed demands [42] and muscle imbalances caused by spinal cord injury. This study showed that the selected exercise program could be effective in correcting the scapula direction and movements during arm elevation in wheelchair basketball players. This finding is consistent with the Shaman and Caldwell results, which examined the impact of scapula exercise programs [43, 44].
The study’s limitations were the small sample size and its non-blindness according to the research conditions. It is suggested that similar studies on scapula disorders be performed in other groups of athletes with wheelchairs, especially spinal cord injuries (such as tennis, archery, etc.) and women.
The study results supported the effectiveness of the scapula stability-based correction exercising program in improving scapula movements in wheelchair basketball players. The scapula has an essential role in shoulder movements, whose postural and movement disorders can cause secondary problems such as shoulder pain, shoulder entrapment syndrome, and limited motion range. So, physicians and trainers devote part of their training program to scapula stabilizers. Despite our results, more research and follow-up are needed to prepare an effective exercise therapy program for wheelchair athletes and identify its long-term effects in preventing injury and determining its benefits in wheelchair athletes, especially wheelchair basketball players.
Ethical Considerations
Compliance with ethical guidelines
Necessary coordination was arranged with the head of the welfare department of Mashhad City and Imam Khomeini and Shahid Fayyaz Bakhsh rehabilitation centers. The proposal was approved by the Research Commission of the University of Guilan. The participants were informed of the purpose of the research and its implementation stages. A written consent has been obtained from the subjects. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. The Helsinki Convention was also observed.
Funding
This article was extracted from the PhD. dissertation of the first authorat Department of Sports Injuries & Corrective Exercise, School of Physical Education and Sport Sciences, University of Guilan, Rasht.
Authors' contributions
Conceptualization, methodology, data collection, and data analysis: Abdollah Maarouf, Hassan Daneshmandi, Ali Asghar Norasteh; Writing – original draf: Hassan Daneshmandi, Ali Asghar Norasteh and Ahmad Ebrahimi Atri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We appreciate the wheelchair basketball players with disabilities of Imam Khomeini and Shahid Fayyazbakhsh Rehabilitation Centers in Mashhad City, who participated in this study.
References
thletes who mainly use their upper limbs in sports usually complain of shoulder disorders and pain [1, 2]. Inman et al. were the first to measure scapulohumeral rhythm by radiography and suggested a 2:1 ratio for glenohumeral elevation and scapulothoracic upward rotation [3]. Some of the literature suggests the 2:1 ratio is not consistent across an entire arc of shoulder elevation and that variability in this ratio may increase when considering the scapulohumeral rhythm exhibited by shoulder injured subjects [5, 4]. Some previous studies have suggested that scapula muscle dysfunction can lead to abnormal alignment and upper limb dysfunction [6, 7]. One of the scapula’s abnormal problems is its low rotation syndrome, which causes the scapula to fall, drain, and tilt [8, 9]. Previous research in people who use wheelchairs examined their scapulae condition in activities such as translocation and weight loss [10, 11, 12]. According to these studies, changes in the scapula directions and movements and arm during these activities reduce the space under the acromion, which increases the risk of injury [10, 11, 12]. Transmissions in people who use wheelchairs are performed with compensatory changes in the scapula kinematics, maintaining space under the acromion during activity [11].
The previous scapula kinematics results of wheelchair drivers are mainly concluded from studies that have examined the scapula movements unilaterally (right or left) [13, 14, 15]. But wheelchair driving is a bilateral activity that requires coordination of both upper limbs, and therefore its symmetry cannot be ignored [16]. Although previous data show scapula asymmetry when driving in a wheelchair [16, 17, 18, 19, 20], we still need to research scapula movements bilaterally (right and left). Wheelchair players are at risk of overworked shoulder injuries due to the frequent use of their upper limbs to drive wheelchairs. Repeated wheelchair mechanisms cause repetitive scapular protrusions that can lead to postural changes, stabilizing muscle weakness, and anterior muscle stiffness. Compensatory muscle imbalances may be due to prolonged wheelchair use or defects in the rotator cuff and scapula stabilizers’ strength training programs. This condition can lead to musculoskeletal injuries in athletes who require different movement patterns (such as swimming, throwing, or racket sports) [21, 22]. However, it is unknown whether activation has a protective effect on the musculoskeletal system [23]. Previous studies in this field have investigated the scapulohumeral rhythm in injured people and healthy athletes. However, no studies have been performed on wheelchair basketball players, and the effect of exercise interventions on the scapula in these people has not been studied. Thus, we aimed to investigate the indexes of scapular upward rotation and scapulohumeral rhythm in wheelchair basketball players and see the exercise program’s results based on scapula stability on these indexes.
Materials and Methods
The research method is quasi-experimental. According to the research conditions, 24 wheelchair basketball players with spinal cord injuries participated in this study. First, 8 players from each sports class (sports class 1 to 1.5, sports class 2 to 2.5, and sports class 3 to 4.5) were selected. Then, four people from each sports class were randomly assigned to the control or experimental group (12 control and 12 experimental). Thus, an equal number of three sports classes were present in each group. Wheelchair basketball players were professional players in the Mashhad City League, Iran. The participants were classified according to the IWBF classification and the relevant sports classification from the Veterans and Disabled Sports Federation of the Islamic Republic of Iran (IRISFD), both of which are required for people with physical disabilities to participate in competitions. Individuals with a history of shoulder surgery, injury, and pain were excluded from the study 6 months before the test. Two digital inclinometers were used to measure the motion of the arm and scapula range at rest position and 45°, 90°, and 135° shoulder abduction angles at the scapula scaption surface. The study’s final results to measure the scapular upward rotation in resting positions (ICC=0.89) and angles 45° (ICC=0.88), 90° (ICC=0.89), and 135° (ICC=0.82), arm abduction had internal reliability between tests.
The exercise group performed a corrective exercise program based on scapula stability for eight weeks to strengthen and stretch the scapula stabilizing muscles. In the first session, all subjects received about one hour of training on how to do the exercises, and also each subject was given written instructions and a picture of how to do the exercises for guidance at home. The training program included five days a week, daily stretching exercises, and three days of strength training. Each training session consisted of a maximum of 60 minutes (10 minutes of warm-up, 10 minutes of stretching and range of movement after warm-up or cooling, and a maximum of 30 minutes of strength and postural exercises based on scapula stability and 10 minutes of cooling). In each training session, the examiner and a bodybuilding instructor were present to guide the subjects. This exercise program has been prepared using Gym exercises for people with spinal cord injury provided by Harborview Medical Center and following The American College of Sports Medicine (ACSM). guidelines for these people [24, 25]. The independent t-test, Aanalysis of Variance (ANOVA), and Analysis of Covariance (ANCOVA) were used to analyze the data. The significance level was determined at P≤0.05 in all tests.
Results
Table 1 presents the demographic information of the subjects.
.jpg)
Tables 2 and 4 show the scapular upward rotation and the scapulohumeral rhythm before and after the exercise program in the control and exercise groups.
.jpg)
.jpg)
ANCOVA showed a significant difference between the control and exercise groups in the scapular upward rotation in resting positions and 45°, 90°, and 135° shoulder abduction angles after exercise in preferred and non-preferred hands. The results showed a significant improvement in scapulohumeral rhythm ratio after non-preferred hand training at 90° and 135° shoulder abduction angles. The results showed no significant asymmetry between the preferred and non-preferred shoulder in the scapular upward rotation (Figure 1) at different shoulder angles, but there was a significant difference in the scapulohumeral rhythm ratio at the 45° angle of shoulder abduction in the preferred and non-preferred shoulder (Table 3).
.jpg)
Based on the variance test results analysis, there was a significant difference in the scapular upward rotation and scapulohumeral rhythm in different sports classes at resting position, 45°, 90°, and 135° shoulder abduction (Table 5).
Discussion and Conclusion
This study aimed to investigate the indexes of scapular upward rotation and scapulohumeral rhythm in wheelchair basketball players and measure the effectiveness of an exercise program based on scapula stability on these indexes.
The results showed no significant asymmetry in the scapular upward rotation in different degrees of shoulder abduction between the preferred and non-preferred shoulders in these athletes. At a 45-degree shoulder abduction angle, the scapulohumeral rhythm ratio in the preferred shoulder was lower than that in the non-preferred shoulder. The scapula in the preferred shoulder of athletes with lower sports classes (2 to 2.5 and 3 to 4.5) had a less low rotation at resting position and more upward rotation at 45°, 90°, and 135° shoulder abduction angles.
The ratio of scapulohumeral rhythm in athletes with different sports classes was not significantly different. The scapula’s further upward rotation was observed as the arm elevation increased in the frontal plane, which corresponds to the scapula’s role in overhead activities to optimize performance. At resting position, the lower rotation was observed some more. But at different degrees of shoulder abduction, less upward rotation was observed in the scapula. Almost like the scapulohumeral rhythm, the share of the scapular upward rotation in the entire shoulder elevation arch is different, consistent with previous reports [26, 27]. Some kinematic studies have shown differences in the scapula position and movements on both sides [28, 29, 30, 31, 32, 33], while others suggest symmetry in the scapula kinematics in the preferred and non-preferred shoulder [27, 34].
Barry et al. reported internal rotation, upward rotation, and anterior scapular tilt during wheelchair driving [35]. Martin et al. showed wheelchair tennis players had a more posterior tilt in the scapula during arm elevation and lowering it to the preferred than non-preferred position [36]. The scapula in these individuals had more upward rotation to the preferred side during the arm’s elevation on the scapula plate than those with shoulder involvement [36, 37, 38, 39]. It can be concluded that asymmetry, especially an anterior tilt pattern or the internal scapula rotation, is associated with shoulder pathology or its susceptibility. It seems that one of the reasons for the anterior glenohumeral instability in athletes is throwing, which can make them prone to shear stress and damage to the capsule anterior structure and labrum.
The results showed no significant difference between the preferred and non-preferred shoulders of wheelchair basketball players in the scapula resting position. However, the scapula had lower rotation in the preferred shoulder than the non-preferred shoulder. These results are probably due to adaptations to the particular position used in the musculoskeletal system, such as muscle length imbalances in the scapulothoracic muscles due to repeated but different frequency and movement patterns in the preferred and non-preferred shoulder [6, 29, 40]. It was also observed the mean amount of the scapular upward rotation at resting position, 45°, 90°, and 135° angles of arm abduction in the preferred shoulder of wheelchair basketball athletes with different sports classes was significantly different, which may be due to muscle imbalance.
People with lower exercise classes have better muscle control over the trunk, and the trunk-scapular muscles provide more scapular stability during arm elevation. This study showed that a corrective exercise program based on scapula stability improved scapular upward rotation in wheelchair basketball players. After the training program, the scapular downward rotation decreased in dominant and non-dominant shoulder in the resting position (effect size respectively, 0.33, 0.52) and scapular upward rotation had a significant increase in 45º and 135º of shoulder abduction in dominant side (effect size respectively, 0.3, 0.22) and had a significant increase in 45º, 90º and 135º of shoulder abduction in non-dominant side (effect size respectively, 0.52, 0.25, 0.47). Although no significant improvement was observed in the scapulohumeral rhythm ratio in the preferred shoulder, it improved in the non-preferred shoulder at 90° and 135° angles of arm abduction (effect size, 0.27, 0.28, respectively).
The scapula muscle strengthening was associated with a significant increase in its upward rotation angle and a significant decrease in scapulohumeral rhythm. According to this study results, the scapula direction, as described by Kendall et al. [41], deviated somewhat from the normal state. Therefore, a corrective exercise program based on scapula stability can maintain and restore the scapula’s normal position and possibly repair and improve the standard muscle length in the upper rotator scapula muscles.
Overall, this study showed that wheelchair basketball players have some asymmetry in the upward scapular rotation and the ratio of the scapulohumeral rhythm between the preferred and non-preferred shoulder. It is due to specific adaptations to imposed demands [42] and muscle imbalances caused by spinal cord injury. This study showed that the selected exercise program could be effective in correcting the scapula direction and movements during arm elevation in wheelchair basketball players. This finding is consistent with the Shaman and Caldwell results, which examined the impact of scapula exercise programs [43, 44].
The study’s limitations were the small sample size and its non-blindness according to the research conditions. It is suggested that similar studies on scapula disorders be performed in other groups of athletes with wheelchairs, especially spinal cord injuries (such as tennis, archery, etc.) and women.
The study results supported the effectiveness of the scapula stability-based correction exercising program in improving scapula movements in wheelchair basketball players. The scapula has an essential role in shoulder movements, whose postural and movement disorders can cause secondary problems such as shoulder pain, shoulder entrapment syndrome, and limited motion range. So, physicians and trainers devote part of their training program to scapula stabilizers. Despite our results, more research and follow-up are needed to prepare an effective exercise therapy program for wheelchair athletes and identify its long-term effects in preventing injury and determining its benefits in wheelchair athletes, especially wheelchair basketball players.
Ethical Considerations
Compliance with ethical guidelines
Necessary coordination was arranged with the head of the welfare department of Mashhad City and Imam Khomeini and Shahid Fayyaz Bakhsh rehabilitation centers. The proposal was approved by the Research Commission of the University of Guilan. The participants were informed of the purpose of the research and its implementation stages. A written consent has been obtained from the subjects. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. The Helsinki Convention was also observed.
Funding
This article was extracted from the PhD. dissertation of the first authorat Department of Sports Injuries & Corrective Exercise, School of Physical Education and Sport Sciences, University of Guilan, Rasht.
Authors' contributions
Conceptualization, methodology, data collection, and data analysis: Abdollah Maarouf, Hassan Daneshmandi, Ali Asghar Norasteh; Writing – original draf: Hassan Daneshmandi, Ali Asghar Norasteh and Ahmad Ebrahimi Atri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We appreciate the wheelchair basketball players with disabilities of Imam Khomeini and Shahid Fayyazbakhsh Rehabilitation Centers in Mashhad City, who participated in this study.
References
- Jobe F, Pink M. Shoulder pain in golf. Clinics in Sport Medicine.1996; 15(1):55-63. [DOI:10.1016/S0278-5919(20)30158-7]
- Ranson C, Gregory P. Shoulder injury in professional cricketers. Physical Therapy in Sport. 2008; 9(1):34-39. [DOI:10.1016/j.ptsp.2007.08.001] [PMID]
- Fayad F, Hoffmann G, Hanneton S, Yazbeck C, Lefevre-Colau MM, Poiraudeau S, et al. 3-D scapular kinematics during arm elevation: Effect of motion velocity. Clinical Biomechanics. 2006; 21(9):932-41. [DOI:10.1016/j.clinbiomech.2006.04.015] [PMID]
- Sobush DC, Simoneau GG, Dietz KE, Levene JA, Grossman RE, Smith WB. The lennie test for measuring scapular position in healthy young adult females: A reliability and validity study. Journal of Orthopaedic & Sports Physical Therapy. 1996; 23(1):39-50. [DOI:10.2519/jospt.1996.23.1.39] [PMID]
- Magee DJ. Orthopedic physical assessment. Philadelphia: W. B. Saunders Company; 1997.
- Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St. Louis: Mosby; 2002.
- Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. Muscles: Testing and function with posture and pain. Baltimore: Williams & Wilkins; 2005.
- Inman VT, Saunders JB, Abbott LC. Observations of the function of the shoulder joint. 1944. Clinical Orthopaedics and Related Research. 1996; (330):3-12. [DOI:10.1097/00003086-199609000-00002] [PMID]
- Crosbie J, Kilbreath SL, Hollmann L, York S. Scapulohumeral rhythm and associated spinal motion. Clinical Biomechanics (Bristol, Avon). 2008; 23(2):184-92. [DOI:10.1016/j.clinbiomech.2007.09.012] [PMID]
- Scibek JS, Mell AG, Downie BK, Carpenter JE, Hughes RE. Shoulder kinematics in patients with full-thickness rotator cuff tears after a subacromial injection. Journal of Shoulder and Elbow Surgery. 2008; 17(1):172-81. [DOI:10.1016/j.jse.2007.05.010] [PMID]
- Borstad JD. Resting position variables at the shoulder: Evidence to support a posture impairment association. Physical Therapy. 2006; 86(4):549-57. [DOI:10.1093/ptj/86.4.549] [PMID]
- Page P, Frank C, Lardner R. Assessment and treatment of muscle imbalance: The Janda approach. Journal of Orthopedic & Sports Physical Therapy. 2011; 41(10):799-800. http://www.jandacrossedsyndromes.com/wp-content/uploads/2011/10/JOSPT2011JandaReview.pdf
- Ha SM, Kwon OY, Yi CH, Jeon HS, Lee WH. Effects of passive correction of scapular position on pain, proprioception, and range of motion in neck-pain patients with bilateral scapular downward-rotation syndrome. Manual Therapy. 2011; 16(6):585-9. [DOI:10.1016/j.math.2011.05.011] [PMID]
- Lee JH, Cynn HS, Choi WJ, Jeong HJ, Yoon TL. Various shrug exercises can change scapular kinematics and scapular rotator muscle activities in subjects with scapular downward rotation syndrome. Human Movement Science. 2016; (45)119-29. [DOI:10.1016/j.humov.2015.11.016] [PMID]
- Caldwell C, Sahrmann S, Van Dillen L. Use of a movement system impairment diagnosis for physical therapy in the management of a patient with shoulder pain.Journal of Orthopaedic & Sports Physical Therapy. 2007; 37(9):551-63. [DOI:10.2519/jospt.2007.2283] [PMID]
- Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. Journal of Orthopaedic & Sports Physical Therapy. 1999; 29(10):574-83. [DOI:10.2519/jospt.1999.29.10.574] [PMID]
- Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Physical Therapy. 2000; 80(3):276-91. [DOI:10.1093/ptj/80.3.276] [PMID]
- Hebert LJ, Moffet H, McFadyen BJ, Dionne CE. Scapular behaviour in shoulder impingement syndrome. Archives of Physical Medicine and Rehabilitation. 2002; 83(1):60-9. [DOI:10.1053/apmr.2002.27471] [PMID]
- Warner JJP, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moiré topographic analysis. Clinical Orthopaedics and Related Research. 1992; 285:191-9. [DOI:10.1097/00003086-199212000-00024]
- Morrow MMB, Kaufman KR, An KN. Scapular kinematics and associated impingement risk in manual wheelchair users during propulsion and during a weight relief lift. Clinical Biomechanics. 2011; 26(4):352-7. [DOI:10.1016/j.clinbiomech.2010.12.001] [PMID] [PMCID]
- Zhao KD, van Straaten MG, Cloud BA, Morrow MM, An KN, Ludewig PM. Scapulothoracic and glenohumeral kinematics during daily tasks in users of manual wheelchairs. Frontiers in Bioengineering and Biotechnology. 2015; 3:1-10. [DOI:10.3389/fbioe.2015.00183] [PMID] [PMCID]
- Raina S, McNitt-Gray JL, Mulroy S, Requejo PS. Effect of increased load on scapular kinematics during manual wheelchair propulsion in individuals with paraplegia and tetraplegia. Human Movement Science. 2012; 31(2):397-407. [DOI:10.1016/j.humov.2011.05.006] [PMID]
- Nawoczenski DA, Clobes SM, Gore SL, Neu JL, Olsen JE, Borstad JD, et al. Three-dimensional shoulder kinematics during a pressure relief technique and wheelchair transfer. Archives of Physical Medicine and Rehabilitation. 2003; 84(9):1293-300. [DOI:10.1016/S0003-9993(03)00260-0]
- Finley MA, Mcquade KJ, Rodgers MM. Scapular kinematics during transfers in manual wheelchair users with and without shoulder impingement. Clinical Biomechanics. 2005; 20(1):32-40. [DOI:10.1016/j.clinbiomech.2004.06.011] [PMID]
- Riek LM, Ludewig PM, Nawoczenski DA. Comparative shoulder kinematics during free standing, standing depression lifts and daily functional activities in persons with paraplegia: Considerations for shoulder health. Spinal Cord. 2008; 46(5):335-43. DOI:10.1038/sj.sc.3102140] [PMID]
- Hurd WJ, Morrow MM, Kaufman KR, An KN. Biomechanic evaluation of upper extremity symmetry during manual wheelchair propulsion over varied terrain. Archives of Physical Medicine and Rehabilitation. 2008; 89(10):1996-2002. [DOI:10.1016/j.apmr.2008.03.020] [PMID] [PMCID]
- Fay BT, Boninger ML, Fitzgerald SG, Souza AL, Cooper RA, Koontz AM. Manual wheelchair pushrim dynamics in people with multiple sclerosis. Archives of Physical Medicine and Rehabilitation. 2004; 85(6):935-42. [DOI:10.1016/j.apmr.2003.08.093] [PMID]
- Vegter RJ, Lamoth CJ, De Groot S, Veeger DH, Van der Woude LH. Variability in bimanual wheelchair propulsion: Consistency of two instrumented wheels during handrim wheelchair propulsion on a motor driven treadmill. Journal of NeuroEngineering and Rehabilitation. 2013; 10(1):1-11. [DOI:10.1186/1743-0003-10-9] [PMID] [PMCID]
- Stephens CL, Engsberg JR. Comparison of overground and treadmill propulsion patterns of manual wheelchair users with tetraplegia. Disability and Rehabilitation: Assistive Technology. 2010; 5(6):420-7. [DOI:10.3109/17483101003793420] [PMID]
- Schnorenberg AJ, Slavens BA, Wang M, Vogel LC, Smith PA, Harris GF. Biomechanic model for evaluation of paediatric upper extremity joint dynamicsduring wheelchair mobility. Journal of Biomechanics. 2014; 47(1):269-76. [DOI:10.1016/j.jbiomech.2013.11.014] [PMID] [PMCID]
- Soltau SL, Slowik JS, Requejo PS, Mulroy SJ, Neptune RR. An investigation of bilateral symmetry during manual wheelchair propulsion. Frontiers in Bioengineering and Biotechnology. 2015; 3:1-6. [DOI:10.3389/fbioe.2015.00086] [PMID] [PMCID]
- Dec KL, Sparrow KJ, McKeag DB. The physically challenged athlete: medical issues and assessment. Sports Medicine. 2000; 29(4):245-58. [DOI:10.2165/00007256-200029040-00003] [PMID]
- Aydan A, Aslican Z, Nihan O P, Ayca A T, Nevin E. Scapular resting position, shoulder pain and function in disabled athletes. Prosthetics and Orthotics International. 2015; 39(5):390-6. https://journals.sagepub.com/doi/full/10.1177/0309364614534295
- Wylie EJ, Chakera TM. Degenrative joint abnormalities in patients with paraplegia of duration greater than 20 years. Paraplegia. 1988; 26(2):101-6. [DOI:10.1038/sc.1988.20] [PMID]
- McDonell MK, Sahrmann SA, Van Dillen L. A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: A case report. Journal of Orthopaedic & Sports Physical Therapy. 2005; 30(1):3-15. [DOI:10.2519/jospt.2005.35.1.3] [PMID]
- Andrade GT, Azevedo DC, De Assis Lorentz I, Galo Neto RS, Sadala Do Pinho V, Ferraz Gonçalves RT, et al. Influence of scapular position on cervical rotation range of motion.Journal of Orthopaedic & Sports Physical Therapy. 2008; 38(11):668-73. [DOI:10.2519/jospt.2008.2820] [PMID]
- Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. Journal of Orthopaedic & Sports Physical Therapy. 2001; 31(2):81-9. [DOI:10.2519/jospt.2001.31.2.81] [PMID]
- Struyf F, Nijs J, De Graeve J, Mottram S, Meeusen R. Scapular positioning in overhead athletes with and without shoulder pain: A case-control study. Scandinavian Journal of Medicine & Science in Sports. 2011; 21(6):809-18. [DOI:10.1111/j.1600-0838.2010.01115.x] [PMID]
- Kaupang K. Get Moving: Exercise and SCI [Internet]. 2013 [Updated 2013 February 12]. Available from: https://sci.washington.edu/info/forums/reports/exercise_2013.asp
- Linda S. ACSM’s guidelines for exercise testing and prescription. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2014. https://books.google.com/books?id=TtiCAwAAQBAJ&printsec
- Witwer A, Sauers EL. Clinical measures of shoulder mobil- ity in college water-polo players. Journal of Sport Rehabilitation. 2006;15(1):45-57. [DOI:10.1123/jsr.15.1.45]
- Yoshizaki K, Hamada J, Tamai K, Sahara R, Fujiwara T, Fujimoto T. Analysis of the scapulohumeral rhythm and electromyography of the shoulder muscles during elevation and lowering: Comparison of dominant and nondominant shoulders. ournal of Shoulder and Elbow Surgery. 2009; 18(5):756-63. [DOI:10.1016/j.jse.2009.02.021] [PMID]
- Matsuki K, Matsuki KO, Mu S, Yamaguchi S, Ochiai N, Sasho T, et al. In vivo 3- dimensional analysis of scapular kinematics: comparison of dominant and nondominant shoulders. Journal of Shoulder and Elbow Surgery. 2011; 20(4):659-65. [DOI:10.1016/j.jse.2010.09.012] [PMID]
- Morais NV, Pascoal AG. Scapular positioning assessment: Is side-to-side comparison clinically acceptable? Manual Therapy. 2013; 18(1):46-53. [DOI:10.1016/j.math.2012.07.001] [PMID]
- Hosseinimehr SH, Anbarian M, Norasteh AA, Fardmal J, Khosravi MT, The Comparison of scapular upward rotation and scapulohumeral rhythm between dominant and nondominant shoulder in male overhead athletes and non-athletes. Manual Therapy. 2015; 20(6):758-62. [DOI:10.1016/j.math.2015.02.010]
- Nodehi Moghadam A, Ashrafi Z. [Comparison of scapular position in two dominant and non-dominant organs in healthy girls (Persain)]. Journal of Rehabilitation. 2007; 8(3):39-44. http://rehabilitationj.uswr.ac.ir/article-1-180-en.html
- Azarsa MH, Shadmehr A, Jalaei SH. [The relationship between body mass index and exercise history in Scapular kinematics in healthy basketball men (Persain)]. Physical Treatments Journal. 2014; 3(4)9-15.
- Yano Y, Hamada J, Tamai K, Yoshizaki K, Sahara R, Fujiwara T, et al. Different scapular kinematics in healthy subjects during arm elevation and lowering: glenohumeral and scapulothoracic patterns. Journal of Shoulder and Elbow Surgery. 2010; 19(2):209-15. [DOI:10.1016/j.jse.2009.09.007] [PMID]
- Lee SK, Yang DS, Kim HY, Choy WS. A comparison of 3D scapular kinematics between dominant and nondominant shoulders during multiplanar arm motion. Indian Journal of Orthopaedics. 2013; 47(2):135-42. [DOI:10.4103/0019-5413.108882] [PMID] [PMCID]
- Barry S. Mason BS, Vegter RJK, Paulson TAW, Morrissey D, van der Scheer JW, et al. Bilateral scapular kinematics, asymmetries and shoulder pain in wheelchair athletes. Gait & Posture. 2018; 65:151-6. [DOI:10.1016/j.gaitpost.2018.07.170] [PMID]
- Martin BW, Wilson D, Markus OH, Dan W, Peter W, Sarah M, et al. Scapular kinematics in professional wheelchair tennis players. Clinical Biomechanics. 2018; 53:7-13. [DOI:10.1016/j.clinbiomech.2018.01.022] [PMID]
- Nodehi Moghadam A, Ebrahimi E, Aivazi M, Salavati M. [Comparison of the position and direction of three-dimensional scapular positioning in patients with shoulder impingement syndrome and healthy controls (Persain)]. Journal of Rehabilitation. 2006; 7(1):14-21. https://www.sid.ir/fa/journal/ViewPaper.aspx?ID=44427
- Keshavarz R, Shakeri H, Arab AM, Ashrafi H, Talim Khani A. Scapular position and orientation during abduction, flexion and scapular plane elevation phase. Iranian Rehabilitation Journal. 2014; 12(19):22-30. http://irj.uswr.ac.ir/article-1-322-en.html
- Keshavarz R, Shakeri H, Arab AM, Gholamian M, Tabatabaei Ghomsheh F, Raeisosadat A. [Comparison of scapular rotational movements between patients with impingement Shoulder syndrome and healthy people in lifting the arm on the Scapular plate using acromion cluster marker (Persain)]. Archives of Rehabilitation. 2012; 12(4):67-74. https://rehabilitationj.uswr.ac.ir/article-1-1021-fa.html
- Nazarymoghadam S, Nodehimoghadam A, Arab AM, Zeinalzade A. [A comparison between females with and without general hypermobility syndrome in arm elevation (Persain)]. Journal of Rehabilitation. 2010; 11(2):82. http://ensani.ir/file/download/article/20101004171426
- Burkhat SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology. Part III: The SICK scapula, scapular dyskinesis, the chain, and rehabilitation. Arthroscoov. 2003; 19(6):641-61. [DOI:10.1016/S0749-8063(03)00389-X]
- Wang J, Sainburg R. The dominant and nondominant arms are specialized for stabilizing different features of task performance. Experimental Brain Research. 2007; 178(4):565-70. [DOI:10.1007/s00221-007-0936-x] [PMID]
- Sale D, MacDougall D. Specificity in strength training: A review for the coach and athlete. Journal Canadien Des Sciences Appliquées Au Sport. 1986; 6(2):87-92. [PMID]
- Bunch WH, Siegel IM. Scapulothoracic arthrodesis in facioscapulohumeral muscular dystrophy. Review of seventeen procedures with three to twenty-one-year follow-up. Journal of Bone and Joint Surgery. 1993; 75(3):372-6. [DOI:10.2106/00004623-199303000-00008] [PMID]
- Hrysomallis C, Goodman C. A review of resistance exercise and posture realignment. The Journal of Strength and Conditioning Research. 2001; 15(3):385-90. [DOI:10.1519/1533-4287(2001)0152.0.CO;2] [PMID]
Type of Study: Original |
Subject:
Rehabilitation
Received: 27/10/2019 | Accepted: 5/03/2020 | Published: 1/01/2021
Received: 27/10/2019 | Accepted: 5/03/2020 | Published: 1/01/2021
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







.jpg)
