Volume 24, Issue 3 (Autumn 2023)
jrehab 2023, 24(3): 382-397 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Taheri M, Talebi G, Taghipour M, Bahrami M, Gholinia H. Frequency of Adverse Neural Tension and Its Association With Functional Disability in Upper Extremity Musculoskeletal Pain Syndromes: A Cross-sectional Study. jrehab 2023; 24 (3) :382-397
URL: http://rehabilitationj.uswr.ac.ir/article-1-3263-en.html
URL: http://rehabilitationj.uswr.ac.ir/article-1-3263-en.html
1- Department of Physiotherapy, School of Rehabilitation, Babol University of Medical Sciences, Babol, Iran., Babol University of Medical Sciences
2- Mobility Impairment Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran. ,talebiali2@yahoo.co.in
3- Mobility Impairment Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran., Babol University of Medical Sciences
4- Department of Orthopedic, School of Medicine, Babol University of Medical Sciences, Babol, Iran., Babol University of Medical Sciences
5- Health Research Center, Babol University of Medical Sciences, Babol, Iran., Babol University of Medical Sciences
2- Mobility Impairment Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran. ,
3- Mobility Impairment Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran., Babol University of Medical Sciences
4- Department of Orthopedic, School of Medicine, Babol University of Medical Sciences, Babol, Iran., Babol University of Medical Sciences
5- Health Research Center, Babol University of Medical Sciences, Babol, Iran., Babol University of Medical Sciences
Keywords: Neurodynamic test, Peripheral nerves, Median nerve, Radial nerve, Ulnar nerve, Upper extremity, Musculoskeletal pain syndrome
Full-Text [PDF 3354 kb]
(396 Downloads)
| Abstract (HTML) (4912 Views)
Full-Text: (537 Views)
Introduction
Musculoskeletal diseases rank among the most prevalent causes of long-term pain and physical disability worldwide [1, 2]. Musculoskeletal injuries result from overuse after prolonged and inappropriate repetitive movements and submaximal loads [3, 4]. Based on the pathomechanics of musculoskeletal pain syndrome, recent studies have reported the possibility of concurrent dynamic disorders and adverse neural tension in these syndromes [5-11]. In the same way, poor posture and inappropriate repetitive movements can predispose people to musculoskeletal pain syndromes, they may also affect the nerve neurodynamic (sliding, elongation, and normal tension capability of nerves). When we talk about neural tension or dynamic disorders, it does not necessarily involve severe damage, such as tearing or crushing, but rather disorders of the movement of nerve structures within the surrounding tissues or disorders in the nerve’s normal elongation or normal tensionability. In neural tension disorders, the nerve may still not have a problem regarding its ability to conduct signals. Still, it functions abnormally in terms of movement tolerance and stretchability, and for this reason, it causes symptoms [12-14]. Nerve conduction studies and electrodiagnostic findings may be normal in these patients because no high correlation exists between subjective clinical symptoms and electrodiagnostic findings [15, 16].
Regarding the intricate relationship between the mechanical and physiological functions of the nervous system, any disturbance in them can be evaluated through neurodynamic maneuvers [12, 13, 17]. Neurodynamic maneuvers serve as both clinical evaluation tools and manual treatment in many patients with neuromuscular system disorders [5, 12, 18].
The high recurrence rate and inability to fully explain the symptoms of patients with musculoskeletal pain syndromes may be associated with overlooked dynamic nerve disorders in evaluations and conventional treatment protocols. To our knowledge, little information and evidence exist regarding neurodynamic disturbances with overuse musculoskeletal pain syndromes. As a result, for patients who refer to physiotherapy with the diagnosis of musculoskeletal pain syndrome, the treatment is usually focused on the musculoskeletal structures, and less attention is paid to neurodynamic evaluation [14]. Therefore, the assessment and planning of physical therapy could be improved by understanding the prevalence of adverse neural tension in such patients and the relationship between pain intensity and functional disability. Also, most studies in this field have involved a limited number of participants [5, 6], and there is no exact estimation of the frequency of adverse neural tension in patients with these syndromes. Consequently, this study was primarily conducted to determine the frequency of adverse neural tension and its relationship with functional disability in upper extremity musculoskeletal pain syndromes.
Materials and Methods
This single-blind cross-sectional study was conducted at Shahid Beheshti Hospital in Babol City, Iran, from May 2021 to June 2022. The sample size was determined using relevant literature [11], resulting in recruiting 100 patients with musculoskeletal pain syndromes based on the inclusion and exclusion criteria.
The inclusion criteria included individuals aged 20 to 50 years diagnosed with upper extremity musculoskeletal pain syndromes, including shoulder impingement syndrome, lateral and medial epicondylitis of the elbow, and De Quervain syndrome [19-22]. The exclusion criteria comprised consumption of anti-inflammatory and analgesic drugs in the last 24 hours, suffering from systemic diseases (eg. diabetes, arthrosis, and rheumatoid arthritis), history of the spine and upper extremity surgery, restrictions of joint movement (eg. acute inflammation, infection, tissue tear, and fracture), severe trauma in the last 3 months, diseases that lead to adverse neural tension (such as cervical radiculopathy and peripheral neuropathies), bone abnormalities (eg. rib cervical and rostral acromion), a history of corticosteroid injection in the past one month, a history of physiotherapy treatment in the past 3 months, and significant limitations in the range of motion in each joint of the upper extremity, preventing the implementation of the neurodynamic test [23-26].
Data collection
Demographic information was collected via a standard questionnaire covering age, gender, height, weight, and duration of the lesion. Body mass index (BMI) was calculated by dividing weight in kg by the square of body height in meters [27]. Pain intensity was assessed through a visual analog scale (VAS) [28]. The functional disability of the upper extremity was investigated using the quick disabilities of the arm, shoulder, and hand (QDASH) questionnaire [29]. Ebrahimzadeh et al. proved the validity and reliability of the Persian version of this questionnaire [30].
Neurodynamic assessment
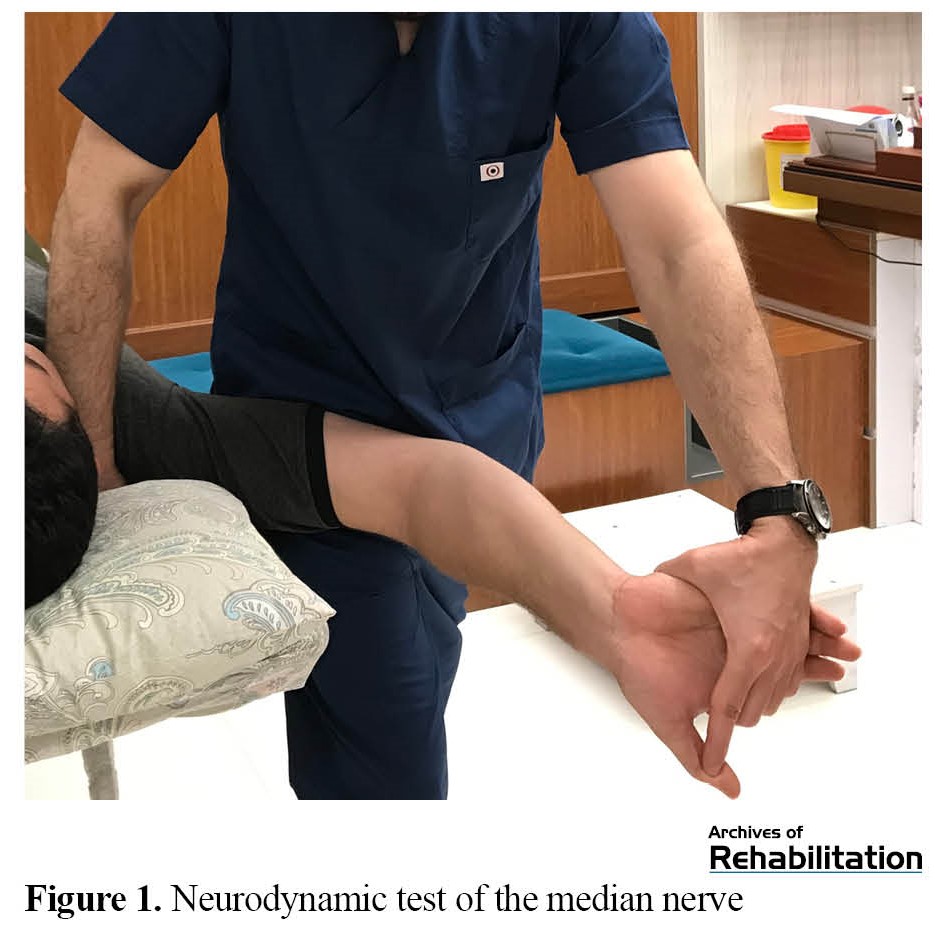
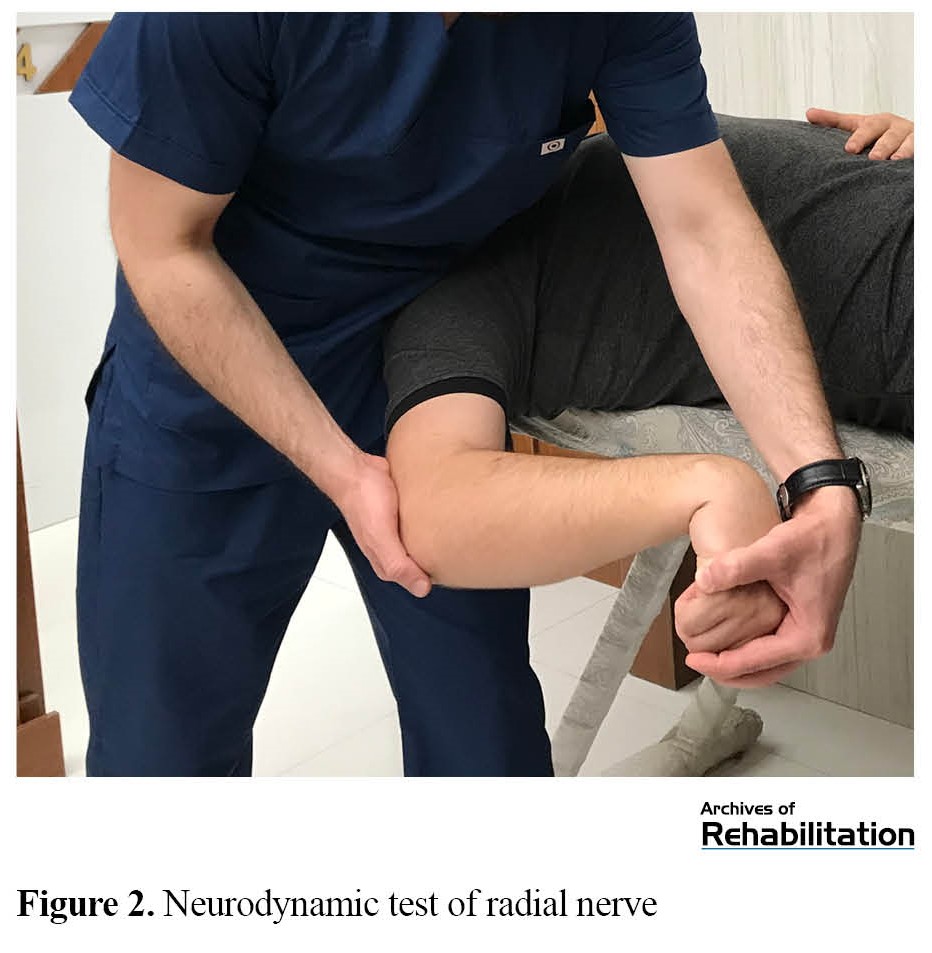
Before starting the main phase of the study, the reproducibility of these tests was examined by one intraexaminer and two interexaminers. 24 asymptomatic people participated in this study [31]. Neurodynamic evaluation was performed using the standard method provided by Shacklock and Butler for the median (Figure 1), radial (Figure 2), and ulnar (Figure 3) nerves bilaterally for both upper extremities [13, 32]. A 5 minute rest was observed between each test to avoid the therapeutic effects of the neurodynamic maneuver [33, 34]. Joint angles were measured using a standard goniometer according to the method of Martínez et al. and Covill et al. [35, 36]. For the neurodynamic evaluation of the median and radial nerves, the extension angle of the elbow joint, and for assessing the ulnar nerve, the abduction angle of the shoulder joint was measured when the test was positive.
The structural differentiation test determines the neurodynamic test’s positive result [13, 32]. If the patients’ symptoms increased during the neurodynamic test, increasing or decreasing the cumulative tension in the nerve on the reproduced symptoms was checked by moving a component completely away from the place of reporting the symptoms [13, 32]. When the main symptoms or complaints of the patients were not reproduced or aggravated by neurodynamic tests, the difference in the range of motion measured between the two extremities was recorded when a strong stretch was felt in the tested extremity. A significant difference in range of motion between elbow extension range (for median and radial nerve neurodynamic tests) and shoulder abduction range (for ulnar nerve neurodynamic test) on both sides was considered a positive neurodynamic evaluation. This difference was considered 27° for the median nerve, 20° for the radial nerve, and 6° for the ulnar nerve [35, 36].
Statistical analysis
Statistical analysis was performed using SPSS software, version 24. The relationship between quantitative variables was examined using the Pearson correlation test. The normality of the distribution of the variables was analyzed using the Kolmogorov-Smirnov test, indicating a normal distribution for all study variables. In this analysis, a P<0.05 was considered statistically significant.
Results
The demographic characteristics, including age, gender, height, weight, and BMI, were analyzed among the participants (Table 1).

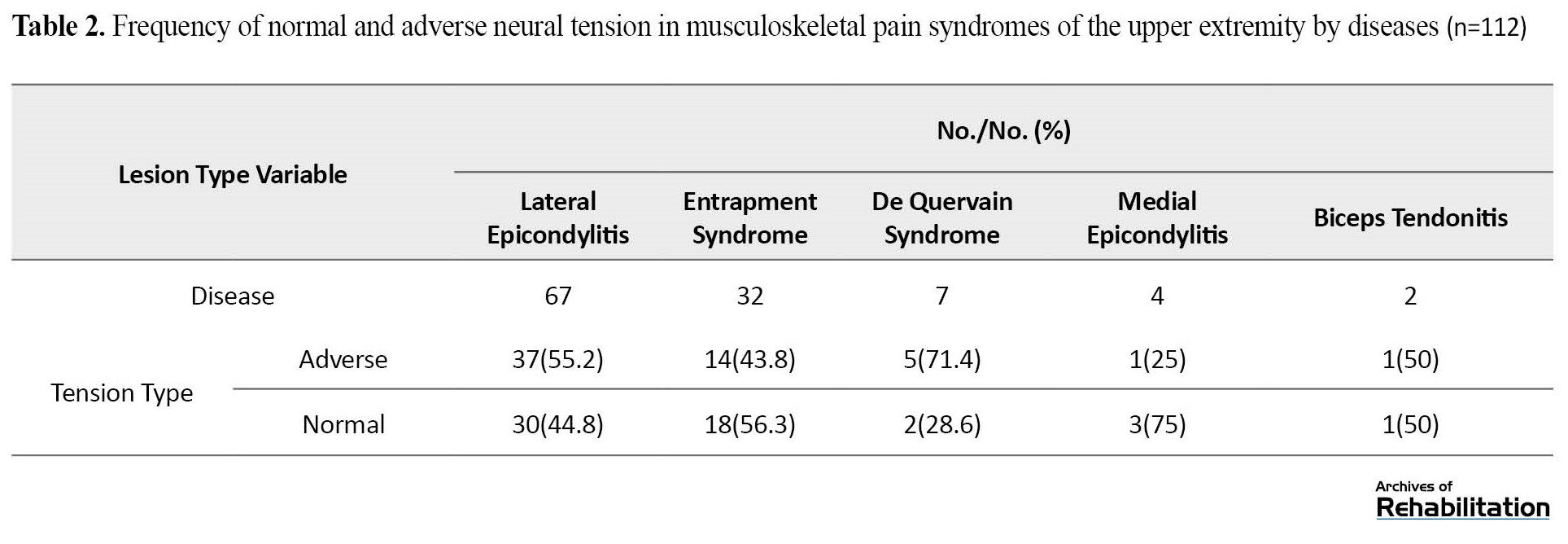
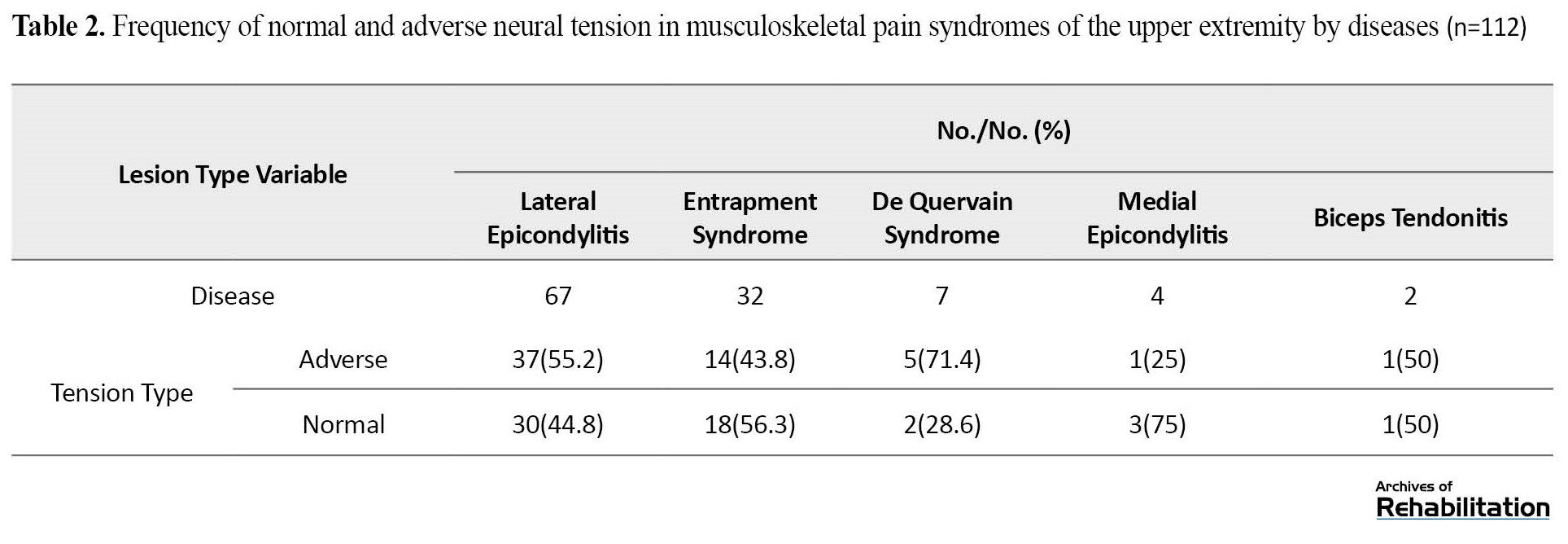
The result of data frequency analysis showed that regardless of the type of lesion, out of 100 participants (some participants had more than one disease, a total of 112 cases of the disease were reported) who underwent neurodynamic evaluation, 50 patients (50%) exhibited at least one disorder in median, radial, or ulnar neural tension so that neurodynamic tests in 19 patients (19%) led to the reproduction or exacerbation of symptoms and in 39 patients (39%), a significant difference was observed in range of motion of joints on both sides. Table 2 presents the frequency of normal and adverse neural tension in upper extremity musculoskeletal pain syndromes by disease.
In 28 patients, the neurodynamic test of the median nerve yielded a positive result. Of these, the positive result of the median nerve test in 8 patients (8%) was based on the reproduction and worsening of symptoms, and in 20 patients (20%), based on a significant difference (>27°) in the elbow joint extension range of motion between the two sides.
In 30 patients (30%), adverse neural tension of the radial nerve was observed. The positive neurodynamic test of the radial nerve in 21 patients (21%) was based on the reproduction of symptoms and in 9 patients (9%) based on a significant difference (>20°) between the two sides in the range of motion of elbow joint extension.
The neurodynamic evaluation of the ulnar nerve showed that in 9 patients (9%), a significant difference (>6°) was observed in the abduction angle of the shoulder joint in both hands. In none of the participants, the neurodynamic test of the ulnar nerve led to the reproduction or exacerbation of symptoms.
The Pearson correlation test demonstrated no significant relationship between the level of functional disability and the intensity of adverse neural tension (according to the extension angle of the elbow joint) of the median and radial nerves. In addition, no significant relationship was observed between the level of functional disability and the severity of adverse neural tension (in terms of the abduction angle of the shoulder joint) of the ulnar nerve (Table 3).

Discussion
The results of our study indicate that at least one neurodynamic test was positive in 50% of patients with upper limb musculoskeletal pain syndromes (regardless of the type of lesion). Yaxley and Jull [11], showed adverse neural tension in some patients with tennis elbow; in addition, several other studies have pointed to neurodynamic disorders in patients with musculoskeletal pain syndromes [5, 6, 10].
The high prevalence of adverse neural tension observed may be due to different definitions of concepts and criteria for considering neurodynamic tests positive. This issue may lead to differences in the interpretation of the results of the study studies, especially when the positive criterion for the concept of adverse neural tension is crucial. The limited range of motion of the joints and the significant difference with the other side can be caused by the stretching of the muscle structures, its effect on the mechanical sensitivity of the nerve roots, and the creation of adverse neural tension [37].
The results showed that the highest frequency of adverse neural tension in the upper extremity was related to the radial nerve, followed by the median nerve, and the least frequency in the ulnar nerve. The high adverse radial neural tension rate can be explained by the higher prevalence of lateral epicondylitis among participants (67%) despite a higher incidence of shoulder impingement syndrome [38, 39]. The frequency of adverse tension of the radial nerve in patients with lateral epicondylitis was 40.3%; this rate was lower than the results of Yaxeley et al. [11]. Adverse neural tension of the radial nerve in patients with De Quervain syndrome may be due to the involvement of the superficial branch of the radial nerve in patients with this syndrome [40].
The adverse radial neural tension in patients with medial epicondylitis and shoulder impingement syndrome may be due to the transmission of the generated tension to the brachial plexus. As Kleinrensink et al. have shown, when a specific nerve in the upper extremity is examined via neurodynamic tests, the tension is transferred to the proximal part and the brachial plexus. A disorder in the common nerve roots can lead to reproduction or worsening symptoms [41].
The median nerve innervates the muscles involved in medial epicondylitis. Regarding the common nerve roots in the median and radial nerves (C6-8 roots), suprascapular, axillary, and radial nerves (C6 root), the disorder in common nerve roots can lead to adverse tension during the radial nerve test in patients with medial epicondylitis and shoulder impingement syndrome.
Regarding the common roots of the median nerve with the suprascapular, axillary, musculocutaneous (C6 root), and radial (C6-8 root) nerves, it is possible to check the disorders of these nerve roots with the median nerve test [41]. In addition, the muscle structures involved in medial epicondylitis are directly fed by the median nerve. The results showed that with regard to the more specific median nerve test compared to the radial and ulnar nerves; we can use this test to evaluate nerves with common roots [41].
The neurodynamic test of the ulnar nerve did not lead to the reproduction or worsening of symptoms in any participant; however, in 9 patients, a significant difference was observed in the abduction angle of the shoulder joint on both sides. The absence of reproduction or worsening of symptoms may be attributed to the level of tension disorder of the ulnar nerve, as it is lower than the other two nerves, and patients who suffer from tension disorders of the ulnar nerve show mild, latent, and subclinical symptoms. These disorders can manifest as limitations in the range of motion of the joints. In addition, none of the structures involved in the investigated lesions were directly innervated by the ulnar nerve.
Like Vegstein et al. and Fernández-de-Las-Peñas et al. study, our research suggests that patients with musculoskeletal pain syndromes may not initially present neurological symptoms [10, 42]. However, according to neurological theory, injury to musculoskeletal structures can lead to microscopic damage in the connective tissue of peripheral nerves, affecting the axoplasmic flow of nerves and disrupting nerve function [14, 43]. To our knowledge, past studies have not reported the prevalence or the role of adverse neural tension disorders in patients with upper extremity musculoskeletal pain syndromes, making it impossible to compare the obtained results with other studies.
According to our results, in patients with musculoskeletal pain syndromes with adverse neural tension, no significant relationship was observed between the level of functional disability, pain intensity, lesion duration, age, and BMI with the severity of adverse neural median, radial, and ulnar tension. In patients with higher intensity of adverse neural median and radial tension, the test becomes positive sooner (at higher angles) during a neurodynamic test when the elbow joint is extended. However, in the patients with higher intensity of adverse neural ulnar tension, the test becomes positive sooner (at lower angles) during a neurodynamic test when the elbow joint is extended.
Conclusion
According to our results, at least one of the neurodynamic tests becomes positive in a significant percentage of patients with upper extremity musculoskeletal pain syndromes. Considering the outcomes of this study, it is necessary to consider the neurological component in evaluating patients with musculoskeletal pain syndromes. A neurodynamic assessment helps therapists assess the role and contribution of neurological disorders in the development of symptoms, facilitating the design of an appropriate treatment plan based on the etiology of the injury.
Ethical Considerations
Compliance with ethical guidelines
Objectives, procedures, possible advantages and disadvantages of the study clearly for the participants were explained. Each participant signed a written informed consent form. All methods in accordance with ethical approval and guidelines and regulations the relevant was done at the study site. The study protocol was approved by the Ethics Committee of Babol University of Medical Sciences (Code: IR.MUBABOL.REC.1400.063).
Funding
The paper was extracted from the master's thesis of Milad Taheri, approved by the Department of Physiotherapy, School of Rehabilitation, Babol University of Medical Sciences. This study was also supported by Vice President of Research and Technology of Babol University of Medical Sciences.
Authors' contributions
Conceptualization: Milad Taheri, Ghadamali Talebiand Mohammad Taghipour; Methodology and validation: Milad Taheri, Ghadamali Talebi, Mohammad Taghipour and Massoud Bahrami; Visualization: Milad Taheri; Analysis and research: All authors; Writing-original draft: Milad Taheri; Editing and finalization: Ghadamali Talebi, Mohammad Taghipour; Supervision: Ghadamali Talebi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate and thank the honorable personnel of the physiotherapy department of Shahid Beheshti Hospital in Babol for the services of this study.
References
Musculoskeletal diseases rank among the most prevalent causes of long-term pain and physical disability worldwide [1, 2]. Musculoskeletal injuries result from overuse after prolonged and inappropriate repetitive movements and submaximal loads [3, 4]. Based on the pathomechanics of musculoskeletal pain syndrome, recent studies have reported the possibility of concurrent dynamic disorders and adverse neural tension in these syndromes [5-11]. In the same way, poor posture and inappropriate repetitive movements can predispose people to musculoskeletal pain syndromes, they may also affect the nerve neurodynamic (sliding, elongation, and normal tension capability of nerves). When we talk about neural tension or dynamic disorders, it does not necessarily involve severe damage, such as tearing or crushing, but rather disorders of the movement of nerve structures within the surrounding tissues or disorders in the nerve’s normal elongation or normal tensionability. In neural tension disorders, the nerve may still not have a problem regarding its ability to conduct signals. Still, it functions abnormally in terms of movement tolerance and stretchability, and for this reason, it causes symptoms [12-14]. Nerve conduction studies and electrodiagnostic findings may be normal in these patients because no high correlation exists between subjective clinical symptoms and electrodiagnostic findings [15, 16].
Regarding the intricate relationship between the mechanical and physiological functions of the nervous system, any disturbance in them can be evaluated through neurodynamic maneuvers [12, 13, 17]. Neurodynamic maneuvers serve as both clinical evaluation tools and manual treatment in many patients with neuromuscular system disorders [5, 12, 18].
The high recurrence rate and inability to fully explain the symptoms of patients with musculoskeletal pain syndromes may be associated with overlooked dynamic nerve disorders in evaluations and conventional treatment protocols. To our knowledge, little information and evidence exist regarding neurodynamic disturbances with overuse musculoskeletal pain syndromes. As a result, for patients who refer to physiotherapy with the diagnosis of musculoskeletal pain syndrome, the treatment is usually focused on the musculoskeletal structures, and less attention is paid to neurodynamic evaluation [14]. Therefore, the assessment and planning of physical therapy could be improved by understanding the prevalence of adverse neural tension in such patients and the relationship between pain intensity and functional disability. Also, most studies in this field have involved a limited number of participants [5, 6], and there is no exact estimation of the frequency of adverse neural tension in patients with these syndromes. Consequently, this study was primarily conducted to determine the frequency of adverse neural tension and its relationship with functional disability in upper extremity musculoskeletal pain syndromes.
Materials and Methods
This single-blind cross-sectional study was conducted at Shahid Beheshti Hospital in Babol City, Iran, from May 2021 to June 2022. The sample size was determined using relevant literature [11], resulting in recruiting 100 patients with musculoskeletal pain syndromes based on the inclusion and exclusion criteria.
The inclusion criteria included individuals aged 20 to 50 years diagnosed with upper extremity musculoskeletal pain syndromes, including shoulder impingement syndrome, lateral and medial epicondylitis of the elbow, and De Quervain syndrome [19-22]. The exclusion criteria comprised consumption of anti-inflammatory and analgesic drugs in the last 24 hours, suffering from systemic diseases (eg. diabetes, arthrosis, and rheumatoid arthritis), history of the spine and upper extremity surgery, restrictions of joint movement (eg. acute inflammation, infection, tissue tear, and fracture), severe trauma in the last 3 months, diseases that lead to adverse neural tension (such as cervical radiculopathy and peripheral neuropathies), bone abnormalities (eg. rib cervical and rostral acromion), a history of corticosteroid injection in the past one month, a history of physiotherapy treatment in the past 3 months, and significant limitations in the range of motion in each joint of the upper extremity, preventing the implementation of the neurodynamic test [23-26].
Data collection
Demographic information was collected via a standard questionnaire covering age, gender, height, weight, and duration of the lesion. Body mass index (BMI) was calculated by dividing weight in kg by the square of body height in meters [27]. Pain intensity was assessed through a visual analog scale (VAS) [28]. The functional disability of the upper extremity was investigated using the quick disabilities of the arm, shoulder, and hand (QDASH) questionnaire [29]. Ebrahimzadeh et al. proved the validity and reliability of the Persian version of this questionnaire [30].
Neurodynamic assessment
Before starting the main phase of the study, the reproducibility of these tests was examined by one intraexaminer and two interexaminers. 24 asymptomatic people participated in this study [31]. Neurodynamic evaluation was performed using the standard method provided by Shacklock and Butler for the median (Figure 1), radial (Figure 2), and ulnar (Figure 3) nerves bilaterally for both upper extremities [13, 32]. A 5 minute rest was observed between each test to avoid the therapeutic effects of the neurodynamic maneuver [33, 34]. Joint angles were measured using a standard goniometer according to the method of Martínez et al. and Covill et al. [35, 36]. For the neurodynamic evaluation of the median and radial nerves, the extension angle of the elbow joint, and for assessing the ulnar nerve, the abduction angle of the shoulder joint was measured when the test was positive.
The structural differentiation test determines the neurodynamic test’s positive result [13, 32]. If the patients’ symptoms increased during the neurodynamic test, increasing or decreasing the cumulative tension in the nerve on the reproduced symptoms was checked by moving a component completely away from the place of reporting the symptoms [13, 32]. When the main symptoms or complaints of the patients were not reproduced or aggravated by neurodynamic tests, the difference in the range of motion measured between the two extremities was recorded when a strong stretch was felt in the tested extremity. A significant difference in range of motion between elbow extension range (for median and radial nerve neurodynamic tests) and shoulder abduction range (for ulnar nerve neurodynamic test) on both sides was considered a positive neurodynamic evaluation. This difference was considered 27° for the median nerve, 20° for the radial nerve, and 6° for the ulnar nerve [35, 36].
Statistical analysis
Statistical analysis was performed using SPSS software, version 24. The relationship between quantitative variables was examined using the Pearson correlation test. The normality of the distribution of the variables was analyzed using the Kolmogorov-Smirnov test, indicating a normal distribution for all study variables. In this analysis, a P<0.05 was considered statistically significant.
Results
The demographic characteristics, including age, gender, height, weight, and BMI, were analyzed among the participants (Table 1).

The result of data frequency analysis showed that regardless of the type of lesion, out of 100 participants (some participants had more than one disease, a total of 112 cases of the disease were reported) who underwent neurodynamic evaluation, 50 patients (50%) exhibited at least one disorder in median, radial, or ulnar neural tension so that neurodynamic tests in 19 patients (19%) led to the reproduction or exacerbation of symptoms and in 39 patients (39%), a significant difference was observed in range of motion of joints on both sides. Table 2 presents the frequency of normal and adverse neural tension in upper extremity musculoskeletal pain syndromes by disease.
In 28 patients, the neurodynamic test of the median nerve yielded a positive result. Of these, the positive result of the median nerve test in 8 patients (8%) was based on the reproduction and worsening of symptoms, and in 20 patients (20%), based on a significant difference (>27°) in the elbow joint extension range of motion between the two sides.
In 30 patients (30%), adverse neural tension of the radial nerve was observed. The positive neurodynamic test of the radial nerve in 21 patients (21%) was based on the reproduction of symptoms and in 9 patients (9%) based on a significant difference (>20°) between the two sides in the range of motion of elbow joint extension.
The neurodynamic evaluation of the ulnar nerve showed that in 9 patients (9%), a significant difference (>6°) was observed in the abduction angle of the shoulder joint in both hands. In none of the participants, the neurodynamic test of the ulnar nerve led to the reproduction or exacerbation of symptoms.
The Pearson correlation test demonstrated no significant relationship between the level of functional disability and the intensity of adverse neural tension (according to the extension angle of the elbow joint) of the median and radial nerves. In addition, no significant relationship was observed between the level of functional disability and the severity of adverse neural tension (in terms of the abduction angle of the shoulder joint) of the ulnar nerve (Table 3).

Discussion
The results of our study indicate that at least one neurodynamic test was positive in 50% of patients with upper limb musculoskeletal pain syndromes (regardless of the type of lesion). Yaxley and Jull [11], showed adverse neural tension in some patients with tennis elbow; in addition, several other studies have pointed to neurodynamic disorders in patients with musculoskeletal pain syndromes [5, 6, 10].
The high prevalence of adverse neural tension observed may be due to different definitions of concepts and criteria for considering neurodynamic tests positive. This issue may lead to differences in the interpretation of the results of the study studies, especially when the positive criterion for the concept of adverse neural tension is crucial. The limited range of motion of the joints and the significant difference with the other side can be caused by the stretching of the muscle structures, its effect on the mechanical sensitivity of the nerve roots, and the creation of adverse neural tension [37].
The results showed that the highest frequency of adverse neural tension in the upper extremity was related to the radial nerve, followed by the median nerve, and the least frequency in the ulnar nerve. The high adverse radial neural tension rate can be explained by the higher prevalence of lateral epicondylitis among participants (67%) despite a higher incidence of shoulder impingement syndrome [38, 39]. The frequency of adverse tension of the radial nerve in patients with lateral epicondylitis was 40.3%; this rate was lower than the results of Yaxeley et al. [11]. Adverse neural tension of the radial nerve in patients with De Quervain syndrome may be due to the involvement of the superficial branch of the radial nerve in patients with this syndrome [40].
The adverse radial neural tension in patients with medial epicondylitis and shoulder impingement syndrome may be due to the transmission of the generated tension to the brachial plexus. As Kleinrensink et al. have shown, when a specific nerve in the upper extremity is examined via neurodynamic tests, the tension is transferred to the proximal part and the brachial plexus. A disorder in the common nerve roots can lead to reproduction or worsening symptoms [41].
The median nerve innervates the muscles involved in medial epicondylitis. Regarding the common nerve roots in the median and radial nerves (C6-8 roots), suprascapular, axillary, and radial nerves (C6 root), the disorder in common nerve roots can lead to adverse tension during the radial nerve test in patients with medial epicondylitis and shoulder impingement syndrome.
Regarding the common roots of the median nerve with the suprascapular, axillary, musculocutaneous (C6 root), and radial (C6-8 root) nerves, it is possible to check the disorders of these nerve roots with the median nerve test [41]. In addition, the muscle structures involved in medial epicondylitis are directly fed by the median nerve. The results showed that with regard to the more specific median nerve test compared to the radial and ulnar nerves; we can use this test to evaluate nerves with common roots [41].
The neurodynamic test of the ulnar nerve did not lead to the reproduction or worsening of symptoms in any participant; however, in 9 patients, a significant difference was observed in the abduction angle of the shoulder joint on both sides. The absence of reproduction or worsening of symptoms may be attributed to the level of tension disorder of the ulnar nerve, as it is lower than the other two nerves, and patients who suffer from tension disorders of the ulnar nerve show mild, latent, and subclinical symptoms. These disorders can manifest as limitations in the range of motion of the joints. In addition, none of the structures involved in the investigated lesions were directly innervated by the ulnar nerve.
Like Vegstein et al. and Fernández-de-Las-Peñas et al. study, our research suggests that patients with musculoskeletal pain syndromes may not initially present neurological symptoms [10, 42]. However, according to neurological theory, injury to musculoskeletal structures can lead to microscopic damage in the connective tissue of peripheral nerves, affecting the axoplasmic flow of nerves and disrupting nerve function [14, 43]. To our knowledge, past studies have not reported the prevalence or the role of adverse neural tension disorders in patients with upper extremity musculoskeletal pain syndromes, making it impossible to compare the obtained results with other studies.
According to our results, in patients with musculoskeletal pain syndromes with adverse neural tension, no significant relationship was observed between the level of functional disability, pain intensity, lesion duration, age, and BMI with the severity of adverse neural median, radial, and ulnar tension. In patients with higher intensity of adverse neural median and radial tension, the test becomes positive sooner (at higher angles) during a neurodynamic test when the elbow joint is extended. However, in the patients with higher intensity of adverse neural ulnar tension, the test becomes positive sooner (at lower angles) during a neurodynamic test when the elbow joint is extended.
Conclusion
According to our results, at least one of the neurodynamic tests becomes positive in a significant percentage of patients with upper extremity musculoskeletal pain syndromes. Considering the outcomes of this study, it is necessary to consider the neurological component in evaluating patients with musculoskeletal pain syndromes. A neurodynamic assessment helps therapists assess the role and contribution of neurological disorders in the development of symptoms, facilitating the design of an appropriate treatment plan based on the etiology of the injury.
Ethical Considerations
Compliance with ethical guidelines
Objectives, procedures, possible advantages and disadvantages of the study clearly for the participants were explained. Each participant signed a written informed consent form. All methods in accordance with ethical approval and guidelines and regulations the relevant was done at the study site. The study protocol was approved by the Ethics Committee of Babol University of Medical Sciences (Code: IR.MUBABOL.REC.1400.063).
Funding
The paper was extracted from the master's thesis of Milad Taheri, approved by the Department of Physiotherapy, School of Rehabilitation, Babol University of Medical Sciences. This study was also supported by Vice President of Research and Technology of Babol University of Medical Sciences.
Authors' contributions
Conceptualization: Milad Taheri, Ghadamali Talebiand Mohammad Taghipour; Methodology and validation: Milad Taheri, Ghadamali Talebi, Mohammad Taghipour and Massoud Bahrami; Visualization: Milad Taheri; Analysis and research: All authors; Writing-original draft: Milad Taheri; Editing and finalization: Ghadamali Talebi, Mohammad Taghipour; Supervision: Ghadamali Talebi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate and thank the honorable personnel of the physiotherapy department of Shahid Beheshti Hospital in Babol for the services of this study.
References
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bulletin of The World Health Organization. 2003; 81(9):646-56. [PMID]
- Horton R. GBD 2010: Understanding disease, injury, and risk. The Lancet. 2012; 380(9859):2053-4. [DOI:10.1016/S0140-6736(12)62133-3] [PMID]
- Bernard BP. Musculoskeletal Disorders (MSDs) and workplace factors: A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. US Department of Health and Human Services. Washington: National Institute for Occupational Safety and Health; 1997. [Link]
- Panel on Musculoskeletal Disorders and the Workplace, Institute of Medicine. Musculoskeletal disorders and the workplace: Low back and upper extremities. Washington: National Academy Press; 2001. [Link]
- Ekstrom RA, Holden K. Examination of and intervention for a patient with chronic lateral elbow pain with signs of nerve entrapment. Physical Therapy. 2002; 82(11):1077-86. [DOI:10.1093/ptj/82.11.1077]
- Farrell K, Lampe K. Addressing neurodynamic irritability in a patient with adhesive capsulitis: A case report. Journal of Manual & Manipulative Therapy. 2017; 25(1):47-56. [DOI:10.1179/2042618614Y.0000000092] [PMID]
- Matocha MA, Baker RT, Nasypany AM, Seegmiller JG. Effects of neuromobilization on tendinopathy: Part II. International Journal of Athletic Therapy and Training. 2015; 20(2):41-7. [DOI:10.1123/ijatt.2014-0097]
- Matocha MA, Baker RT, Nasypany AM, Seegmiller JG. Effects of neuromobilization on tendinopathy: Part I. International Journal of Athletic Therapy and Training. 2015; 20(2):36-40. [Link]
- Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Physical Therapy in Sport. 2006; 7(1):36-49. [DOI:10.1016/j.ptsp.2005.10.002]
- Vegstein K, Robinson HS, Jensen R. Neurodynamic tests for patellofemoral pain syndrome: A pilot study. Chiropractic & Manual Therapies. 2019; 27:26. [DOI:10.1186/s12998-019-0242-2] [PMID]
- Yaxley GA, Jull GA. Adverse tension in the neural system. A preliminary study of tennis elbow. Australian Journal of Physiotherapy. 1993; 39(1):15-22. [DOI:10.1016/S0004-9514(14)60465-7] [PMID]
- Shacklock M. Neurodynamics. Physiotherapy. 1995; 81(1):9-16. [DOI:10.1016/S0031-9406(05)67024-1]
- Shacklock M. Clinical neurodynamics: A new system of neuromusculoskeletal treatment. Amsterdam: Elsevier Health Sciences; 2005. [Link]
- Butler DS, Matheson J. The sensitive nervous system. Adelaide: Noigroup Publications; 2000. [Link]
- Chan L, Turner JA, Comstock BA, Levenson LM, Hollingworth W, Heagerty PJ, et al. The relationship between electrodiagnostic findings and patient symptoms and function in carpal tunnel syndrome. Archives of Physical Medicine and Rehabilitation. 2007; 88(1):19-24. [DOI:10.1016/j.apmr.2006.10.013] [PMID]
- Mackinnon SE. Double and multiple” crush” syndromes. Double and multiple entrapment neuropathies. Hand Clinics. 1992; 8(2):369-90. [DOI:10.1016/S0749-0712(21)00722-8] [PMID]
- Butler DS, Jones MA. Mobilisation of the nervous system. London: Churchill Livingstone; 2004. [Link]
- George SZ. Characteristics of patients with lower extremity symptoms treated with slump stretching: A case series. Journal of Orthopaedic & Sports Physical Therapy. 2002; 32(8):391-8. [DOI:10.2519/jospt.2002.32.8.391] [PMID]
- Kheterpal AB, Bredella MA. Overuse injuries of the elbow. Radiologic Clinics Of North America. 2019; 57(5):931-42. [DOI:10.1016/j.rcl.2019.03.005] [PMID]
- Llopis E, Restrepo R, Kassarjian A, Cerezal L. Overuse injuries of the wrist. Radiologic Clinics of North America. 2019; 57(5):957-76. [DOI:10.1016/j.rcl.2019.05.001] [PMID]
- Budoff JE, Nirschl RP, Guidi EJ. Débridement of partial-thickness tears of the rotator cuff without acromioplasty. Long-term follow-up and review of the literature. The Journal of Bone and Joint Surgery. American Volume. 1998; 80(5):733-48. [DOI:10.2106/00004623-199805000-00016] [PMID]
- Arumugam V, Selvam S, MacDermid JC. Radial nerve mobilization reduces lateral elbow pain and provides short-term relief in computer users. The Open Orthopaedics Journal. 2014; 8:368-71. [DOI:10.2174/1874325001408010368] [PMID]
- Akhtar M, Karimi H, Gilani SA, Ahmad A. Effects of routine physiotherapy with and without neuromobilization in the management of internal shoulder impingement syndrome: A randomized controlled trial. Pakistan Journal of Medical Sciences. 2020; 36(4):596-602. [DOI:10.12669/pjms.36.4.1545] [PMID]
- Villafañe JH, Silva GB, Bishop MD, Fernandez-Carnero J. Radial nerve mobilization decreases pain sensitivity and improves motor performance in patients with thumb carpometacarpal osteoarthritis: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2012; 93(3):396-403. [DOI:10.1016/j.apmr.2011.08.045] [PMID]
- Schmid AB, Brunner F, Luomajoki H, Held U, Bachmann LM, Künzer S, et al. Reliability of clinical tests to evaluate nerve function and mechanosensitivity of the upper limb peripheral nervous system. BMC Musculoskeletal Disorders. 2009; 10:11. [DOI:10.1186/1471-2474-10-11] [PMID]
- Brown M, Hislop H, Avers D. Daniels and Worthingham’s muscle Testing-E-Book: Techniques of manual examination and performance testing. Amsterdam: Elsevier Health Sciences; 2013. [Link]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet (London, England). 2004; 363(9403):157-63. [DOI:10.1016/S0140-6736(03)15268-3]
- Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Research in Nursing & Health. 1990; 13(4):227-36. [DOI:10.1002/nur.4770130405] [PMID]
- Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (Quick DASH): Validity and reliability based on responses within the full-length DASH. BMC Musculoskeletal Disorders. 2006; 7:44.[DOI:10.1186/1471-2474-7-44] [PMID]
- Ebrahimzadeh MH, Moradi A, Vahedi E, Kachooei AR, Birjandinejad A. Validity and reliability of the Persian version of shortened Disabilities of The Arm, Shoulder and Hand Questionnaire (quick-DASH). International Journal of Preventive Medicine. 2015; 6:59. [DOI:10.4103/2008-7802.160336] [PMID]
- Taheri M, Talebi G, Taghipour M, Bahrami M, Gholinia H. Reliability of Upper Limb Neurodynamic Tests: Median, radial, and ulnar nerves. Archives of Rehabilitation. 2022; 23(3):334-51. [DOI:10.32598/RJ.23.3.71.3]
- Butler D, Gifford L. The concept of adverse mechanical tension in the nervous system part 1: Testing for “Dural tension”. Physiotherapy. 1989; 75(11):622-9. [DOI:10.1016/S0031-9406(10)62374-7]
- Vanti C, Conteddu L, Guccione A, Morsillo F, Parazza S, Viti C, et al. The Upper Limb Neurodynamic Test 1: Intra-and intertester reliability and the effect of several repetitions on pain and resistance. Journal of Manipulative and Physiological Therapeutics. 2010; 33(4):292-9. [DOI:10.1016/j.jmpt.2010.03.003] [PMID]
- Coppieters M, Stappaerts K, Janssens K, Jull G. Reliability of detecting ‘onset of pain’ and ‘submaximal pain’ during neural provocation testing of the upper quadrant. Physiotherapy Research International. 2002; 7(3):146-56. [DOI:10.1002/pri.251] [PMID]
- Martínez MD, Cubas CL, Girbés EL. Ulnar nerve neurodynamic test: Study of the normal sensory response in asymptomatic individuals. Journal of Orthopaedic & Sports Physical Therapy. 2014; 44(6):450-6. [DOI:10.2519/jospt.2014.5207] [PMID]
- Covill LG, Petersen SM. Upper extremity neurodynamic tests: Range of motion asymmetry may not indicate impairment. Physiotherapy Theory and Practice. 2012; 28(7):535-41. [DOI:10.3109/09593985.2011.641198] [PMID]
- Lohkamp M, Small K. Normal response to upper limb neurodynamic test 1 and 2A. Manual Therapy. 2011; 16(2):125-30. [DOI:10.1016/j.math.2010.07.008] [PMID]
- Ostör AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL. Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology. 2005; 44(6):800-5. [DOI:10.1093/rheumatology/keh598] [PMID]
- Herquelot E, Guéguen A, Roquelaure Y, Bodin J, Sérazin C, Ha C, et al. Work-related risk factors for incidence of lateral epicondylitis in a large working population. Scandinavian Journal of Work, Environment & Health. 2013; 39(6):578-88. [DOI:10.5271/sjweh.3380] [PMID]
- Becciolini M, Pivec C, Raspanti A, Riegler G. Ultrasound of the radial nerve: A pictorial review. Journal of Ultrasound in Medicine. 2021; 40(12):2751-71. [DOI:10.1002/jum.15664] [PMID]
- Kleinrensink GJ, Stoeckart R, Mulder PG, Hoek G, Broek T, Vleeming A, et al. Upper limb tension tests as tools in the diagnosis of nerve and plexus lesions. Anatomical and biomechanical aspects. Clinical Biomechanics. 2000; 15(1):9-14. [DOI:10.1016/S0268-0033(99)00042-X] [PMID]
- Fernández-de-Las-Peñas C, Ortega-Santiago R, Ambite-Quesada S, Jiménez-Garcí A R, Arroyo-Morales M, Cleland JA. Specific mechanical pain hypersensitivity over peripheral nerve trunks in women with either unilateral epicondylalgia or carpal tunnel syndrome. Journal of Orthopaedic & Sports Physical Therapy. 2010; 40(11):751-60. [DOI:10.2519/jospt.2010.3331] [PMID]
- Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006; 45(5):508-21. [DOI:10.1093/rheumatology/kel046] [PMID]
Type of Study: Original |
Subject:
Physical Therapy
Received: 10/02/2023 | Accepted: 20/05/2023 | Published: 1/10/2023
Received: 10/02/2023 | Accepted: 20/05/2023 | Published: 1/10/2023
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |