Volume 21, Issue 2 (Summer 2020)
jrehab 2020, 21(2): 236-255 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadeghi Z, Afshar M, Ebadi A, Baghban K, Qureshi Z S. Swallowing Disorder in Multiple Sclerosis: Modified Version of the Screening Tool. jrehab 2020; 21 (2) :236-255
URL: http://rehabilitationj.uswr.ac.ir/article-1-2643-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-2643-en.html
1- Student Research Committee, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Behavioral Sciences Research Center, Research Institute for Life Style, School of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran.
3- Department of Speech Therapy, School of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,zahraqoreishi@yahoo.com
2- Behavioral Sciences Research Center, Research Institute for Life Style, School of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran.
3- Department of Speech Therapy, School of Rehabilitation, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Keywords: Multiple Sclerosis, Dysphagia, Dysphagia in Multiple Sclerosis Questionnaire, Construct Validity, Screening
Full-Text [PDF 6742 kb]
(1771 Downloads)
| Abstract (HTML) (4985 Views)
Full-Text: (2629 Views)
Introduction
Multiple Sclerosis (MS) is an inflammatory autoimmune disease, which is associated with a wide range of symptoms related to nervous system involvement, including impaired muscle strength, motor coordination, balance, visual impairment, and mental health issues [1-6]. Swallowing disorders are also a relatively common symptom in these patients. Based on the findings of a meta-analysis, its prevalence was estimated at 36% [7]. Swallowing disorders can lead to serious problems such as increased risk of dehydration, weight loss and aspiration pneumonia [8-11]. Therefore, its early detection is an important factor in limiting the problems that follow this disorder.
Having an effective screening tool is very useful for early detection of the risk of swallowing disorder and referral for more accurate tests and instrumental evaluations. The 10-item Dysphagia in Multiple Sclerosis (DYMUS) questionnaireis the only questionnaire specifically developed for screening for swallowing disorders in MS patients by Bergamaschi et al. [12] in 2008. This self-report questionnaire consists of 10 items that are considered in two subgroups: “swallowing disorder for solid foods” and “swallowing disorder in liquids”. Based on the findings of this study [12], it was shown that the average scores of the questionnaire in patients who claimed to have swallowing disorders were significantly higher than patients who did not complain of swallowing disorders. Also, except for 10th item of the questionnaire, the correlation coefficient of other items for both subscales was high [12, 13].
The validity and reliability of the questionnaire were evaluated in different groups of MS patients in Greek [14], Portuguese [15], French [16], and Turkish [17]. Based on the findings of factor analysis in the studies of Printza et al. [14] and Alali et al. [18], a modified 9-item version of the questionnaire has been proposed due to more favorable psychometric indices. The Persian version of this questionnaire has been prepared recently [20, 19] and confirmatory factor analysis has been used to test the two-factor structure of the questionnaire. Despite previous research, in these studies the correlation coefficient of all items is high.
Although dysphagia was diagnosed as a clinical finding in MS in 1877 [21], it has not yet received sufficient attention. The use of appropriate rehabilitation tools for early diagnosis of swallowing disorders and timely referral for accurate evaluation and treatment plan design can prevent serious problems from this disorder. Therefore, the aim of the present study was to first translate and culturally adapt and evaluate the validity and reliability of the questionnaire and then determine the frequency of swallowing disorders in patients referred to the MS Society of Tehran with the help of DYMUS Persian version and also to investigate the relationship between swallowing disorders and Expanded Disability Status Scale (EDSS) were the duration of the disease and the type of MS.
Materials and Methods
This research is a test-making and descriptive-analytical cross-sectional study. The statistical population of the study included patients referred to the Tehran MS Association and the statistical sample included 108 patients who were selected by available methods. Patients diagnosed with MS by a neurologist who did not have a history of any disease associated with swallowing disorders were included in the study. These people should not have had a recurrence of the disease in the last month. Exclusion criteria also included patients’ unwillingness to complete the questionnaire, lack of understanding of the questionnaire and recurrence of the disease within 2 weeks of re-evaluation.
An informed consent was obtained from patients. Also, the ethics committee of the University of Social Welfare and Rehabilitation Sciences has reviewed, approved and approved the research plan (Code: IR.USWR.REC.1397.083).
Translation and Cultural Adaptation of the questionnaire
The translation process was based on 5 stages of translation and cultural adaptation suggested by Beaton [22]. Two speech and language pathologists translated the questionnaire into Persian. The final version was translated into English by two bilingual translators, and after the translators agreed, the translated version was compared with the original version and sent to the author of the questionnaire, and the accuracy of the translation of the concepts was confirmed. Then the Persian version of the questionnaire was evaluated by two neurologists and two speech and language pathologists in the field of swallowing. Finally, these experts agreed on the Persian version of the questionnaire (P-DYMUS). The final version of the questionnaire was distributed among 10 patients and they expressed their views on the clarity, simplicity and comprehensibility of the questionnaire items.
Reliability and validity
Confirmatory Factor Analysis (CFA) was used to evaluate the validity of the structure. In the present study, the most common indicators of goodness of fit that have been introduced to test the validity of the model [23, 24], were used. Also, the operational ability of the questionnaire to identify swallowing disorders was assessed by self-reported method [25, 26]. Before completing the questionnaire, all patients were asked the question “Do you have difficulty swallowing?”
Convergent validity of the questionnaire was assessed by examining the relationship between P-DYMUS scores and Dysphagia Handicap Index (DHI) scores. The DHI questionnaire is used to identify swallowing disorders and its effect on quality of life [27]. This questionnaire has been translated into Persian and its Persian version has a high internal stability (Cronbach’s alpha coefficient between 0.82 to 0.94) and also the reliability of the high retest test (r=0.89) [28].
Kuder Richardson 20 (KR-20) was used to estimate the internal consistency of the Swallowing Disturbance Questionnaire as a general concept as well as for its two subgroups. The correlation matrix between items was also calculated to assess the homogeneity of the items. Reliability by open test method was performed on 19 participants with a time interval of 2 weeks [29].
Statistical analysis
In the present study, KR-20 reliability coefficient, Intra-cluster Correlation Coefficient (ICC), item correlation matrix, Mann-Whitney test and Spearman rank correlation coefficient were used. Statistical analysis was performed using SPSS V. 16 and LISREL V. 8.8. P<0.05 was considered as the level of significance.
Results
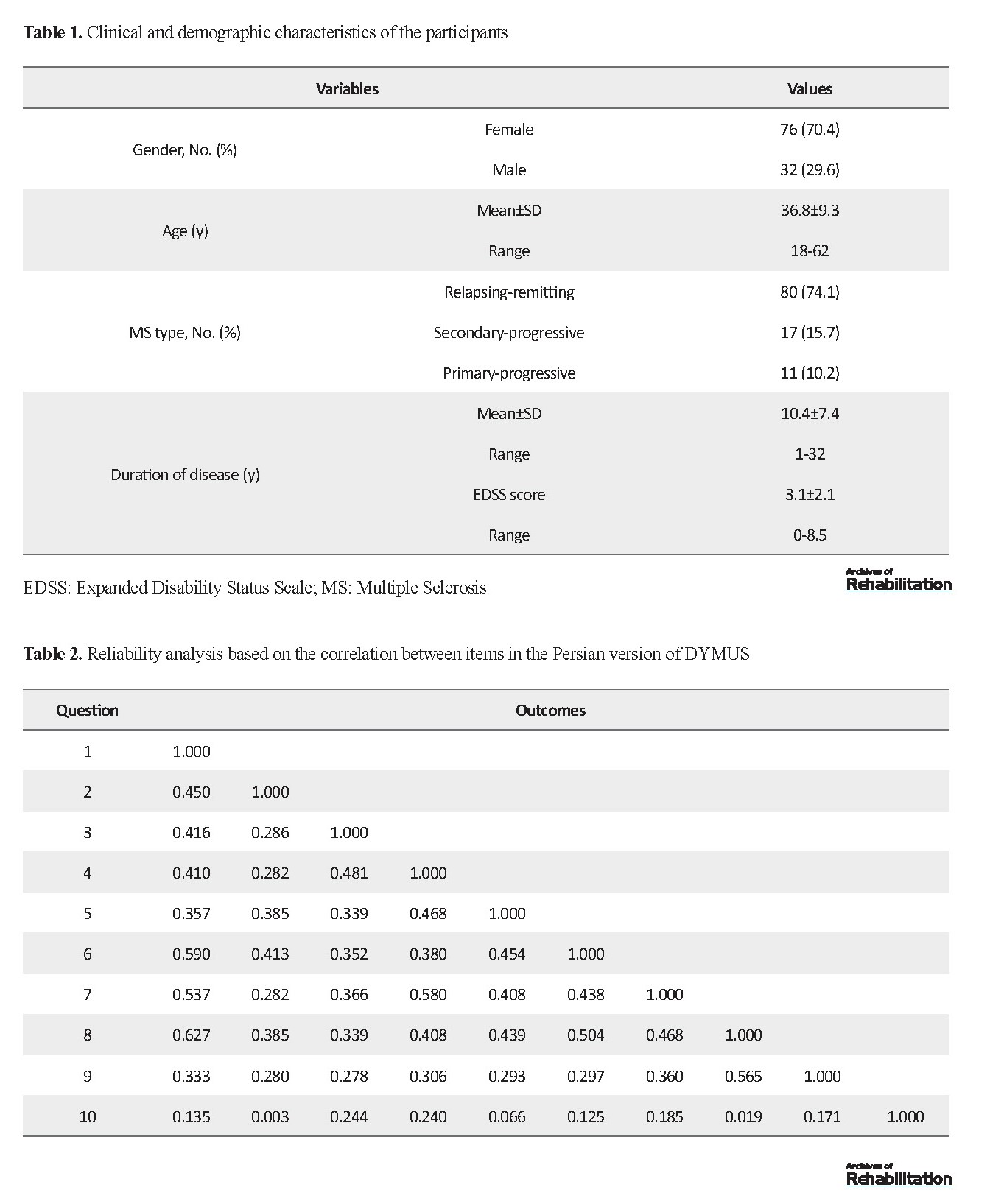
In this study, 108 patients including 76 females and 32 males participated. Of them, 80 patients were Relapsing-remitting (RR), 17 patients were Secondary Progressive (SP) and 11 patients were Primary Progressive (PP). The mean age of patients was 36.8 years, the mean duration of illness was 10.4 years and the mean EDSS score was 3.1 (Table 1).
Multiple Sclerosis (MS) is an inflammatory autoimmune disease, which is associated with a wide range of symptoms related to nervous system involvement, including impaired muscle strength, motor coordination, balance, visual impairment, and mental health issues [1-6]. Swallowing disorders are also a relatively common symptom in these patients. Based on the findings of a meta-analysis, its prevalence was estimated at 36% [7]. Swallowing disorders can lead to serious problems such as increased risk of dehydration, weight loss and aspiration pneumonia [8-11]. Therefore, its early detection is an important factor in limiting the problems that follow this disorder.
Having an effective screening tool is very useful for early detection of the risk of swallowing disorder and referral for more accurate tests and instrumental evaluations. The 10-item Dysphagia in Multiple Sclerosis (DYMUS) questionnaireis the only questionnaire specifically developed for screening for swallowing disorders in MS patients by Bergamaschi et al. [12] in 2008. This self-report questionnaire consists of 10 items that are considered in two subgroups: “swallowing disorder for solid foods” and “swallowing disorder in liquids”. Based on the findings of this study [12], it was shown that the average scores of the questionnaire in patients who claimed to have swallowing disorders were significantly higher than patients who did not complain of swallowing disorders. Also, except for 10th item of the questionnaire, the correlation coefficient of other items for both subscales was high [12, 13].
The validity and reliability of the questionnaire were evaluated in different groups of MS patients in Greek [14], Portuguese [15], French [16], and Turkish [17]. Based on the findings of factor analysis in the studies of Printza et al. [14] and Alali et al. [18], a modified 9-item version of the questionnaire has been proposed due to more favorable psychometric indices. The Persian version of this questionnaire has been prepared recently [20, 19] and confirmatory factor analysis has been used to test the two-factor structure of the questionnaire. Despite previous research, in these studies the correlation coefficient of all items is high.
Although dysphagia was diagnosed as a clinical finding in MS in 1877 [21], it has not yet received sufficient attention. The use of appropriate rehabilitation tools for early diagnosis of swallowing disorders and timely referral for accurate evaluation and treatment plan design can prevent serious problems from this disorder. Therefore, the aim of the present study was to first translate and culturally adapt and evaluate the validity and reliability of the questionnaire and then determine the frequency of swallowing disorders in patients referred to the MS Society of Tehran with the help of DYMUS Persian version and also to investigate the relationship between swallowing disorders and Expanded Disability Status Scale (EDSS) were the duration of the disease and the type of MS.
Materials and Methods
This research is a test-making and descriptive-analytical cross-sectional study. The statistical population of the study included patients referred to the Tehran MS Association and the statistical sample included 108 patients who were selected by available methods. Patients diagnosed with MS by a neurologist who did not have a history of any disease associated with swallowing disorders were included in the study. These people should not have had a recurrence of the disease in the last month. Exclusion criteria also included patients’ unwillingness to complete the questionnaire, lack of understanding of the questionnaire and recurrence of the disease within 2 weeks of re-evaluation.
An informed consent was obtained from patients. Also, the ethics committee of the University of Social Welfare and Rehabilitation Sciences has reviewed, approved and approved the research plan (Code: IR.USWR.REC.1397.083).
Translation and Cultural Adaptation of the questionnaire
The translation process was based on 5 stages of translation and cultural adaptation suggested by Beaton [22]. Two speech and language pathologists translated the questionnaire into Persian. The final version was translated into English by two bilingual translators, and after the translators agreed, the translated version was compared with the original version and sent to the author of the questionnaire, and the accuracy of the translation of the concepts was confirmed. Then the Persian version of the questionnaire was evaluated by two neurologists and two speech and language pathologists in the field of swallowing. Finally, these experts agreed on the Persian version of the questionnaire (P-DYMUS). The final version of the questionnaire was distributed among 10 patients and they expressed their views on the clarity, simplicity and comprehensibility of the questionnaire items.
Reliability and validity
Confirmatory Factor Analysis (CFA) was used to evaluate the validity of the structure. In the present study, the most common indicators of goodness of fit that have been introduced to test the validity of the model [23, 24], were used. Also, the operational ability of the questionnaire to identify swallowing disorders was assessed by self-reported method [25, 26]. Before completing the questionnaire, all patients were asked the question “Do you have difficulty swallowing?”
Convergent validity of the questionnaire was assessed by examining the relationship between P-DYMUS scores and Dysphagia Handicap Index (DHI) scores. The DHI questionnaire is used to identify swallowing disorders and its effect on quality of life [27]. This questionnaire has been translated into Persian and its Persian version has a high internal stability (Cronbach’s alpha coefficient between 0.82 to 0.94) and also the reliability of the high retest test (r=0.89) [28].
Kuder Richardson 20 (KR-20) was used to estimate the internal consistency of the Swallowing Disturbance Questionnaire as a general concept as well as for its two subgroups. The correlation matrix between items was also calculated to assess the homogeneity of the items. Reliability by open test method was performed on 19 participants with a time interval of 2 weeks [29].
Statistical analysis
In the present study, KR-20 reliability coefficient, Intra-cluster Correlation Coefficient (ICC), item correlation matrix, Mann-Whitney test and Spearman rank correlation coefficient were used. Statistical analysis was performed using SPSS V. 16 and LISREL V. 8.8. P<0.05 was considered as the level of significance.
Results
In this study, 108 patients including 76 females and 32 males participated. Of them, 80 patients were Relapsing-remitting (RR), 17 patients were Secondary Progressive (SP) and 11 patients were Primary Progressive (PP). The mean age of patients was 36.8 years, the mean duration of illness was 10.4 years and the mean EDSS score was 3.1 (Table 1).
Validity and reliability of P-DYMUS
According to the findings of the Mann-Whitney test, people who answered positively to the initial question “Do you have difficulty swallowing?” had higher scores on P-DYMUS compared to patients who responded negatively (P<0.001; Z score=-6.734). This result indicates the distinguishing power of the questionnaire between people with and without swallowing disorders. Matrix analysis of the correlation between items showed a positive correlation between all items. The range of correlation coefficients between items was 0.003 to 0.627 and the lowest correlation coefficient was related to item 10 (Table 2).
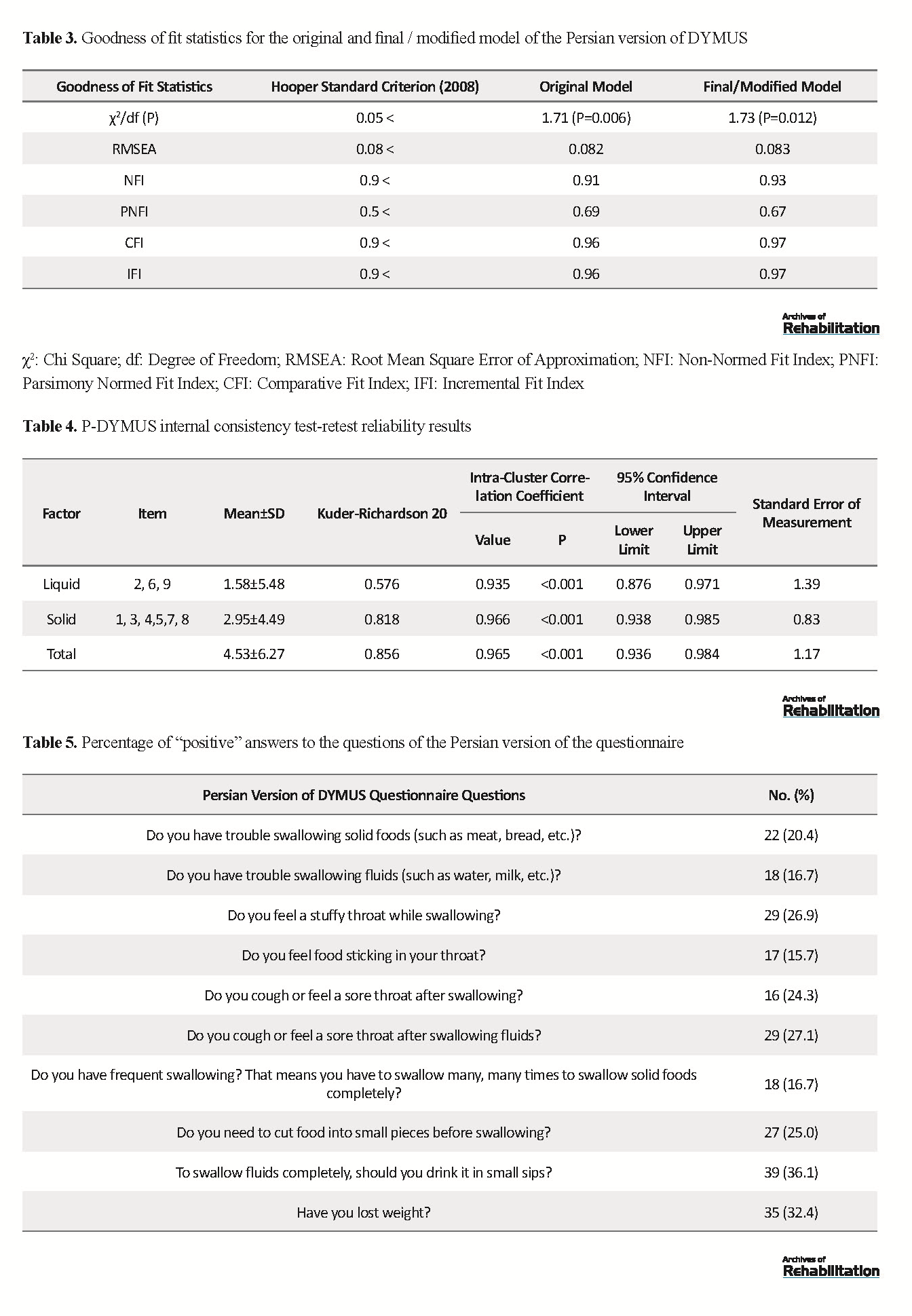
Confirmatory factor analysis was used to compare the fit indices of 9-item and 10-item P-DYMUS models and to examine the main structure of the questionnaire. Due to the low correlation of item 10, this item was removed from the model and the obtained 9-item model showed the best goodness of fit with the observed data. Table 3 shows the main indicators of model fit. Of the two proposed models, the 9-item model showed the best fit for the sample data (Figure 1, Table 3). The CFA results showed that item 10 had the least effect in measuring »solids swallowing disorder«. Figure 1 (confirmatory factor analysis diagram) shows the final model diagram with the factor loads of the remaining items (between 0.52 and 0.76).
According to the findings of the Mann-Whitney test, people who answered positively to the initial question “Do you have difficulty swallowing?” had higher scores on P-DYMUS compared to patients who responded negatively (P<0.001; Z score=-6.734). This result indicates the distinguishing power of the questionnaire between people with and without swallowing disorders. Matrix analysis of the correlation between items showed a positive correlation between all items. The range of correlation coefficients between items was 0.003 to 0.627 and the lowest correlation coefficient was related to item 10 (Table 2).
Confirmatory factor analysis was used to compare the fit indices of 9-item and 10-item P-DYMUS models and to examine the main structure of the questionnaire. Due to the low correlation of item 10, this item was removed from the model and the obtained 9-item model showed the best goodness of fit with the observed data. Table 3 shows the main indicators of model fit. Of the two proposed models, the 9-item model showed the best fit for the sample data (Figure 1, Table 3). The CFA results showed that item 10 had the least effect in measuring »solids swallowing disorder«. Figure 1 (confirmatory factor analysis diagram) shows the final model diagram with the factor loads of the remaining items (between 0.52 and 0.76).
To evaluate the convergent validity, the relationship between P-DYMUS questionnaire scores and DHI questionnaire scores was examined. The result of Spearman correlation coefficient showed a significant positive correlation between the scores of these two questionnaires (P>0.001, rs=0.693).
The reliability coefficient of KR-20 of P-DYMUS questionnaire was equal to 0.856, which indicates the high internal stability of the Persian version of the questionnaire items. KR-20 was also calculated for two swallowing disorder subscales for solids and liquids. The KR-20 value was 0.818 for 6 items of swallowing disorder for solids and 0.576 for 3 items of swallowing disorder for liquids. The reliability of the open test was excellent and the ICC for the whole score was 0.965 (P>0.001) (Table 4).
Findings related to P-DYMUS
Table 5 shows the percentage of positive answers to P-DYMUS questions. According to P-DYMUS results, 34.3% of patients were in the group without swallowing disorders and 65.7% of patients were in the group with swallowing disorders. Regarding the severity of swallowing disorder, 25.9% of participants had mild swallowing disorder and 39.8% had warning swallowing disorder. The mean scores of the questionnaire in SP patients were significantly higher than RR patients (P= 0.023, Z= -2.265), but the difference between the mean scores of P-DYMUS in PP and SP patients (P= 0.492, Z= -0.688) and PP and RR patients (P= 0.283, Z= -0.074) were not significant. Spearman correlation coefficient also showed that P-DYMUS scores had a significant positive correlation with disease duration (p=0.040, rs=0.198) and EDSS score (P= 0.014, rs =0.235).
The reliability coefficient of KR-20 of P-DYMUS questionnaire was equal to 0.856, which indicates the high internal stability of the Persian version of the questionnaire items. KR-20 was also calculated for two swallowing disorder subscales for solids and liquids. The KR-20 value was 0.818 for 6 items of swallowing disorder for solids and 0.576 for 3 items of swallowing disorder for liquids. The reliability of the open test was excellent and the ICC for the whole score was 0.965 (P>0.001) (Table 4).
Findings related to P-DYMUS
Table 5 shows the percentage of positive answers to P-DYMUS questions. According to P-DYMUS results, 34.3% of patients were in the group without swallowing disorders and 65.7% of patients were in the group with swallowing disorders. Regarding the severity of swallowing disorder, 25.9% of participants had mild swallowing disorder and 39.8% had warning swallowing disorder. The mean scores of the questionnaire in SP patients were significantly higher than RR patients (P= 0.023, Z= -2.265), but the difference between the mean scores of P-DYMUS in PP and SP patients (P= 0.492, Z= -0.688) and PP and RR patients (P= 0.283, Z= -0.074) were not significant. Spearman correlation coefficient also showed that P-DYMUS scores had a significant positive correlation with disease duration (p=0.040, rs=0.198) and EDSS score (P= 0.014, rs =0.235).
Discussion
Lack of early diagnosis and late management of swallowing disorders can cause serious problems. Therefore, it is necessary to use a simple, fast, valid and reliable tool to screen swallowing disorders in these patients. In the present study, the DYMUS questionnaire was translated and its psychometric properties were evaluated in 108 MS patients.
The results of this study in line with the results of previous studies [13, 15] showed that the mean scores of P-DYMUS were higher in patients who reported the presence of swallowing disorders compared to patients who reported the absence of swallowing disorders. This finding demonstrates the ability of this questionnaire to differentiate between patients with and without swallowing disorders. Findings on convergent validity also indicated a positive correlation between P-DYMUS scores and DHI.
Findings related to test-retest reliability showed that P-DYMUS questionnaire is a reliable tool in diagnosing swallowing disorders. The results in line with the findings of the present study for reliability by the test-retest method have been reported in previous studies [14, 18, 19]. Based on the findings of KR-20 reliability coefficient, the present study showed that the Persian version of the questionnaire has high internal stability. The value of internal consistency in previous studies has been reported for the Italian version of the questionnaire [13] 0.914, the Portuguese version [15] 0.72, the Turkish version [17] 0.91 and the Greek version [14] 0.866. These results indicate the similarity of the questionnaire items and consequently its reliability.
The results of item correlation matrix analysis in the present study showed a positive correlation between all items except item 10 (Have you lost weight?) Item 10 had the lowest correlation coefficient in the present study and studies by Sales et al. [15], Alali et al. [18] And showed Printza et al. [14]. This item in the original version of DYMUS also had a low correlation with other items [13]. Contrary to the findings of studies by Jafari et al. [19] and Assadollahpour et al. [20], the results of CFA in the present study showed that item 10 has the least help in identifying swallowing disorders and by removing this item the internal consistency of the questionnaire increases. Also, the modified 9-item questionnaire achieved the best fit.
This finding is in line with previous studies that have proposed a modified 9-item version of the questionnaire based on the findings of factor analysis [18, 14]. One possible reason for this finding is that dysphagia is just one of the causes of weight loss in MS patients. Numerous causes such as side effects of drugs, decreased mobility, fatigue and depression lead to malnutrition and dehydration in these patients [30, 31]. Another reason that can be suggested is that MS patients in this study had mild degrees of disability (their mean EDSS score was 3.1). However, the association between weight loss and swallowing disorders is seen in advanced levels of neurological disorders in patients [31].
Another purpose of this study was to evaluate the frequency and severity of swallowing disorders in people with MS in Tehran. Findings of this study showed that swallowing disorder is a common problem in MS patients (65.7%) and the percentage of warning swallowing disorder is higher than mild swallowing disorder. The frequency of swallowing disorders in MS patients using DYMUS questionnaire in studies by Sales et al. [15], Bergamaschi et al. [12, 13] and Daneshpajooh et al. [32] also reported 58%, 35%, 31% and 54%, respectively. Has been. The differences in the frequency of swallowing disorders in different studies may be related to the different characteristics of the studies. Recently, based on the findings of a meta-analysis study, the prevalence of swallowing disorders has been estimated between 10 and 90% depending on the diagnosis method and the study population [7].
Another finding of this study was the existence of a significant relationship between swallowing disorder and MS type for SP subgroup, which is in line with previous studies [33, 34]. The severity of swallowing disorder was higher in SP subgroup than the other two subgroups, indicating that patients with progressive and secondary forms of the disease often have more severe swallowing disorders. Also, as reported in previous studies [8, 10, 31], P-DYMUS scores were significantly correlated with disease duration and EDSS score. Swallowing disorders were more common in patients with higher EDSS scores and longer duration of illness. Another notable finding is that in the present study, as reported in the scholarly study [32], a number of patients with low EDSS scores were diagnosed with swallowing disorders. In the study of Abraham et al. [35], it was reported that out of 43% of MS patients with swallowing disorders, about 17% had low levels of disability (EDSS score lower than 2.5). Based on this, it can be said that although EDSS is an indicator of performance and disability level of MS patients [36], but it does not indicate the severity of swallowing disorder and screening tools such as DYMUS questionnaire provide additional information about patients’ ability to swallow. it helps. Having a comprehensive profile of the patient’s condition, including information such as the type of MS, the duration of the illness, and the EDSS score, although not a predictor of swallowing disorder, is useful as a clue to the severity of swallowing disorder.
It should be noted that the sample of the present study was extracted only from an MS center in Tehran, which may limit the generalization of the study findings to other clinical centers or the communities. Also, in this study, the diagnostic accuracy (sensitivity and specificity) of the DYMUS questionnaire was not evaluated.
Conclusion
The modified 9-item Persian version of DYMUS is a simple, stable, valid, and reliable tool for the initial diagnosis of swallowing disorder and early referral for specific instrumental assessments that has better validity and reliability indicators than the 10-item version of the questionnaire. Our findings showed that the frequency of swallowing disorders in MS patients is high and is related to the advanced form of the disease, the duration of the disease and the EDSS score. Therefore, therapists and patients need to consider swallowing disorder as a serious problem that needs to be evaluated and intervened to prevent subsequent problems.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1397.83). All ethical principles are considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; moreover, they were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
The present paper was extracted from the research project of Zahra Sadeghi, Approved by the Student Research Committee, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Authors' contributions
Conceptualization: All authors; Methodology, analysis: Zahra Sadeghi, Mohammad Reza Afshar, Kowsar Baghban, Abbas Ebadi; Drafting: Zahra Sadeghi and Mohammad Reza Afshar; Editing and finalizing: Kowsar Baghban, Abbas Ebadi, Zahrasadat Qureshi, Supervision: Zahra Sadat Qureshi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank Dr. Mona Ibrahimipour for her contribution in this study.
Lack of early diagnosis and late management of swallowing disorders can cause serious problems. Therefore, it is necessary to use a simple, fast, valid and reliable tool to screen swallowing disorders in these patients. In the present study, the DYMUS questionnaire was translated and its psychometric properties were evaluated in 108 MS patients.
The results of this study in line with the results of previous studies [13, 15] showed that the mean scores of P-DYMUS were higher in patients who reported the presence of swallowing disorders compared to patients who reported the absence of swallowing disorders. This finding demonstrates the ability of this questionnaire to differentiate between patients with and without swallowing disorders. Findings on convergent validity also indicated a positive correlation between P-DYMUS scores and DHI.
Findings related to test-retest reliability showed that P-DYMUS questionnaire is a reliable tool in diagnosing swallowing disorders. The results in line with the findings of the present study for reliability by the test-retest method have been reported in previous studies [14, 18, 19]. Based on the findings of KR-20 reliability coefficient, the present study showed that the Persian version of the questionnaire has high internal stability. The value of internal consistency in previous studies has been reported for the Italian version of the questionnaire [13] 0.914, the Portuguese version [15] 0.72, the Turkish version [17] 0.91 and the Greek version [14] 0.866. These results indicate the similarity of the questionnaire items and consequently its reliability.
The results of item correlation matrix analysis in the present study showed a positive correlation between all items except item 10 (Have you lost weight?) Item 10 had the lowest correlation coefficient in the present study and studies by Sales et al. [15], Alali et al. [18] And showed Printza et al. [14]. This item in the original version of DYMUS also had a low correlation with other items [13]. Contrary to the findings of studies by Jafari et al. [19] and Assadollahpour et al. [20], the results of CFA in the present study showed that item 10 has the least help in identifying swallowing disorders and by removing this item the internal consistency of the questionnaire increases. Also, the modified 9-item questionnaire achieved the best fit.
This finding is in line with previous studies that have proposed a modified 9-item version of the questionnaire based on the findings of factor analysis [18, 14]. One possible reason for this finding is that dysphagia is just one of the causes of weight loss in MS patients. Numerous causes such as side effects of drugs, decreased mobility, fatigue and depression lead to malnutrition and dehydration in these patients [30, 31]. Another reason that can be suggested is that MS patients in this study had mild degrees of disability (their mean EDSS score was 3.1). However, the association between weight loss and swallowing disorders is seen in advanced levels of neurological disorders in patients [31].
Another purpose of this study was to evaluate the frequency and severity of swallowing disorders in people with MS in Tehran. Findings of this study showed that swallowing disorder is a common problem in MS patients (65.7%) and the percentage of warning swallowing disorder is higher than mild swallowing disorder. The frequency of swallowing disorders in MS patients using DYMUS questionnaire in studies by Sales et al. [15], Bergamaschi et al. [12, 13] and Daneshpajooh et al. [32] also reported 58%, 35%, 31% and 54%, respectively. Has been. The differences in the frequency of swallowing disorders in different studies may be related to the different characteristics of the studies. Recently, based on the findings of a meta-analysis study, the prevalence of swallowing disorders has been estimated between 10 and 90% depending on the diagnosis method and the study population [7].
Another finding of this study was the existence of a significant relationship between swallowing disorder and MS type for SP subgroup, which is in line with previous studies [33, 34]. The severity of swallowing disorder was higher in SP subgroup than the other two subgroups, indicating that patients with progressive and secondary forms of the disease often have more severe swallowing disorders. Also, as reported in previous studies [8, 10, 31], P-DYMUS scores were significantly correlated with disease duration and EDSS score. Swallowing disorders were more common in patients with higher EDSS scores and longer duration of illness. Another notable finding is that in the present study, as reported in the scholarly study [32], a number of patients with low EDSS scores were diagnosed with swallowing disorders. In the study of Abraham et al. [35], it was reported that out of 43% of MS patients with swallowing disorders, about 17% had low levels of disability (EDSS score lower than 2.5). Based on this, it can be said that although EDSS is an indicator of performance and disability level of MS patients [36], but it does not indicate the severity of swallowing disorder and screening tools such as DYMUS questionnaire provide additional information about patients’ ability to swallow. it helps. Having a comprehensive profile of the patient’s condition, including information such as the type of MS, the duration of the illness, and the EDSS score, although not a predictor of swallowing disorder, is useful as a clue to the severity of swallowing disorder.
It should be noted that the sample of the present study was extracted only from an MS center in Tehran, which may limit the generalization of the study findings to other clinical centers or the communities. Also, in this study, the diagnostic accuracy (sensitivity and specificity) of the DYMUS questionnaire was not evaluated.
Conclusion
The modified 9-item Persian version of DYMUS is a simple, stable, valid, and reliable tool for the initial diagnosis of swallowing disorder and early referral for specific instrumental assessments that has better validity and reliability indicators than the 10-item version of the questionnaire. Our findings showed that the frequency of swallowing disorders in MS patients is high and is related to the advanced form of the disease, the duration of the disease and the EDSS score. Therefore, therapists and patients need to consider swallowing disorder as a serious problem that needs to be evaluated and intervened to prevent subsequent problems.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1397.83). All ethical principles are considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; moreover, they were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
The present paper was extracted from the research project of Zahra Sadeghi, Approved by the Student Research Committee, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Authors' contributions
Conceptualization: All authors; Methodology, analysis: Zahra Sadeghi, Mohammad Reza Afshar, Kowsar Baghban, Abbas Ebadi; Drafting: Zahra Sadeghi and Mohammad Reza Afshar; Editing and finalizing: Kowsar Baghban, Abbas Ebadi, Zahrasadat Qureshi, Supervision: Zahra Sadat Qureshi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank Dr. Mona Ibrahimipour for her contribution in this study.
Type of Study: Original |
Subject:
Speech & Language Pathology
Received: 20/05/2019 | Accepted: 15/09/2019 | Published: 1/07/2020
Received: 20/05/2019 | Accepted: 15/09/2019 | Published: 1/07/2020
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |